Abstract
Bimaxillary orthognathic surgery is widely used for the correction of dentoskeletal deformities. Surgery sequencing (maxilla or mandible first) remains debated, and guidelines and consensus are lacking. This scoping review summarizes the state of the art and compares the advantages and disadvantages of both approaches. The review was conducted following PRISMA-ScR guidelines. Three electronic databases (PubMed, Scopus, Web of Science) were searched using the PICO protocol and key words in orthognathic surgical sequencing. Four reviewers screened the records independently, and disagreement was resolved by consensus. A total of 23 records met the inclusion criteria. The advantages and disadvantages of the two approaches were compared and assessed for accuracy of reporting. Within the limitations of the present study, available evidence for the intrinsic advantages and the accuracy of the mandible-first sequence supports the choice of this approach in most cases. Nevertheless, each clinical case needs to be evaluated individually, as no dogmatic recommendations can be given for sequencing in bimaxillary orthognathic surgery.
1. Introduction
Since the introduction of internal rigid fixation, it has become the surgeon’s choice to decide which jaw to operate first in bimaxillary surgery for correcting malocclusion and improving facial appearance simultaneously [1,2]. In the past, at the time of wire fixation, the only way to perform bimaxillary surgery was to osteotomize the maxilla first because it was the only jaw that could be properly stabilized so as to be used as a reference point to safely reposition the mandible [1,3]. For this reason, most maxillofacial surgeons were trained to operate following a maxilla-first sequence.
With the introduction of titanium plates and screws, however, operating the mandible first has become a valid alternative, as it can be rigidly fixed and used as a stable reference point to reposition the maxilla. Surgeons can now easily stabilize both jaws effectively regardless of the sequence. Although the mandible-first sequence has attracted increasing interest among orthognathic surgeons, it is not known whether the mandible-first sequence is an alternative to the maxilla-first sequence out of convention or due to its real advantages.
To achieve optimal outcomes, surgical protocols should be closely followed to minimize the risk of complications and improve long-term results. Deciding which sequence to choose on a case-by-case basis in bimaxillary surgery is fundamental for improving the reliability of such a technically complex surgery and for achieving predictable outcomes [1,4,5].
Currently, very few studies summarize or compare the advantages and disadvantages of the two sequences. An extensive review of the topic is beyond the scope of the present article. The aim was to:
- -
- Provide a summary of the available literature on sequencing in bimaxillary surgery;
- -
- Compare the advantages and the disadvantages of both sequences;
- -
- Provide clear indications for both sequences;
- -
- Suggest a systematic study approach to those who intend to review the recent literature on this topic.
2. Materials and Methods
This scoping review was conducted according to PRISMA Extension for Scoping Reviews (PRISMA-Scr) guidelines [6]. This study was registered in the INPLASY platform. A summary of the protocol is provided in Table 1. A team of four reviewers differing in knowledge and experience in orthognathic surgery was recruited. Three electronic databases (PubMed, Scopus, Web of Science) were queried for publications on sequencing in bimaxillary orthognathic surgery published between 1977 and 2023. To do this, each reviewer drafted a list of keywords for the topic and created a search string following the PICO protocol (Table 2). The records were screened in a blind fashion by the four reviewers according to title and abstract. A calibration exercise was performed to ensure consensus among the reviewers. Studies with useful information about orthognathic sequencing were included, whereas studies on other concepts in orthognathics were excluded. After consensus on inclusion and exclusion criteria was reached, the full text of the records was analyzed, and a data charting form was created to identify which variables to extract. Each reviewer independently charted the data and discussed the results. By consensus, Table 3 was created to summarize the extrapolated data. A risk of bias assessment involving patients/measurements was performed using RevMan.

Table 1.
Summary of the study protocol according to the Prisma-ScR guidelines.

Table 2.
Keywords for the research string according to the PICO protocol.

Table 3.
Study Sample.
3. Results
A total of 82 abstracts were retrieved from the three databases (75) and through in-text citations (7). After removal of duplicates, the remaining 42 abstracts were analyzed for relevance: consensus by all four reviewers was reached for 16; 6 were excluded, and 20 were listed as uncertain. The uncertain ones were further discussed: 7 were included in the study, and 13 were excluded. The final pool for this scoping review consisted of 23 records (Figure 1), which were fully read and summarized (Table 3).
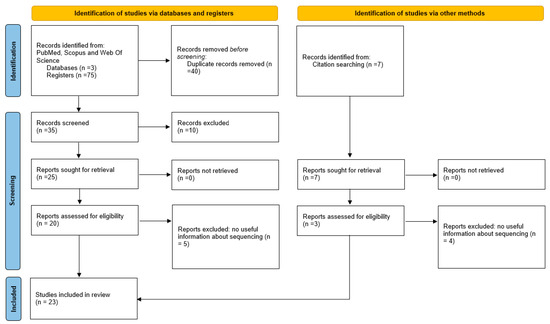
Figure 1.
PRISMA flow diagram of inclusion/exclusion.
A shift in study topics was noted over the years. While initially, there was interest in the advantages and the disadvantages of the mandible-first sequence with regard to surgical planning and surgical execution, the more recent studies investigated surgical accuracy and patient-specific implants (PSI) with both sequences. Most studies underscored the advantages of the mandible-first sequence, while few discussed the advantages of the maxilla-first sequence.
The risk of bias assessment showed an overall high quality of the studies, particularly for blinding and objectiveness of the measurements and completeness of data (Figure 2 and Figure 3). There were small issues with patient randomization, which is intrinsic to orthognathic surgery: treatment cannot be randomized, since it may affect the intervention outcome.
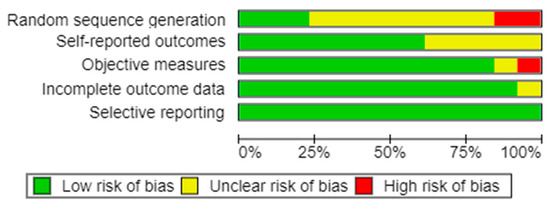
Figure 2.
Risk of bias graph generated with RevMan.
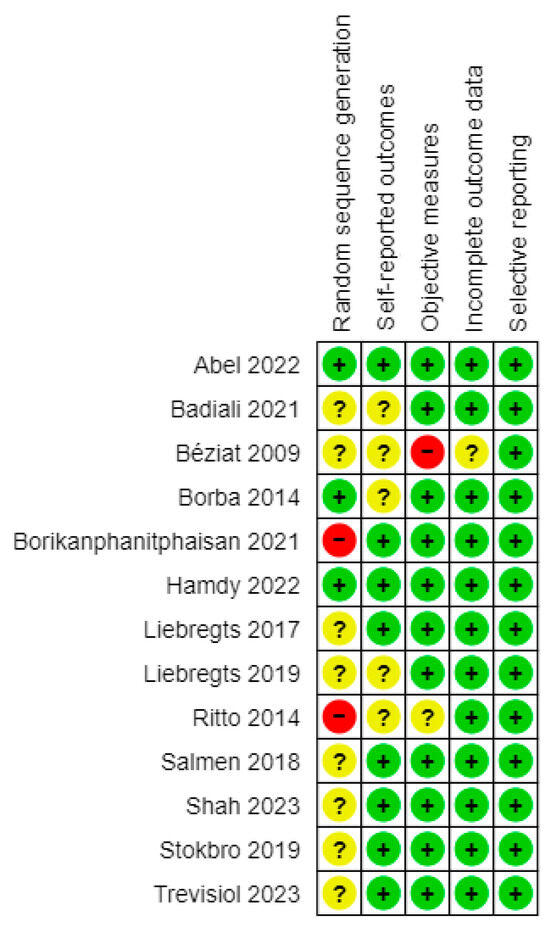
Figure 3.
Risk of bias summary generated with RevMan. Evaluations are given according to RevMan risk of bias assessment criterias (“+” means low risk of bias; “?” means uncclear risk of bias; “–” means high risk of bias).
4. Discussion
Sequencing in bimaxillary orthognathic surgery has attracted intense debate, especially since the introduction of internal rigid fixation, which raised questions about the most appropriate sequence of osteotomies for correcting dentofacial deformities and achieving stable clinical results [2]. Interest was further kindled by Virtual Surgical Planning (VSP), which allows surgeons to plan sequences by their own preferences. Despite the longstanding debate over the advantages and the disadvantages of maxilla- and mandible-first sequences and despite the research conducted so far on the accuracy and surgical results of both approaches, consensus has yet to be reached, and neither the maxilla-first nor mandible-first sequence has been reported to be more advantageous.
This scoping review identified several key-points to consider before adopting the traditional or the inverted sequencing. What is beyond any doubt is that the decision about which jaw to operate on first must be taken at the time of surgical planning [2]. The entity of the defect to be treated (small/large sagittal movements), the direction of rotation of the maxillo-mandibular complex (clockwise or counter-clockwise), the importance of the reliability of the Centric Relation (CR) registration, and the need for maxillary segmentations and splint thickness are widely recognized as being decisive factors in the choice of surgical sequencing.
For example, the maxilla-first sequence is indicated in the clockwise rotation of the jaws, when a single-piece Le Fort I osteotomy is performed or when internal rigid fixation is unfeasible. This sequencing is also preferred in small maxillo-mandibular advancements or when maxillary impaction is required, which allows for the design of an intermediate splint that is thin enough to facilitate intraoperative rigid Maxillo-Mandibular Fixation (MMF) [14].
Choosing the mandible for the first osteotomy seems to be beneficial in the following scenarios. As stated by Posnick et. al., the mandible-first sequence is required when an accurate and reliable preoperative bite registration is not possible [10] and when concurrent Temporomandibular Joint (TMJ) surgery is performed before the orthognathic procedure, as it inevitably changes the position of the condyles [1,3]. Use of the non-operated maxilla as a fixed reference point allows for the accurate repositioning of the mandibular distal segment independently from the centric relation of the condyles during MMF, although the final position of the mandible (at MMF release) is dependent on the proper condyle repositioning in its fossa during plating [2,24].
Operating the mandible first is also advantageous in multi-segmental maxillary osteotomies in which maxillary fragments are oriented according to the mandibular arch; this provides an occlusal guide for achieving accurate and deep intercuspation, without the need for a palatal splint [1]. Perez et al. highlighted that a further advantage of the alternative sequence is that a large maxillo-mandibular advancement and counter-clockwise rotation can be easily performed: dental contacts are maximized, and the intermediate splint is thinner and fits better, resulting in better stability. The mandible-first sequence is to be preferred in maxillary down-grafting; otherwise, the intermediate splint would be too thick, and the TMJ might be displaced during surgery. A cleft lip also constitutes an indication for the mandible-first sequence [1,3,13,15].
Although the mandible-first sequence seems to be a reliable technique, it has several noticeable drawbacks. When a bad split of the mandible cannot be properly managed and the condyle cannot be passively placed in the fossae, the operation may need to be interrupted. Additionally, when a large maxillo-mandibular advancement with clockwise rotation is planned, the intermediate splint in a mandible-first sequence could create a large anterior open bite and make rigid MMF difficult to achieve; in such cases, a maxilla-first sequence is advised. Table 4 presents a summary of the factors to consider when selecting the sequence.

Table 4.
Factors to consider in surgical sequencing.
An additional consideration is the extent to which the choice of a surgical sequence could influence the treatment accuracy. Some authors stated that the two sequences are equally accurate, as both adhere to virtual surgical planning with comparable precision [5,19,21]. In contrast, other authors reported that the conventional sequence achieves more accurate results [12], with differences in specific surgical movements. Stokbro et al. found the mandible-first sequence to be more accurate when counter-clockwise (CCW) rotation was performed, while the conventional sequence apparently produced more accurate results when the rotation was clockwise (CW) [17].
Salmen et al. reported that the conventional sequence produced better esthetic outcomes due to the better accuracy of the vertical position of the upper incisors. In contrast, the mandible-first sequence was more accurate for the Pogonion vertical position [14]. Shah et al. and Abel et al. reported that the mandible-first sequence tended to underachieve maxillo-mandibular advancement in the sagittal direction [22,23]. It should be noted, however, that the discrepancies reported by all studies are clinically not significant, so both sequences may be considered equally accurate.
The development of Patient-Specific Implants (PSIs) with customized cutting guides and plates could represent a further improvement regarding this aspect. According to Badiali et al., PSIs produce clinically accurate results with both sequences [20]. Therefore, the choice of which jaw to operate first in a splintless bimaxillary surgery should follow the same principles as those stated in Table 4.
A final concern relates to the amount of mandibular autorotation required for the creation of the intermediate splint. It is postulated that the greater the amount of mouth opening, the greater the degree of inaccuracy. Recent studies, however, refute this postulate, as no correlation was found between mandibular autorotation and the inaccuracy of the final result [24].
In conclusion, based on the indications and the contraindications for sequencing, the mandible-first sequence appears to be the better choice in most bimaxillary surgery procedures. The surgeon’s personal experience and expertise play a central role in the choice of the surgical sequence, in which each case is evaluated individually, without dogmatic recommendations on which jaw should be operated first.
The present review has several limitations, including its vast and largely conceptual topic and the relatively small sample size. Prospective case-control studies are needed to establish the scientific soundness of the concepts underpinning orthognathic sequencing.
Author Contributions
Conceptualization, L.T., M.B. and A.D.; methodology, M.B., G.L. and R.S.; validation, L.T. and A.D.; formal analysis, L.T., M.B., G.L. and R.S.; investigation, L.T., M.B., G.L. and R.S.; data curation, M.B.; writing—original draft preparation, M.B., G.L. and R.S.; writing—review and editing, L.T., M.B., G.L., R.S. and A.D. All authors have read and agreed to the published version of the manuscript.
Funding
This study was financially supported by the Strasbourg Osteosynthesis Research Group (S.O.R.G. e.V.).
Institutional Review Board Statement
Not applicable.
Informed Consent Statement
Not applicable.
Data Availability Statement
No new data were created or analyzed in this study. Data sharing is not applicable.
Conflicts of Interest
The authors declare no conflict of interest.
References
- Perez, D.; Ellis, E. Sequencing bimaxillary surgery: Mandible first. J. Oral Maxillofac. Surg. 2011, 69, 2217–2224. [Google Scholar] [CrossRef]
- Borba, A.M.; Borges, A.H.; Cé, P.S.; Venturi, B.A.; Naclério-Homem, M.G.; Miloro, M. Mandible-first sequence in bimaxillary orthognathic surgery: A systematic review. Int. J. Oral Maxillofac. Surg. 2016, 45, 472–475. [Google Scholar] [CrossRef] [PubMed]
- Perez, D.; Ellis, E. Implications of Sequencing in Simultaneous Maxillary and Mandibular Orthognathic Surgery. Atlas Oral Maxillofac. Surg. Clin. N. Am. 2016, 24, 45–53. [Google Scholar] [CrossRef]
- Turvey, T. Sequencing of two-jaw surgery: The case for operating on the maxilla first. J. Oral Maxillofac. Surg. 2011, 69, 2225. [Google Scholar] [CrossRef]
- Ritto, F.G.; Ritto, T.G.; Ribeiro, D.P.; Medeiros, P.J.; de Moraes, M. Accuracy of maxillary positioning after standard and inverted orthognathic sequencing. Oral Surg. Oral Med. Oral Pathol. Oral Radiol. 2014, 117, 567–574. [Google Scholar] [CrossRef]
- Tricco, A.C.; Lillie, E.; Zarin, W.; O’Brien, K.K.; Colquhoun, H.; Levac, D.; Moher, D.; Peters, M.D.J.; Horsley, T.; Weeks, L.; et al. PRISMA Extension for Scoping Reviews (PRISMA-ScR): Checklist and Explanation. Ann. Intern. Med. 2018, 169, 467–473. [Google Scholar] [CrossRef]
- Cottrell, D.A.; Wolford, L.M. Altered orthognathic surgical sequencing and a modified approach to model surgery. J. Oral Maxillofac. Surg. 1994, 52, 1010–1020. [Google Scholar] [CrossRef] [PubMed]
- Béziat, J.-L.; Babic, B.; Ferreira, S.; Gleizal, A. Justification de l’ordre mandibule-maxillaire dans l’ostéotomie maxillomandibulaire. Rev. Stomatol. Chir. Maxillofac. 2009, 110, 323–326. [Google Scholar] [CrossRef]
- Borba, A.M.; Ribeiro-Junior, O.; Brozoski, M.A.; Cé, P.S.; Espinosa, M.M.; Deboni, M.C.Z.; Miloro, M.; Naclério-Homem, M.G. Accuracy of perioperative mandibular positions in orthognathic surgery. Int. J. Oral Maxillofac. Surg. 2014, 43, 972–979. [Google Scholar] [CrossRef] [PubMed]
- Posnick, J.C. Mandible-First Analytic Model Planning for Orthognathic Surgery; Elsevier Inc.: Amsterdam, The Netherlands, 2013; pp. 424–440. ISBN 978-145572698-1. [Google Scholar] [CrossRef]
- Iwai, T.; Omura, S.; Honda, K.; Yamashita, Y.; Shibutani, N.; Fujita, K.; Takasu, H.; Murata, S.; Tohnai, I. An accurate bimaxillary repositioning technique using straight locking miniplates for the mandible-first approach in bimaxillary orthognathic surgery. Odontology 2017, 105, 122–126. [Google Scholar] [CrossRef]
- Liebregts, J.; Baan, F.; de Koning, M.; Ongkosuwito, E.; Bergé, S.; Maal, T.; Xi, T. Achievability of 3D planned bimaxillary osteotomies: Maxilla-first versus mandible-first surgery. Sci. Rep. 2017, 7, 9314. [Google Scholar] [CrossRef]
- Perez, D.E.; Liddell, A. Controversies in Orthognathic Surgery. Oral Maxillofac. Surg. Clin. N. Am. 2017, 29, 425–440. [Google Scholar] [CrossRef]
- Salmen, F.S.; de Oliveira, T.F.M.; Gabrielli, M.a.C.; Pereira Filho, V.A.; Real Gabrielli, M.F. Sequencing of bimaxillary surgery in the correction of vertical maxillary excess: Retrospective study. Int. J. Oral Maxillofac. Surg. 2018, 47, 708–714. [Google Scholar] [CrossRef] [PubMed]
- Naran, S.; Steinbacher, D.M.; Taylor, J.A. Current Concepts in Orthognathic Surgery. Plast. Reconstr. Surg. 2018, 141, 925e–936e. [Google Scholar] [CrossRef]
- Liebregts, J.; Baan, F.; van Lierop, P.; de Koning, M.; Bergé, S.; Maal, T.; Xi, T. One-year postoperative skeletal stability of 3D planned bimaxillary osteotomies: Maxilla-first versus mandible-first surgery. Sci. Rep. 2019, 9, 3000. [Google Scholar] [CrossRef]
- Stokbro, K.; Liebregts, J.; Baan, F.; Bell, R.B.; Maal, T.; Thygesen, T.; Xi, T. Does Mandible-First Sequencing Increase Maxillary Surgical Accuracy in Bimaxillary Procedures? J. Oral Maxillofac. Surg. 2019, 77, 1882–1893. [Google Scholar] [CrossRef] [PubMed]
- Parente, E.V.; Antonini, F.; Zanardi, G.; Pagnoncelli, R.M. Tridimensional virtual planning protocol for double-jaw orthognathic surgery with mandible first surgical sequence. Oral Maxillofac. Surg. 2019, 23, 253–262. [Google Scholar] [CrossRef] [PubMed]
- Borikanphanitphaisan, T.; Lin, C.-H.; Chen, Y.-A.; Ko, E.W.-C. Accuracy of Mandible-First versus Maxilla-First Approach and of Thick versus Thin Splints for Skeletal Position after Two-Jaw Orthognathic Surgery. Plast. Reconstr. Surg. 2021, 147, 421–431. [Google Scholar] [CrossRef] [PubMed]
- Badiali, G.; Bevini, M.; Lunari, O.; Lovero, E.; Ruggiero, F.; Bolognesi, F.; Feraboli, L.; Bianchi, A.; Marchetti, C. PSI-Guided Mandible-First Orthognathic Surgery: Maxillo-Mandibular Position Accuracy and Vertical Dimension Adjustability. J. Pers. Med. 2021, 11, 1237. [Google Scholar] [CrossRef] [PubMed]
- Mahmoud, M.H.; Elfaramawi, T.I. Maxillary stability in patients with skeletal class III malocclusion treated by bimaxillary orthognathic surgery: Comparison of mandible-first and maxilla-first approaches in a randomised controlled study. Br. J. Oral Maxillofac. Surg. 2022, 60, 761–766. [Google Scholar] [CrossRef] [PubMed]
- Abel, A.R.; Ho, K.; Neugarten, J.M. What Is the Accuracy of Bimaxillary Orthognathic Surgery Using Occlusally-Based Guides and Patient-Specific Fixation in Both Jaws? A Cohort Study and Discussion of Surgical Techniques. J. Oral Maxillofac. Surg. 2022, 80, 1912–1926. [Google Scholar] [CrossRef] [PubMed]
- Shah, B.; Hallinan, B.; Kramer, A.; Caccamese, J.F. Predictability of the virtual surgical plan for orthognathic surgery with the mandible surgery first sequence. Int. J. Oral Maxillofac. Surg. 2023, 52, 1179–1187. [Google Scholar] [CrossRef] [PubMed]
- Trevisiol, L.; Bersani, M.; Martinez Garza, A.; Alvarado, E.; Arnett, G.W.; D’agostino, A. Accuracy of virtual surgical planning in bimaxillary orthognathic surgery with mandible first sequence: A retrospective study. J. Cranio-Maxillofac. Surg. 2023, 51, 280–287. [Google Scholar] [CrossRef] [PubMed]
Disclaimer/Publisher’s Note: The statements, opinions and data contained in all publications are solely those of the individual author(s) and contributor(s) and not of MDPI and/or the editor(s). MDPI and/or the editor(s) disclaim responsibility for any injury to people or property resulting from any ideas, methods, instructions or products referred to in the content. |
© 2023 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).