Tacrolimus as a Promising Drug for Epistaxis and Gastrointestinal Bleeding in HHT
Abstract
:1. Introduction
2. Materials and Methods
2.1. Participants and Study Design
2.2. Study Outcomes and Evaluations
2.3. Statistical Analysis
3. Results
4. Discussion
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Acknowledgments
Conflicts of Interest
References
- Shovlin, C.L.; Guttmacher, A.E.; Buscarini, E.; Faughnan, M.E.; Hyland, R.H.; Westermann, C.J.J.; Kjeldsen, A.D.; Plauchu, H. Diagnostic criteria for Hereditary Hemorrhagic Telangiectasia (RenduOsler-Weber Syndrome). Am. J. Med. Genet. 2000, 91, 66–67. [Google Scholar] [CrossRef]
- Shovlin, C.L. Hereditary haemorrhagic telangiectasia: Pathophysiology, diagnosis and treatment. Blood Rev. 2010, 24, 203–219. [Google Scholar] [CrossRef] [PubMed]
- Shovlin, C.L. Pulmonary arteriovenous malformations. Am. J. Respir. Crit. Care Med. 2014, 190, 1217–1228. [Google Scholar] [CrossRef] [PubMed]
- Kjeldsen, A.D.; Vase, P.; Green, A. Hereditary haemorrhagic telangiectasia: A population-based study of prevalence and mortality in Danish patients. J. Intern. Med. 1999, 245, 31–39. [Google Scholar] [CrossRef] [PubMed]
- Jessurun, G.A.J.; Kamphuis, D.J.; Van der Zande, F.H.R.; Nossent, J.C. Cerebral arteriovenous malformations in the Netherlands Antilles. High prevalence of hereditary hemorrhagic telangiectasia-related single and multiple cerebral arteriovenous malformations. Clin. Neurol. Neurosurg. 1993, 95, 193–198. [Google Scholar] [CrossRef]
- McAllister, K.A.; Grogg, K.M.; Johnson, D.W.; Gallione, C.J.; Baldwin, M.A.; Jackson, C.E.; Helmbold, E.A.; Markel, D.S.; McKinnon, W.C.; Murrel, J.; et al. Endoglin, a TGF- β binding protein of endothelial cells, is the gene for hereditary haemorrhagic telangiectasia type 1. Nat. Genet. 1994, 8, 345–351. [Google Scholar] [CrossRef] [PubMed]
- Johnson, D.W.; Berg, J.N.; Baldwin, M.A.; Gallione, C.J.; Marondel, I.; Yoon, S.J.; Stenzel, T.T.; Speer, M.; Pericak-Vance, M.A.; Diamond, A.; et al. Mutations in the activin receptor-like kinase 1 gene in hereditary haemorrhagic telangiectasia type. Nat. Genet. 1996, 13, 189–195. [Google Scholar] [CrossRef] [PubMed]
- Gallione, C.J.; Repetto, G.M.; Legius, E.; Rustgi, A.K.; Schelley, S.L.; Tejpar, S.; Mitchell, G.; Drouin, É.; Westermann, C.J.J.; Marchuk, D.A. A combined syndrome of juvenile polyposis and hereditary haemorrhagic telangiectasia associated with mutations in MADH4 (SMAD4). Lancet 2004, 363, 852–859. [Google Scholar] [CrossRef]
- Duan, X.Y.; Guo, D.C.; Regalado, E.S.; Shen, H.; Coselli, J.S.; Estrera, A.L.; Safi, H.J.; Bamshad, M.J.; Nickerson, D.A.; LeMaire, S.A.; et al. SMAD4 rare variants in individuals and families with thoracic aortic aneurysms and dissections. Eur. J. Hum. Genet. 2019, 27, 1054–1060. [Google Scholar] [CrossRef]
- Cole, S.G.; Begbie, M.E.; Wallace, G.M.F.; Shovlin, C.L.L. A new locus for hereditary haemorrhagic telangiectasia (HHT3) maps to chromosome 5. J. Med. Genet. 2005, 42, 577–582. [Google Scholar] [CrossRef]
- Bayrak-Toydemir, P.; McDonald, J.; Akarsu, N.; Toydemir, R.M.; Calderon, F.; Tuncali, T.; Tang, W.; Miller, F.; Mao, R. A fourth locus for hereditary hemorrhagic telangiectasia maps to chromosome 7. Am. J. Med. Genet. 2006, 140, 2155–2162. [Google Scholar] [CrossRef] [PubMed]
- Wooderchak-Donahue, W.L.; McDonald, J.; O’Fallon, B.; Upton, P.D.; Li, W.; Roman, B.L.; Young, S.; Plant, P.; Fülöp, G.T.; Langa, C.; et al. BMP9 mutations cause a vascular-anomaly syndrome with phenotypic overlap with hereditary hemorrhagic telangiectasia. Am. J. Hum. Genet. 2013, 93, 530–537. [Google Scholar] [CrossRef] [PubMed]
- Morales-Angulo, C.; Del Valle-Zapico, A. Hereditary hemorrhagic telangiectasia. Otolaryngol. Head Neck Surg. 1998, 119, 293. [Google Scholar] [PubMed]
- Assar, O.S.; Friedman, C.M.; White, R.I. The Natural History of Epistaxis in Hereditary Hemorrhagic Telangiectasia. Laryngoscope 1991, 101, 977–980. [Google Scholar] [CrossRef]
- Geisthoff, U.W.; Schneider, G.; Fischinger, J.; Plinkert, P.K. Hereditäre hämorrhagische teleangiektasie (Morbus Osler). Eine interdisziplinäre herausforderung. HNO 2002, 50, 114–128. [Google Scholar] [CrossRef] [PubMed]
- Ingrosso, M.; Sabbà, C.; Pisani, A.; Principi, M.; Gallitelli, M.; Cirulli, A.; Francavilla, A. Evidence of small-bowel involvement in hereditary hemorrhagic telangiectasia: A capsule-endoscopic study. Endoscopy 2004, 36, 1074–1079. [Google Scholar] [CrossRef]
- Vase, P.; Grove, O. Gastrointestinal Lesions in Hereditary Hemorrhagic Telangiectasia. Gastroenterology 1986, 91, 1079–1083. [Google Scholar] [CrossRef]
- Skaro, A.I.; Marotta, P.J. Regression of cutaneous and gastrointestinal telangiectasia with sirolimus and aspirin in a patient with hereditary hemorrhagic telangiectasia. Ann. Intern. Med. 2006, 144, 226–227. [Google Scholar]
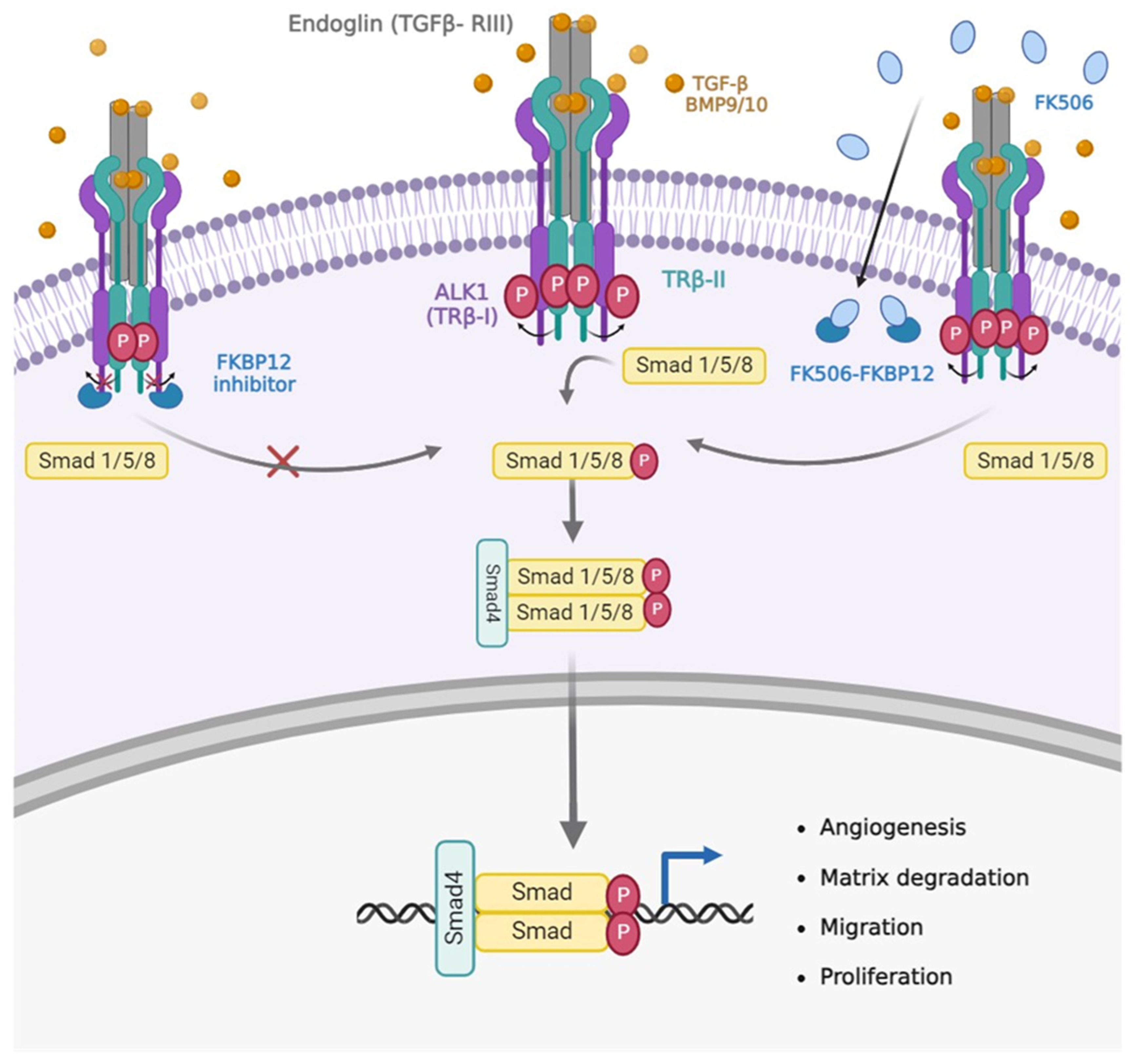
- Albiñana, V.; Sanz-Rodríguez, F.; Recio-Poveda, L.; Bernabéu, C.; Botella, L.M. Immunosuppressor FK506 increases endoglin and activin receptor-like kinase 1 expression and modulates transforming growth factor- β1 signaling in endothelial cells. Mol. Pharmacol. 2011, 79, 833–843. [Google Scholar] [CrossRef]
- Albiñana, V.; Velasco, L.; Zarrabeitia, R.; Botella, L.M. Tacrolimus as a therapeutic drug in hereditary hemorrhagic telangiectasia (HHT). In Tacrolimus: Effectiveness, Safety and Drug Interactions; Nova Science Publishers: Hauppauge, NY, USA, 2013; pp. 163–172. ISBN 9781628083668. [Google Scholar]
- Ruiz, S.; Chandakkar, P.; Zhao, H.; Papoin, J.; Chatterjee, P.K.; Christen, E.; Metz, C.N.; Blanc, L.; Campagne, F.; Marambaud, P. Tacrolimus rescues the signaling and gene expression signature of endothelial ALK1 loss-of-function and improves HHT vascular pathology. Hum. Mol. Genet. 2017, 26, 4786–4798. [Google Scholar] [CrossRef]
- Ruiz, S.; Zhao, H.; Chandakkar, P.; Papoin, J.; Choi, H.; Nomura-Kitabayashi, A.; Patel, R.; Gillen, M.; Diao, L.; Chatterjee, P.; et al. Correcting Smad1/5/8, mTOR, and VEGFR2 treats pathology in hereditary hemorrhagic telangiectasia models. J. Clin. Investig. 2020, 130, 942–957. [Google Scholar] [CrossRef] [PubMed]
- Dupuis-Girod, S.; Fargeton, A.E.; Grobost, V.; Rivière, S.; Beaudoin, M.; Decullier, E.; Bernard, L.; Bréant, V.; Colombet, B.; Philouze, P.; et al. Efficacy and Safety of a 0.1% Tacrolimus Nasal Ointment as a Treatment for Epistaxis in Hereditary Hemorrhagic Telangiectasia: A Double-Blind, Randomized, Placebo-Controlled, Multicenter Trial. J. Clin. Med. 2020, 9, 1262. [Google Scholar] [CrossRef] [PubMed]
- Hoag, J.B.; Terry, P.; Mitchell, S.; Reh, D.; Merlo, C.A. An epistaxis severity score for hereditary hemorrhagic telangiectasia. Laryngoscope 2010, 120, 838–843. [Google Scholar] [CrossRef]
- Peterson, A.M.; Kallogjeri, D.; Spitznagel, E.; Chakinala, M.M.; Schneider, J.S.; Piccirillo, J.F. Development and Validation of the Nasal Outcome Score for Epistaxis in Hereditary Hemorrhagic Telangiectasia (NOSE HHT). JAMA Otolaryngol. Head Neck Surg. 2020, 146, 999–1005. [Google Scholar] [CrossRef]
- Albiñana, V.; Cuesta, A.M.; Rojas-P, I.; Gallardo-Vara, E.; Recio-Poveda, L.; Bernabéu, C.; Botella, L.M. Review of Pharmacological Strategies with Repurposed Drugs for Hereditary Hemorrhagic Telangiectasia Related Bleeding. J. Clin. Med. 2020, 9, 1766. [Google Scholar] [CrossRef] [PubMed]
- Sommer, N.; Droege, F.; Gamen, K.E.; Geisthoff, U.; Gall, H.; Tello, K.; Richter, M.J.; Deubner, L.M.; Schmiedel, R.; Hecker, M.; et al. Treatment with low-dose tacrolimus inhibits bleeding complications in a patient with hereditary hemorrhagic telangiectasia and pulmonary arterial hypertension. Pulm. Circ. 2019, 9, 2045894018805406. [Google Scholar] [CrossRef] [PubMed]
- Hosman, A.; Kroon, S.; Vorselaars, V.; Doef, H.; Post, M.; Snijder, R.; Mager, J. Tacrolimus treatment for two rare complications caused by hereditary haemorrhagic telangiectasia: A description of two cases. Angiogenesis 2019, 22, 629. [Google Scholar]
- Hessels, J.; Kroon, S.; Boerman, S.; Nelissen, R.C.; Grutters, J.C.; Snijder, R.J.; Lebrin, F.; Post, M.C.; Mummery, C.L.; Mager, J.-J. Efficacy and Safety of Tacrolimus as Treatment for Bleeding Caused by Hereditary Hemorrhagic Telangiectasia: An Open-Label, Pilot Study. J. Clin. Med. 2022, 11, 5280. [Google Scholar] [CrossRef] [PubMed]
- Guilhem, A.; Malcus, C.; Clarivet, B.; Plauchu, H.; Dupuis-Girod, S. Immunological abnormalities associated with hereditary haemorrhagic telangiectasia. J. Intern. Med. 2013, 274, 351–362. [Google Scholar] [CrossRef]
- Droege, F.; Pylaeva, E.; Siakaeva, E.; Bordbari, S.; Spyra, I.; Thangavelu, K.; Lueb, C.; Domnich, M.; Lang, S.; Geisthoff, U.; et al. Impaired Release of Neutrophil Extracellular Traps and Anemia-Associated T Cell Deficiency in Hereditary Hemorrhagic Telangiectasia. J. Clin. Med. 2020, 9, 767. [Google Scholar] [CrossRef]
- Amati, L.; Passeri, M.E.; Resta, F.; Triggiani, V.; Jirillo, E.; Sabbà, C. Ablation of T-helper 1 cell derived cytokines and of monocyte-derived tumor necrosis factor-alpha in hereditary hemorrhagic telangiectasia: Immunological consequences and clinical considerations. Curr. Pharm. Des. 2006, 12, 1201–1208. [Google Scholar] [PubMed]

| Patient | Dose | Start | End | Tolerance | Sex | Age | Genetics | ESS Pre | ESS Post | Hb before (g/dL) | Hb upon Treatment (g/dL) | Epistaxis, Telangiectasis | Internal Arteriovenous Malformations | Previous Procedures | Previous Drugs | ||
|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|
| P1 | 1 mg/24 h | 2019 | - | Good | F | 61 | Unknown | 7.5 | 6.15 | 9.1 | 12.3 | Yes | - | HAVMs | CAVM | Embolization right and left external carotid artery branches | Propranolol, raloxifen. IV iron |
| P2 | 1 mg/24 h | 2019 | 2020 | Good | M | 61 | ACVRL1/ALK-1 c.1208T > C p.L403P Missense | 4.2 | 2.42 | 12 | 15.3 | Yes | GI AVMs | HAVMs | - | - | Propranolol, bevacizumab IV iron |
| P3 | 1 mg/24 h | 2019 | - | Good | F | 64 | ENG c360 + 1G > A | 4 | 2.9 | 10.2 | 14.1 | Yes | GI AVMs | HAVM (arterio-portal), (Portal Hypertension) | PAVMs. CAVMs. Anemia | Nasal sclerosis Pulmonar embolization | Amchafibrin. Octeotride and oral tamoxifene |
| P4 | 0.5 mg/24 h | 2019 | - | Good | F | 54 | unknown | 5.9 | 2.1 | 8.7 | 11.2 | Yes | - | HAVMs | Anemia | Nasal sclerosis | Propranolol, amchafibrin. Oral iron |
| P5 | 0.5 mg/24 h | 2019 | 2021 | Digestive Intolerant | M | 55 | unknown | 7.1 | 3.5 | 8.3 | 13.6 | Yes | - | HAVMs | PAVMs | - | IV iron |
| P6 | 1 mg/24 h | 2018 | - | Good | M | 64 | Not found in ENG. ALK1/ACVRL1 | 6.2 | 3.3 | 7.1 | 11 | Yes | - | - | GI AVMs Anemia | Laser for GI AVMs. | IV iron |
| P7 | 1 mg/12 h | 2018 | 2020 | Digestive Intolerant | M | 65 | ENG c.663C > G p.W221X nonsense | 4.2 | 2.1 | 13.8 | 11.5 | Yes | - | - | - | Inner Maxilar Artery embolization. Young procedure. Sphenopalatine artery embolization.Nasal sclerosis | Amchafibrin Oral iron, blood transfusions, 5 Bevacizumab cycles in 2017 |
| P8 | 1.5 mg/24 h | 2018 | - | Good | M | 27 | ACVRL1/ALK1. Intron 9 c.1377 + 45T > C & c.1377 + 65A > G | 0 | 0 | 13.9 | 15.6 | Yes | Buccal AVMs | - | - | Nasal Sclerosis | Propranolol |
| P9 | 0.5 mg/12 h | 2018 | - | Good | F | 51 | ENG/HHT1 | 7.1 | 2.1 | 10.5 | 15 | Yes | PAVMs | - | Anemia | Nasal Sclerosis | Amchafibrin blood Transfusions |
| P10 | 0.5 mg/12 h | 2021 | - | Good | F | 47 | ACVRL1/ALK1 ex 8 c.1129 G > A p.A377T | 8 | 6.1 | 7.2 | 14.6 | Yes | - | - | Anemia | Nasal Sclerosis | Oral iron |
| P11 | 1 mg/12 h | 2018 | - | Good | M | 65 | ENG ex 5 c.646 A > G p.K216Q | 10 | 3.3 | 4.9 | 10.5 | Yes | GI AVM | - | Anemia | Nasal Sclerosis | - |
Disclaimer/Publisher’s Note: The statements, opinions and data contained in all publications are solely those of the individual author(s) and contributor(s) and not of MDPI and/or the editor(s). MDPI and/or the editor(s) disclaim responsibility for any injury to people or property resulting from any ideas, methods, instructions or products referred to in the content. |
© 2023 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Álvarez-Hernández, P.; Patier, J.L.; Marcos, S.; Gómez del Olmo, V.; Lorente-Herraiz, L.; Recio-Poveda, L.; Botella, L.M.; Viteri-Noël, A.; Albiñana, V. Tacrolimus as a Promising Drug for Epistaxis and Gastrointestinal Bleeding in HHT. J. Clin. Med. 2023, 12, 7410. https://doi.org/10.3390/jcm12237410
Álvarez-Hernández P, Patier JL, Marcos S, Gómez del Olmo V, Lorente-Herraiz L, Recio-Poveda L, Botella LM, Viteri-Noël A, Albiñana V. Tacrolimus as a Promising Drug for Epistaxis and Gastrointestinal Bleeding in HHT. Journal of Clinical Medicine. 2023; 12(23):7410. https://doi.org/10.3390/jcm12237410
Chicago/Turabian StyleÁlvarez-Hernández, Paloma, José Luis Patier, Sol Marcos, Vicente Gómez del Olmo, Laura Lorente-Herraiz, Lucía Recio-Poveda, Luisa María Botella, Adrián Viteri-Noël, and Virginia Albiñana. 2023. "Tacrolimus as a Promising Drug for Epistaxis and Gastrointestinal Bleeding in HHT" Journal of Clinical Medicine 12, no. 23: 7410. https://doi.org/10.3390/jcm12237410
APA StyleÁlvarez-Hernández, P., Patier, J. L., Marcos, S., Gómez del Olmo, V., Lorente-Herraiz, L., Recio-Poveda, L., Botella, L. M., Viteri-Noël, A., & Albiñana, V. (2023). Tacrolimus as a Promising Drug for Epistaxis and Gastrointestinal Bleeding in HHT. Journal of Clinical Medicine, 12(23), 7410. https://doi.org/10.3390/jcm12237410







