Caesarean Section for Orthopedic Indications
Abstract
1. Introduction
Physiological Adaptation of the Musculoskeletal System during Pregnancy
2. Methods
2.1. Inclusion and Exclusion Criteria and Identification of Studies
2.2. Data Extraction
3. Results
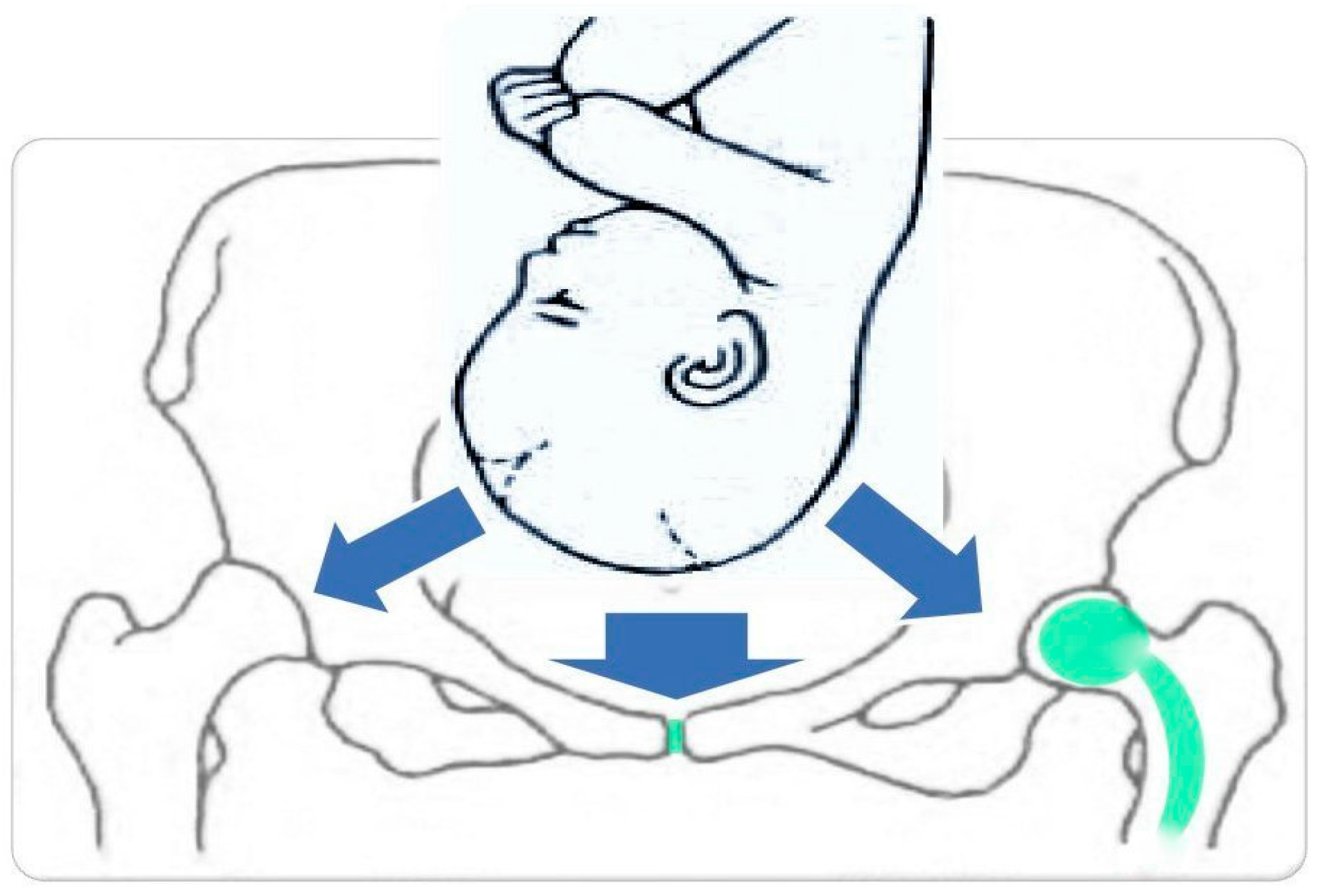
4. Postpartum Pubic Symphysis Diastasis (PPSD)
5. Lumbar Disc Herniation (LDH)
6. Status Post Hip Arthroplasty
7. Pelvic Bone Fracture
8. Limitations and Bias
9. Conclusions
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Conflicts of Interest
References
- Venturella, R.; Quaresima, P.; Micieli, M.; Rania, E.; Palumbo, A.; Visconti, F.; Zullo, F.; Di Carlo, C. Non-obstetrical indications for cesarean section: A state-of-the-art review. Arch. Gynecol. Obstet. 2018, 298, 9–16. [Google Scholar] [CrossRef] [PubMed]
- Gross, G.A.; George, J.W. Orthopedic Injury in Pregnancy. Clin. Obstet. Gynecol. 2016, 59, 629–638. [Google Scholar] [CrossRef]
- Daneau, C.; Abboud, J.; Marchand, A.-A.; Houle, M.; Pasquier, M.; Ruchat, S.-M.; Descarreaux, M. Mechanisms Underlying Lumbopelvic Pain During Pregnancy: A Proposed Model. Front. Pain Res. 2021, 2, 773988. [Google Scholar] [CrossRef]
- Heckman, J.; Sassard, R. Musculoskeletal considerations in pregnancy. J. Bone Jt. Surg. 1994, 76, 1720–1730. [Google Scholar] [CrossRef]
- Cherni, Y.; Desseauve, D.; Decatoire, A.; Veit-Rubinc, N.; Begon, M.; Pierre, F.; Fradet, L. Evaluation of ligament laxity during pregnancy. J. Gynecol. Obstet. Hum. Reprod. 2019, 48, 351–357. [Google Scholar] [CrossRef]
- Morino, S.; Ishihara, M.; Umezaki, F.; Hatanaka, H.; Yamashita, M.; Aoyama, T. Pelvic alignment changes during the perinatal period. PLoS ONE 2019, 14, e0223776. [Google Scholar] [CrossRef]
- Hernigou, P.; Jammal, S.; Pariat, J.; Flouzat-Lachaniette, C.H.; Dubory, A. Hip osteonecrosis and pregnancy in healthy women. Int. Orthop. 2017, 42, 1203–1211. [Google Scholar] [CrossRef]
- Hadji, P.; Boekhoff, J.; Hahn, M.; Hellmeyer, L.; Hars, O.; Kyvernitakis, I. Pregnancy-associated transient osteoporosis of the hip: Results of a case-control study. Arch. Osteoporos. 2017, 12, 11. [Google Scholar] [CrossRef]
- Toussia-Cohen, S.; Eshed, I.; Segal, O.; Schonfeld, M.; Meyer, R.; Axelrod, M.; Gat, I.; Dulitzky, M. Transient osteoporosis of the hip in pregnancy—A case series. J. Matern. Neonatal Med. 2023, 36, 2175659. [Google Scholar] [CrossRef]
- Thanatsis, N.; Kollia, G.; Gkliatis, J.; Decavalas, G.; Adonakis, G. Bilateral transient osteoporosis of the hip in pregnancy. J. Obstet. Gynaecol. 2017, 38, 415–416. [Google Scholar] [CrossRef]
- Quaresima, P.; Angeletti, M.; Luziatelli, D.; Luziatelli, S.; Venturella, R.; Di Carlo, C.; Bernardo, S. Pregnancy associated transient osteoporosis of the hip (PR-TOH): A non–obstetric indication to caesarean section. A case report with literature review. Eur. J. Obstet. Gynecol. Reprod. Biol. 2021, 262, 28–35. [Google Scholar] [CrossRef]
- Kwon, Y.-J.; Hyung, E.-J.; Yang, K.-H.; Lee, H.-O. How Different Modes of Child Delivery Influence Abdominal Muscle Activities in the Active Straight Leg Raise. J. Phys. Ther. Sci. 2014, 26, 1271–1274. [Google Scholar] [CrossRef][Green Version]
- Sung, J.-H.; Kang, M.; Lim, S.-J.; Choi, S.-J.; Oh, S.-Y.; Roh, C.-R. A case–control study of clinical characteristics and risk factors of symptomatic postpartum pubic symphysis diastasis. Sci. Rep. 2021, 11, 3289. [Google Scholar] [CrossRef]
- Heim, J.A.; Vang, S.; Lips, E.; Asche, S.E.; Ly, T.; Das, K. Pubic Symphysis Separation and Regression in Vaginal versus Cesarean Delivery. J. Obstet. Gynaecol. Can. 2021, 44, 42–47. [Google Scholar] [CrossRef]
- Urraca-Gesto, M.A.; Plaza-Manzano, G.; Ferragut-Garcías, A.; Pecos-Martín, D.; Gallego-Izquierdo, T.; Romero-Franco, N. Diastasis of symphysis pubis and labor: Systematic review. J. Rehabil. Res. Dev. 2015, 52, 629–640. [Google Scholar] [CrossRef]
- Shnaekel, K.L.; Magann, E.F.; Ahmadi, S. Pubic Symphysis Rupture and Separation During Pregnancy. Obstet. Gynecol. Surv. 2015, 70, 713–718. [Google Scholar] [CrossRef]
- Khorashadi, L.; Petscavage, J.M.; Richardson, M.L. Postpartum symphysis pubis diastasis. Radiol. Case Rep. 2011, 6, 542. [Google Scholar] [CrossRef]
- Nitsche, J.F.; Howell, T. Peripartum Pubic Symphysis Separation: A Case Report and Review of the Literature. Obstet. Gynecol. Surv. 2011, 66, 153–158. [Google Scholar] [CrossRef]
- Stolarczyk, A.; Stępiński, P.; Sasinowski, Ł.; Czarnocki, T.; Dębiński, M.; Maciąg, B. Peripartum Pubic Symphysis Diastasis—Practical Guidelines. J. Clin. Med. 2021, 10, 2443. [Google Scholar] [CrossRef] [PubMed]
- Norvilaite, K.; Kezeviciute, M.; Ramasauskaite, D.; Arlauskiene, A.; Bartkeviciene, D.; Uvarovas, V. Postpartum pubic symphysis diastasis-conservative and surgical treatment methods, incidence of complications: Two case reports and a review of the literature. World J. Clin. Cases 2020, 8, 110–119. [Google Scholar] [CrossRef] [PubMed]
- Nikolaou, M.; Katsafarou, M.; Papadocostakis, G.; Katasos, T. Intrapartum pubic symphysis diastasis in a primigravida woman. HJOG 2022, 21, 47–52. [Google Scholar] [CrossRef]
- Culligan, P.; Hill, S.; Heit, M. Rupture of the symphysis pubis during vaginal delivery followed by two subsequent uneventful pregnancies. Obstet. Gynecol. 2002, 100, 1114–1117. [Google Scholar] [CrossRef] [PubMed]
- Rustamova, S.; Predanic, M.; Sumersille, M.; Cohen, W.R. Changes in symphysis pubis width during labor. J. Perinat. Med. 2009, 37, 370–373. [Google Scholar] [CrossRef]
- Anastasio, M.K.; Anastasio, A.T.; Kuller, J.A. Peripartum Pubic Symphysis Diastasis. Obstet. Gynecol. Surv. 2023, 78, 369–375. [Google Scholar] [CrossRef]
- Stover, M.D.; Edelstein, A.I.; Matta, J.M. Chronic Anterior Pelvic Instability: Diagnosis and Management. J. Am. Acad. Orthop. Surg. 2017, 25, 509–517. [Google Scholar] [CrossRef]
- Chawla, J.J.; Arora, D.; Sandhu, N.; Jain, M.; Kumari, A. Pubic Symphysis Diastasis: A Case Series and Literature Review. Oman Med. J. 2017, 32, 510–514. [Google Scholar] [CrossRef]
- Capitán, B.A.; Torán, M.M. Síndrome de cauda equina en paciente embarazada con hernia de disco masiva. Rev. Española Cirugía Ortopédica Traumatol. 2017, 61, 63–65. [Google Scholar] [CrossRef]
- Croissant, K.; Pathak, S. Managing Symptomatic Severe Disc Prolapse in Pregnancy with Normal Vaginal Delivery: An MDT Approach. J. Clin. Case Rep. 2015, 5, 2. [Google Scholar] [CrossRef]
- Çevik, S.; Yılmaz, H.; Kaplan, A.; Yetkinel, S.; Evran, Ş.; Çalış, F.; Akkaya, E.; Katar, S.; Baygül, A.; Hanımoğlu, H. Association between parity and lumbar spine degenerative disorders in young women. Br. J. Neurosurg. 2019, 34, 172–175. [Google Scholar] [CrossRef]
- Cunha, C.; Silva, A.J.; Pereira, P.; Vaz, R.; Gonçalves, R.M.; Barbosa, M.A. The inflammatory response in the regression of lumbar disc herniation. Arthritis Res. Ther. 2018, 20, 251. [Google Scholar] [CrossRef] [PubMed]
- Ochi, H.; Ohno, R.; Kubota, M.; Hanyu, R.; Sakai, K.; Sugawara, Y.; Mukasa, F.; Kaneko, K. Case report: The operation for the lumbar disk herniation just after cesarean delivery in the third trimester of pregnancy. Int. J. Surg. Case Rep. 2014, 5, 1178–1182. [Google Scholar] [CrossRef]
- Paslaru, F.G.; Giovani, A.; Iancu, G.; Panaitescu, A.; Peltecu, G.; Gorgan, R.M. Methods of Delivery in Pregnant Women with Lumbar Disc Herniation: A Narrative Review of General Management and Case Report. J. Med. Life 2020, 13, 517–522. [Google Scholar] [CrossRef]
- Brown, M.D.; Levi, A.D.O. Surgery for Lumbar Disc Herniation During Pregnancy. Spine 2001, 26, 440–443. [Google Scholar] [CrossRef]
- Ahern, D.P.; Gibbons, D.; Dodds, M.; Timlin, M.; Cassidy, N.; Morris, S.; Synnott, K.; Butler, J.S. Operative Management of Perinatal Lumbar Disc Herniation and Cauda Equina Syndrome: A Case Series. Ir. Med. J. 2018, 111, 843. [Google Scholar]
- Whiles, E.; Shafafy, R.; Valsamis, E.M.; Horton, C.; Morassi, G.L.; Stokes, O.; Elsayed, S. The Management of Symptomatic Lumbar Disc Herniation in Pregnancy: A Systematic Review. Glob. Spine J. 2019, 10, 908–918. [Google Scholar] [CrossRef]
- Berkmann, S.; Fandino, J. Pregnancy and childbirth after microsurgery for lumbar disc herniation. Acta Neurochir. 2011, 154, 329–334. [Google Scholar] [CrossRef]
- Brown, M.D.; Brookfield, K.F. Lumbar disc excision and cesarean delivery during the same anesthesia: A case report. J. Bone Jt. Surg. 2004, 86, 2030–2032. [Google Scholar] [CrossRef]
- Simionescu, A.A.; Cirstoiu, M.M.; Cirstoiu, C.; Stanescu, A.M.A.; Crețu, B. Current Evidence about Developmental Dysplasia of the Hip in Pregnancy. Medicina 2021, 57, 655. [Google Scholar] [CrossRef]
- Sierra, R.J.; Trousdale, R.T.; Cabanela, M.E. Authors’ reply. J. Bone Jt. Surg. 2005, 87, 21–24. [Google Scholar] [CrossRef]
- Kuitunen, I.; Skyttä, E.T.; Artama, M.; Huhtala, H.; Eskelinen, A. No effect of delivery on total hip replacement survival: A nationwide register study in Finland. Acta Orthop. 2019, 90, 433–438. [Google Scholar] [CrossRef] [PubMed]
- Oliviero, A.; Aicale, R.; Maffulli, N. Pregnancy and parturition after hip arthroplasty. Surgeon 2022, 20, 378–382. [Google Scholar] [CrossRef]
- McDowell, C.M.; Lachiewicz, P.F. Pregnancy After Total Hip Arthroplasty. J. Bone Jt. Surg. 2001, 83, 1490–1494. [Google Scholar] [CrossRef] [PubMed]
- Kuitunen, I.; Artama, M.; Eskelinen, A.; Skyttä, E.T.; Huhtala, H.; Uotila, J. Pregnancy outcome in women after total hip replacement: A population-based study. Eur. J. Obstet. Gynecol. Reprod. Biol. 2019, 238, 143–147. [Google Scholar] [CrossRef]
- Lundin, N.; Huttunen, T.T.; E Berg, H.; Marcano, A.; Felländer-Tsai, L.; Enocson, A. Increasing incidence of pelvic and acetabular fractures. A nationwide study of 87,308 fractures over a 16-year period in Sweden. Injury 2021, 52, 1410–1417. [Google Scholar] [CrossRef] [PubMed]
- Tejwani, N.; Klifto, K.; Looze, C.; Klifto, C.S. Treatment of Pregnant Patients With Orthopaedic Trauma. J. Am. Acad. Orthop. Surg. 2017, 25, e90–e101. [Google Scholar] [CrossRef] [PubMed]
- Vallier, H.A.; Cureton, B.A.; Schubeck, D. Pregnancy Outcomes After Pelvic Ring Injury. J. Orthop. Trauma 2012, 26, 302–307. [Google Scholar] [CrossRef]
- Vaajala, M.; Kuitunen, I.; Liukkonen, R.; Ponkilainen, V.; Kekki, M.; Mattila, V.M. The rate of elective cesarean section after pelvic or hip fracture remains high even after the long-term follow-up: A nationwide register-based study in Finland. Eur. J. Obstet. Gynecol. Reprod. Biol. 2022, 277, 77–83. [Google Scholar] [CrossRef]
- Hoehmann, C.L.; Doss, W.; DeTore, S. Pelvic Ring Disruption During Childbirth: A Case Report. J. Bone Jt. Surg. 2022, 12, e21. [Google Scholar] [CrossRef]
- Riehl, J.T. Caesarean section rates following pelvic fracture: A systematic review. Injury 2014, 45, 1516–1521. [Google Scholar] [CrossRef]
- Vaajala, M.; Kuitunen, I.; Nyrhi, L.; Ponkilainen, V.; Kekki, M.; Huttunen, T.T.; Mattila, V.M. Birth rate after major trauma in fertile-aged women: A nationwide population-based cohort study in Finland. Reprod. Health 2022, 19, 73. [Google Scholar] [CrossRef]
- Na, E.D.; Baek, M.J.; Moon, J.H.; Park, C.W.; Yoon, J.; Lee, H.; Park, S.H.; Jang, J.H. Predicting mid-pelvic interspinous distance in women using height and pubic arch angle. PLoS ONE 2023, 18, e0289814. [Google Scholar] [CrossRef] [PubMed]

Disclaimer/Publisher’s Note: The statements, opinions and data contained in all publications are solely those of the individual author(s) and contributor(s) and not of MDPI and/or the editor(s). MDPI and/or the editor(s) disclaim responsibility for any injury to people or property resulting from any ideas, methods, instructions or products referred to in the content. |
© 2023 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Ziętek, M.; Ziętek, P.; Kotrych, D.; Szczuko, M. Caesarean Section for Orthopedic Indications. J. Clin. Med. 2023, 12, 7336. https://doi.org/10.3390/jcm12237336
Ziętek M, Ziętek P, Kotrych D, Szczuko M. Caesarean Section for Orthopedic Indications. Journal of Clinical Medicine. 2023; 12(23):7336. https://doi.org/10.3390/jcm12237336
Chicago/Turabian StyleZiętek, Maciej, Paweł Ziętek, Daniel Kotrych, and Małgorzata Szczuko. 2023. "Caesarean Section for Orthopedic Indications" Journal of Clinical Medicine 12, no. 23: 7336. https://doi.org/10.3390/jcm12237336
APA StyleZiętek, M., Ziętek, P., Kotrych, D., & Szczuko, M. (2023). Caesarean Section for Orthopedic Indications. Journal of Clinical Medicine, 12(23), 7336. https://doi.org/10.3390/jcm12237336





