Could We Expect Postoperative Cup Anteversion after Total Hip Arthroplasty Using Postoperative Plain Anteroposterior and Lateral Radiograph? A Three-Dimensional Experimental Operation Study
Abstract
:1. Background
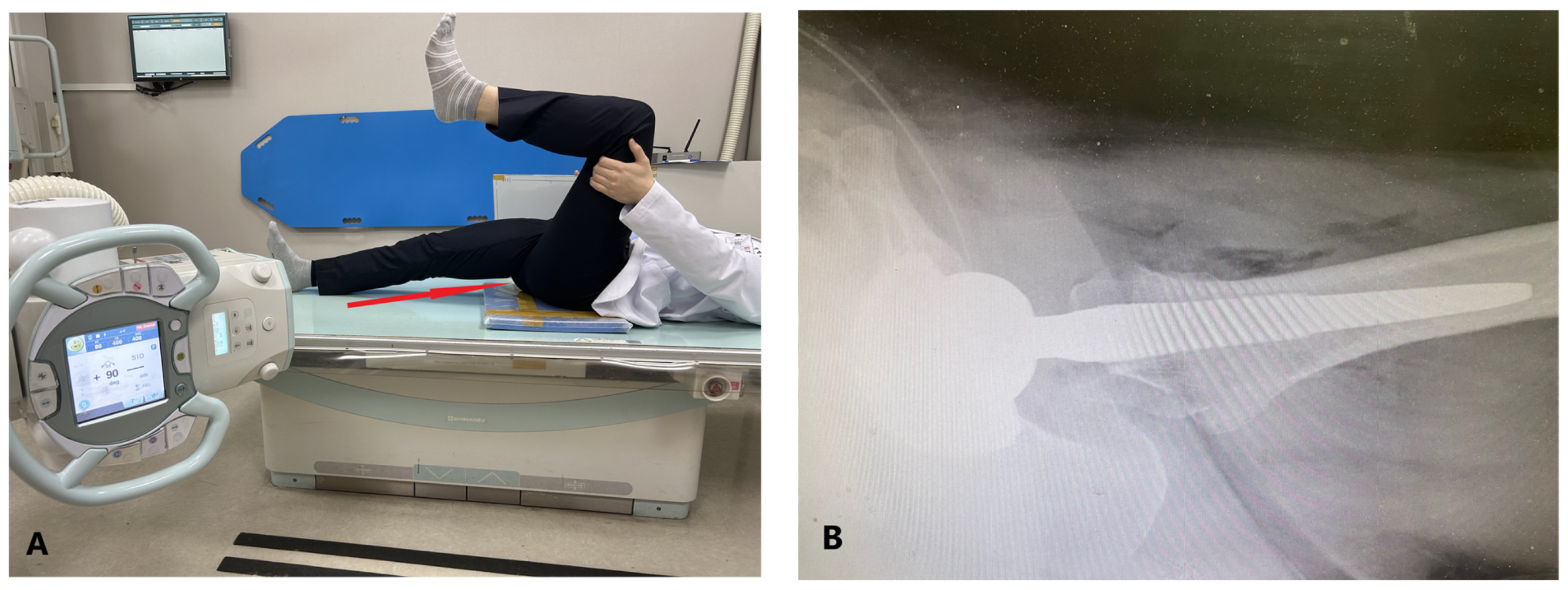
2. Methods
2.1. Data Collection
2.2. Statistical Analysis
3. Results
4. Discussion
5. Conclusions
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Acknowledgments
Conflicts of Interest
References
- Statstics Korea. Top 20 Frequent Diseases by Operation. Available online: https://kosis.kr/statHtml/statHtml.do?orgId=350&tblId=DT_350004N_A003&conn_path=I2 (accessed on 15 June 2023).
- Charnley, J. Arthroplasty of the hip. A new operation. Lancet 1961, 1, 1129–1132. [Google Scholar] [CrossRef]
- Meek, R.M.; Allan, D.B.; McPhillips, G.; Kerr, L.; Howie, C.R. Epidemiology of Dislocation after Total Hip Arthroplasty. Clin. Orthop. Relat. Res. 2006, 447, 9–18. [Google Scholar] [CrossRef]
- Soong, M.; Rubash, H.E.; Macaulay, W. Dislocation after total hip arthroplasty. J. Am. Acad. Orthop. Surg. 2004, 12, 314–321. [Google Scholar] [CrossRef]
- Woo, R.Y.; Morrey, B.F. Dislocations after total hip arthroplasty. J. Bone Joint Surg. Am. 1982, 64, 1295–1306. [Google Scholar] [CrossRef]
- Ali Khan, M.A.; Brakenbury, P.H.; Reynolds, I.S. Dislocation following total hip replacement. J. Bone Joint Surg. Br. 1981, 63-b, 214–218. [Google Scholar] [CrossRef]
- Gillinov, S.M.; Joo, P.Y.; Zhu, J.R.; Moran, J.; Rubin, L.E.; Grauer, J.N. Incidence, Timing, and Predictors of Hip Dislocation After Primary Total Hip Arthroplasty for Osteoarthritis. J. Am. Acad. Orthop. Surg. 2022, 30, 1047–1053. [Google Scholar] [CrossRef]
- Ciriello, V.; La China, R.; Chirillo, D.F.; Bianco, G.; Fusini, F.; Scarlato, U.; Albanese, C.; Bonzanini, G.; Banci, L.; Piovani, L. Is Modular Dual Mobility Superior to Standard Bearings for Reducing Dislocation Risk after Primary Total Hip Arthroplasty? A Retrospective Comparative Multicenter Study. J. Clin. Med. 2023, 12, 4200. [Google Scholar] [CrossRef]
- Rowan, F.E.; Benjamin, B.; Pietrak, J.R.; Haddad, F.S. Prevention of Dislocation After Total Hip Arthroplasty. J. Arthroplast. 2018, 33, 1316–1324. [Google Scholar] [CrossRef] [PubMed]
- Gwam, C.U.; Mistry, J.B.; Mohamed, N.S.; Thomas, M.; Bigart, K.C.; Mont, M.A.; Delanois, R.E. Current Epidemiology of Revision Total Hip Arthroplasty in the United States: National Inpatient Sample 2009 to 2013. J. Arthroplast. 2017, 32, 2088–2092. [Google Scholar] [CrossRef] [PubMed]
- Fackler, C.D.; Poss, R. Dislocation in total hip arthroplasties. Clin. Orthop. Relat. Res. 1980, 151, 169–178. [Google Scholar] [CrossRef]
- Seagrave, K.G.; Troelsen, A.; Malchau, H.; Husted, H.; Gromov, K. Acetabular cup position and risk of dislocation in primary total hip arthroplasty. Acta Orthop. 2017, 88, 10–17. [Google Scholar] [CrossRef] [PubMed]
- Opperer, M.; Lee, Y.Y.; Nally, F.; Blanes Perez, A.; Goudarz-Mehdikhani, K.; Gonzalez Della Valle, A. A critical analysis of radiographic factors in patients who develop dislocation after elective primary total hip arthroplasty. Int. Orthop. 2016, 40, 703–708. [Google Scholar] [CrossRef] [PubMed]
- Lewinnek, G.E.; Lewis, J.L.; Tarr, R.; Compere, C.L.; Zimmerman, J.R. Dislocations after total hip-replacement arthroplasties. J. Bone Joint Surg. Am. 1978, 60, 217–220. [Google Scholar] [CrossRef]
- Snijders, T.E.; Schlösser, T.P.C.; Heckmann, N.D.; Tezuka, T.; Castelein, R.M.; Stevenson, R.P.; Weinans, H.; de Gast, A.; Dorr, L.D. The Effect of Functional Pelvic Tilt on the Three-Dimensional Acetabular Cup Orientation in Total Hip Arthroplasty Dislocations. J. Arthroplast. 2021, 36, 2184–2188.e2181. [Google Scholar] [CrossRef]
- Brown, T.D.; Elkins, J.M.; Pedersen, D.R.; Callaghan, J.J. Impingement and dislocation in total hip arthroplasty: Mechanisms and consequences. Iowa Orthop. J. 2014, 34, 1–15. [Google Scholar]
- Liaw, C.K.; Hou, S.M.; Yang, R.S.; Wu, T.Y.; Fuh, C.S. A new tool for measuring cup orientation in total hip arthroplasties from plain radiographs. Clin. Orthop. Relat. Res. 2006, 451, 134–139. [Google Scholar] [CrossRef]
- Widmer, K.H. A simplified method to determine acetabular cup anteversion from plain radiographs. J. Arthroplast. 2004, 19, 387–390. [Google Scholar] [CrossRef] [PubMed]
- Hassan, D.M.; Johnston, G.H.; Dust, W.N.; Watson, L.G.; Cassidy, D. Radiographic calculation of anteversion in acetabular prostheses. J. Arthroplast. 1995, 10, 369–372. [Google Scholar] [CrossRef] [PubMed]
- Ackland, M.K.; Bourne, W.B.; Uhthoff, H.K. Anteversion of the acetabular cup. Measurement of angle after total hip replacement. J. Bone Joint Surg. Br. 1986, 68, 409–413. [Google Scholar] [CrossRef] [PubMed]
- Marx, A.; von Knoch, M.; Pförtner, J.; Wiese, M.; Saxler, G. Misinterpretation of cup anteversion in total hip arthroplasty using planar radiography. Arch. Orthop. Trauma. Surg. 2006, 126, 487–492. [Google Scholar] [CrossRef]
- Kalteis, T.; Handel, M.; Herold, T.; Perlick, L.; Paetzel, C.; Grifka, J. Position of the acetabular cup -- accuracy of radiographic calculation compared to CT-based measurement. Eur. J. Radiol. 2006, 58, 294–300. [Google Scholar] [CrossRef]
- Pulos, N.; Tiberi Iii, J.V., 3rd; Schmalzried, T.P. Measuring acetabular component position on lateral radiographs—Ischio-lateral method. Bull. NYU Hosp. Jt. Dis. 2011, 69 (Suppl. S1), S84–S89. [Google Scholar]
- Nunley, R.M.; Keeney, J.A.; Zhu, J.; Clohisy, J.C.; Barrack, R.L. The reliability and variation of acetabular component anteversion measurements from cross-table lateral radiographs. J. Arthroplast. 2011, 26, 84–87. [Google Scholar] [CrossRef]
- Yao, L.; Yao, J.; Gold, R.H. Measurement of acetabular version on the axiolateral radiograph. Clin. Orthop. Relat. Res. 1995, 106–111. [Google Scholar] [CrossRef]
- Reikeras, O.; Gunderson, R.B. Cross table lateral radiography for measurement of acetabular cup version. Ann. Transl. Med. 2016, 4, 169. [Google Scholar] [CrossRef]
- Shin, W.C.; Lee, S.M.; Lee, K.W.; Cho, H.J.; Lee, J.S.; Suh, K.T. The reliability and accuracy of measuring anteversion of the acetabular component on plain anteroposterior and lateral radiographs after total hip arthroplasty. Bone Joint J. 2015, 97-b, 611–616. [Google Scholar] [CrossRef] [PubMed]
- Murray, D.W. The definition and measurement of acetabular orientation. J. Bone Joint Surg. Br. 1993, 75, 228–232. [Google Scholar] [CrossRef] [PubMed]
- Pankaj, A.; Mittal, A.; Chawla, A. The validity and reproducibility of cross table radiographs compared with CT scans for the measurement of anteversion of the acetabular component after total hip arthroplasty. Bone Joint J. 2017, 99-b, 1006–1011. [Google Scholar] [CrossRef] [PubMed]
- Lim, S.J.; Park, Y.S. Plain Radiography of the Hip: A Review of Radiographic Techniques and Image Features. Hip Pelvis 2015, 27, 125–134. [Google Scholar] [CrossRef]
- Faul, F.; Erdfelder, E.; Buchner, A.; Lang, A.G. Statistical power analyses using G*Power 3.1: Tests for correlation and regression analyses. Behav. Res. Methods 2009, 41, 1149–1160. [Google Scholar] [CrossRef] [PubMed]
- Faul, F.; Erdfelder, E.; Lang, A.G.; Buchner, A. G*Power 3: A flexible statistical power analysis program for the social, behavioral, and biomedical sciences. Behav. Res. Methods 2007, 39, 175–191. [Google Scholar] [CrossRef] [PubMed]
- Harris, W.H. Advances in surgical technique for total hip replacement: Without and with osteotomy of the greater trochanter. Clin. Orthop. Relat. Res. 1980, 188–204. [Google Scholar] [CrossRef]
- Pradhan, R. Planar anteversion of the acetabular cup as determined from plain anteroposterior radiographs. J. Bone Joint Surg. Br. 1999, 81, 431–435. [Google Scholar] [CrossRef] [PubMed]
- Zuh, S.G.; Zazgyva, A.; Gergely, I.; Pop, T.S. Acetabuloplasty with bone grafting in uncemented hip replacement for protrusion. Int. Orthop. 2015, 39, 1757–1763. [Google Scholar] [CrossRef] [PubMed]
- Stephens, A.; Munir, S.; Shah, S.; Walter, W.L. The kinematic relationship between sitting and standing posture and pelvic inclination and its significance to cup positioning in total hip arthroplasty. Int. Orthop. 2015, 39, 383–388. [Google Scholar] [CrossRef]





| Gender | ||||
|---|---|---|---|---|
| Total | Male | Female | p Value | |
| AA | 20.1 ± 6.1 | 18.0 ± 5.7 | 22.6 ± 5.8 | 0.004 |
| RA | 15.5 ± 4.8 | 14.0 ± 4.6 | 17.1 ± 4.6 | 0.008 |
| OA | 23.3 ± 7.3 | 21.4 ± 6.9 | 25.2 ± 7.2 | 0.04 |
| AI | 51.5 ± 4.7 | 51.8 ± 5.0 | 51.1 ± 4.6 | 0.57 |
| RI | 49.5 ± 4.9 | 50.3 ± 5.0 | 48.8 ± 4.7 | 0.23 |
| OI | 46.9 ± 4.5 | 48.0 ± 4.7 | 45.7 ± 4.1 | 0.04 |
| WM | 15.6 ± 4.8 | 14.1 ± 4.6 | 17.2 ± 4.6 | 0.009 |
Disclaimer/Publisher’s Note: The statements, opinions and data contained in all publications are solely those of the individual author(s) and contributor(s) and not of MDPI and/or the editor(s). MDPI and/or the editor(s) disclaim responsibility for any injury to people or property resulting from any ideas, methods, instructions or products referred to in the content. |
© 2023 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Lee, T.S.; Kwon, H.M.; Park, J.Y.; Kim, D.K.; Kang, K.T.; Park, K.K. Could We Expect Postoperative Cup Anteversion after Total Hip Arthroplasty Using Postoperative Plain Anteroposterior and Lateral Radiograph? A Three-Dimensional Experimental Operation Study. J. Clin. Med. 2023, 12, 6664. https://doi.org/10.3390/jcm12206664
Lee TS, Kwon HM, Park JY, Kim DK, Kang KT, Park KK. Could We Expect Postoperative Cup Anteversion after Total Hip Arthroplasty Using Postoperative Plain Anteroposterior and Lateral Radiograph? A Three-Dimensional Experimental Operation Study. Journal of Clinical Medicine. 2023; 12(20):6664. https://doi.org/10.3390/jcm12206664
Chicago/Turabian StyleLee, Tae Sung, Hyuck Min Kwon, Jun Young Park, Dong Ki Kim, Kyoung Tak Kang, and Kwan Kyu Park. 2023. "Could We Expect Postoperative Cup Anteversion after Total Hip Arthroplasty Using Postoperative Plain Anteroposterior and Lateral Radiograph? A Three-Dimensional Experimental Operation Study" Journal of Clinical Medicine 12, no. 20: 6664. https://doi.org/10.3390/jcm12206664







