How Effective Are Non-Frictional Techniques Compared to Sliding Techniques in the Retraction of Upper Anterior Teeth When Using Buccal Fixed-Appliance Therapy? A Systematic Review
Abstract
:1. Introduction
2. Materials and Methods
2.1. Eligibility Criteria
2.2. Search Strategy
2.3. Study Selection and Data Extraction
2.4. Assessment of Risk of Bias in Individual Studies
3. Results
3.1. Literature Search Flow and the Retrieved Studies
3.2. Characteristics of the Included Studies
3.3. Risk of Bias of Included Studies
3.4. Effects of Intervention
3.4.1. First: Canine Retraction
Rate of Canine Retraction
Canine Tipping and Rotation Change during Canine Retraction
Anchorage Loss following Canine Retraction
Root Resorption following Canine Retraction
3.4.2. Second: Incisor Retraction
Rate of the Incisor Retraction
Anchorage Loss following Incisor Retraction
3.4.3. Third: Retraction of the Upper Six Anterior Teeth
Rate of the En-Masse Retraction
Anchorage Loss following En-Masse Retraction
Changes in Anterior Tooth Torque following En-Masse Retraction
4. Discussion
4.1. Rate of Canine Retraction
4.2. Canine Tipping and Rotation Change
4.3. Anchorage Loss of Canine Retraction
4.4. Root Resorption of Canine Retraction
4.5. Anchorage Loss following Incisor Retraction
4.6. Rate and Torque Change of En-Masse Retraction
4.7. Anchorage Loss following En-Masse Retraction
4.8. Limitations
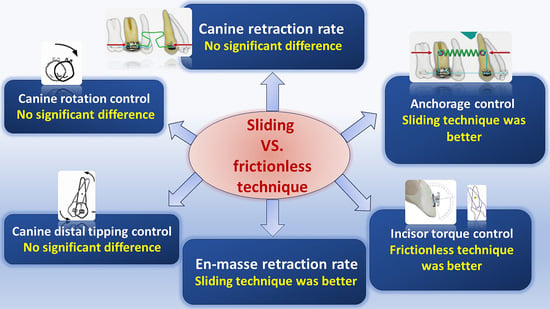
5. Conclusions
Supplementary Materials
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Conflicts of Interest
Appendix A
| PubMed | #1 (permanent occlusion OR class II relationship OR excessive overjet OR maxillary dentoalveolar protrusion OR bimaxillary protrusion OR severe crowding OR anterior open bite OR first premolar extraction) #2 (Anterior teeth retraction OR incisors retraction OR canine retraction OR En masse retraction OR moving anterior teeth backward OR space closure) #3 (Orthodontic tooth movement rate OR orthodontic tooth movement amount OR orthodontic tooth movement velocity OR orthodontic tooth movement speed OR orthodontic tooth movement duration OR anchorage loss OR Rotation OR inclination OR torque OR angulation OR tipping OR root resorption) #4 (Segmental technique OR Segmented technique OR sectional OR Frictionless Mechanics OR T-loop OR L-loop OR Loop-based technique OR Ricketts’s spring OR Gjessing retraction arch OR Ladanyi spring OR Marcotte spring OR Reverse Closing Loop OR Retraction spring) #5 #1 AND #2 AND #3 AND #4 |
| CENTRAL (The Cochrane Library) | #1 (permanent occlusion OR class Ⅱ relationship OR excessive overjet OR maxillary dentoalveolar protrusion OR bimaxillary protrusion OR severe crowding OR anterior open bite OR first premolar extraction) #2 (Anterior teeth retraction OR incisors retraction OR canine retraction OR En masse retraction OR moving anterior teeth backward OR space closure) #3 (Orthodontic tooth movement rate OR orthodontic tooth movement amount OR orthodontic tooth movement velocity OR orthodontic tooth movement speed OR orthodontic tooth movement duration OR anchorage loss OR Rotation OR inclination OR torque OR angulation OR tipping OR root resorption) #4 (Segmental technique OR Segmented technique OR sectional OR Frictionless Mechanics OR T-loop OR L-loop OR Loop-based technique OR Ricketts’s spring OR Gjessing retraction arch OR Ladanyi spring OR Marcotte spring OR Reverse Closing Loop OR Retraction spring) #5 #1 AND #2 AND #3 AND #4 |
| Web of Science | #1TS= (permanent occlusion OR class Ⅱ relationship OR excessive overjet OR maxillary dentoalveolar protrusion OR bimaxillary protrusion OR severe crowding OR anterior open bite OR first premolar extraction) #2TS = (Anterior teeth retraction OR incisors retraction OR canine retraction OR En masse retraction OR moving anterior teeth backward OR space closure) #3TS = (Orthodontic tooth movement rate OR orthodontic tooth movement amount OR orthodontic tooth movement velocity OR orthodontic tooth movement speed OR orthodontic tooth movement duration OR anchorage loss OR Rotation OR inclination OR torque OR angulation OR tipping OR root resorption) #4TS = (Segmental technique OR Segmented technique OR sectional OR Frictionless Mechanics OR T-loop OR L-loop OR Loop-based technique OR Ricketts’s spring OR Gjessing retraction arch OR Ladanyi spring OR Marcotte spring OR Reverse Closing Loop OR Retraction spring) #5 #1 AND #2 AND #3 AND #4 |
| Scopus | #1 TITLE ABS-KEY (permanent occlusion OR class II relationship OR excessive overjet OR maxillary dentoalveolar protrusion OR bimaxillary protrusion OR severe crowding OR anterior open bite OR first premolar extraction) #2 TITLE ABS-KEY (Anterior teeth retraction OR incisors retraction OR canine retraction OR En masse retraction OR moving anterior teeth backward OR space closure) #3 TITLE ABS-KEY (Orthodontic tooth movement rate OR orthodontic tooth movement amount OR orthodontic tooth movement velocity OR orthodontic tooth movement speed OR orthodontic tooth movement duration OR anchorage loss OR Rotation OR inclination OR torque OR angulation OR tipping OR root resorption) #4 TITLE ABS-KEY (Segmental technique OR Segmented technique OR sectional OR Frictionless Mechanics OR T-loop OR L-loop OR Loop-based technique OR Ricketts’s spring OR Gjessing retraction arch OR Ladanyi spring OR Marcotte spring OR Reverse Closing Loop OR Retraction spring) #5 #1 AND #2 AND #3 AND #4 |
| EMBASE | #1 (permanent occlusion OR class II relationship OR excessive overjet OR maxillary dentoalveolar protrusion OR bimaxillary protrusion OR severe crowding OR anterior open bite OR first premolar extraction) #2 (Anterior teeth retraction OR incisors retraction OR canine retraction OR En masse retraction OR moving anterior teeth backward OR space closure) #3 (Orthodontic tooth movement rate OR orthodontic tooth movement amount OR orthodontic tooth movement velocity OR orthodontic tooth movement speed OR orthodontic tooth movement duration OR anchorage loss OR Rotation OR inclination OR torque OR angulation OR tipping OR root resorption) #4 (Segmental technique OR Segmented technique OR sectional OR Frictionless Mechanics OR T-loop OR L-loop OR Loop-based technique OR Ricketts’s spring OR Gjessing retraction arch OR Ladanyi spring OR Marcotte spring OR Reverse Closing Loop OR Retraction spring) #5 #1 AND #2 AND #3 AND #4 |
| Google scholar | (permanent occlusion OR class II relationship OR excessive overjet OR maxillary dentoalveolar protrusion OR bimaxillary protrusion OR severe crowding OR anterior open bite OR first premolar extraction) AND (Anterior teeth retraction OR incisors retraction OR canine retraction OR En masse retraction OR moving anterior teeth backward OR space closure) AND (Orthodontic tooth movement rate OR orthodontic tooth movement amount OR orthodontic tooth movement velocity OR orthodontic tooth movement speed OR orthodontic tooth movement duration OR anchorage loss OR Rotation OR inclination OR torque OR angulation OR tipping OR root resorption) AND (Segmental technique OR Segmented technique OR sectional OR Frictionless Mechanics OR T-loop OR L-loop OR Loop-based technique OR Ricketts’s spring OR Gjessing retraction arch OR Ladanyi spring OR Marcotte spring OR Reverse Closing Loop OR Retraction spring) |
| Trip | (permanent occlusion OR class II relationship OR excessive overjet OR maxillary dentoalveolar protrusion OR bimaxillary protrusion OR severe crowding OR anterior open bite OR first premolar extraction) AND (Anterior teeth retraction OR incisors retraction OR canine retraction OR En masse retraction OR moving anterior teeth backward OR space closure) AND (Orthodontic tooth movement rate OR orthodontic tooth movement amount OR orthodontic tooth movement velocity OR orthodontic tooth movement speed OR orthodontic tooth movement duration OR anchorage loss OR Rotation OR inclination OR torque OR angulation OR tipping OR root resorption) AND (Segmental technique OR Segmented technique OR sectional OR Frictionless Mechanics OR T-loop OR L-loop OR Loop-based technique OR Ricketts’s spring OR Gjessing retraction arch OR Ladanyi spring OR Marcotte spring OR Reverse Closing Loop OR Retraction spring) |
References
- Bishara, S.E. Textbook of Orthodontics; WB Saunders Company: Philadelphia, PA, USA, 2001. [Google Scholar]
- Khlef, H.N.; Hajeer, M.Y.; Ajaj, M.A.; Heshmeh, O.; Youssef, N.; Mahaini, L. The effectiveness of traditional corticotomy vs flapless corticotomy in miniscrew-supported en-masse retraction of maxillary anterior teeth in patients with Class II Division 1 malocclusion: A single-centered, randomized controlled clinical trial. Am. J. Orthod. Dentofac. Orthop. 2020, 158, e111–e120. [Google Scholar] [CrossRef] [PubMed]
- Al-Sibaie, S.; Hajeer, M.Y. Assessment of changes following en-masse retraction with mini-implants anchorage compared to two-step retraction with conventional anchorage in patients with class II division 1 malocclusion: A randomized controlled trial. Eur. J. Orthod. 2014, 36, 275–283. [Google Scholar] [CrossRef]
- Leonardi, R.; Annunziata, A.; Licciardello, V.; Barbato, E. Soft tissue changes following the extraction of premolars in nongrowing patients with bimaxillary protrusion. A systematic review. Angle Orthod. 2010, 80, 211–216. [Google Scholar] [CrossRef] [PubMed]
- Masaes, M.M.; Burhan, A.S.; Youssef, M.; Nawaya, F.R. T-loop spring vs. Ricketts maxillary canine retractor in canine retraction efficacy and anchorage loss control: A CBCT study. AJO-DO Clin. Companion 2022, 2, 26–40. [Google Scholar]
- Mohammed, H.; Rizk, M.Z.; Wafaie, K.; Almuzian, M. Effectiveness of nickel-titanium springs vs elastomeric chains in orthodontic space closure: A systematic review and meta-analysis. Orthod. Craniofac. Res. 2018, 21, 12–19. [Google Scholar] [CrossRef]
- Felemban, N.H.; Al-Sulaimani, F.F.; Murshid, Z.A.; Hassan, A.H. En masse retraction versus two-step retraction of anterior teeth in extraction treatment of bimaxillary protrusion. J. Orthod. Sci. 2013, 2, 28–37. [Google Scholar] [CrossRef]
- Sarikaya, S.; Haydar, B.; Ciger, S.; Ariyurek, M. Changes in alveolar bone thickness due to retraction of anterior teeth. Am. J. Orthod. Dentofac. Orthop. 2022, 122, 15–26. [Google Scholar] [CrossRef]
- Al-Imam, G.M.F.; Ajaj, M.A.; Hajeer, M.Y.; Al-Mdalal, Y.; Almashaal, E. Evaluation of the effectiveness of piezocision-assisted flapless corticotomy in the retraction of four upper incisors: A randomized controlled clinical trial. Dent. Med. Probl. 2019, 56, 385–394. [Google Scholar] [CrossRef]
- Al-Horini, O.S.; Baba, F.; Hajeer, M.Y.; Mousa, M.M. The Effect of Elastic and Metallic Ligation Methods on the Unloading Forces for Three Different Types of Nickel-Titanium Archwires Inserted Into Metallic Brackets: An In-vitro Study. Cureus 2022, 14, e31952. [Google Scholar] [CrossRef]
- Alfawal, A.M.H.; Hajeer, M.Y.; Ajaj, M.A.; Hamadah, O.; Brad, B. Evaluation of piezocision and laser-assisted flapless corticotomy in the acceleration of canine retraction: A randomized controlled trial. Head Face Med. 2018, 14, 4. [Google Scholar] [CrossRef]
- Reznikov, N.; Har-Zion, G.; Barkana, I.; Abed, Y.; Redlich, M. Measurement of friction forces between stainless steel wires and “reduced-friction” self-ligating brackets. Am. J. Orthod. Dentofac. Orthop. 2010, 138, 330–338. [Google Scholar] [CrossRef] [PubMed]
- Tidy, D.C. Frictional forces in fixed appliances. Am. J. Orthod. Dentofac. Orthop. 1989, 96, 249–254. [Google Scholar] [CrossRef]
- Kusy, R.P.; Whitley, J.Q. Assessment of second-order clearances between orthodontic archwires and bracket slots via the critical contact angle for binding. Angle Orthod. 1999, 69, 71–80. [Google Scholar] [PubMed]
- Zufall, S.W.; Kennedy, K.C.; Kusy, R.P. Frictional characteristics of composite orthodontic archwires against stainless steel and ceramic brackets in the passive and active configurations. J. Mater. Sci. Mater. Med. 1998, 9, 611–620. [Google Scholar] [CrossRef] [PubMed]
- Alhadlaq, A.; Alkhadra, T.; El-Bialy, T. Anchorage condition during canine retraction using transpalatal arch with continuous and segmented arch mechanics. Angle Orthod. 2016, 86, 380–385. [Google Scholar] [CrossRef] [PubMed]
- Ziegler, P.; Ingervall, B. A clinical study of maxillary canine retraction with a retraction spring and with sliding mechanics. Am. J. Orthod. Dentofac. Orthop. 1989, 95, 99–106. [Google Scholar] [CrossRef]
- Burstone, C.J.; Choy, K. The Biomechanical Foundation of Clinical Orthodontics; Quintessence Publishing Company, Incorporated: Batavia, IL, USA, 2015. [Google Scholar]
- Proffit, W.; Fields, H.; Sarver, D. Biomechanics, mechanics and contemporary orthodontic appliances. In Contemporary Orthodontics, 4th ed.; Proffit, W.R., Fields, H.W., Sarver, D.M., Eds.; Mosby Elsevier: St. Louis, MO, USA, 2007. [Google Scholar]
- Kuhlberg, A.J.; Priebe, D. Testing force systems and biomechanics--measured tooth movements from differential moment closing loops. Angle Orthod. 2003, 73, 270–280. [Google Scholar]
- Ribeiro, G.L.; Jacob, H.B. Understanding the basis of space closure in Orthodontics for a more efficient orthodontic treatment. Dent. Press J. Orthod. 2016, 21, 115–125. [Google Scholar] [CrossRef]
- Nanda, R. Biomechanics and Esthetic Strategies in Clinical Orthodontics; Elsevier Health Sciences: Amsterdam, The Netherlands, 2005. [Google Scholar]
- Makhlouf, M.; Aboul-Ezz, A.; Fayed, M.S.; Hafez, H. Evaluating the Amount of Tooth Movement and Root Resorption during Canine Retraction with Friction versus Frictionless Mechanics Using Cone Beam Computed Tomography. Open Access Maced. J. Med. Sci. 2018, 6, 384–388. [Google Scholar] [CrossRef]
- Higgins, J.P.; Altman, D.G.; Gotzsche, P.C.; Juni, P.; Moher, D.; Oxman, A.D.; Savovic, J.; Schulz, K.F.; Weeks, L.; Sterne, J.A. Cochrane Bias Methods Group; Cochrane Statistical Methods Group. The Cochrane Collaboration’s tool for assessing risk of bias in randomised trials. BMJ 2011, 343, d5928. [Google Scholar] [CrossRef]
- Sterne, J.A.; Hernán, M.A.; Reeves, B.C.; Savović, J.; Berkman, N.D.; Viswanathan, M.; Henry, D.; Altman, D.G.; Ansari, M.T.; Boutron, I. ROBINS-I: A tool for assessing risk of bias in non-randomised studies of interventions. BMJ 2016, 355, i4919. [Google Scholar] [CrossRef] [PubMed]
- Arvind, P.T.R.; Ramasamy, N.; Rengalakshmi, S. Comparative Evaluation of Anchorage Loss with Implant-Aided Retraction and Frictionless Mechanics with Conventional Anchorage in Bimaxillary Protrusion Cases. J. Long Term Eff. Med. Implant. 2021, 31, 21–26. [Google Scholar] [CrossRef]
- Bakhit, D.I.; Dehis, H.M.; Moustafa, Y.A.; El Sharaby, F.A. Evaluation of anchorage loss following anterior segment retraction using friction versus frictionless mechanics: A randomized clinical trial. Future Dent. J. 2022, 8, 21–27. [Google Scholar] [CrossRef]
- Goyal, V.; Singh, G.; Izhar, A.; Singh, R.; Gupta, N. To Evaluate and Compare the Rate of Space Closure and Incisor Retraction between Sliding Mechanics and CNA Mushroom Loop Archwire Using Indirect Anchorage. J. Contemp. Orthod. 2019, 3, 13–18. [Google Scholar]
- Hayashi, K.; Uechi, J.; Murata, M.; Mizoguchi, I. Comparison of maxillary canine retraction with sliding mechanics and a retraction spring: A three-dimensional analysis based on a midpalatal orthodontic implant. Eur. J. Orthod. 2004, 26, 585–589. [Google Scholar] [CrossRef]
- Koyama, I.; Iino, S.; Abe, Y.; Takano-Yamamoto, T.; Miyawaki, S. Differences between sliding mechanics with implant anchorage and straight-pull headgear and intermaxillary elastics in adults with bimaxillary protrusion. Eur. J. Orthod. 2011, 33, 126–131. [Google Scholar] [CrossRef] [PubMed]
- Sardana, R.; Chugh, V.K.; Bhatia, N.K.; Shastri, D.; Moungkhom, P.; Kumar, P.; Chugh, A.; Singh, S. Rate and anchorage loss during en-masse retraction between friction and frictionless mechanics: A randomized clinical trial. Orthod. Craniofac. Res. 2023, 26, 598–607. [Google Scholar] [CrossRef]
- Tawfik, M.G.Y.; Izzat Bakhit, D.; El Sharaby, F.A.; Moustafa, Y.A.; Dehis, H.M. Evaluation of the rate of anterior segment retraction in orthodontic patients with bimaxillary protrusion using friction vs frictionless mechanics: A single-center, single-blind randomized clinical trial. Angle Orthod. 2022, 92, 738–745. [Google Scholar] [CrossRef]
- Ricketts, R. Development of retraction sections. Found. Orthod. Res. Newsl. 1974, 5, 41–44. [Google Scholar]

| Type of occlusion and malocclusion | Permanent occlusion, class II relationship, excessive overjet, maxillary dentoalveolar protrusion, bimaxillary protrusion, severe crowding, anterior open bite, first premolar extraction. |
| Treatment planning | Anterior teeth retraction, incisor retraction, canine retraction, en-masse retraction, moving anterior teeth backward, space closure. |
| Outcomes | Orthodontic tooth movement rate, orthodontic tooth movement amount, orthodontic tooth movement velocity, orthodontic tooth movement speed, orthodontic tooth movement duration, anchorage loss, rotation, inclination, torque, angulation, tipping, root resorption. |
| Interventions | Segmental technique, Segmented technique, sectional, Frictionless Mechanics, T-loop, L-loop, Loop-based technique, Ricketts’s spring, Gjessing retraction arch, Ladanyi spring, Marcotte spring, Reverse Closing Loop, Retraction spring. |
| Authors | Number of Patients/Mean Age/Study Design | The Mechanism of Application/Force Intensity | Outcomes | Follow-Up Period | Extraction Time/Anchorage | Assessment Tool |
|---|---|---|---|---|---|---|
| Canine retraction studies | ||||||
| Ziegler et al., 1989 [17] | 21 (5 male, 16 female). Range: 10 to 27 y, median age: 13 y 6 m Split-mouth Class II malocclusion | Sliding M: on 0.018-inch (0.45 mm) S.S by PCT (Canines secured by ligatures to avoid rotations). Sectional A: Gjessing’s Retraction Spring Force magnitude: SM: 380 g → 200 g–SA: 160 g. The brackets were of the twin type with an 0.018-inch slot. The brackets used on the canines were 3.5 mm wide without angulation or torque. Sliding on 0.018 ss | Canine retraction rate, anchorage loss, tipping and rotation of the canines | Until completion of canine retraction | Immediately before retraction TPA + headgear was worn 10 to 14 h per day | Casts: T1: before movement; T2: after movement. Dental analysis was performed on photographed study models in a standard way. The angulation study was carried out clinically by the method of pin and bar. |
| Hayashi et al., 2004 [29] | 8 (3 male, 5 female). Range: 19 y to 29 y Mean age: 23 y, 2 m Parallel-group: 2 groups Class II malocclusion | Sliding M: 0.018-inch S.S. Bracket: standard edgewise 0.022 × 0.028 Sectional A: Ricketts’s Canine Retraction Spring. Bracket: standard edgewise 0.018 × 0.025. Force magnitude: 1 N | Distal movement, tipping and rotation of canine | 2 months | Osseo-integrated midpalatal implants | Impressions of the maxillary arch each week. A 3D surface-scanning system using a slit laser beam was used to measure the series of dental casts. |
| Alhadlaq et al., 2016 [16] | 20 Parallel group: 2 groups (n = 10) Class II malocclusion | Sliding M: On 0.018 × 0.025-inch S.S. Sectional A: T-loop fabricated from 0.019 × 0.025-inch TMA (RMO) using synergy bracket system (0.022 × 0.025 in) | Ricketts cephalometric analysis (Anchorage loss by U6-PT Vertical) | Until completion of canine retraction | TPA | CRs were obtained at the beginning of the treatment (T0) and immediately after complete canine retraction (T1). |
| Makhlouf et al., 2018 [23] | 10 (3 male, 7 female) Split-mouth Class II malocclusion | Sliding M: coil spring (on 0.016 × 0.022-inch S.S.) (left side) Sectional A: T-loops (0.017 × 0.025 TMA wires) (right side). Force magnitude: 150 g MBT 0.022 | Amount of canine retraction, root resorption | (4 months). | CBCT pre-retraction and post-retraction | |
| Incisor retraction studies | ||||||
| Bakhit et al., 2022 [27] | 40 (40 fe). Mean age: 15.6 y (friction group)/16 y (frictionless group) Bimaxillary protrusion RCT | Sliding M: PCT/on 0.017 × 0.025 S.S. Sectional A: 0.017 × 0.025-inch TMA T-loops. Force magn: SM-SA: 160 g. bracket system: Roth 0.022-inch | Anchorage loss, Torque changes of the incisors, ANB°, and B° change | After incisor retraction was completed and normal overjet obtained | Mini-screws | CBCT pre-retraction and post-complete retraction |
| Tawfik et al., 2022 [32] | 30 (30 fe). Mean age: 18.3 ± 3.7 y. Parallel group: 2 groups (n = 15) Bimaxillary protrusion. RCT | Sliding M: PCT/on 0.017 × 0.025-inch S.S. Sectional A: 0.017 × 0.025-inch TMA T-loops. Force magn: 160 g. bracket system: Roth 0.022-inch | The rate of retraction, anchorage loss | Until the closure of the extraction space and establishment of normal overjet | TADs for indirect anchorage | Study models were scanned using a 3Shape R500 scanner. |
| En-masse retraction studies | ||||||
| Koyama et al., 2011 [30] | 28 (3 ma, 25 fe). Mean age: 24.9 ± 5 y. Parallel-group: 2 groups Bimaxillary protrusion En-masse retraction in group 1. Two-step retraction in group 2. Retrospective study. | Group 1 (Sliding M): PCT/on 0.016 × 0.022 inches of stainless steel. Bracket system: Edgewise 0.018-inch slot Group 2 (Sectional A): straight-pull headgear and intermaxillary elastics Two-step retraction (the canines by sliding by PCT (100 g) then the incisors were closed with vertical loops and intermaxillary elastics. | SNA, SNB, ANB, SN-MP°, SN-U1°, SN-L1°, U1 and U6 position, L1 and L6 position, overjet, and overbite changes | - | Sliding M: implant anchorage Sectional A: straight-pull headgear (200 g/12 h a day) and intermaxillary elastics | CRs analysis |
| Goyal et al., 2019 [28] | 22 2 groups (n = 11) Class II malocclusion | Sliding M: coil spring/0.019 × 0.025 inches of stainless steel. Sectional A: CNA mushroom loop archwire. Force magn: 150 g | The rate of space closure. Anchorage loss. Torque changes | After 6 months of retraction | Indirect anchorage was taken from mini-screws | Lateral cephalograms were taken for each patient after 6 months of retraction. Study models and photographs |
| Arvind et al., 2021 [26] | 40 2 groups (n = 20) Bimaxillary protrusion En-masse anterior retraction Retrospective study. | Sliding M: On 0.019 × 0.025 S.S. archwire with hooks. Sectional A: continuous T-loop fabricated with 17 × 25 TMA | Molar anchorage loss | Sectional A: TPA + inclusion of second molars to the anchor unit. | CRs analysis | |
| Sardana et al., 2023 [31] | 36 (10 ma, 26 fe). Parallel-group: 2 groups (n = 19) Angle’s Class II Division 1 and Class I bimaxillary dentoalveolar protrusion Malocclusion RCT | Sliding M: On 0.019 × 0.025-inch S.S. archwire with a mild curve of Spee. Sectional A: using 0.017 × 0.025-inch (CNA Beta Titanium) mushroom looped continuous archwire. bracket system: MBT 0.022-inch | The rate of en-masse retraction. Anchorage loss | The closure of the extraction spaces and normal overjet establishment | Maxillary second molars were bonded to augment anchorage, and a transpalatal arch was placed for transverse control | Study models and cephalometric |
| Canine Retraction Studies | ||||
|---|---|---|---|---|
| Authors | Rate of Canine Retraction | Tipping * | Rotation | Anchorage Loss & Root Resorption |
| Ziegler et al., 1989 [17] | Sliding M: 1.4 mm/30 days Sectional A: 1.91 mm/30 days | Sliding M: 1.41 ± 1.29°/mm. Sectional A: 0.77 ± 0.82°/mm. Difference: 0.6°. | Sliding M.: 4.04 ± 2.37/mm. Sectional A.: 5.07 ± 1.50/mm. Nonsignificant | The average anchorage loss: Sliding M: 0.4 mm; Sectional A: 0.6 mm Anchorage loss per millimeter of canine retraction: Sliding M: 0.07 mm; Sectional A: 0.09 mm |
| Hayashi et al., 2004 [29] | Sliding M: 3.62 ± 0.19 mm/2 months Sect A: 3.95 ± 0.34 mm/2 months Nonsignificant | Sliding M: 7.94°/2 months. Sectional A: 7.89°/2 months. Nonsignificant | Sliding M: 4.07/2 months. Sectional A: 22.06/2 months. Significant | |
| Alhadlaq et al., 2016 [16] | Anchorage loss: Sliding M: 4.5 ± 3; Sectional A: −0.7 ± 1.4. In Sliding M, the upper first molars moved forward > Sectional A. | |||
| Makhlouf et al., 2018 [23] | Sliding M: 0.775 mm/month. Sectional A: 0.1 mm/month. Significant | Root resorption: Sliding M: 0.05 mm/month. Sectional A: 0.275 mm/month. Nonsignificant | ||
| Incisor retraction studies | ||||
| Authors | Rate of the retraction | Anchorage loss | ||
| Bakhit et al., 2022 [27] | Sliding M: U6 MB = 0.593° L6 = 0.532° Sectional A: U6: 1.095° L6: 0.061° Nonsignificant | |||
| Tawfik et al., 2022 [32] | Sliding M: 0.68 ± 0.18 mm/month. Sectional A: 0.88 ± 0.27 mm/month. Nonsignificant | Sliding M: 0.48 mm/4.8 month. Sectional A: 2.1 mm/4.3 month. significant | ||
| En-masse retraction studies | ||||
| Authors | Rate of en-masse retraction | Torque changes | Anchorage loss | |
| Koyama et al., 2011 [30] | SN-U1°: Sliding M: −10.3 ± 5.8°; Sectional A: −11.1 ± 5.9°: nonsignificant SN-L1°: Sliding M: −6.8 ± 2.1°; Sectional A: −4.6 ± 3.0°: nonsignificant | Upper jaw: Sliding M: 0.1 ± 0.5 mm; Sectional A: 2.1 ± 1.3 mm: significant Lower jaw: Sliding M: 1.3 ± 1.3 mm; Sectional A: 2.5 ± 1.3 mm: significant | ||
| Goyal et al., 2019 [28] | Sliding M: 0.74 mm/month; Sectional A: 0.39 mm/month: significant. | Sliding M: −12.73°; sectional A: −7.27°: significant. | Sliding M: 0.21 mm; Sectional A: 0.18 mm: nonsignificant | |
| Arvind et al., 2021 [26] | Sliding M: 0.95 ± 0.36 mm; Sectional A: 2.44 ± 0.46 mm: significant | |||
| Sardana et al., 2023 [31] | Sliding M: 0.7 mm/month; Sectional A: 0.8 mm/month: nonsignificant | Sliding M: 10.9° ± 4.6°; Sectional A: 11.45° ± 3.9°: nonsignificant | Sliding M: 2.28 ± 238 mm; Sectional A: 1.13 ± 1.42 mm: nonsignificant | |
Disclaimer/Publisher’s Note: The statements, opinions and data contained in all publications are solely those of the individual author(s) and contributor(s) and not of MDPI and/or the editor(s). MDPI and/or the editor(s) disclaim responsibility for any injury to people or property resulting from any ideas, methods, instructions or products referred to in the content. |
© 2023 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Kheshfeh, M.N.; Hajeer, M.Y.; Al Hinnawi, M.F.; Awawdeh, M.A.; Aljhani, A.S.; Alhazmi, N. How Effective Are Non-Frictional Techniques Compared to Sliding Techniques in the Retraction of Upper Anterior Teeth When Using Buccal Fixed-Appliance Therapy? A Systematic Review. J. Clin. Med. 2023, 12, 6757. https://doi.org/10.3390/jcm12216757
Kheshfeh MN, Hajeer MY, Al Hinnawi MF, Awawdeh MA, Aljhani AS, Alhazmi N. How Effective Are Non-Frictional Techniques Compared to Sliding Techniques in the Retraction of Upper Anterior Teeth When Using Buccal Fixed-Appliance Therapy? A Systematic Review. Journal of Clinical Medicine. 2023; 12(21):6757. https://doi.org/10.3390/jcm12216757
Chicago/Turabian StyleKheshfeh, Mohammad Naem, Mohammad Younis Hajeer, Mhd. Firas Al Hinnawi, Mohammed Adel Awawdeh, Ali S. Aljhani, and Nora Alhazmi. 2023. "How Effective Are Non-Frictional Techniques Compared to Sliding Techniques in the Retraction of Upper Anterior Teeth When Using Buccal Fixed-Appliance Therapy? A Systematic Review" Journal of Clinical Medicine 12, no. 21: 6757. https://doi.org/10.3390/jcm12216757
APA StyleKheshfeh, M. N., Hajeer, M. Y., Al Hinnawi, M. F., Awawdeh, M. A., Aljhani, A. S., & Alhazmi, N. (2023). How Effective Are Non-Frictional Techniques Compared to Sliding Techniques in the Retraction of Upper Anterior Teeth When Using Buccal Fixed-Appliance Therapy? A Systematic Review. Journal of Clinical Medicine, 12(21), 6757. https://doi.org/10.3390/jcm12216757