Anatomical and Functional Effects of an Oral Supplementation of Bromelain and Curcugreen in Patients with Focal Diabetic Macular Edema
Abstract
:1. Introduction
2. Materials and Methods
Statistical Methods
3. Results
4. Discussion
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Conflicts of Interest
References
- Teo, Z.L.; Tham, Y.C.; Yu, M.; Chee, M.L.; Rim, T.H.; Cheung, N.; Bikbov, M.M.; Wang, Y.X.; Tang, Y.; Lu, Y.; et al. Global Prevalence of Diabetic Retinopathy and Projection of Burden through 2045: Systematic Review and Meta-analysis. Ophthalmology 2021, 128, 1580–1591. [Google Scholar] [CrossRef] [PubMed]
- Cheung, N.; Mitchell, P.; Wong, T.Y. Diabetic retinopathy. Lancet 2010, 376, 124–136. [Google Scholar] [CrossRef] [PubMed]
- Daruich, A.; Matet, A.; Moulin, A.; Kowalczuk, L.; Nicolas, M.; Sellam, A.; Rothschild, P.R.; Omri, S.; Gélizé, E.; Jonet, L.; et al. Mechanisms of macular edema: Beyond the surface. Prog. Retin. Eye Res. 2018, 63, 20–68. [Google Scholar] [CrossRef] [PubMed]
- Chen, Y.H.; Chou, H.C.; Lin, S.T.; Chen, Y.W.; Lo, Y.W.; Chan, H.L. Effect of high glucose on secreted proteome in cultured retinal pigmented epithelium cells: Its possible relevance to clinical diabetic retinopathy. J. Proteom. 2012, 77, 111–128. [Google Scholar] [CrossRef] [PubMed]
- Inumaru, J.; Nagano, O.; Takahashi, E.; Ishimoto, T.; Nakamura, S.; Suzuki, Y.; Niwa, S.; Umezawa, K.; Tanihara, H.; Saya, H. Molecular mechanisms regulating dissociation of cell-cell junction of epithelial cells by oxidative stress. Genes Cells 2009, 14, 703–716. [Google Scholar] [CrossRef] [PubMed]
- Omri, S.; Behar-Cohen, F.; Rothschild, P.R.; Gélizé, E.; Jonet, L.; Jeanny, J.C.; Omri, B.; Crisanti, P. PKCζ mediates breakdown of outer blood-retinal barriers in diabetic retinopathy. PLoS ONE 2013, 8, e81600. [Google Scholar] [CrossRef] [PubMed]
- Cachafeiro, M.; Bemelmans, A.P.; Samardzija, M.; Afanasieva, T.; Pournaras, J.A.; Grimm, C.; Kostic, C.; Philippe, S.; Wenzel, A.; Arsenijevic, Y. Hyperactivation of retina by light in mice leads to photoreceptor cell death mediated by VEGF and retinal pigment epithelium permeability. Cell Death Dis. 2013, 4, e781. [Google Scholar] [CrossRef]
- Bandello, F.; Battaglia Parodi, M.; Lanzetta, P.; Loewenstein, A.; Massin, P.; Menchini, F.; Veritti, D. Diabetic Macular Edema. Dev. Ophthalmol. 2017, 58, 102–138. [Google Scholar]
- Gurung, R.L.; Fitzgerald, L.M.; McComish, B.J.; Verma, N.; Burdon, K.P. Identifying Genetic Risk Factors for Diabetic Macular Edema and the Response to Treatment. J. Diabetes Res. 2020, 2020, 5016916. [Google Scholar] [CrossRef]
- Michaelides, M.; Kaines, A.; Hamilton, R.D.; Fraser-Bell, S.; Rajendram, R.; Quhill, F.; Boos, C.J.; Xing, W.; Egan, C.; Peto, T.; et al. A prospective randomized trial of intravitreal bevacizumab or laser therapy in the management of diabetic macular edema (BOLT study) 12-month data: Report 2. Ophthalmology 2010, 117, 1078–1086.e2. [Google Scholar] [CrossRef]
- Wells, J.A.; Glassman, A.R.; Ayala, A.R.; Jampol, L.M.; Bressler, N.M.; Bressler, S.B.; Brucker, A.J.; Ferris, F.L.; Hampton, G.R.; Jhaveri, C.; et al. Diabetic Retinopathy Clinical Research Network. Aflibercept, Bevacizumab, or Ranibizumab for Diabetic Macular Edema: Two-Year Results from a Comparative Effectiveness Randomized Clinical Trial. Ophthalmology 2016, 123, 1351–1359. [Google Scholar] [CrossRef]
- Boyer, D.S.; Yoon, Y.H.; Belfort, R., Jr.; Bandello, F.; Maturi, R.K.; Augustin, A.J.; Li, X.Y.; Cui, H.; Hashad, Y.; Whitcup, S.M. Ozurdex MEAD Study Group. Three-year, randomized, sham-controlled trial of dexamethasone intravitreal implant in patients with diabetic macular edema. Ophthalmology 2014, 121, 1904–1914. [Google Scholar] [CrossRef] [PubMed]
- Schmidt-Erfurth, U.; Garcia-Arumi, J.; Bandello, F.; Berg, K.; Chakravarthy, U.; Gerendas, B.S.; Jonas, J.; Larsen, M.; Tadayoni, R.; Loewenstein, A. Guidelines for the Management of Diabetic Macular Edema by the European Society of Retina Specialists (EURETINA). Ophthalmologica 2017, 237, 185–222. [Google Scholar] [CrossRef] [PubMed]
- Rossino, M.G.; Casini, G. Nutraceuticals for the Treatment of Diabetic Retinopathy. Nutrients 2019, 2, 771. [Google Scholar] [CrossRef]
- Taussig, S.J.; Batkin, S. Bromelain, the enzyme complex of pineapple (Ananas comosus) and its clinical application. An update. J. Ethnopharmacol. 1988, 22, 191–203. [Google Scholar] [CrossRef]
- Hikisz, P.; Bernasinska-Slomczewska, J. Beneficial Properties of Bromelain. Nutrients 2021, 13, 4313. [Google Scholar] [CrossRef]
- Flynn, D.L.; Rafferty, M.F.; Boctor, A.M. Inhibition of 5-hydroxy-eicosatetraenoic acid (5-HETE) formation in intact human neutrophils by naturally-occurring diarylheptanoids: Inhibitory activities of curcuminoids and yakuchinones. Prostaglandins Leukot. Med. 1986, 22, 357–360. [Google Scholar] [CrossRef]
- Peddada, K.V.; Brown, A.; Verma, V.; Nebbioso, M. Therapeutic potential of curcumin in major retinal pathologies. Int. Ophthalmol. 2019, 39, 725–734. [Google Scholar] [CrossRef]
- Huang, M.T.; Lysz, T.; Ferraro, T.; Abidi, T.F.; Laskin, J.D.; Conney, A.H. Inhibitory effects of curcumin on in vitro lipoxygenase and cyclooxygenase activities in mouse epidermis. Cancer Res. 1991, 51, 813–819. [Google Scholar]
- Manna, J.; Dunbar, G.L.; Maiti, P. Curcugreen Treatment Prevented Splenomegaly and Other Peripheral Organ Abnormalities in 3xTg and 5xFAD Mouse Models of Alzheimer’s Disease. Antioxidants 2021, 10, 899. [Google Scholar] [CrossRef]
- Huang, D.; Swanson, E.A.; Lin, C.P.; Schuman, J.S.; Stinson, W.G.; Chang, W.; Hee, M.R.; Flotte, T.; Gregory, K.; Puliafito, C.A.; et al. Optical coherence tomography. Science 1991, 254, 1178–1181. [Google Scholar] [CrossRef] [PubMed]
- Cole, E.D.; Novais, E.A.; Louzada, R.N.; Waheed, N.K. Contemporary retinal imaging techniques in diabetic retinopathy: A review. Clin. Exp. Ophthalmol. 2016, 44, 289–299. [Google Scholar] [CrossRef]
- Wang, R.K.; Jacques, S.L.; Ma, Z.; Hurst, S.; Hanson, S.R.; Gruber, A. Three dimensional optical angiography. Opt. Express. 2007, 15, 4083–4097. [Google Scholar] [CrossRef] [PubMed]
- Munia, I.; Gafray, L.; Bringer, M.A.; Goldschmidt, P.; Proukhnitzky, L.; Jacquemot, N.; Cercy, C.; Ramchani Ben Otman, K.; Errera, M.H.; Ranchon-Cole, I. Cytoprotective Effects of Natural Highly Bio-Available Vegetable Derivatives on Human-Derived Retinal Cells. Nutrients 2020, 12, 879. [Google Scholar] [CrossRef] [PubMed]
- Allegri, P.; Mastromarino, A.; Neri, P. Management of chronic anterior uveitis relapses: Efficacy of oral phospholipidic curcumin treatment. Long-term follow-up. Clin. Ophthalmol. 2010, 4, 1201–1206. [Google Scholar] [CrossRef]
- Mandal, M.N.; Patlolla, J.M.; Zheng, L.; Agbaga, M.P.; Tran, J.T.; Wicker, L.; Kasus-Jacobi, A.; Elliott, M.H.; Rao, C.V.; Anderson, R.E. Curcumin protects retinal cells from light-and oxidant stress-induced cell death. Free Radic. Biol. Med. 2009, 46, 672–679. [Google Scholar] [CrossRef]
- Muangnoi, C.; Sharif, U.; Ratnatilaka Na Bhuket, P.; Rojsitthisak, P.; Paraoan, L. Protective Effects of Curcumin Ester Prodrug, Curcumin Diethyl Disuccinate against H2O2-Induced Oxidative Stress in Human Retinal Pigment Epithelial Cells: Potential Therapeutic Avenues for Age-Related Macular Degeneration. Int. J. Mol. Sci. 2019, 20, 3367. [Google Scholar] [CrossRef]
- Mazzolani, F.; Togni, S. Oral administration of a curcumin-phospholipid delivery system for the treatment of central serous chorioretinopathy: A 12-month follow-up study. Clin. Ophthalmol. 2013, 7, 939–945. [Google Scholar] [CrossRef]
- Wilkinson, C.P.; Ferris, F.L., III; Klein, R.E.; Lee, P.P.; Agardh, C.D.; Davis, M.; Dills, D.; Kampik, A.; Pararajasegaram, R.; Verdaguer, J.T. Global Diabetic Retinopathy Project Group. Proposed international clinical diabetic retinopathy and diabetic macular edema disease severity scales. Ophthalmology 2003, 110, 1677–1682. [Google Scholar] [CrossRef]
- Kalra, E.K. Nutraceutical--definition and introduction. AAPS PharmSci. 2003, 5, E25. [Google Scholar] [CrossRef]
- Aggarwal, B.B.; Van Kuiken, M.E.; Iyer, L.H.; Harikumar, K.B.; Sung, B. Molecular targets of nutraceuticals derived from dietary spices: Potential role in suppression of inflammation and tumorigenesis. Exp. Biol. Med. 2009, 234, 825–849. [Google Scholar] [CrossRef]
- Parravano, M.; Allegrini, D.; Carnevali, A.; Costanzo, E.; Giannaccare, G.; Giorno, P.; Scorcia, V.; Spedicato, G.A.; Varano, M.; Romano, M.R. Effectiveness of a Hydrophilic Curcumin-Based Formulation in Coadjuvating the Therapeutic Effect of Intravitreal Dexamethasone in Subjects with Diabetic Macular Edema. Front. Pharmacol. 2022, 4, 726104. [Google Scholar] [CrossRef] [PubMed]
- Mazzolani, F.; Togni, S.; Giacomelli, L.; Eggenhoffner, R.; Franceschi, F. Oral administration of a curcumin-phospholipid formulation (Meriva®) for treatment of chronic diabetic macular edema: A pilot study. Eur. Rev. Med. Pharmacol. Sci. 2018, 22, 3617–3625. [Google Scholar]
- Guarino, O.; Iovino, C.; Di Iorio, V.; Rosolia, A.; Schiavetti, I.; Lanza, M.; Simonelli, F. Anatomical and Functional Effects of Oral Administration of Curcuma Longa and Boswellia Serrata Combination in Patients with Treatment-Naïve Diabetic Macular Edema. J. Clin. Med. 2022, 11, 4451. [Google Scholar] [CrossRef] [PubMed]
- Carnevali, A.; Sacconi, R.; Corbelli, E.; Tomasso, L.; Querques, L.; Zerbini, G.; Scorcia, V.; Bandello, F.; Querques, G. Optical coherence tomography angiography analysis of retinal vascular plexuses and choriocapillaris in patients with type 1 diabetes without diabetic retinopathy. Acta Diabetol. 2017, 54, 695–702. [Google Scholar] [CrossRef] [PubMed]
- Chiosi, F.; Rinaldi, M.; Campagna, G.; Manzi, G.; De Angelis, V.; Calabrò, F.; D’Andrea, L.; Tranfa, F.; Costagliola, C. Effect of a Fixed Combination of Curcumin, Artemisia, Bromelain, and Black Pepper Oral Administration on Optical Coherence Tomography Angiography Indices in Patients with Diabetic Macular Edema. Nutrients 2022, 14, 1520. [Google Scholar] [CrossRef]
- Sun, Z.; Tang, F.; Wong, R.; Lok, J.; Szeto, S.K.H.; Chan, J.C.K.; Chan, C.K.M.; Tham, C.C.; Ng, D.S.; Cheung, C.Y. OCT Angiography Metrics Predict Progression of Diabetic Retinopathy and Development of Diabetic Macular Edema: A Prospective Study. Ophthalmology 2019, 126, 1675–1684. [Google Scholar] [CrossRef]
| Total n = 33 | Group A n = 18 | Group B n = 15 | p | |
|---|---|---|---|---|
| Age, mean ± SD, years | 64.30 ± 10.39 | 68.56 ± 6.96 | 59.20 ± 11.69 | 0.2883 |
| Male, N (%) | 21 (63.63) | 13 (72.22) | 8 (53.33) | 0.3005 |
| BCVA, mean ± SD, ETDRS Letters | 43.91 ± 7.34 | 43.06 ± 8.02 | 44.93 ± 6.55 | 0.4732 |
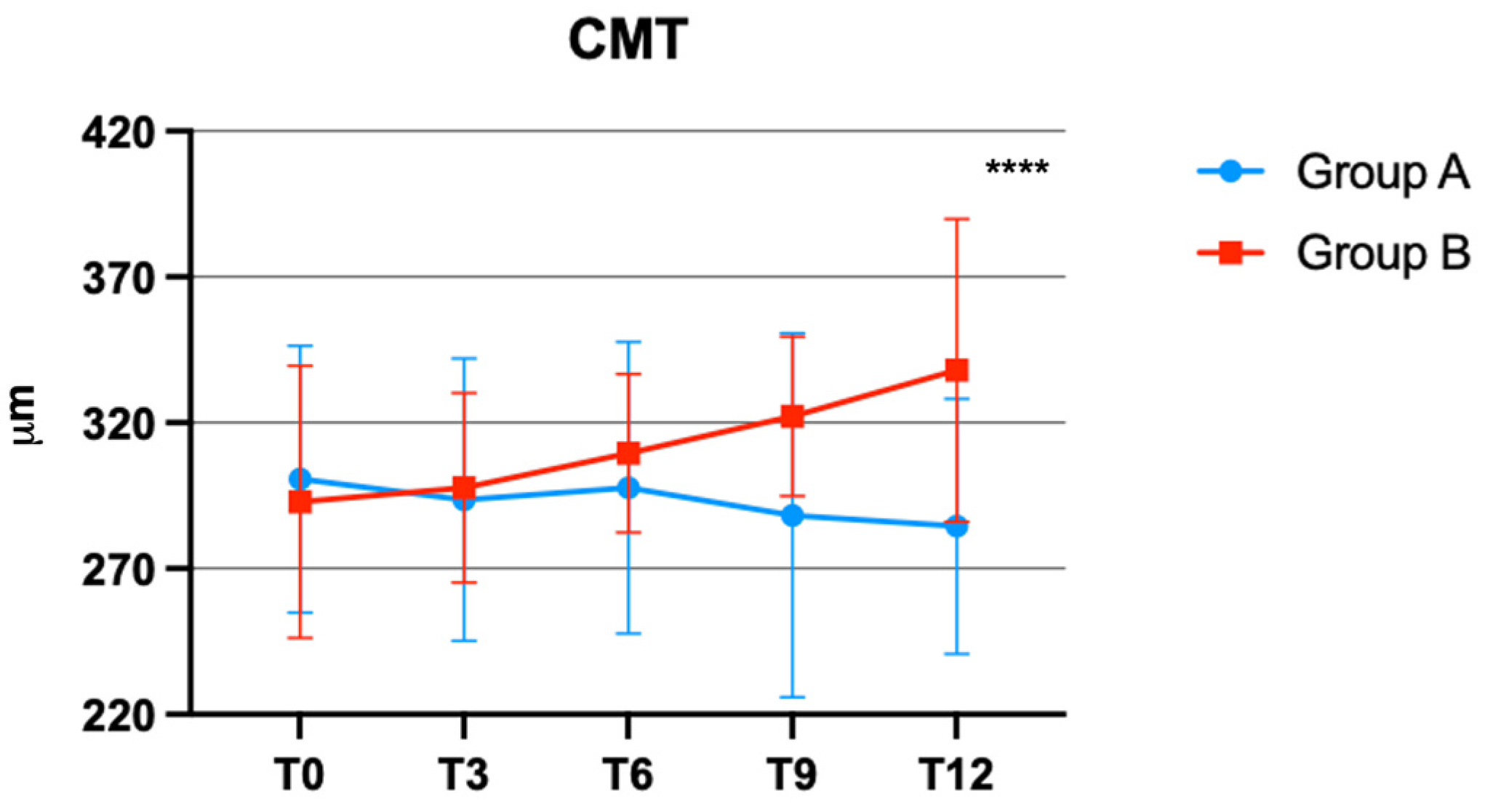
| CMT, mean ± SD, μm | 297 ± 45.61 | 300.7 ± 45.73 | 292.9 ± 46.69 | 0.6328 |
| SCP 3 × 3 whole, mean ± SD, % | 34.96 ± 3.69 | 35.00 ± 3.80 | 34.92 ± 3.68 | 0.9495 |
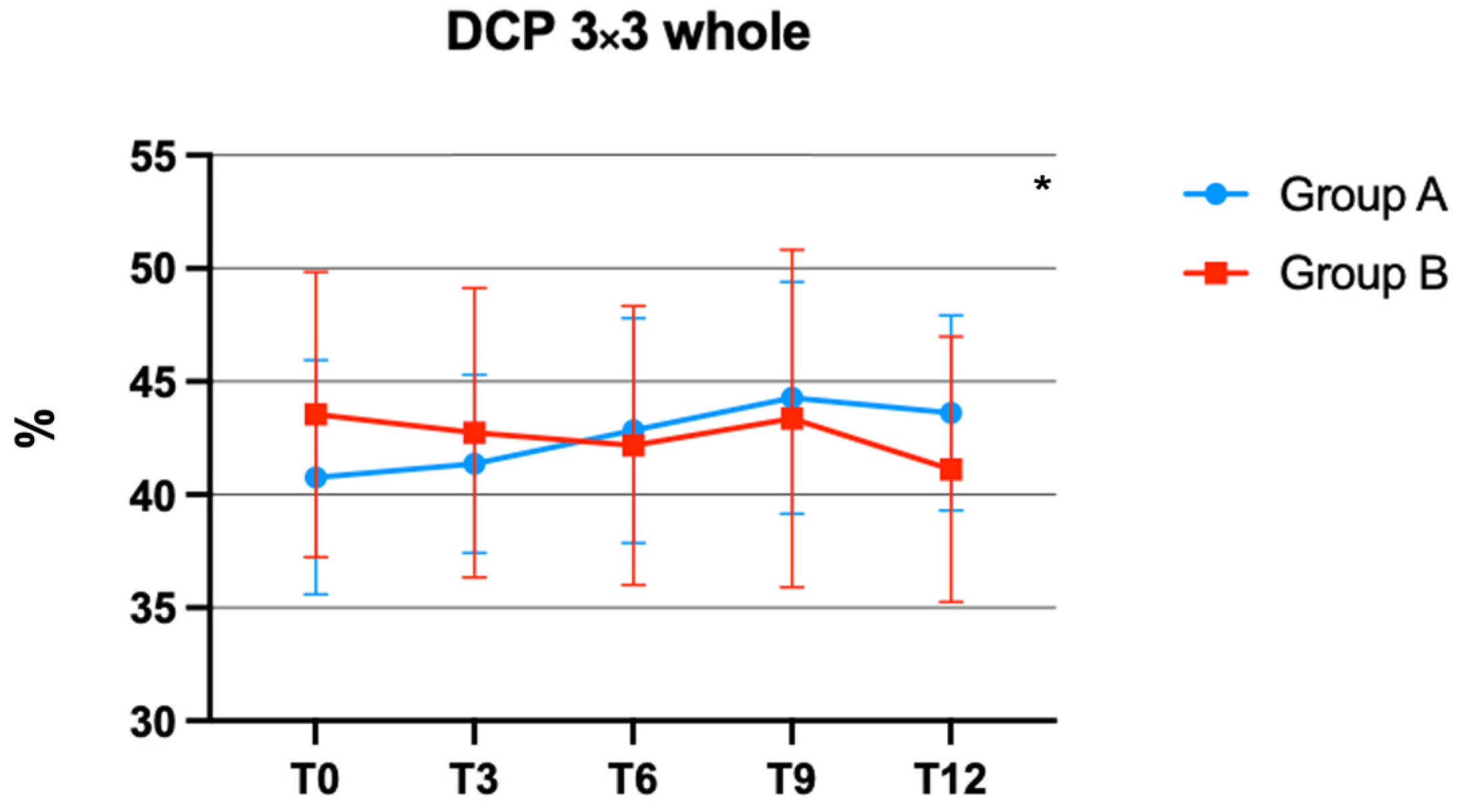
| DCP 3 × 3 whole, mean ± SD, % | 42.03 ± 5.80 | 40.77 ± 5.18 | 43.55 ± 6.30 | 0.1739 |
| Glycated hemoglobin A1c, mean ± SD, % | 6.68 ± 0.21 | 6.72 ± 0.20 | 6.63 ± 0.23 | 0.2510 |
Disclaimer/Publisher’s Note: The statements, opinions and data contained in all publications are solely those of the individual author(s) and contributor(s) and not of MDPI and/or the editor(s). MDPI and/or the editor(s) disclaim responsibility for any injury to people or property resulting from any ideas, methods, instructions or products referred to in the content. |
© 2023 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Carnevali, A.; Vaccaro, S.; Borselli, M.; Bousyf, S.; Lamonica, L.; Randazzo, G.; Giannaccare, G.; Scorcia, V. Anatomical and Functional Effects of an Oral Supplementation of Bromelain and Curcugreen in Patients with Focal Diabetic Macular Edema. J. Clin. Med. 2023, 12, 7318. https://doi.org/10.3390/jcm12237318
Carnevali A, Vaccaro S, Borselli M, Bousyf S, Lamonica L, Randazzo G, Giannaccare G, Scorcia V. Anatomical and Functional Effects of an Oral Supplementation of Bromelain and Curcugreen in Patients with Focal Diabetic Macular Edema. Journal of Clinical Medicine. 2023; 12(23):7318. https://doi.org/10.3390/jcm12237318
Chicago/Turabian StyleCarnevali, Adriano, Sabrina Vaccaro, Massimiliano Borselli, Soufiane Bousyf, Luca Lamonica, Giorgio Randazzo, Giuseppe Giannaccare, and Vincenzo Scorcia. 2023. "Anatomical and Functional Effects of an Oral Supplementation of Bromelain and Curcugreen in Patients with Focal Diabetic Macular Edema" Journal of Clinical Medicine 12, no. 23: 7318. https://doi.org/10.3390/jcm12237318
APA StyleCarnevali, A., Vaccaro, S., Borselli, M., Bousyf, S., Lamonica, L., Randazzo, G., Giannaccare, G., & Scorcia, V. (2023). Anatomical and Functional Effects of an Oral Supplementation of Bromelain and Curcugreen in Patients with Focal Diabetic Macular Edema. Journal of Clinical Medicine, 12(23), 7318. https://doi.org/10.3390/jcm12237318











