New-Onset Atrial Fibrillation in the Critically Ill COVID-19 Patients Hospitalized in the Intensive Care Unit
Abstract
1. Introduction
2. Incidence of New-Onset Atrial Fibrillation in Patients with Severe COVID-19
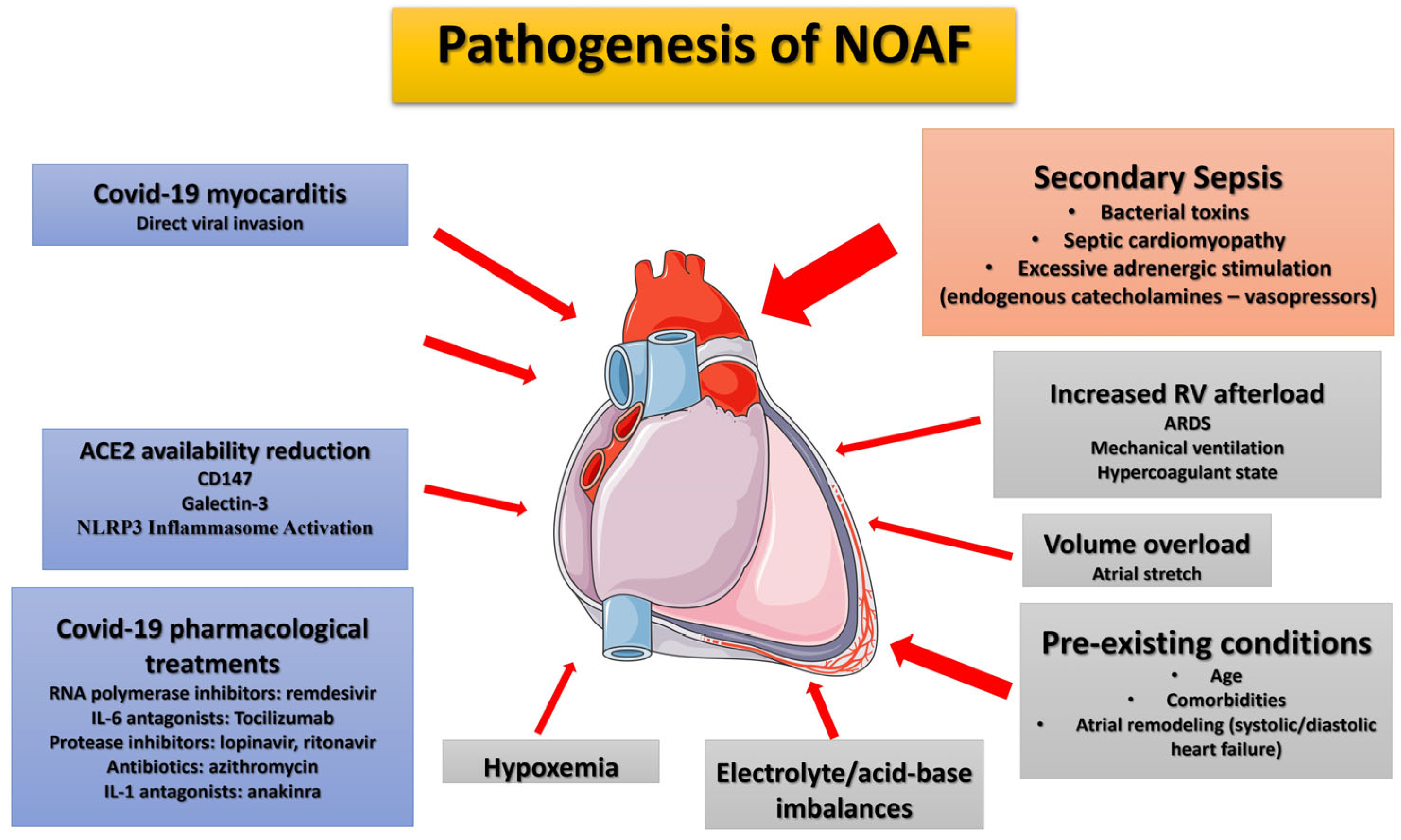
3. Pathophysiological Mechanisms Assumed to Be Involved in the Appearance of NOAF
- (a)
- Reduced availability of angiotensin-converting enzyme (ACE) 2: Atrial ACE2 catabolizes transforming growth factor-β1 (TGF-β1), the principal pro-fibrotic cytokine [101]. This may underlie atrial arrhythmogenesis and potentially increase susceptibility to atrial fibrillation (AF) in COVID-19 patients [102].
- (b)
- CD147 as an adjunctive player: CD147 facilitates SARS-CoV-2 invasion into host cells, including cardiomyocytes, by interacting with the viral spike protein [103,104]. In cardiomyocytes, CD147 strongly induces IL-18, activating matrix metalloproteinases (MMPs), and elevated circulating IL-18 levels are positively correlated with AF development [105]. Moreover, higher plasma levels of MMP-9 found in AF patients suggest that MMP-9 can serve as a marker of atrial remodeling [106]. Increased circulating MMP-9 has also been observed in COVID-19 patients [107]. CD147 also stimulates oxidative stress in cardiomyocytes and promotes negative ionotropic effects [108].
- (c)
- Role of Galectin-3: Galectin-3 plays a role in the progression of atrial fibrosis and is involved in extracellular matrix formation. Elevated galectin-3 levels correlate with advanced AF and worse outcomes [109]. Notably, galectin-3 levels are increased in the serum of COVID-19 patients and correlate with COVID-19 severity [110,111].
- (d)
- NLRP3 Inflammasome Activation: SARS-CoV-2, by binding to ACE2, purinergic receptors, and components of the complement-mediated pathway, stimulates the formation of the NOD-like receptor pyrin domain-containing 3 (NLRP3) inflammasome [112]. A causal link exists between NLRP3 inflammasome activation in atrial cardiomyocytes and the development of AF [85,113,114].
- (e)
- Systemic Immune Cell Over-Activation: SARS-CoV-2 infection is characterized by systemic immune cell over-activation, leading to an imbalance between T-helper-1 and Th2 cells, elevated levels of various cytokines, including IL-1β, IL-2, IL-6, IL-7, interferons, TNF-α, monocyte chemoattractant protein-1, and macrophage inflammatory protein-1A [115,116,117]. At the cardiac level, pro-inflammatory cytokines, particularly IL-6, stimulate vascular smooth muscle proliferation, endothelial cell and platelet activation, and lead to apoptosis or necrosis of myocardial cells, which could mediate intra-atrial repolarization [118].
- (f)
- Sympathetic Nervous System Activation: In viral infections like COVID-19, activation of the sympathetic nervous system [119] leads to increased Ca2+ influx and cardiomyocyte overload. Ca2+ release, along with the subsequent generation of delayed afterdepolarizations (DADs) and action potentials, increases the probability of AF events [120].
4. Outcome of Severely Ill COVID-19 Patients with NOAF
5. Management of Severely Ill COVID-19 Patients with NOAF
6. Conclusions
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Conflicts of Interest
References
- Phua, J.; Weng, L.; Ling, L.; Egi, M.; Lim, C.M.; Divatia, J.V.; Shrestha, B.R.; Arabi, Y.M.; Ng, J.; Gomersall, C.D.; et al. Intensive care management of coronavirus disease 2019 (COVID-19): Challenges and recommendations. Lancet Respir. Med. 2020, 8, 506–517. [Google Scholar] [CrossRef] [PubMed]
- Grasselli, G.; Zangrillo, A.; Zanella, A.; Antonelli, M.; Cabrini, L.; Castelli, A.; Cereda, D.; Coluccello, A.; Foti, G.; Fumagalli, R.; et al. COVID-19 Lombardy ICU Network. Baseline Characteristics and Outcomes of 1591 Patients Infected with SARS-CoV-2 Admitted to ICUs of the Lombardy Region, Italy. JAMA 2020, 323, 1574–1581. [Google Scholar] [CrossRef] [PubMed]
- Cummings, M.J.; Baldwin, M.R.; Abrams, D.; Jacobson, S.D.; Meyer, B.J.; Balough, E.M.; Aaron, J.G.; Claassen, J.; Rabbani, L.E.; Hastie, J.; et al. Epidemiology, clinical course, and outcomes of critically ill adults with COVID-19 in New York City: A prospective cohort study. Lancet 2020, 395, 1763–1770. [Google Scholar] [CrossRef] [PubMed]
- Gawałko, M.; Kapłon-Cieślicka, A.; Hohl, M.; Dobrev, D.; Linz, D. COVID-19 associated atrial fibrillation: Incidence, putative mechanisms and potential clinical implications. Int. J. Cardiol. Heart Vasc. 2020, 30, 100631. [Google Scholar] [CrossRef]
- Wang, Y.; Shu, H.; Liu, H.; Li, X.; Zhou, X.; Zou, X.; Pan, S.; Xu, J.; Xu, D.; Zhao, X.; et al. The peak levels of highly sensitive troponin I predicts in-hospital mortality in COVID-19 patients with cardiac injury: A retrospective study. Eur. Heart J. Acute Cardiovasc. Care 2021, 10, 6–15. [Google Scholar] [CrossRef]
- Tsolaki, V.; Zakynthinos, G.E. Are Patients with COVID-19 Dying of or with Cardiac Injury? Am. J. Respir. Crit. Care Med. 2020, 202, 300–301. [Google Scholar] [CrossRef]
- Siripanthong, B.; Nazarian, S.; Muser, D.; Deo, R.; Santangeli, P.; Khanji, M.Y.; Cooper, L.T., Jr.; Chahal, C.A.A. Recognizing COVID-19-related myocarditis: The possible pathophysiology and proposed guideline for diagnosis and management. Heart Rhythm 2020, 17, 1463–1471. [Google Scholar] [CrossRef]
- Imazio, M.; Klingel, K.; Kindermann, I.; Brucato, A.; De Rosa, F.G.; Adler, Y.; De Ferrari, G.M. COVID-19 pandemic and troponin: Indirect myocardial injury, myocardial inflammation or myocarditis? Heart 2020, 106, 1127–1131. [Google Scholar] [CrossRef]
- Yarmohammadi, H.; Morrow, J.P.; Dizon, J.; Biviano, A.; Ehlert, F.; Saluja, D.; Waase, M.; Elias, P.; Poterucha, T.J.; Berman, J.; et al. Frequency of Atrial Arrhythmia in Hospitalized Patients With COVID-19. Am. J. Cardiol. 2021, 147, 52–57. [Google Scholar] [CrossRef]
- Angeli, F.; Spanevello, A.; De Ponti, R.; Visca, D.; Marazzato, J.; Palmiotto, G.; Feci, D.; Reboldi, G.; Fabbri, L.M.; Verdecchia, P. Electrocardiographic features of patients with COVID-19 pneumonia. Eur. J. Intern. Med. 2020, 78, 101–106. [Google Scholar] [CrossRef]
- Bhatla, A.; Mayer, M.M.; Adusumalli, S.; Hyman, M.C.; Oh, E.; Tierney, A.; Moss, J.; Chahal, A.A.; Anesi, G.; Denduluri, S.; et al. COVID-19 and cardiac arrhythmias. Heart Rhythm 2020, 17, 1439–1444. [Google Scholar] [CrossRef] [PubMed]
- Iacopino, S.; Placentino, F.; Colella, J.; Pesce, F.; Pardeo, A.; Filannino, P.; Artale, P.; Desiro, D.; Sorrenti, P.; Campagna, G.; et al. New-Onset Cardiac Arrhythmias during COVID-19 Hospitalization. Circ. Arrhythmia Electrophysiol. 2020, 13, e009040. [Google Scholar] [CrossRef] [PubMed]
- Colon, C.M.; Barrios, J.G.; Chiles, J.W.; McElwee, S.K.; Russell, D.W.; Maddox, W.R.; Kay, G.N. Atrial Arrhythmias in COVID-19 Patients. JACC Clin. Electrophysiol. 2020, 6, 1189–1190. [Google Scholar] [CrossRef] [PubMed]
- Goyal, P.; Choi, J.J.; Pinheiro, L.C.; Schenck, E.J.; Chen, R.; Jabri, A.; Satlin, M.J.; Campion, T.R., Jr.; Nahid, M.; Ringel, J.B.; et al. Clinical Characteristics of Covid-19 in New York City. N. Engl. J. Med. 2020, 382, 2372–2374. [Google Scholar] [CrossRef] [PubMed]
- Babapoor-Farrokhran, S.; Rasekhi, R.T.; Gill, D.; Babapoor, S.; Amanullah, A. Arrhythmia in COVID-19. SN Compr. Clin. Med. 2020, 2, 1430–1435. [Google Scholar] [CrossRef]
- Vahey, G.M.; Marshall, K.E.; McDonald, E.; Martin, S.W.; Tate, J.E.; Midgley, C.M.; Killerby, M.E.; Kawasaki, B.; Herlihy, R.K.; Alden, N.B.; et al. Symptom Profiles and Progression in Hospitalized and Nonhospitalized Patients with Coronavirus Disease, Colorado, USA, 2020. Emerg. Infect. Dis. 2021, 27, 385–395. [Google Scholar] [CrossRef]
- Bosch, N.A.; Cimini, J.; Walkey, A.J. Atrial Fibrillation in the ICU. Chest 2018, 154, 1424–1434. [Google Scholar] [CrossRef]
- Wetterslev, M.; Haase, N.; Hassager, C.; Belley-Cote, E.P.; McIntyre, W.F.; An, Y.; Shen, J.; Cavalcanti, A.B.; Zampieri, F.G.; Guimaraes, H.P.; et al. New-onset atrial fibrillation in adult critically ill patients: A scoping review. Intensive Care Med. 2019, 45, 928–938. [Google Scholar] [CrossRef]
- Walkey, A.J.; Benjamin, E.J.; Lubitz, S.A. New-onset atrial fibrillation during hospitalization. J. Am. Coll. Cardiol. 2014, 64, 2432–2433. [Google Scholar] [CrossRef]
- Arrigo, M.; Ishihara, S.; Feliot, E.; Rudiger, A.; Deye, N.; Cariou, A.; Guidet, B.; Jaber, S.; Leone, M.; Resche-Rigon, M.; et al. New-onset atrial fibrillation in critically ill patients and its association with mortality: A report from the FROG-ICU study. Int. J. Cardiol. 2018, 266, 95–99. [Google Scholar] [CrossRef]
- Zakynthinos, G.E.; Tsolaki, V.; Karavidas, N.; Vazgiourakis, V.; Dimeas, G.; Mantzarlis, K.; Vavougios, G.; Makris, D. Secondary bacterial infections are a leading factor triggering New Onset Atrial Fibrillation in intubated ICU COVID-19 ARDS patients. J. Infect. Public Health 2022, 15, 766–772. [Google Scholar] [CrossRef] [PubMed]
- Meierhenrich, R.; Steinhilber, E.; Eggermann, C.; Weiss, M.; Voglic, S.; Bögelein, D.; Gauss, A.; Georgieff, M.; Stahl, W. Incidence and prognostic impact of new-onset atrial fibrillation in patients with septic shock: A prospective observational study. Crit. Care 2010, 14, R108. [Google Scholar] [CrossRef] [PubMed]
- Salman, S.; Bajwa, A.; Gajic, O.; Afessa, B. Paroxysmal atrial fibrillation in critically ill patients with sepsis. J. Intensive Care Med. 2008, 23, 178–183. [Google Scholar] [CrossRef] [PubMed]
- Seguin, P.; Signouret, T.; Laviolle, B.; Branger, B.; Mallédant, Y. Incidence and risk factors of atrial fibrillation in a surgical intensive care unit. Crit. Care Med. 2004, 32, 722–726. [Google Scholar] [CrossRef]
- Manolis, A.S.; Manolis, A.A.; Manolis, T.A.; Apostolopoulos, E.J.; Papatheou, D.; Melita, H. COVID-19 infection and cardiac arrhythmias. Trends Cardiovasc. Med. 2020, 30, 451–460. [Google Scholar] [CrossRef]
- Nishiga, M.; Wang, D.W.; Han, Y.; Lewis, D.B.; Wu, J.C. COVID-19 and cardiovascular disease: From basic mechanisms to clinical perspectives. Nat. Rev. Cardiol. 2020, 17, 543–558. [Google Scholar] [CrossRef]
- Liu, K.; Fang, Y.Y.; Deng, Y.; Liu, W.; Wang, M.F.; Ma, J.P.; Xiao, W.; Wang, Y.N.; Zhong, M.H.; Li, C.H.; et al. Clinical characteristics of novel coronavirus cases in tertiary hospitals in Hubei Province. Chin. Med. J. 2020, 133, 1025–1031. [Google Scholar] [CrossRef]
- Kanthasamy, V.; Schilling, R.J. Incidence and Prognostic Impact of New-Onset Atrial Fibrillation in Patients with Severe Covid-19: A Retrospective Cohort Study. J. Atr. Fibrillation 2021, 14, 20200457. [Google Scholar] [CrossRef]
- Kensara, R.; Aljuhani, O.; Korayem, G.B.; Alkofide, H.; Almohareb, S.N.; Alosaimi, Y.S.; Altebainawi, A.F.; Bin Saleh, K.; Andas, N.A.; Harbi, S.A.; et al. Incidence and Clinical Outcomes of New-Onset Atrial Fibrillation in Critically Ill Patients with COVID-19: A Multicenter Cohort Study—New-Onset Atrial Fibrillation and COVID-19. Clin. Appl. Thromb. Hemost. 2023, 29, 10760296231156178. [Google Scholar] [CrossRef]
- Ergün, B.; Ergan, B.; Sözmen, M.K.; Küçük, M.; Yakar, M.N.; Cömert, B.; Gökmen, A.N.; Yaka, E. New-onset atrial fibrillation in critically ill patients with coronavirus disease 2019 (COVID-19). J. Arrhythmia 2021, 37, 1196–1204. [Google Scholar] [CrossRef]
- Romiti, G.F.; Corica, B.; Lip, G.Y.H.; Proietti, M. Prevalence and Impact of Atrial Fibrillation in Hospitalized Patients with COVID-19: A Systematic Review and Meta-Analysis. J. Clin. Med. 2021, 10, 2490. [Google Scholar] [CrossRef] [PubMed]
- Gasperetti, A.; Schiavone, M.; Tondo, C.; Mitacchione, G.; Viecca, M.; Galli, M.; Sarzi-Puttini, P.; Forleo, G.B. QT Interval Monitoring and Drugs Management during COVID-19 Pandemic. Curr. Rev. Clin. Exp. Pharmacol. 2021, 16, 306–317. [Google Scholar] [CrossRef] [PubMed]
- Malin, J.J.; Suárez, I.; Priesner, V.; Fätkenheuer, G.; Rybniker, J. Remdesivir against COVID-19 and Other Viral Diseases. Clin. Microbiol. Rev. 2020, 34, e00162-20. [Google Scholar] [CrossRef] [PubMed]
- Grein, J.; Ohmagari, N.; Shin, D.; Diaz, G.; Asperges, E.; Castagna, A.; Feldt, T.; Green, G.; Green, M.L.; Lescure, F.X.; et al. Compassionate Use of Remdesivir for Patients with Severe Covid-19. N. Engl. J. Med. 2020, 382, 2327–2336. [Google Scholar] [CrossRef]
- Bistrovic, P.; Lucijanic, M. Remdesivir might induce changes in electrocardiogram beyond bradycardia in patients with coronavirus disease 2019—The pilot study. J. Med. Virol. 2021, 93, 5724–5725. [Google Scholar] [CrossRef]
- Benjamin, E.J.; Levy, D.; Vaziri, S.M.; D’Agostino, R.B.; Belanger, A.J.; Wolf, P.A. Independent risk factors for atrial fibrillation in a population-based cohort. The Framingham Heart Study. JAMA 1994, 271, 840–844. [Google Scholar] [CrossRef]
- Roselli, C.; Rienstra, M.; Ellinor, P.T. Genetics of Atrial Fibrillation in 2020: GWAS, Genome Sequencing, Polygenic Risk, and Beyond. Circ. Res. 2020, 127, 21–33. [Google Scholar] [CrossRef]
- Rosenblatt, A.G.; Ayers, C.R.; Rao, A.; Howell, S.J.; Hendren, N.S.; Zadikany, R.H.; Ebinger, J.E.; Daniels, J.D.; Link, M.S.; de Lemos, J.A.; et al. New-Onset Atrial Fibrillation in Patients Hospitalized with COVID-19: Results from the American Heart Association COVID-19 Cardiovascular Registry. Circ. Arrhythmia Electrophysiol. 2022, 15, e010666. [Google Scholar] [CrossRef]
- Gundlund, A.; Olesen, J.B.; Butt, J.H.; Christensen, M.A.; Gislason, G.H.; Torp-Pedersen, C.; Køber, L.; Kümler, T.; Fosbøl, E.L. One-year outcomes in atrial fibrillation presenting during infections: A nationwide registry-based study. Eur. Heart J. 2020, 41, 1112–1119. [Google Scholar] [CrossRef]
- Boos, C.J. Infection and atrial fibrillation: Inflammation begets AF. Eur. Heart J. 2020, 41, 1120–1122. [Google Scholar] [CrossRef]
- Walkey, A.J.; Evans, S.R.; Winter, M.R.; Benjamin, E.J. Practice Patterns and Outcomes of Treatments for Atrial Fibrillation during Sepsis: A Propensity-Matched Cohort Study. Chest 2016, 149, 74–83. [Google Scholar] [CrossRef]
- Klein Klouwenberg, P.M.; Frencken, J.F.; Kuipers, S.; Ong, D.S.; Peelen, L.M.; van Vught, L.A.; Schultz, M.J.; van der Poll, T.; Bonten, M.J.; Cremer, O.L.; et al. Incidence, Predictors, and Outcomes of New-Onset Atrial Fibrillation in Critically Ill Patients with Sepsis. A Cohort Study. Am. J. Respir. Crit. Care Med. 2017, 195, 205–211. [Google Scholar] [CrossRef]
- Artucio, H.; Pereira, M. Cardiac arrhythmias in critically ill patients: Epidemiologic study. Crit. Care Med. 1990, 18, 1383–1388. [Google Scholar] [CrossRef]
- Tralhão, A.; Póvoa, P. Cardiovascular Events After Community-Acquired Pneumonia: A Global Perspective with Systematic Review and Meta-Analysis of Observational Studies. J. Clin. Med. 2020, 9, 414. [Google Scholar] [CrossRef] [PubMed]
- Corica, B.; Tartaglia, F.; Oliva, A.; Raparelli, V.; Cangemi, R.; Basili, S.; Lip, G.Y.H.; Proietti, M.; Romiti, G.F. Prevalence of new-onset atrial fibrillation in hospitalized patients with community-acquired pneumonia: A systematic review and meta-analysis. Intern. Emerg. Med. 2023, 18, 127–135. [Google Scholar] [CrossRef] [PubMed]
- Søgaard, M.; Skjøth, F.; Nielsen, P.B.; Smit, J.; Dalager-Pedersen, M.; Larsen, T.B.; Lip, G.Y.H. Thromboembolic Risk in Patients with Pneumonia and New-Onset Atrial Fibrillation Not Receiving Anticoagulation Therapy. JAMA Netw. Open 2022, 5, e2213945. [Google Scholar] [CrossRef] [PubMed]
- Kochi, A.N.; Tagliari, A.P.; Forleo, G.B.; Fassini, G.M.; Tondo, C. Cardiac and arrhythmic complications in patients with COVID-19. J. Cardiovasc. Electrophysiol. 2020, 31, 1003–1008. [Google Scholar] [CrossRef]
- Helms, J.; Combes, A.; Aissaoui, N. Cardiac injury in COVID-19. Intensive Care Med. 2022, 48, 111–113. [Google Scholar] [CrossRef]
- Zhou, F.; Yu, T.; Du, R.; Fan, G.; Liu, Y.; Liu, Z.; Xiang, J.; Wang, Y.; Song, B.; Gu, X.; et al. Clinical course and risk factors for mortality of adult inpatients with COVID-19 in Wuhan, China: A retrospective cohort study. Lancet 2020, 395, 1054–1062. [Google Scholar] [CrossRef]
- Chen, C.; Zhou, Y.; Wang, D.W. SARS-CoV-2: A potential novel etiology of fulminant myocarditis. Herz 2020, 45, 230–232. [Google Scholar] [CrossRef]
- Yang, X.; Yu, Y.; Xu, J.; Shu, H.; Xia, J.; Liu, H.; Wu, Y.; Zhang, L.; Yu, Z.; Fang, M.; et al. Clinical course and outcomes of critically ill patients with SARS-CoV-2 pneumonia in Wuhan, China: A single-centered, retrospective, observational study. Lancet Respir. Med. 2020, 8, 475–481. [Google Scholar] [CrossRef] [PubMed]
- Tian, S.; Xiong, Y.; Liu, H.; Niu, L.; Guo, J.; Liao, M.; Xiao, S.Y. Pathological study of the 2019 novel coronavirus disease (COVID-19) through postmortem core biopsies. Mod. Pathol. 2020, 33, 1007–1014. [Google Scholar] [CrossRef] [PubMed]
- D’Alto, M.; Marra, A.M.; Severino, S.; Salzano, A.; Romeo, E.; De Rosa, R.; Stagnaro, F.M.; Pagnano, G.; Verde, R.; Murino, P.; et al. Right ventricular-arterial uncoupling independently predicts survival in COVID-19 ARDS. Crit. Care 2020, 24, 670. [Google Scholar] [CrossRef]
- Bagate, F.; Masi, P.; d’Humières, T.; Al-Assaad, L.; Chakra, L.A.; Razazi, K.; de Prost, N.; Carteaux, G.; Derumeaux, G.; Mekontso Dessap, A. Advanced echocardiographic phenotyping of critically ill patients with coronavirus-19 sepsis: A prospective cohort study. J. Intensive Care 2021, 9, 12. [Google Scholar] [CrossRef] [PubMed]
- van den Heuvel, F.M.A.; Vos, J.L.; Koop, Y.; van Dijk, A.P.J.; Duijnhouwer, A.L.; de Mast, Q.; van de Veerdonk, F.L.; Bosch, F.; Kok, B.; Netea, M.G.; et al. Cardiac function in relation to myocardial injury in hospitalised patients with COVID-19. Neth. Heart J. 2020, 28, 410–417. [Google Scholar] [CrossRef]
- Bieber, S.; Kraechan, A.; Hellmuth, J.C.; Muenchhoff, M.; Scherer, C.; Schroeder, I.; Irlbeck, M.; Kaeaeb, S.; Massberg, S.; Hausleiter, J.; et al. Left and right ventricular dysfunction in patients with COVID-19-associated myocardial injury. Infection 2021, 49, 491–500. [Google Scholar] [CrossRef]
- Huang, S.; Vignon, P.; Mekontso-Dessap, A.; Tran, S.; Prat, G.; Chew, M.; Balik, M.; Sanfilippo, F.; Banauch, G.; Clau-Terre, F.; et al. Echocardiography findings in COVID-19 patients admitted to intensive care units: A multi-national observational study (the ECHO-COVID study). Intensive Care Med. 2022, 48, 667–678. [Google Scholar] [CrossRef]
- Janus, S.E.; Hajjari, J.; Karnib, M.; Tashtish, N.; Al-Kindi, S.G.; Hoit, B.D. Prognostic Value of Left Ventricular Global Longitudinal Strain in COVID-19. Am. J. Cardiol. 2020, 131, 134–136. [Google Scholar] [CrossRef]
- Karagodin, I.; Carvalho Singulane, C.; Woodward, G.M.; Xie, M.; Tucay, E.S.; Tude Rodrigues, A.C.; Vasquez-Ortiz, Z.Y.; Alizadehasl, A.; Monaghan, M.J.; Ordonez Salazar, B.A.; et al. Echocardiographic Correlates of In-Hospital Death in Patients with Acute COVID-19 Infection: The World Alliance Societies of Echocardiography (WASE-COVID) Study. J. Am. Soc. Echocardiogr. 2021, 34, 819–830. [Google Scholar] [CrossRef]
- Cheng, M.P.; Cau, A.; Lee, T.C.; Brodie, D.; Slutsky, A.; Marshall, J.; Murthy, S.; Lee, T.; Singer, J.; Demir, K.K.; et al. Acute Cardiac Injury in Coronavirus Disease 2019 and Other Viral Infections—A Systematic Review and Meta-Analysis. Crit. Care Med. 2021, 49, 1558–1566. [Google Scholar] [CrossRef]
- Bleakley, C.; Singh, S.; Garfield, B.; Morosin, M.; Surkova, E.; Mandalia, M.S.; Dias, B.; Androulakis, E.; Price, L.C.; McCabe, C.; et al. Right ventricular dysfunction in critically ill COVID-19 ARDS. Int. J. Cardiol. 2021, 327, 251–258. [Google Scholar] [CrossRef] [PubMed]
- McCall, P.J.; Willder, J.M.; Stanley, B.L.; Messow, C.M.; Allan, J.; Gemmell, L.; Puxty, A.; Strachan, D.; Berry, C.; Shelley, B.G.; et al. Right ventricular dysfunction in patients with COVID-19 pneumonitis whose lungs are mechanically ventilated: A multicentre prospective cohort study. Anaesthesia 2022, 77, 772–784. [Google Scholar] [CrossRef] [PubMed]
- Corica, B.; Marra, A.M.; Basili, S.; Cangemi, R.; Cittadini, A.; Proietti, M.; Romiti, G.F. Prevalence of right ventricular dysfunction and impact on all-cause death in hospitalized patients with COVID-19: A systematic review and meta-analysis. Sci. Rep. 2021, 11, 17774. [Google Scholar] [CrossRef] [PubMed]
- Evrard, B.; Goudelin, M.; Giraudeau, B.; François, B.; Vignon, P. Right ventricular failure is strongly associated with mortality in patients with moderate-to-severe COVID-19-related ARDS and appears related to respiratory worsening. Intensive Care Med. 2022, 48, 765–767. [Google Scholar] [CrossRef]
- Karagodin, I.; Singulane, C.C.; Descamps, T.; Woodward, G.M.; Xie, M.; Tucay, E.S.; Sarwar, R.; Vasquez-Ortiz, Z.Y.; Alizadehasl, A.; Monaghan, M.J.; et al. Ventricular Changes in Patients with Acute COVID-19 Infection: Follow-up of the World Alliance Societies of Echocardiography (WASE-COVID) Study. J. Am. Soc. Echocardiogr. 2022, 35, 295–304. [Google Scholar] [CrossRef]
- Bursi, F.; Santangelo, G.; Sansalone, D.; Valli, F.; Vella, A.M.; Toriello, F.; Barbieri, A.; Carugo, S. Prognostic utility of quantitative offline 2D-echocardiography in hospitalized patients with COVID-19 disease. Echocardiography 2020, 37, 2029–2039. [Google Scholar] [CrossRef]
- Li, Y.; Li, H.; Zhu, S.; Xie, Y.; Wang, B.; He, L.; Zhang, D.; Zhang, Y.; Yuan, H.; Wu, C.; et al. Prognostic Value of Right Ventricular Longitudinal Strain in Patients With COVID-19. JACC Cardiovasc. Imaging 2020, 13, 2287–2299. [Google Scholar] [CrossRef]
- Slobod, D.; Assanangkornchai, N.; Alhazza, M.; Mettasittigorn, P.; Magder, S. Right Ventricular Loading by Lung Inflation during Controlled Mechanical Ventilation. Am. J. Respir. Crit. Care Med. 2022, 205, 1311–1319. [Google Scholar] [CrossRef]
- Schmitt, J.M.; Vieillard-Baron, A.; Augarde, R.; Prin, S.; Page, B.; Jardin, F. Positive end-expiratory pressure titration in acute respiratory distress syndrome patients: Impact on right ventricular outflow impedance evaluated by pulmonary artery Doppler flow velocity measurements. Crit. Care Med. 2001, 29, 1154–1158. [Google Scholar] [CrossRef]
- Protti, A.; Santini, A.; Pennati, F.; Chiurazzi, C.; Cressoni, M.; Ferrari, M.; Iapichino, G.E.; Carenzo, L.; Lanza, E.; Picardo, G. Lung Response to a Higher Positive End-Expiratory Pressure in Mechanically Ventilated Patients with COVID-19. Chest 2022, 161, 979–988. [Google Scholar] [CrossRef]
- Tsolaki, V.; Zakynthinos, G.E.; Mantzarlis, K.; Vazgiourakis, V.; Makris, D. Pathophysiology of COVID-19-associated acute respiratory distress syndrome. Lancet Respir. Med. 2021, 9, e2. [Google Scholar] [CrossRef] [PubMed]
- Tsolaki, V.; Zakynthinos, G.E.; Papanikolaou, J.; Karavidas, N.; Vazgiourakis, V.; Papadonta, M.E.; Zygoulis, P.; Pantazopoulos, I.; Makris, D.; Zakynthinos, E. Positive End-Expiratory Pressure Deescalation in COVID-19-induced Acute Respiratory Distress Syndrome Unloads the Right Ventricle, Improving Hemodynamics and Oxygenation. Am. J. Respir. Crit. Care Med. 2023, 208, 205–208. [Google Scholar] [CrossRef]
- Kawakami, R.; Sakamoto, A.; Kawai, K.; Gianatti, A.; Pellegrini, D.; Nasr, A.; Kutys, B.; Guo, L.; Cornelissen, A.; Mori, M.; et al. Pathological Evidence for SARS-CoV-2 as a Cause of Myocarditis: JACC Review Topic of the Week. J. Am. Coll. Cardiol. 2021, 77, 314–325. [Google Scholar] [CrossRef] [PubMed]
- Kim, J.S.; Kim, M.; Kim, Y.J.; Ryoo, S.M.; Sohn, C.H.; Ahn, S.; Kim, W.Y. Troponin Testing for Assessing Sepsis-Induced Myocardial Dysfunction in Patients with Septic Shock. J. Clin. Med. 2019, 8, 239. [Google Scholar] [CrossRef] [PubMed]
- Wu, A.H. Increased troponin in patients with sepsis and septic shock: Myocardial necrosis or reversible myocardial depression? Intensive Care Med. 2001, 27, 959–961. [Google Scholar] [CrossRef] [PubMed]
- Jeong, H.S.; Lee, T.H.; Bang, C.H.; Kim, J.H.; Hong, S.J. Risk factors and outcomes of sepsis-induced myocardial dysfunction and stress-induced cardiomyopathy in sepsis or septic shock: A comparative retrospective study. Medicine 2018, 97, e0263. [Google Scholar] [CrossRef] [PubMed]
- Vieillard-Baron, A.; Caille, V.; Charron, C.; Belliard, G.; Page, B.; Jardin, F. Actual incidence of global left ventricular hypokinesia in adult septic shock. Crit. Care Med. 2008, 36, 1701–1706. [Google Scholar] [CrossRef]
- Spathoulas, K.; Tsolaki, V.; Zakynthinos, G.E.; Karelas, D.; Makris, D.; Zakynthinos, E.; Papanikolaou, J. The Role of Left Ventricular Ejection Fraction and Left Ventricular Outflow Tract Velocity-Time Integral in Assessing Cardiovascular Impairment in Septic Shock. J. Pers. Med. 2022, 12, 1786. [Google Scholar] [CrossRef]
- Seguin, P.; Laviolle, B.; Maurice, A.; Leclercq, C.; Mallédant, Y. Atrial fibrillation in trauma patients requiring intensive care. Intensive Care Med. 2006, 32, 398–404. [Google Scholar] [CrossRef]
- Walkey, A.J.; Wiener, R.S.; Ghobrial, J.M.; Curtis, L.H.; Benjamin, E.J. Incident stroke and mortality associated with new-onset atrial fibrillation in patients hospitalized with severe sepsis. JAMA 2011, 306, 2248–2254. [Google Scholar] [CrossRef]
- Walkey, A.J.; Greiner, M.A.; Heckbert, S.R.; Jensen, P.N.; Piccini, J.P.; Sinner, M.F.; Curtis, L.H.; Benjamin, E.J. Atrial fibrillation among Medicare beneficiaries hospitalized with sepsis: Incidence and risk factors. Am. Heart J. 2013, 165, 949–955.e3. [Google Scholar] [CrossRef]
- Vieillard-Baron, A.; Boyd, J. Non-antiarrhythmic interventions in new onset and paroxysmal sepsis-related atrial fibrillation. Intensive Care Med. 2018, 44, 94–97. [Google Scholar] [CrossRef]
- Schotten, U.; Verheule, S.; Kirchhof, P.; Goette, A. Pathophysiological mechanisms of atrial fibrillation: A translational appraisal. Physiol. Rev. 2011, 91, 265–325. [Google Scholar] [CrossRef] [PubMed]
- Seemann, A.; Boissier, F.; Razazi, K.; Carteaux, G.; de Prost, N.; Brun-Buisson, C.; Mekontso Dessap, A. New-onset supraventricular arrhythmia during septic shock: Prevalence, risk factors and prognosis. Ann. Intensive Care 2015, 5, 27. [Google Scholar] [CrossRef]
- Yao, C.; Veleva, T.; Scott, L., Jr.; Cao, S.; Li, L.; Chen, G.; Jeyabal, P.; Pan, X.; Alsina, K.M.; Abu-Taha, I.; et al. Enhanced Cardiomyocyte NLRP3 Inflammasome Signaling Promotes Atrial Fibrillation. Circulation 2018, 138, 2227–2242. [Google Scholar] [CrossRef]
- Sirish, P.; Li, N.; Timofeyev, V.; Zhang, X.D.; Wang, L.; Yang, J.; Lee, K.S.; Bettaieb, A.; Ma, S.M.; Lee, J.H.; et al. Molecular Mechanisms and New Treatment Paradigm for Atrial Fibrillation. Circ. Arrhythmia Electrophysiol. 2016, 9, e003721. [Google Scholar] [CrossRef] [PubMed]
- Donniacuo, M.; De Angelis, A.; Rafaniello, C.; Cianflone, E.; Paolisso, P.; Torella, D.; Sibilio, G.; Paolisso, G.; Castaldo, G.; Urbanek, K.; et al. COVID-19 and atrial fibrillation: Intercepting lines. Front. Cardiovasc. Med. 2023, 10, 1093053. [Google Scholar] [CrossRef] [PubMed]
- Libby, P.; Lüscher, T. COVID-19 is, in the end, an endothelial disease. Eur. Heart J. 2020, 41, 3038–3044. [Google Scholar] [CrossRef]
- Manjili, R.H.; Zarei, M.; Habibi, M.; Manjili, M.H. COVID-19 as an Acute Inflammatory Disease. J. Immunol. 2020, 205, 12–19. [Google Scholar] [CrossRef]
- Salama, C.; Han, J.; Yau, L.; Reiss, W.G.; Kramer, B.; Neidhart, J.D.; Criner, G.J.; Kaplan-Lewis, E.; Baden, R.; Pandit, L.; et al. Tocilizumab in Patients Hospitalized with Covid-19 Pneumonia. N. Engl. J. Med. 2021, 384, 20–30. [Google Scholar] [CrossRef]
- Huang, Q.; Wu, X.; Zheng, X.; Luo, S.; Xu, S.; Weng, J. Targeting inflammation and cytokine storm in COVID-19. Pharmacol. Res. 2020, 159, 105051. [Google Scholar] [CrossRef] [PubMed]
- Gerotziafas, G.T.; Catalano, M.; Colgan, M.P.; Pecsvarady, Z.; Wautrecht, J.C.; Fazeli, B.; Olinic, D.M.; Farkas, K.; Elalamy, I.; Falanga, A. Guidance for the Management of Patients with Vascular Disease or Cardiovascular Risk Factors and COVID-19: Position Paper from VAS-European Independent Foundation in Angiology/Vascular Medicine. Thromb. Haemost. 2020, 120, 1597–1628. [Google Scholar] [CrossRef] [PubMed]
- Gencer, S.; Lacy, M.; Atzler, D.; van der Vorst, E.P.C.; Döring, Y.; Weber, C. Immunoinflammatory, Thrombohaemostatic, and Cardiovascular Mechanisms in COVID-19. Thromb. Haemost. 2020, 120, 1629–1641. [Google Scholar] [CrossRef]
- Bikdeli, B.; Madhavan, M.V.; Gupta, A.; Jimenez, D.; Burton, J.R.; Der Nigoghossian, C.; Chuich, T.; Nouri, S.N.; Dreyfus, I.; Driggin, E.; et al. Pharmacological Agents Targeting Thromboinflammation in COVID-19: Review and Implications for Future Research. Thromb. Haemost. 2020, 120, 1004–1024. [Google Scholar] [CrossRef] [PubMed]
- Zylla, M.M.; Merle, U.; Vey, J.A.; Korosoglou, G.; Hofmann, E.; Müller, M.; Herth, F.; Schmidt, W.; Blessing, E.; Göggelmann, C.; et al. Predictors and Prognostic Implications of Cardiac Arrhythmias in Patients Hospitalized for COVID-19. J. Clin. Med. 2021, 10, 133. [Google Scholar] [CrossRef] [PubMed]
- Huang, C.; Wang, Y.; Li, X.; Ren, L.; Zhao, J.; Hu, Y.; Zhang, L.; Fan, G.; Xu, J.; Gu, X.; et al. Clinical features of patients infected with 2019 novel coronavirus in Wuhan, China. Lancet 2020, 395, 497–506. [Google Scholar] [CrossRef] [PubMed]
- Wong, C.K.; Lam, C.W.; Wu, A.K.; Ip, W.K.; Lee, N.L.; Chan, I.H.; Lit, L.C.; Hui, D.S.; Chan, M.H.; Chung, S.S.; et al. Plasma inflammatory cytokines and chemokines in severe acute respiratory syndrome. Clin. Exp. Immunol. 2004, 136, 95–103. [Google Scholar] [CrossRef]
- Zeng, Z.; Yu, H.; Chen, H.; Qi, W.; Chen, L.; Chen, G.; Yan, W.; Chen, T.; Ning, Q.; Han, M.; et al. Longitudinal changes of inflammatory parameters and their correlation with disease severity and outcomes in patients with COVID-19 from Wuhan, China. Crit. Care 2020, 24, 525. [Google Scholar] [CrossRef]
- Buetti, N.; Ruckly, S.; de Montmollin, E.; Reignier, J.; Terzi, N.; Cohen, Y.; Siami, S.; Dupuis, C.; Timsit, J.F. COVID-19 increased the risk of ICU-acquired bloodstream infections: A case-cohort study from the multicentric OUTCOMEREA network. Intensive Care Med. 2021, 47, 180–187. [Google Scholar] [CrossRef]
- Rouzé, A.; Martin-Loeches, I.; Povoa, P.; Makris, D.; Artigas, A.; Bouchereau, M.; Lambiotte, F.; Metzelard, M.; Cuchet, P.; Boulle Geronimi, C.; et al. Relationship between SARS-CoV-2 infection and the incidence of ventilator-associated lower respiratory tract infections: A European multicenter cohort study. Intensive Care Med. 2021, 47, 188–198. [Google Scholar] [CrossRef]
- Goudis, C.A.; Kallergis, E.M.; Vardas, P.E. Extracellular matrix alterations in the atria: Insights into the mechanisms and perpetuation of atrial fibrillation. Europace 2012, 14, 623–630. [Google Scholar] [CrossRef] [PubMed]
- Rodrigues, R.; Costa de Oliveira, S. The Impact of Angiotensin-Converting Enzyme 2 (ACE2) Expression Levels in Patients with Comorbidities on COVID-19 Severity: A Comprehensive Review. Microorganisms 2021, 9, 1692. [Google Scholar] [CrossRef] [PubMed]
- Behl, T.; Kaur, I.; Aleya, L.; Sehgal, A.; Singh, S.; Sharma, N.; Bhatia, S.; Al-Harrasi, A.; Bungau, S. CD147-spike protein interaction in COVID-19: Get the ball rolling with a novel receptor and therapeutic target. Sci. Total Environ. 2022, 808, 152072. [Google Scholar] [CrossRef]
- Wang, K.; Chen, W.; Zhang, Z.; Deng, Y.; Lian, J.Q.; Du, P.; Wei, D.; Zhang, Y.; Sun, X.X.; Gong, L.; et al. CD147-spike protein is a novel route for SARS-CoV-2 infection to host cells. Signal Transduct. Target. Ther. 2020, 5, 283. [Google Scholar] [CrossRef] [PubMed]
- Pituch-Noworolska, A.M. NK cells in SARS-CoV-2 infection. Cent. Eur. J. Immunol. 2022, 47, 95–101. [Google Scholar] [CrossRef] [PubMed]
- Li, X.; Guo, X.; Chang, Y.; Zhang, N.; Sun, Y. Analysis of alterations of serum inflammatory cytokines and fibrosis makers in patients with essential hypertension and left ventricular hypertrophy and the risk factors. Am. J. Transl. Res. 2022, 14, 4097–4103. [Google Scholar] [PubMed]
- Ueland, T.; Holter, J.C.; Holten, A.R.; Müller, K.E.; Lind, A.; Bekken, G.K.; Dudman, S.; Aukrust, P.; Dyrhol-Riise, A.M.; Heggelund, L. Distinct and early increase in circulating MMP-9 in COVID-19 patients with respiratory failure. J. Infect. 2020, 81, e41–e43. [Google Scholar] [CrossRef]
- Peng, X.; Wang, Y.; Xi, X.; Jia, Y.; Tian, J.; Yu, B.; Tian, J. Promising Therapy for Heart Failure in Patients with Severe COVID-19: Calming the Cytokine Storm. Cardiovasc. Drugs Ther. 2021, 35, 231–247. [Google Scholar] [CrossRef]
- Clementy, N.; Piver, E.; Bisson, A.; Andre, C.; Bernard, A.; Pierre, B.; Fauchier, L.; Babuty, D. Galectin-3 in Atrial Fibrillation: Mechanisms and Therapeutic Implications. Int. J. Mol. Sci. 2018, 19, 976. [Google Scholar] [CrossRef]
- Cannavo, A.; Liccardo, D.; Gelzo, M.; Amato, F.; Gentile, I.; Pinchera, B.; Femminella, G.D.; Parrella, R.; DE Rosa, A.; Gambino, G.; et al. Serum galectin-3 and aldosterone: Potential biomarkers of cardiac complications in patients with COVID-19. Minerva Endocrinol. 2022, 47, 270–278. [Google Scholar] [CrossRef]
- Cervantes-Alvarez, E.; la Rosa, N.L.; la Mora, M.S.; Valdez-Sandoval, P.; Palacios-Jimenez, M.; Rodriguez-Alvarez, F.; Vera-Maldonado, B.I.; Aguirre-Aguilar, E.; Escobar-Valderrama, J.M.; Alanis-Mendizabal, J.; et al. Galectin-3 as a potential prognostic biomarker of severe COVID-19 in SARS-CoV-2 infected patients. Sci. Rep. 2022, 12, 1856. [Google Scholar] [CrossRef] [PubMed]
- Che Mohd Nassir, C.M.N.; Zolkefley, M.K.I.; Ramli, M.D.; Norman, H.H.; Abdul Hamid, H.; Mustapha, M. Neuroinflammation and COVID-19 Ischemic Stroke Recovery-Evolving Evidence for the Mediating Roles of the ACE2/Angiotensin-(1-7)/Mas Receptor Axis and NLRP3 Inflammasome. Int. J. Mol. Sci. 2022, 23, 3085. [Google Scholar] [CrossRef] [PubMed]
- Young, L.J.; Antwi-Boasiako, S.; Ferrall, J.; Wold, L.E.; Mohler, P.J.; El Refaey, M. Genetic and non-genetic risk factors associated with atrial fibrillation. Life Sci. 2022, 299, 120529. [Google Scholar] [CrossRef] [PubMed]
- Saljic, A.; Heijman, J.; Dobrev, D. Emerging Antiarrhythmic Drugs for Atrial Fibrillation. Int. J. Mol. Sci. 2022, 23, 4096. [Google Scholar] [CrossRef] [PubMed]
- Farahani, M.; Niknam, Z.; Mohammadi Amirabad, L.; Amiri-Dashatan, N.; Koushki, M.; Nemati, M.; Danesh Pouya, F.; Rezaei-Tavirani, M.; Rasmi, Y.; Tayebi, L. Molecular pathways involved in COVID-19 and potential pathway-based therapeutic targets. Biomed. Pharmacother. 2022, 145, 112420. [Google Scholar] [CrossRef]
- Aleebrahim-Dehkordi, E.; Molavi, B.; Mokhtari, M.; Deravi, N.; Fathi, M.; Fazel, T.; Mohebalizadeh, M.; Koochaki, P.; Shobeiri, P.; Hasanpour-Dehkordi, A. T helper type (Th1/Th2) responses to SARS-CoV-2 and influenza A (H1N1) virus: From cytokines produced to immune responses. Transpl. Immunol. 2022, 70, 101495. [Google Scholar] [CrossRef]
- Mazzoni, A.; Salvati, L.; Maggi, L.; Annunziato, F.; Cosmi, L. Hallmarks of immune response in COVID-19: Exploring dysregulation and exhaustion. Semin. Immunol. 2021, 55, 101508. [Google Scholar] [CrossRef]
- Li, S.; Wang, J.; Yan, Y.; Zhang, Z.; Gong, W.; Nie, S. Clinical Characterization and Possible Pathological Mechanism of Acute Myocardial Injury in COVID-19. Front. Cardiovasc. Med. 2022, 9, 862571. [Google Scholar] [CrossRef]
- Fischer, L.; Barop, H.; Ludin, S.M.; Schaible, H.G. Regulation of acute reflectory hyperinflammation in viral and other diseases by means of stellate ganglion block. A conceptual view with a focus on Covid-19. Auton. Neurosci. Basic Clin. 2022, 237, 102903. [Google Scholar] [CrossRef]
- Bers, D.M. Cardiac excitation-contraction coupling. Nature 2002, 415, 198–205. [Google Scholar] [CrossRef]
- Abdulrahman, A.; Hussain, T.; Nawaz, S.; AlShaikh, S.; Almadani, A.; Bardooli, F. Is Atrial Fibrillation a Risk Factor for Worse Outcomes in Severe COVID-19 Patients: A Single Center Retrospective Cohort. J. Saudi Heart Assoc. 2021, 33, 160–168. [Google Scholar] [CrossRef] [PubMed]
- Ip, R.J.; Ali, A.; Baloch, Z.Q.; Al-Abcha, A.; Jacob, C.; Arnautovic, J.; Boumegouas, M.; Do, S.; Meka, K.; Wilcox, M.; et al. Atrial Fibrillation as a Predictor of Mortality in High Risk COVID-19 Patients: A Multicentre Study of 171 Patients. Heart Lung Circ. 2021, 30, 1151–1156. [Google Scholar] [CrossRef] [PubMed]
- Pardo Sanz, A.; Salido Tahoces, L.; Ortega Pérez, R.; González Ferrer, E.; Sánchez Recalde, Á.; Zamorano Gómez, J.L. New-onset atrial fibrillation during COVID-19 infection predicts poor prognosis. Cardiol. J. 2021, 28, 34–40. [Google Scholar] [CrossRef]
- Offerhaus, J.A.; Joosten, L.P.T.; van Smeden, M.; Linschoten, M.; Bleijendaal, H.; Tieleman, R.; Wilde, A.A.M.; Rutten, F.H.; Geersing, G.J.; Remme, C.A.; et al. Sex- and age specific association of new-onset atrial fibrillation with in-hospital mortality in hospitalised COVID-19 patients. Int. J. Cardiol. Heart Vasc. 2022, 39, 100970. [Google Scholar] [CrossRef] [PubMed]
- Li, Z.; Shao, W.; Zhang, J.; Ma, J.; Huang, S.; Yu, P.; Zhu, W.; Liu, X. Prevalence of Atrial Fibrillation and Associated Mortality Among Hospitalized Patients with COVID-19: A Systematic Review and Meta-Analysis. Front. Cardiovasc. Med. 2021, 8, 720129. [Google Scholar] [CrossRef]
- Russo, V.; Di Maio, M.; Mottola, F.F.; Pagnano, G.; Attena, E.; Verde, N.; Di Micco, P.; Silverio, A.; Scudiero, F.; Nunziata, L.; et al. Clinical characteristics and prognosis of hospitalized COVID-19 patients with incident sustained tachyarrhythmias: A multicenter observational study. Eur. J. Clin. Investig. 2020, 50, e13387. [Google Scholar] [CrossRef]
- Liu, W.C.; Lin, W.Y.; Lin, C.S.; Huang, H.B.; Lin, T.C.; Cheng, S.M.; Yang, S.P.; Lin, J.C.; Lin, W.S. Prognostic impact of restored sinus rhythm in patients with sepsis and new-onset atrial fibrillation. Crit. Care 2016, 20, 373. [Google Scholar] [CrossRef]
- Wang, T.J.; Larson, M.G.; Levy, D.; Vasan, R.S.; Leip, E.P.; Wolf, P.A.; D’Agostino, R.B.; Murabito, J.M.; Kannel, W.B.; Benjamin, E.J. Temporal relations of atrial fibrillation and congestive heart failure and their joint influence on mortality: The Framingham Heart Study. Circulation 2003, 107, 2920–2925. [Google Scholar] [CrossRef]
- Annane, D.; Sébille, V.; Duboc, D.; Le Heuzey, J.Y.; Sadoul, N.; Bouvier, E.; Bellissant, E. Incidence and prognosis of sustained arrhythmias in critically ill patients. Am. J. Respir. Crit. Care Med. 2008, 178, 20–25. [Google Scholar] [CrossRef]
- Carrera, P.; Thongprayoon, C.; Cheungpasitporn, W.; Iyer, V.N.; Moua, T. Epidemiology and outcome of new-onset atrial fibrillation in the medical intensive care unit. J. Crit. Care 2016, 36, 102–106. [Google Scholar] [CrossRef]
- Shaver, C.M.; Chen, W.; Janz, D.R.; May, A.K.; Darbar, D.; Bernard, G.R.; Bastarache, J.A.; Ware, L.B. Atrial Fibrillation Is an Independent Predictor of Mortality in Critically Ill Patients. Crit. Care Med. 2015, 43, 2104–2111. [Google Scholar] [CrossRef] [PubMed]
- Manolis, A.S. Rhythm or Rate Control Management of Atrial Fibrillation: An Overrated Dilemma. Hell. J. Cardiol. 2015, 56, 495–500. [Google Scholar]
- Zimetbaum, P. Antiarrhythmic drug therapy for atrial fibrillation. Circulation 2012, 125, 381–389. [Google Scholar] [CrossRef]
- Kirchhof, P.; Benussi, S.; Kotecha, D.; Ahlsson, A.; Atar, D.; Casadei, B.; Castella, M.; Diener, H.C.; Heidbuchel, H.; Hendriks, J.; et al. 2016 ESC Guidelines for the management of atrial fibrillation developed in collaboration with EACTS. Europace 2016, 18, 1609–1678. [Google Scholar] [CrossRef] [PubMed]
- Manolis, A.S.; Manolis, T.A. Cardiovascular complications of the coronavirus (COVID-19) infection. Rhythmos 2020, 15, 23–28. [Google Scholar]
- Lydtin, H. Side effects and contraindications of beta-receptor blocking agents. Klin. Wochenschr. 1977, 55, 415–422. [Google Scholar] [CrossRef]
- Van Gelder, I.C.; Rienstra, M.; Crijns, H.J.; Olshansky, B. Rate control in atrial fibrillation. Lancet 2016, 388, 818–828. [Google Scholar] [CrossRef]
- Wetterslev, M.; Hylander Møller, M.; Granholm, A.; Hassager, C.; Haase, N.; Lange, T.; Myatra, S.N.; Hästbacka, J.; Arabi, Y.M.; Shen, J.; et al. Atrial Fibrillation (AFIB) in the ICU: Incidence, Risk Factors, and Outcomes: The International AFIB-ICU Cohort Study. Crit. Care Med. 2023, 51, 1124–1137. [Google Scholar] [CrossRef]
- Goette, A.; Brandner, S. Atrial fibrillation on the intensive care unit: The special prognostic importance of the first manifestation. Herzschrittmachertherapie Elektrophysiologie 2022, 33, 391–397. [Google Scholar] [CrossRef]
- Wetterslev, M.; Møller, M.H.; Granholm, A.; Hassager, C.; Haase, N.; Aslam, T.N.; Shen, J.; Young, P.J.; Aneman, A.; Hästbacka, J.; et al. Management of acute atrial fibrillation in the intensive care unit: An international survey. Acta Anaesthesiol. Scand. 2022, 66, 375–385. [Google Scholar] [CrossRef]
- Bedford, J.; Drikite, L.; Corbett, M.; Doidge, J.; Ferrando-Vivas, P.; Johnson, A.; Rajappan, K.; Mouncey, P.; Harrison, D.; Young, D.; et al. Pharmacological and non-pharmacological treatments and outcomes for new-onset atrial fibrillation in ICU patients: The CAFE scoping review and database analyses. Health Technol. Assess. 2021, 25, 1–174. [Google Scholar] [CrossRef]
- Kaufman, E.S.; Zimmermann, P.A.; Wang, T.; Dennish, G.W., 3rd; Barrell, P.D.; Chandler, M.L.; Greene, H.L.; Atrial Fibrillation Follow-up Investigation of Rhythm Management Investigators. Risk of proarrhythmic events in the Atrial Fibrillation Follow-up Investigation of Rhythm Management (AFFIRM) study: A multivariate analysis. J. Am. Coll. Cardiol. 2004, 44, 1276–1282. [Google Scholar] [CrossRef]
- Manolis, A.S.; Tordjman, T.; Mack, K.D.; Estes, N.A., 3rd. Atypical pulmonary and neurologic complications of amiodarone in the same patient. Report of a case and review of the literature. Arch. Intern. Med. 1987, 147, 1805–1809. [Google Scholar] [CrossRef] [PubMed]
- Manolis, A.S. Did PALLAS deliver the final blow to dronedarone? Rhythmos 2012, 7, 1–2. [Google Scholar]
- Chiladakis, J.A.; Kalogeropoulos, A.; Patsouras, N.; Manolis, A.S. Ibutilide added to propafenone for the conversion of atrial fibrillation and atrial flutter. J. Am. Coll. Cardiol. 2004, 44, 859–863. [Google Scholar] [CrossRef]
- Manolis, A.S.; Bethanis, S.; Metaxa, S.; Polytarchou, K.; Sakellaris, N.; Pyrros, I. Use of intravenous vernakalant for atrial fibrillation conversion in the regular ward under only bedside monitoring. Hell. J. Cardiol. 2019, 60, 54–56. [Google Scholar] [CrossRef]
- Pantazopoulos, I.; Mavrovounis, G.; Dimeas, G.; Zikos, N.; Pitsikou, M.; Rousogianni, E.; Mermiri, M.; Michou, A.; Spanos, M.; Maniotis, C.; et al. Remdesivir-induced Bradycardia is not Associated with Worse Outcome in Patients with COVID-19: A Retrospective Analysis. Am. J. Cardiovasc. Drugs 2022, 22, 705–710. [Google Scholar] [CrossRef] [PubMed]
- Berman, J.P.; Abrams, M.P.; Kushnir, A.; Rubin, G.A.; Ehlert, F.; Biviano, A.; Morrow, J.P.; Dizon, J.; Wan, E.Y.; Yarmohammadi, H.; et al. Cardiac electrophysiology consultative experience at the epicenter of the COVID-19 pandemic in the United States. Indian Pacing Electrophysiol. J. 2020, 20, 250–256. [Google Scholar] [CrossRef]
- January, C.T.; Wann, L.S.; Alpert, J.S.; Calkins, H.; Cigarroa, J.E.; Cleveland, J.C., Jr.; Conti, J.B.; Ellinor, P.T.; Ezekowitz, M.D.; Field, M.E.; et al. 2014 AHA/ACC/HRS guideline for the management of patients with atrial fibrillation: A report of the American College of Cardiology/American Heart Association Task Force on practice guidelines and the Heart Rhythm Society. Circulation 2014, 130, e199–e267. [Google Scholar] [CrossRef]
| Study | Study Type | MV (%) | n | M% | ICU % | NOAF (%) | NOAF Ward/ICU | Age Mean | HF Troponin /Echo | Mortality | HF Difference | Mortality 1 No/NOAF |
|---|---|---|---|---|---|---|---|---|---|---|---|---|
| Liu K 2020 [27] | Retrospective | 0 | 137 | 45 | NA | 7.3% palpitations | 57 | NA | 11.7% | NA | NA | |
| Angeli F 2020 [10] | Retrospective | 0 | 50 | 72 | 0 | 3 | NA | 64 | NA | NA | NO | NA |
| Bhatla A 2020 [11] | Retrospective | NA | 700 | 45 | 11 | 25 | NA | 50 | Troponin | 4% | NA | 3/23 |
| Wang Y 2020 [5] | Retrospective | 0 | 319 | 48 | 30 | 20 | NA | 65 | Troponin | NA | NA | NA |
| Kanthasamy V 2021 [28] | Retrospective | NA | 109 | 83 | 100 | 14.6 | NA/14.6 | 59 | Troponin + Echo | 38% | NO | 29/69 |
| Colon C 2020 [13] | Retrospective | NA | 115 | 54 | 60 | 16.5 (NOAF + AF) | 0/27.5 | 57.2 | Troponin | NA | NA | NA |
| Kensara R 2023 [29] | Retrospective | 74.5 | 1256 | 62.3 | 100 | 10.7 | NA/10.7 | 61 | NA | NA | 50.6/63.3 | |
| Zakynthinos G 2022 [21] | Prospective | 100 | 79 | 76 | 100 | 24 | NA/24 | 69 | Troponin + Echo | 45 | NO | 41.7/47 |
| Ergün B 2021 [30] | Retrospective | NA | 248 | 78 | 100 | 14.9 | NA/14.9 | 71 | Troponin | NA | NO | 67/87 |
| Goyal P 2020 [14] | Retrospective | 33 | 393 | 60.6 | NA | 7.1 | MV 17.7/ NO MV 1.9 | 62.2 | NA | 10.2 | NA | NA |
| Romiti G 2021 [31] | Meta-analysis | NA | 187,716 | 70 | NA | 8 | NA | NA | NA | NA | NA | 4-fold increase |
| Rosenblatt A 2022 [32] | Registry | NA | 30,999 | 51 | 26 | 5.4 | NA/11.9 | 61.6 | NA | 13.6 | NA | 11.9/45.2 |
| Abdulrahman A 2021 [33] | Retrospective | NA | 492 | NA | 100 | 6.1 | NA/6.1 | 53.4 | Echo | 16.3 | NO | 13.7/56.7 |
| Ip R 2021 [34] | Retrospective | NA | 171 | 57 | 100 | 18.7 | NA/18.7 | 66.1 | Echo | 46.2 | NA | 40.3/72 |
| Pardo Sanz A 2021 [35] | Retrospective | NA | 160 | 60 | 4 | 7.5 | NA | 65.7 | Troponin | 18.8 | NO | 17.6/33.3 |
| Offerhaus J 2022 [36] | Retrospective | NA | 5782 | 64 | NA | 11 | NA | 67 | NA | 16 | NA | 1.9-fold increase |
| Li Z 2021 [37] | Meta-analysis | NA | 2165 13,075 * | 58.7 | NA | 11 | NA | NA | NA | NA | 29.3/50.6 * | |
| Russo V 2020 [38] | Retrospective | NA | 414 | 61.1 | NA | 17.1 | NA | 66.9 | NA | 25.8 | NA | ND |
Disclaimer/Publisher’s Note: The statements, opinions and data contained in all publications are solely those of the individual author(s) and contributor(s) and not of MDPI and/or the editor(s). MDPI and/or the editor(s) disclaim responsibility for any injury to people or property resulting from any ideas, methods, instructions or products referred to in the content. |
© 2023 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Zakynthinos, G.E.; Tsolaki, V.; Oikonomou, E.; Vavouranakis, M.; Siasos, G.; Zakynthinos, E. New-Onset Atrial Fibrillation in the Critically Ill COVID-19 Patients Hospitalized in the Intensive Care Unit. J. Clin. Med. 2023, 12, 6989. https://doi.org/10.3390/jcm12226989
Zakynthinos GE, Tsolaki V, Oikonomou E, Vavouranakis M, Siasos G, Zakynthinos E. New-Onset Atrial Fibrillation in the Critically Ill COVID-19 Patients Hospitalized in the Intensive Care Unit. Journal of Clinical Medicine. 2023; 12(22):6989. https://doi.org/10.3390/jcm12226989
Chicago/Turabian StyleZakynthinos, George E., Vasiliki Tsolaki, Evangelos Oikonomou, Manolis Vavouranakis, Gerasimos Siasos, and Epaminondas Zakynthinos. 2023. "New-Onset Atrial Fibrillation in the Critically Ill COVID-19 Patients Hospitalized in the Intensive Care Unit" Journal of Clinical Medicine 12, no. 22: 6989. https://doi.org/10.3390/jcm12226989
APA StyleZakynthinos, G. E., Tsolaki, V., Oikonomou, E., Vavouranakis, M., Siasos, G., & Zakynthinos, E. (2023). New-Onset Atrial Fibrillation in the Critically Ill COVID-19 Patients Hospitalized in the Intensive Care Unit. Journal of Clinical Medicine, 12(22), 6989. https://doi.org/10.3390/jcm12226989










