A Modified Technique for Transcatheter Pulmonary Valve Implantation of SAPIEN 3 Valves in Large Right Ventricular Outflow Tract: A Matched Comparison Study
Abstract
:1. Introduction
2. Methods
2.1. Study Design
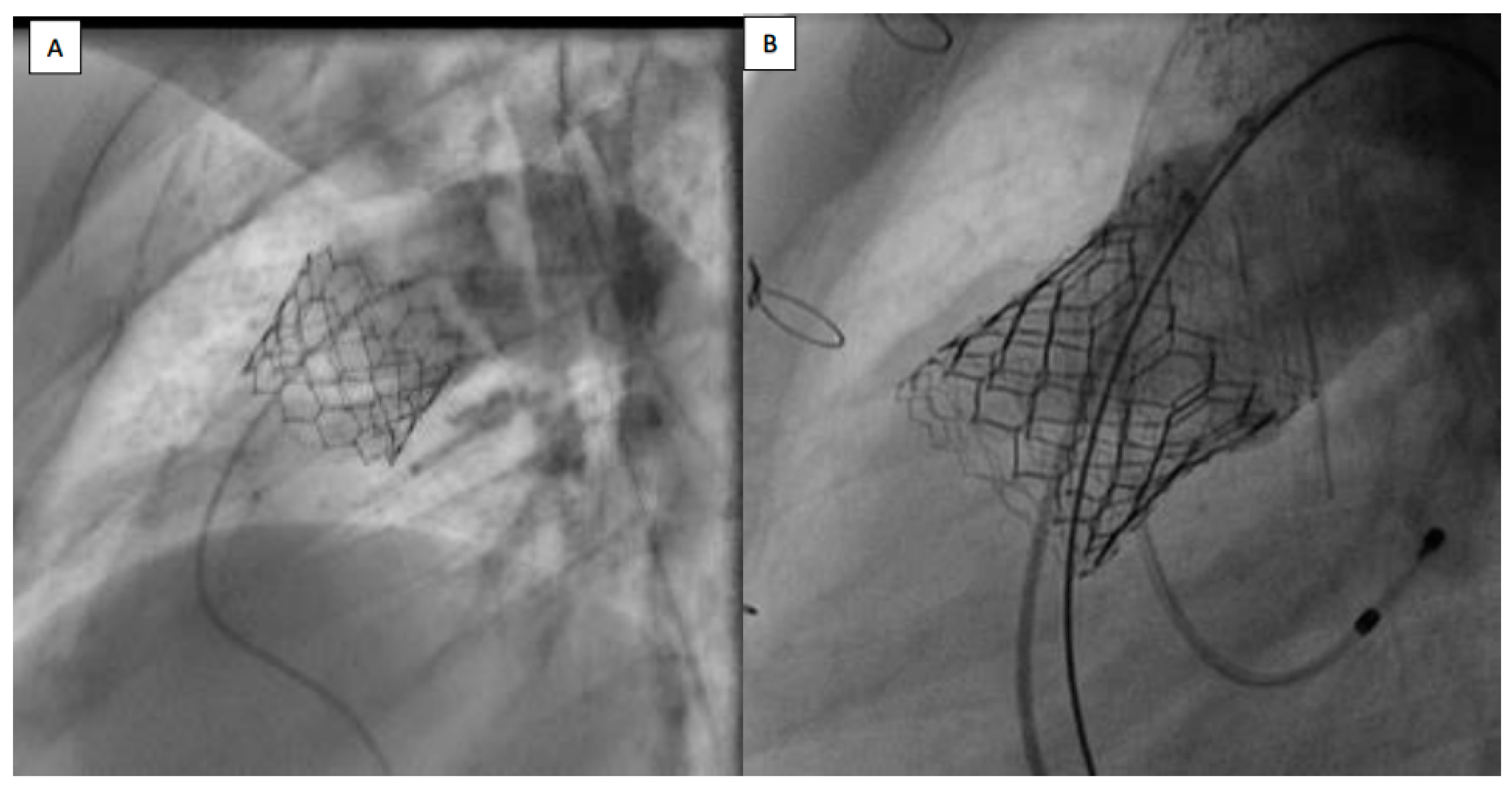
2.2. Percutaneous Pulmonary Valve Implantation Protocol
2.3. Statistical Analysis
3. Results
3.1. Patients’ Selection
3.2. Baseline Characteristics
3.3. Procedures
3.4. Procedure Efficacy
3.5. Procedure Safety
3.6. Procedure Cost
3.7. Follow-Up
4. Discussion
5. Conclusions
Supplementary Materials
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Conflicts of Interest
References
- Bonhoeffer, P.; Boudjemline, Y.; Saliba, Z.; Merckx, J.; Aggoun, Y.; Bonnet, D.; Acar, P.; Le Bidois, J.; Sidi, D.; Kachaner, J. Percutaneous replacement of pulmonary valve in a right-ventricle to pulmonary-artery prosthetic conduit with valve dysfunction. Lancet 2000, 356, 1403–1405. [Google Scholar] [CrossRef]
- Cabalka, A.K.; Hellenbrand, W.E.; Eicken, A.; Kreutzer, J.; Gray, R.G.; Bergersen, L.; Berger, F.; Armstrong, A.K.; Cheatham, J.P.; Zahn, E.M.; et al. Relationships Among Conduit Type, Pre-Stenting, and Outcomes in Patients Undergoing Transcatheter Pulmonary Valve Replacement in the Prospective North American and European Melody Valve Trials. JACC Cardiovasc. Interv. 2017, 10, 1746–1759. [Google Scholar] [CrossRef]
- Haas, N.A.; Moysich, A.; Neudorf, U.; Mortezaeian, H.; Abdel-Wahab, M.; Schneider, H.; De Wolf, D.; Petit, J.; Narayanswami, S.; Laser, K.T.; et al. Percutaneous implantation of the Edwards SAPIEN() pulmonic valve: Initial results in the first 22 patients. Clin. Res. Cardiol. 2013, 102, 119–128. [Google Scholar] [CrossRef]
- Haas, N.A.; Carere, R.G.; Kretschmar, O.; Horlick, E.; Rodes-Cabau, J.; de Wolf, D.; Gewillig, M.; Mullen, M.; Lehner, A.; Deutsch, C.; et al. Early outcomes of percutaneous pulmonary valve implantation using the Edwards SAPIEN XT transcatheter heart valve system. Int. J. Cardiol. 2018, 250, 86–91. [Google Scholar] [CrossRef]
- Kenny, D.; Hijazi, Z.M.; Kar, S.; Rhodes, J.; Mullen, M.; Makkar, R.; Shirali, G.; Fogel, M.; Fahey, J.; Heitschmidt, M.G.; et al. Percutaneous implantation of the Edwards SAPIEN transcatheter heart valve for conduit failure in the pulmonary position: Early phase 1 results from an international multicenter clinical trial. J. Am. Coll. Cardiol. 2011, 58, 2248–2256. [Google Scholar] [CrossRef]
- Boone, R.H.; Webb, J.G.; Horlick, E.; Benson, L.; Cao, Q.L.; Nadeem, N.; Kiess, M.; Hijazi, Z.M. Transcatheter pulmonary valve implantation using the Edwards SAPIEN transcatheter heart valve. Catheter. Cardiovasc. Interv. 2010, 75, 286–294. [Google Scholar] [CrossRef]
- Faccini, A.; Butera, G. Tricuspid regurgitation as a complication of Edwards Sapien XT valve implantation in pulmonary position a problem to deal with. Catheter. Cardiovasc. Interv. 2018, 91, 927–931. [Google Scholar] [CrossRef]
- Karsenty, C.; Malekzadeh-Milani, S.; Fraisse, A.; Gewillig, M.; Bonnet, D.; Aldebert, P.; Ovaert, C.; Bouvaist, H.; Kempny, A.; Houeijeh, A.; et al. Right ventricular outflow tract prestenting with AndraStent XXL before percutaneous pulmonary valve implantation. Arch. Cardiovasc. 2020, 113, 113–120. [Google Scholar] [CrossRef] [PubMed]
- Ghobrial, J.; Levi, D.S.; Aboulhosn, J. Native Right Ventricular Outflow Tract Transcatheter Pulmonary Valve Replacement Without Pre-Stenting. JACC Cardiovasc. Interv. 2018, 11, e41–e44. [Google Scholar] [CrossRef] [PubMed]
- Morgan, G.J.; Sadeghi, S.; Salem, M.M.; Wilson, N.; Kay, J.; Rothman, A.; Galindo, A.; Martin, M.H.; Gray, R.; Ross, M.; et al. SAPIEN valve for percutaneous transcatheter pulmonary valve replacement without "pre-stenting": A multi-institutional experience. Catheter. Cardiovasc. Interv. 2019, 93, 324–329. [Google Scholar] [CrossRef] [PubMed]
- Hascoet, S.; Karsenty, C.; Tortigue, M.; Watkins, A.C.; Riou, J.Y.; Boet, A.; Tahhan, N.; Fabre, D.; Haulon, S.; Brenot, P.; et al. A modified procedure for percutaneous pulmonary valve implantation of the Edwards SAPIEN 3 valve. EuroIntervention J. EuroPCR Collab. Work. Group Interv. Cardiol. Eur. Soc. Cardiol. 2019, 14, 1386–1388. [Google Scholar] [CrossRef]
- Stout, K.K.; Daniels, C.J.; Aboulhosn, J.A.; Bozkurt, B.; Broberg, C.S.; Colman, J.M.; Crumb, S.R.; Dearani, J.A.; Fuller, S.; Gurvitz, M.; et al. 2018 AHA/ACC Guideline for the Management of Adults With Congenital Heart Disease: Executive Summary: A Report of the American College of Cardiology/American Heart Association Task Force on Clinical Practice Guidelines. J. Am. Coll. Cardiol. 2019, 73, 1494–1563. [Google Scholar] [CrossRef]
- Baumgartner, H.; De Backer, J.; Babu-Narayan, S.V.; Budts, W.; Chessa, M.; Diller, G.P.; Lung, B.; Kluin, J.; Lang, I.M.; Meijboom, F.; et al. 2020 ESC Guidelines for the management of adult congenital heart disease. Eur. Heart J. 2021, 42, 563–645. [Google Scholar] [CrossRef]
- Hascoet, S.; Dalla Pozza, R.; Bentham, J.; Carere, R.G.; Kanaan, M.; Ewert, P.; Biernacka, E.K.; Kretschmar, O.; Deutsch, C.; Lecerf, F.; et al. Early outcomes of percutaneous pulmonary valve implantation using the Edwards SAPIEN 3 transcatheter heart valve system. EuroIntervention J. EuroPCR Collab. Work. Group Interv. Cardiol. Eur. Soc. Cardiol. 2019, 14, 1378–1385. [Google Scholar]
- Lehner, A.; Dashkalova, T.; Ulrich, S.; Fernandez Rodriguez, S.; Mandilaras, G.; Jakob, A.; Dalla-Pozza, R.; Fischer, M.; Schneider, H.; Tarusinov, G.; et al. Intermediate outcomes of transcatheter pulmonary valve replacement with the Edwards Sapien 3 valve—German experience. Expert Rev. Med. Devices 2019, 16, 829–834. [Google Scholar] [CrossRef] [PubMed]
- Shahanavaz, S.; Zahn, E.M.; Levi, D.S.; Aboulhousn, J.A.; Hascoet, S.; Qureshi, A.M.; Porras, D.; Morgan, G.J.; Bauser Heaton, H.; Martin, M.H.; et al. Transcatheter Pulmonary Valve Replacement With the Sapien Prosthesis. J. Am. Coll. Cardiol. 2020, 76, 2847–2858. [Google Scholar] [CrossRef]
- Houeijeh, A.; Petit, J.; Isorni, M.A.; Sigal-Cinqualbre, A.; Batteux, C.; Karsenty, C.; Fraisse, A.; Fournier, E.; Ciobotaru, V.; Hascoet, S. 3D modeling and printing in large native right ventricle outflow tract to plan complex percutaneous pulmonary valve implantation. Int. J. Cardiol. Congenit. Heart Dis. 2021, 4, 100161. [Google Scholar] [CrossRef]
- Cardoso, R.; Ansari, M.; Garcia, D.; Sandhu, S.; Brinster, D.; Piazza, N. Prestenting for prevention of melody valve stent fractures: A systematic review and meta-analysis. Catheter. Cardiovasc. Interv. 2016, 87, 534–539. [Google Scholar] [CrossRef] [PubMed]
- McElhinney, D.B.; Cheatham, J.P.; Jones, T.K.; Lock, J.E.; Vincent, J.A.; Zahn, E.M.; Hellenbrand, W.E. Stent fracture, valve dysfunction, and right ventricular outflow tract reintervention after transcatheter pulmonary valve implantation: Patient-related and procedural risk factors in the US Melody Valve Trial. Circ. Cardiovasc. Interv. 2011, 4, 602–614. [Google Scholar] [CrossRef]
- Le Ruz, R.; Plessis, J.; Houeijeh, A.; Baruteau, A.E.; Le Gloan, L.; Warin Fresse, K.; Karsenty, C.; Petit, J.; Godart, F.; Hascoet, S.; et al. Edwards SAPIEN XT transcatheter pulmonary valve implantation: 5-year follow-up in a French Registry. Catheter. Cardiovasc. Interv. 2021, 98, 990–999. [Google Scholar] [CrossRef]
- Sinha, S.; Aboulhosn, J.; Asnes, J.; Bocks, M.; Zahn, E.; Goldstein, B.H.; Zampi, J.; Hellenbrand, W.; Salem, M.; Levi, D. Initial results from the off-label use of the SAPIEN S3 valve for percutaneous transcatheter pulmonary valve replacement: A multi-institutional experience. Catheter. Cardiovasc. Interv. 2019, 93, 455–463. [Google Scholar] [CrossRef]
- Schievano, S.; Taylor, A.M.; Capelli, C.; Lurz, P.; Nordmeyer, J.; Migliavacca, F.; Bonhoeffer, P. Patient specific finite element analysis results in more accurate prediction of stent fractures: Application to percutaneous pulmonary valve implantation. J. Biomech. 2010, 43, 687–693. [Google Scholar] [CrossRef] [PubMed]
- Caimi, A.; Sturla, F.; Pluchinotta, F.R.; Giugno, L.; Secchi, F.; Votta, E.; Carminati, M.; Redaelli, A. Prediction of stenting related adverse events through patient-specific finite element modelling. J. Biomech. 2018, 79, 135–146. [Google Scholar] [CrossRef] [PubMed]
- Tengler, A.; Ulrich, S.; Fischer, M.; Pastor-Villaescusa, B.; Kanaan, M.; Pozza, R.D.; Haas, N.A.; Jakob, A. Rationale and feasibility of transcatheter pulmonary valve implantation in small conduits with the Edwards Sapien valves. Int. J. Cardiol. 2021, 325, 45–50. [Google Scholar] [CrossRef]
- Ebel, S.; Gottschling, S.; Buzan, M.T.A.; Grothoff, M.; Dahnert, I.; Wagner, R.; Grafe, D.; Lurz, P.; Gutberlet, M.; Lucke, C. 3D-assessment of RVOT dimensions prior percutaneous pulmonary valve implantation: Comparison of contrast-enhanced magnetic resonance angiography versus 3D steady-state free precession sequence. Int. J. Cardiovasc. Imaging 2019, 35, 1453–1463. [Google Scholar] [CrossRef]
- Malekzadeh-Milani, S.; Ladouceur, M.; Cohen, S.; Iserin, L.; Boudjemline, Y. Results of transcatheter pulmonary valvulation in native or patched right ventricular outflow tracts. Arch. Cardiovasc. Dis. 2014, 107, 592–598. [Google Scholar] [CrossRef]
- Gillespie, M.J.; Benson, L.N.; Bergersen, L.; Bacha, E.A.; Cheatham, S.L.; Crean, A.M.; Eicken, A.; Ewert, P.; Geva, T.; Hellenbrand, W.E.; et al. Patient Selection Process for the Harmony Transcatheter Pulmonary Valve Early Feasibility Study. Am. J. Cardiol. 2017, 120, 1387–1392. [Google Scholar] [CrossRef]
- Bergersen, L.; Benson, L.N.; Gillespie, M.J.; Cheatham, S.L.; Crean, A.M.; Hor, K.N.; Horlick, E.M.; Lung, T.H.; McHenry, B.T.; Osten, M.D.; et al. Harmony Feasibility Trial: Acute and Short-Term Outcomes With a Self-Expanding Transcatheter Pulmonary Valve. JACC Cardiovasc. Interv. 2017, 10, 1763–1773. [Google Scholar] [CrossRef]
- Lee, S.Y.; Kim, G.B.; Kim, S.H.; Jang, S.I.; Choi, J.Y.; Kang, I.S.; Kim, Y.H. Mid-term outcomes of the Pulsta transcatheter pulmonary valve for the native right ventricular outflow tract. Catheter. Cardiovasc. Interv. 2021, 98, E724–E732. [Google Scholar] [CrossRef] [PubMed]
- Kim, A.Y.; Jung, J.W.; Jung, S.Y.; Shin, J.I.; Eun, L.Y.; Kim, N.K.; Choi, J.Y. Early Outcomes of Percutaneous Pulmonary Valve Implantation with Pulsta and Melody Valves: The First Report from Korea. J. Clin. Med. 2020, 9, 2769. [Google Scholar] [CrossRef]
- Kim, G.B.; Song, M.K.; Bae, E.J.; Park, E.A.; Lee, W.; Lim, H.G.; Kim, Y.J. Successful Feasibility Human Trial of a New Self-Expandable Percutaneous Pulmonary Valve (Pulsta Valve) Implantation Using Knitted Nitinol Wire Backbone and Trileaflet alpha-Gal-Free Porcine Pericardial Valve in the Native Right Ventricular Outflow Tract. Circ. Cardiovasc. Interv. 2018, 11, e006494. [Google Scholar] [CrossRef] [PubMed]
- Morgan, G.; Prachasilchai, P.; Promphan, W.; Rosenthal, E.; Sivakumar, K.; Kappanayil, M.; Sakidjan, I.; Walsh, K.P.; Kenny, D.; Thomson, J.; et al. Medium-term results of percutaneous pulmonary valve implantation using the Venus P-valve: International experience. EuroIntervention J. EuroPCR Collab. Work. Group Interv. Cardiol. Eur. Soc. Cardiol. 2019, 14, 1363–1370. [Google Scholar] [CrossRef] [PubMed]
- Riahi, M.; Ang, H.L.; Jones, M.; Prachasilchai, P.; Baruteau, A.E.; Promphan, W.; Rosenthal, E.; Qureshi, S.A. Infolding of the Venus P-Valve After Transcatheter Pulmonary Valve Implantation. Circ. Cardiovasc. Interv. 2018, 11, e005923. [Google Scholar] [CrossRef] [PubMed]
- Garay, F.; Pan, X.; Zhang, Y.J.; Wang, C.; Springmuller, D. Early experience with the Venus pvalve for percutaneous pulmonary valve implantation in native outflow tract. Neth. Heart J. Mon. J. Neth. Soc. Cardiol. Neth. Heart Found. 2017, 25, 76–81. [Google Scholar]
- Promphan, W.; Prachasilchai, P.; Siripornpitak, S.; Qureshi, S.A.; Layangool, T. Percutaneous pulmonary valve implantation with the Venus P-valve: Clinical experience and early results. Cardiol. Young 2016, 26, 698–710. [Google Scholar] [CrossRef]
- Husain, J.; Praichasilchai, P.; Gilbert, Y.; Qureshi, S.A.; Morgan, G.J. Early European experience with the Venus P-valve(R): Filling the gap in percutaneous pulmonary valve implantation. EuroIntervention J. EuroPCR Collab. Work. Group Interv. Cardiol. Eur. Soc. Cardiol. 2016, 12, e643–e651. [Google Scholar] [CrossRef]
- Shahanavaz, S.; Balzer, D.; Babaliaros, V.; Kim, D.; Dimas, V.; Veeram Reddy, S.R.; Leipsic, J.; Blanke, P.; Shirali, G.; Parthiban, A.; et al. Alterra Adaptive Prestent and SAPIEN 3 THV for Congenital Pulmonic Valve Dysfunction: An Early Feasibility Study. JACC Cardiovasc. Interv. 2020, 13, 2510–2524. [Google Scholar] [CrossRef]
- Fukuda, T.; Tan, W.; Sadeghi, S.; Lin, J.; Salem, M.; Levi, D.; Aboulhosn, J. Utility of the long DrySeal sheath in facilitating transcatheter pulmonary valve implantation with the Edwards Sapien 3 valve. Catheter. Cardiovasc. Interv. 2020, 96, E646–E652. [Google Scholar] [CrossRef]
- Rockefeller, T.; Shahanavaz, S.; Zajarias, A.; Balzer, D. Transcatheter implantation of SAPIEN 3 valve in native right ventricular outflow tract for severe pulmonary regurgitation following tetralogy of fallot repair. Catheter. Cardiovasc. Interv. 2016, 88, E28–E33. [Google Scholar] [CrossRef]
- Plessis, J.; Hascoet, S.; Baruteau, A.; Godart, F.; Le Gloan, L.; Warin Fresse, K.; Tahhan, N.; Riou, J.Y.; Guyomarch, B.; Petit, J.; et al. Edwards SAPIEN Transcatheter Pulmonary Valve Implantation: Results From a French Registry. JACC Cardiovasc. Interv. 2018, 11, 1909–1916. [Google Scholar] [CrossRef]
| Conventional Technique n = 27 | Modified Technique n = 27 | p-Value | |
|---|---|---|---|
| Age (years), median [Q1;Q3] | 30.0 [24.4–47.0] | 31.0 [22.0–36.5] | 0.42 |
| Weight, mediane [Q1;Q3] | 58.0 [52.5–73.2] | 60.3 [51.3–77.4] | 0.85 |
| Height, mediane [Q1;Q3] | 167 [162–173] | 170 [159–177] | 0.85 |
| Male | 14 (51.9%) | 15 (55.6%) | 0.78 |
| Type of congenital heart diseases | 1.00 | ||
| Fallot | 23 (85.2%) | 22 (81.5%) | |
| Pulmonary valvar stenosis | 1 (3.7%) | 2 (7.4%) | |
| Pulmonary atresia with intact ventricular | 1 (3.7%) | 1 (3.7%) | |
| Troncus Arteriosus | 1 (3.7%) | 0 (0.0%) | |
| Transposition of great arteries | 1 (3.7%) | 0 (0.0%) | |
| Aortic valve stenosis + Ross procedure | 0 (0.0%) | 1 (3.7%) | |
| Carcinoid Pulmonary valve lesion | 0 (0.0%) | 1 (3.7%) | |
| Right ventricle outflow tract | 0.97 | ||
| Native | 18 (66.7%) | 18 (66.7%) | |
| Homograft | 1 (3.7%) | 2 (7.4%) | |
| Bioprosthetic valve | 5 (18.5%) | 4 (14.8%) | |
| Conduit | 2 (7.4%) | 2 (7.4%) | |
| Valve-in-valve | 1 (3.7%) | 1 (3.7%) | |
| NYHA status | 0.85 | ||
| 1 | 8 (29.6%) | 6 (22.2%) | |
| 2 | 16 (59.3%) | 16 (59.3%) | |
| 3 | 3 (11.1%) | 4 (14.8%) | |
| 4 | 0 (0.0%) | 1 (3.7%) | |
| Indications | 0.09 | ||
| Pulmonary regurgitation | 16 (59.3%) | 19 (70.4%) | |
| Pulmonary stenosis | 1 (3.7%) | 3 (11.1%) | |
| Mixed lesion | 10 (37.0%) | 5 (18.5%) |
| Traditionnal Techniques n = 27 | Modified Techniques n = 27 | p-Value | |
|---|---|---|---|
| Pre-procedure hemodynamic data | |||
| Systolic aortic pressure | 91 [83–105] | 93 [83–100] | 0.81 |
| Systolic RV pressure | 42 [34–52] | 33 [30–48] | 0.12 |
| RV–pulmonary artery gradient | 23 [13–34] | 21 [10–32] | 0.42 |
| Procedure charecteristics | |||
| Procedure time (min) | 82.6 ± 32.8 | 48.1 ± 19.7 | 0.001 |
| Fluoroscopy time (min) | 29.8 ± 22.1 | 15.2 ± 7.9 | <0.0001 |
| Kerma | 815.0 ± 755.9 | 341.5 ± 300.6 | 0.003 |
| PDS | 9543.3 ± 9726.9 | 3923.4 ± 3714.2 | 0.006 |
| Post-procedure hemodynamic data | |||
| Systolic RV pressure | 34 [30–41] | 32 [28–39] | 0.89 |
| RV–pulmonary artery gradient | 7 [3–15] | 6 [3–9] | 0.78 |
| Last fellow-up data | |||
| RVOT Doppler peak velocity | 2.2 [1.8–2.6] | 2 [1.8–2.2] | 0.68 |
| TV Doppler peak gradient | 40 [30–45] | 35 [30–45] | 0.81 |
Disclaimer/Publisher’s Note: The statements, opinions and data contained in all publications are solely those of the individual author(s) and contributor(s) and not of MDPI and/or the editor(s). MDPI and/or the editor(s) disclaim responsibility for any injury to people or property resulting from any ideas, methods, instructions or products referred to in the content. |
© 2023 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Houeijeh, A.; Karsenty, C.; Combes, N.; Batteux, C.; Lecerf, F.; Remy, F.; Valdeolmillos, E.; Petit, J.; Hascoet, S. A Modified Technique for Transcatheter Pulmonary Valve Implantation of SAPIEN 3 Valves in Large Right Ventricular Outflow Tract: A Matched Comparison Study. J. Clin. Med. 2023, 12, 7656. https://doi.org/10.3390/jcm12247656
Houeijeh A, Karsenty C, Combes N, Batteux C, Lecerf F, Remy F, Valdeolmillos E, Petit J, Hascoet S. A Modified Technique for Transcatheter Pulmonary Valve Implantation of SAPIEN 3 Valves in Large Right Ventricular Outflow Tract: A Matched Comparison Study. Journal of Clinical Medicine. 2023; 12(24):7656. https://doi.org/10.3390/jcm12247656
Chicago/Turabian StyleHoueijeh, Ali, Clément Karsenty, Nicolas Combes, Clément Batteux, Florence Lecerf, Frederic Remy, Estibaliz Valdeolmillos, Jérôme Petit, and Sébastien Hascoet. 2023. "A Modified Technique for Transcatheter Pulmonary Valve Implantation of SAPIEN 3 Valves in Large Right Ventricular Outflow Tract: A Matched Comparison Study" Journal of Clinical Medicine 12, no. 24: 7656. https://doi.org/10.3390/jcm12247656
APA StyleHoueijeh, A., Karsenty, C., Combes, N., Batteux, C., Lecerf, F., Remy, F., Valdeolmillos, E., Petit, J., & Hascoet, S. (2023). A Modified Technique for Transcatheter Pulmonary Valve Implantation of SAPIEN 3 Valves in Large Right Ventricular Outflow Tract: A Matched Comparison Study. Journal of Clinical Medicine, 12(24), 7656. https://doi.org/10.3390/jcm12247656





