Posterior Quadratus Lumborum Block or Thoracolumbar Interfascial Plane Block and Postoperative Analgesia after Spinal Surgery: A Randomized Controlled Trial
Abstract
:1. Introduction
2. Materials and Methods
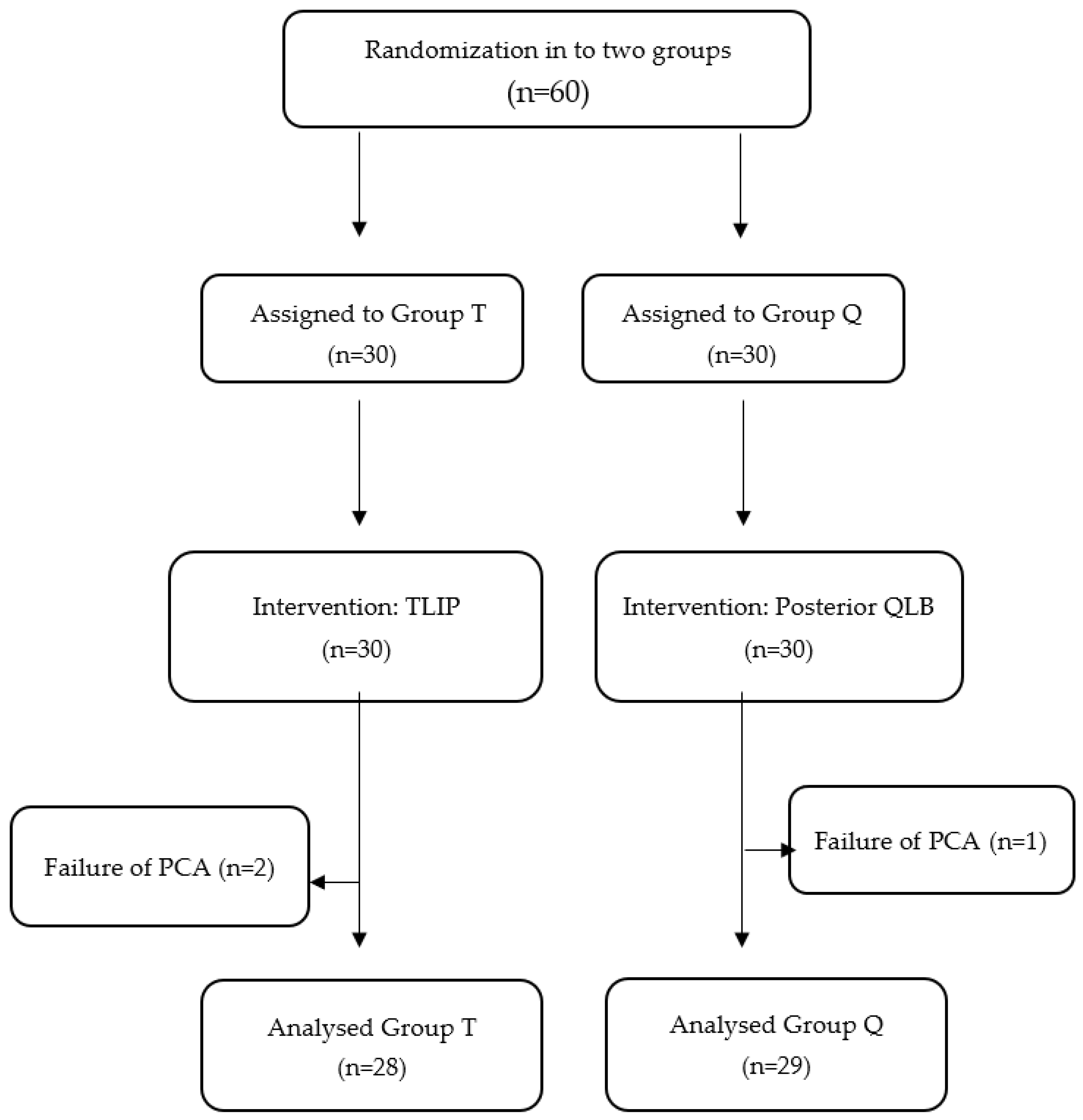
2.1. Study Design
2.2. Randomization and Blinding
2.3. Ultrasound-Guided Block Applications
2.4. Management of General Anesthesia and Perioperative Pain
2.5. Standard Postoperative Analgesia Protocol and Measurements of Pain
2.6. Outcome Measurements
2.7. Sample Size and Statistical Analysis
3. Results
4. Discussion
5. Conclusions
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Conflicts of Interest
References
- Kumar, V.; Bansal, P.; Dhillon, M.; Dhatt, S.S.; Vatkar, A.J. Surgical techniques and perioperative surgical outcomes after discectomy for calcified lumbar disc herniation: A review and meta-analysis. Eur. Spine J. 2023. [Google Scholar] [CrossRef]
- Prabhakar, N.K.; Chadwick, A.L.; Nwaneshiudu, C.; Aggarwal, A.; Salmasi, V.; Lii, T.R.; Hah, J.M. Management of Postoperative Pain in Patients Following Spine Surgery: A Narrative Review. Int. J. Gen. Med. 2022, 15, 4535–4549. [Google Scholar] [CrossRef]
- Yin, F.; Wang, X.H.; Liu, F. Effect of Intravenous Paracetamol on Opioid Consumption in Multimodal Analgesia After Lumbar Disc Surgery: A Meta-Analysis of Randomized Controlled Trials. Front. Pharmacol. 2022, 13, 860106. [Google Scholar] [CrossRef]
- Zhou, Z.; Jin, M.C.; Jensen, M.R.; Guinle, M.I.B.; Ren, A.; Agarwal, A.A.; Leaston, J.; Ratliff, J.K. Opioid Usage in Lumbar Disc Herniation Patients with Nonsurgical, Early Surgical, and Late Surgical Treatments. World Neurosurg. 2023, 173, e180–e188. [Google Scholar] [CrossRef]
- Yayik, A.M.; Cesur, S.; Ozturk, F.; Ahiskalioglu, A.; Ay, A.N.; Celik, E.C.; Karaavci, N.C. Postoperative Analgesic Efficacy of the Ultrasound-Guided Erector Spinae Plane Block in Patients Undergoing Lumbar Spinal Decompression Surgery: A Randomized Controlled Study. World Neurosurg. 2019, 126, e779–e785. [Google Scholar] [CrossRef]
- Melvin, J.P.; Schrot, R.J.; Chu, G.M.; Chin, K.J. Low thoracic erector spinae plane block for perioperative analgesia in lumbosacral spine surgery: A case series. Can. J. Anaesth. 2018, 65, 1057–1065. [Google Scholar] [CrossRef]
- Singh, S.; Chaudhary, N.K. Bilateral Ultasound Guided Erector Spinae Plane Block for Postoperative Pain Management in Lumbar Spine Surgery: A Case Series. J. Neurosurg. Anesthesiol. 2018, 31, 354. [Google Scholar] [CrossRef]
- Hu, Z.; Han, J.; Jiao, B.; Jiang, J.; Sun, Y.; Lv, Z.; Wang, J.; Tian, X.; Wang, H. Efficacy of Thoracolumbar Interfascial Plane Block for Postoperative Analgesia in Lumbar Spine Surgery: A Meta-analysis of Randomized Clinical Trials. Pain Physician 2021, 24, E1085–E1097. [Google Scholar]
- Alver, S.; Ciftci, B.; Celik, E.C.; Sargolzaeimoghaddam, M.; Cetinkal, A.; Erdogan, C.; Ahiskalioglu, A. Postoperative recovery scores and pain management: A comparison of modified thoracolumbar interfascial plane block and quadratus lumborum block for lumbar disc herniation. Eur. Spine J. 2023. [Google Scholar] [CrossRef]
- Benyamin, R.; Trescot, A.M.; Datta, S.; Buenaventura, R.; Adlaka, R.; Sehgal, N.; Glaser, S.E.; Vallejo, R. Opioid complications and side effects. Pain Physician 2008, 11 (Suppl. S2), S105–S120. [Google Scholar] [CrossRef]
- Hand, W.R.; Taylor, J.M.; Harvey, N.R.; Epperson, T.I.; Gunselman, R.J.; Bolin, E.D.; Whiteley, J. Thoracolumbar interfascial plane (TLIP) block: A pilot study in volunteers. Can. J. Anaesth. 2015, 62, 1196–1200. [Google Scholar] [CrossRef]
- Eltaher, E.; Nasr, N.; Abuelnaga, M.E.; Elgawish, Y. Effect of Ultrasound-Guided Thoracolumbar Interfascial Plane Block on the Analgesic Requirements in Patients Undergoing Lumbar Spine Surgery Under General Anesthesia: A Randomized Controlled Trial. J. Pain Res. 2021, 14, 3465–3474. [Google Scholar] [CrossRef]
- Blanco, R.; Ansari, T.; Riad, W.; Shetty, N. Quadratus Lumborum Block Versus Transversus Abdominis Plane Block for Postoperative Pain After Cesarean Delivery: A Randomized Controlled Trial. Reg. Anesth. Pain Med. 2016, 41, 757–762. [Google Scholar] [CrossRef]
- Chin, K.J.; Lirk, P.; Hollmann, M.W.; Schwarz, S.K.W. Mechanisms of action of fascial plane blocks: A narrative review. Reg. Anesth. Pain Med. 2021, 46, 618–628. [Google Scholar] [CrossRef]
- Roofthooft, E.; Joshi, G.P.; Rawal, N.; Van de Velde, M.; PROSPECT Working Group* of the European Society of Regional Anaesthesia and Pain Therapy and supported by the Obstetric Anaesthetists’ Association. PROSPECT guideline for elective caesarean section: Updated systematic review and procedure-specific postoperative pain management recommendations. Anaesthesia 2021, 76, 665–680. [Google Scholar] [CrossRef]
- Koksal, E.; Aygun, H.; Genç, C.; Kaya, C.; Dost, B. Comparison of the analgesic effects of two quadratus lumborum blocks (QLBs), QLB type II vs QLB type III, in caesarean delivery: A randomised study. Int. J. Clin. Pract. 2021, 75, e14513. [Google Scholar] [CrossRef]
- Diren, F.; Ozdemir, O.; Boyali, O.; Bahar-Ozdemir, Y.; Kabatas, S.; Civelek, E. Percutaneous Pain Procedures in Patients Who Underwent Lumbar Disc Herniation Surgery: Is It an Important Tool in the Management of Post-Surgical Ongoing Pain? Turk. Neurosurg. 2023, 33, 898–905. [Google Scholar] [CrossRef]
- Johansson, A.C.; Linton, S.J.; Rosenblad, A.; Bergkvist, L.; Nilsson, O. A prospective study of cognitive behavioural factors as predictors of pain, disability and quality of life one year after lumbar disc surgery. Disabil. Rehabil. 2010, 32, 521–529. [Google Scholar] [CrossRef]
- Costelloe, C.; Burns, S.; Yong, R.J.; Kaye, A.D.; Urman, R.D. An Analysis of Predictors of Persistent Postoperative Pain in Spine Surgery. Curr. Pain Headache Rep. 2020, 24, 11. [Google Scholar] [CrossRef]
- Ahiskalioglu, A.; Yayik, A.M.; Celik, E.C.; Aydin, M.E.; Uzun, G. Ultrasound guided modified Thoracolumbar Interfascial Plane block for low back pain management. J. Clin. Anesth. 2019, 54, 54138–54139. [Google Scholar] [CrossRef]
- Ahiskalioglu, A.; Alici, H.A.; Selvitopi, K.; Yayik, A.M. Ultrasonography-guided modified thoracolumbar interfascial plane block: A new approach. Can. J. Anaesth. 2017, 64, 775–776. [Google Scholar] [CrossRef]
- Long, G.; Liu, C.; Liang, T.; Zhan, X. The efficacy of thoracolumbar interfascial plane block for lumbar spinal surgeries: A systematic review and meta-analysis. J. Orthop. Surg. Res. 2023, 18, 318. [Google Scholar] [CrossRef]
- Ye, Y.; Bi, Y.; Ma, J.; Liu, B. Thoracolumbar interfascial plane block for postoperative analgesia in spine surgery: A systematic review and meta-analysis. PLoS ONE 2021, 16, e0251980. [Google Scholar] [CrossRef]
- Chen, K.; Wang, L.; Ning, M.; Dou, L.; Li, W.; Li, Y. Evaluation of ultrasound-guided lateral thoracolumbar interfascial plane block for postoperative analgesia in lumbar spine fusion surgery: A prospective, randomized, and controlled clinical trial. PeerJ 2019, 7, e7967. [Google Scholar] [CrossRef]
- Wilton, J.; Chiu, H.; Codianne, N.; Knapp, H.; Escolar, V.R.; Burns, S. Continuous quadratus lumborum block as post-operative strategy for pain control in spinal fusion surgery. Indian J. Anaesth. 2020, 64, 869–873. [Google Scholar] [CrossRef]
- Elsharkawy, H.; El-Boghdadly, K.; Barrington, M. Quadratus Lumborum Block: Anatomical Concepts, Mechanisms, and Techniques. Anesthesiology 2019, 130, 322–335. [Google Scholar] [CrossRef]
- Elsharkawy, H.; El-Boghdadly, K.; Kolli, S.; Esa, W.A.S.; DeGrande, S.; Soliman, L.M.; Drake, R.L. Injectate spread following anterior sub-costal and posterior approaches to the quadratus lumborum block. Eur. J. Anaesthesiol. 2017, 34, 587–595. [Google Scholar] [CrossRef]
- Sertçakacilar, G.; Yildiz, G.Ö. Evaluation of the efficacy of posterior approach quadratus lumborum block for postoperative analgesia after lumbar discectomy surgery; Retrospective observational study. JOGHENS 2022, 5, 12–22. [Google Scholar]
| Group T (n = 28) | Group Q (n = 29) | p | |
|---|---|---|---|
| Age (years) | 43.07 ± 14.04 | 42.79 ± 11.70 | 0.935 |
| Gender (male/female) | 17/11 | 16/13 | 0.877 |
| ASA I/II/III (n) | 6/21/1 | 11/16/2 | 0.292 |
| Operation duration (minutes) | 87.43 ± 28.38 | 86.72 ± 20.15 | 0.968 |
| Level of surgery (L2–L3/L3–L4/L4–L5/L5–S1) (n) | 2/14/11/1 | 1/15/13/0 | |
| BMI (kg/m2) | 26.22 ± 3.05 | 26.64 ± 2.87 | 0.594 |
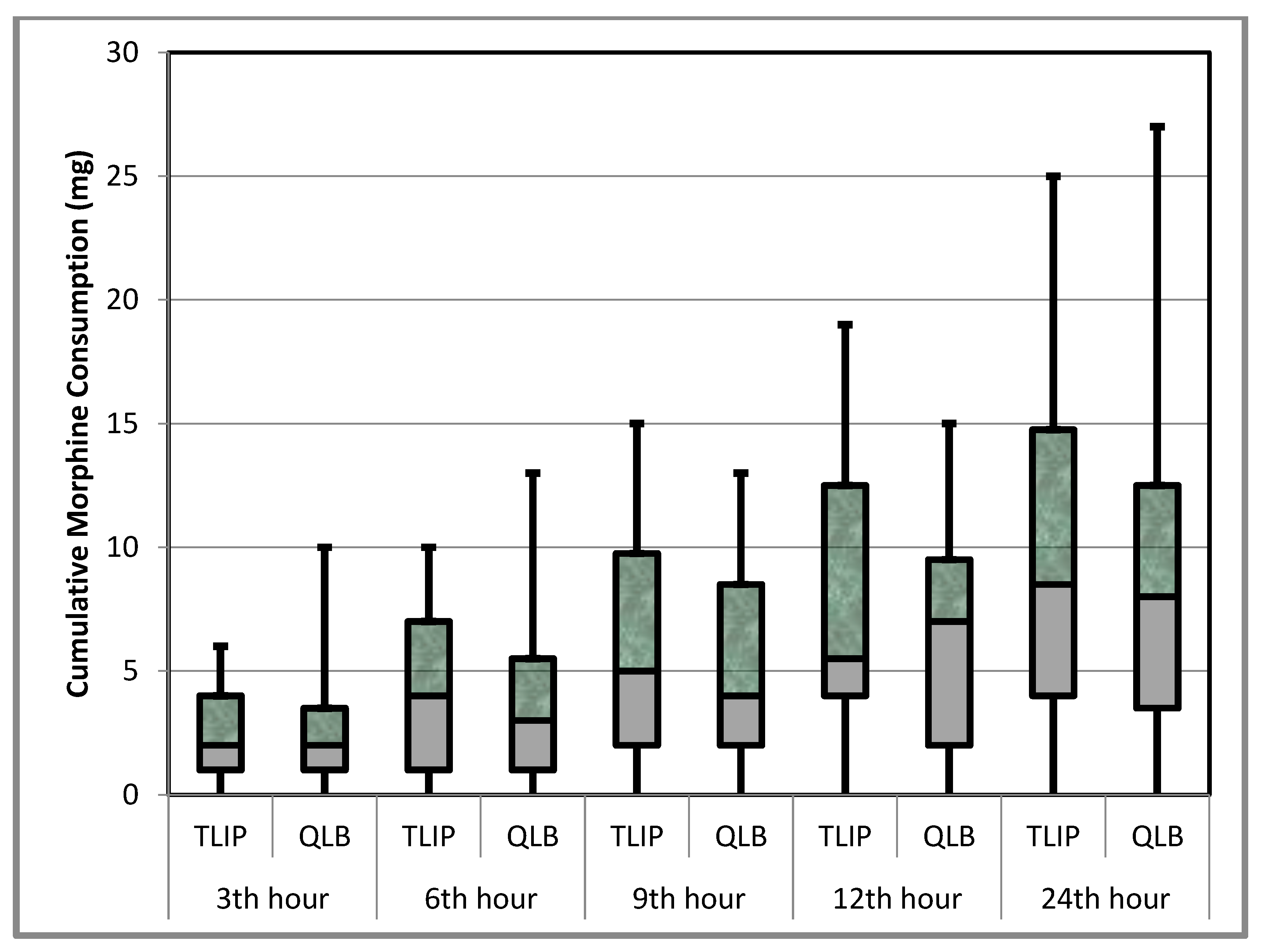
| Morphine Consumption (mg) | Group T (n = 28) | Group Q (n = 29) | p |
|---|---|---|---|
| 0th hour | 0 (0–0) | 0 (0–0) | 0.384 |
| 3rd hour | 2 (1–4) | 2 (1–3.5) | 0.948 |
| 6th hour | 4 (1–7) | 3 (1–5.5) | 0.403 |
| 9th hour | 5 (2–9.75) | 4 (2–8.5) | 0.516 |
| 12th hour | 5.5 (4–12.5) | 7 (2–9.5) | 0.575 |
| 24th hour | 8.5 (4–14.75) | 8 (3.5–12.5) | 0.780 |
| Group T (n = 28) | Group Q (n = 29) | p | |
|---|---|---|---|
| NRS at rest | |||
| 0th hour | 2.5 (0–3) | 2 (0–2.5) | 0.283 |
| 3rd hour | 2 (1.25–3) | 2 (1.5–2.5) | 0.496 |
| 6th hour | 2 (1–2) | 2 (1–2) | 0.635 |
| 9th hour | 1 (1–2) | 2 (1–2) | 0.556 |
| 12th hour | 1 (1–2) | 1 (1–2) | 0.873 |
| 24th hour | 1 (1–2) | 18 (1–2) | 0.937 |
| NRS in motion | |||
| 3rd hour | 3 (2–4) | 3 (2–3) | 0.724 |
| 6th hour | 2 (2–3) | 3 (2–3) | 0.342 |
| 9th hour | 2 (2–3) | 2 (2–3) | 0.110 |
| 12th hour | 2 (2–3) | 2 (2–3) | 0.432 |
| 24th hour | 2 (1.25–2) | 2 (1.5–2) | 0.390 |
Disclaimer/Publisher’s Note: The statements, opinions and data contained in all publications are solely those of the individual author(s) and contributor(s) and not of MDPI and/or the editor(s). MDPI and/or the editor(s) disclaim responsibility for any injury to people or property resulting from any ideas, methods, instructions or products referred to in the content. |
© 2023 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Canikli Adıgüzel, Ş.; Akyurt, D.; Bahadır Altun, H.; Ültan Özgen, G.; Akdeniz, S.; Bayraktar, B.; Tulgar, S.; Yiğit, Y. Posterior Quadratus Lumborum Block or Thoracolumbar Interfascial Plane Block and Postoperative Analgesia after Spinal Surgery: A Randomized Controlled Trial. J. Clin. Med. 2023, 12, 7217. https://doi.org/10.3390/jcm12237217
Canikli Adıgüzel Ş, Akyurt D, Bahadır Altun H, Ültan Özgen G, Akdeniz S, Bayraktar B, Tulgar S, Yiğit Y. Posterior Quadratus Lumborum Block or Thoracolumbar Interfascial Plane Block and Postoperative Analgesia after Spinal Surgery: A Randomized Controlled Trial. Journal of Clinical Medicine. 2023; 12(23):7217. https://doi.org/10.3390/jcm12237217
Chicago/Turabian StyleCanikli Adıgüzel, Şenay, Dilan Akyurt, Hatice Bahadır Altun, Gökçe Ültan Özgen, Sevda Akdeniz, Birol Bayraktar, Serkan Tulgar, and Yavuz Yiğit. 2023. "Posterior Quadratus Lumborum Block or Thoracolumbar Interfascial Plane Block and Postoperative Analgesia after Spinal Surgery: A Randomized Controlled Trial" Journal of Clinical Medicine 12, no. 23: 7217. https://doi.org/10.3390/jcm12237217
APA StyleCanikli Adıgüzel, Ş., Akyurt, D., Bahadır Altun, H., Ültan Özgen, G., Akdeniz, S., Bayraktar, B., Tulgar, S., & Yiğit, Y. (2023). Posterior Quadratus Lumborum Block or Thoracolumbar Interfascial Plane Block and Postoperative Analgesia after Spinal Surgery: A Randomized Controlled Trial. Journal of Clinical Medicine, 12(23), 7217. https://doi.org/10.3390/jcm12237217






