5.2. Surgical Treatment
If conservative treatment fails, surgical excision is recommended based on established algorithms by McMahon (
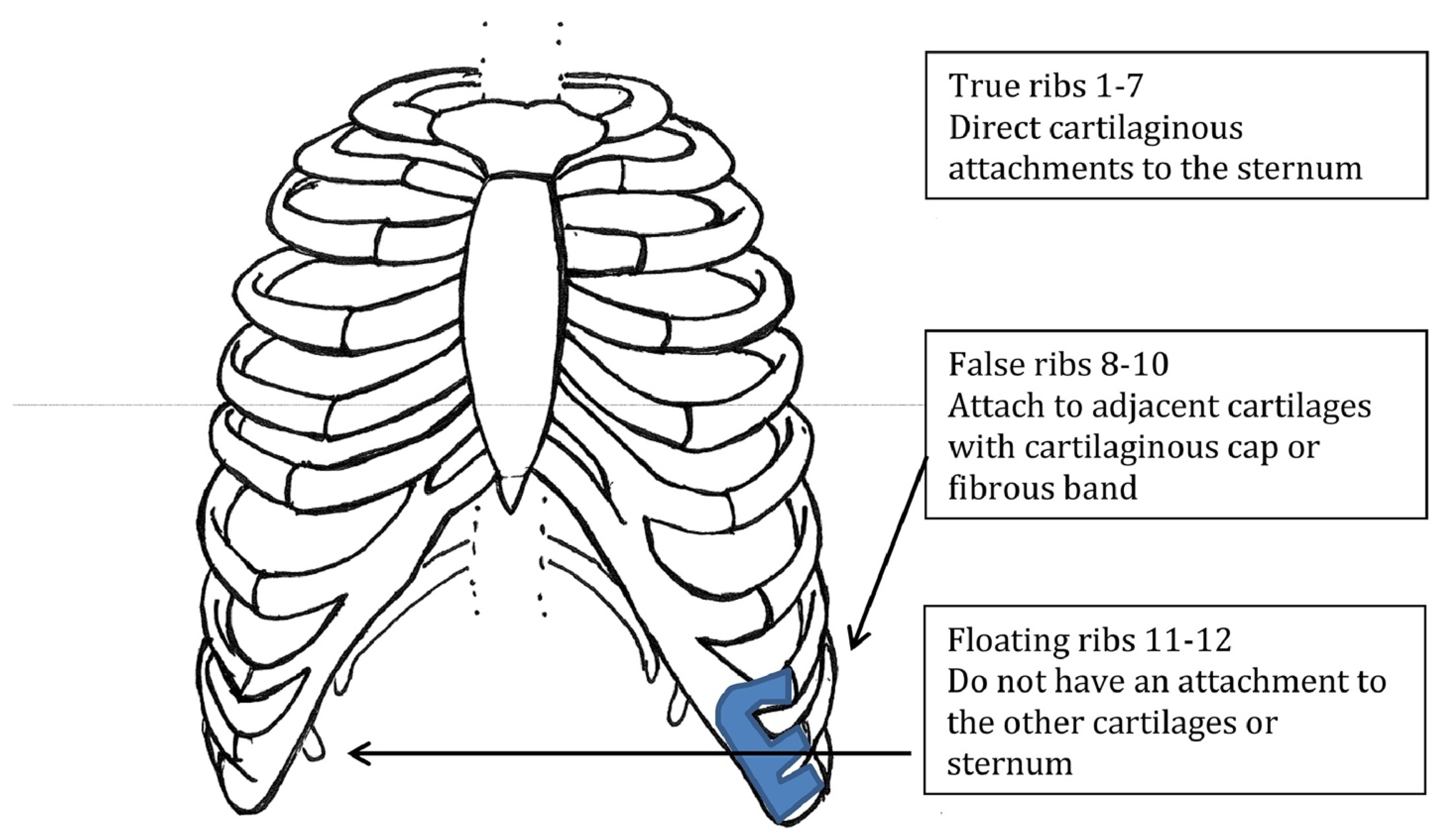
Figure 4). Cartilaginous rib excision (CRE) has been the mainstay of surgical treatment for SRS. This usually involves the resection of two or three rib cartilages. However, in recent years, minimally invasive rib stabilization and cartilaginous rib excision with vertical rib plating has been reported.
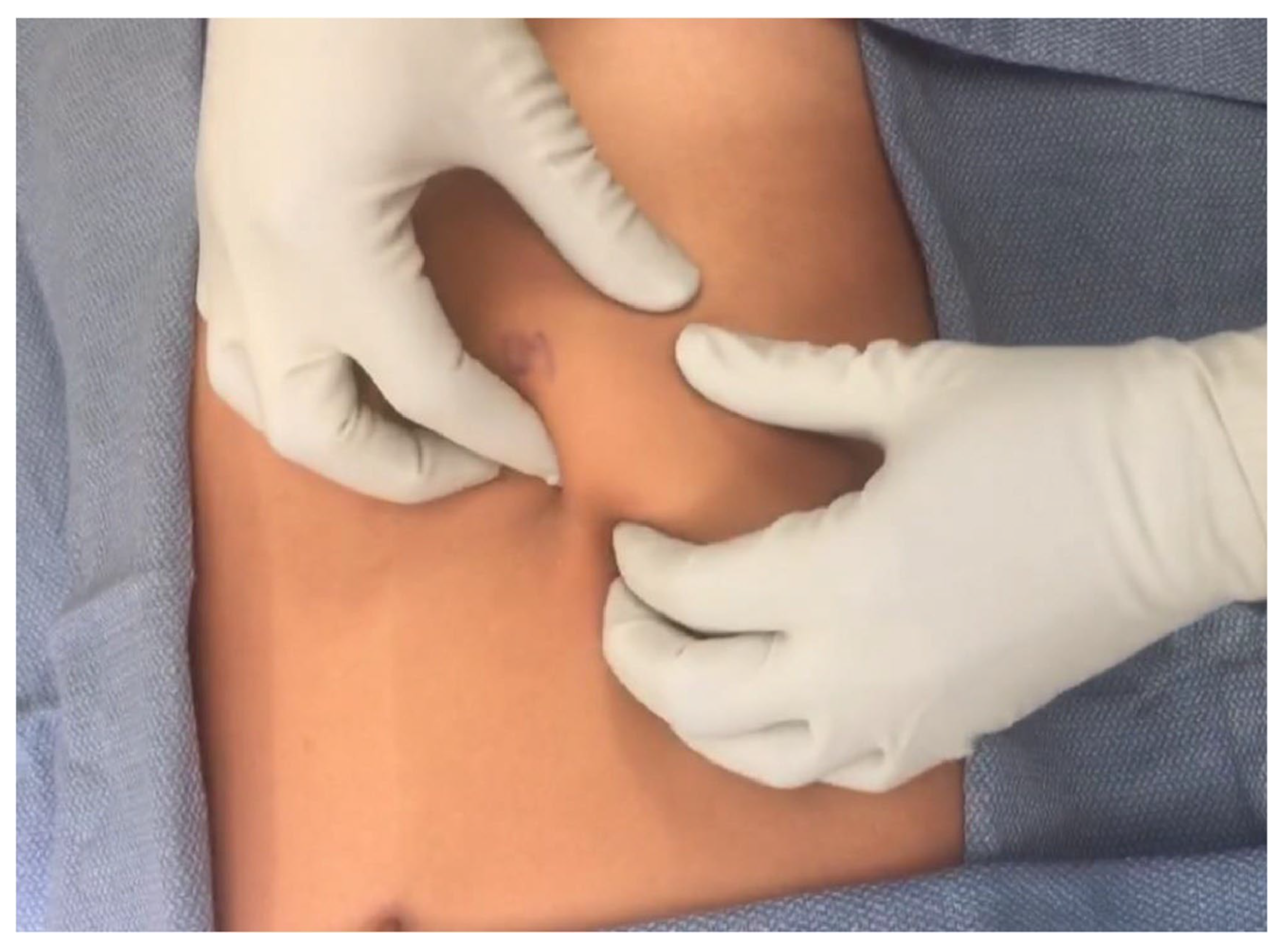
CRE is performed via a small incision at the lower costal margin; the hypermobile cartilaginous rib is identified and excised to the costochondral junction. The rib is left intact, the thoracic cavity is not violated, and the neurovascular bundle is carefully preserved. The current literature shows symptomatic relief following CRE in adult and pediatric SRS patients. In a 2022 single-institution descriptive study, Macgregor et al. reviewed thirteen pediatric patients with SRS who underwent CRE from 2012 to 2020. In total, 91% of patients reported improvement in pain post-operatively, with a median follow-up time of 3.5 months. Unfortunately, this cohort had a median time of 2 years from symptom onset to surgical resection, which is supported by the literature [
10]. Fraser et al. shows similarly high rates of symptom resolution (77%) in pediatric patients undergoing cartilaginous rib excision over a 4.5-year follow-up period. This study also showed a high long-term satisfaction rate over a long follow-up period among patients who underwent CRE, even if a complete cure was not reached [
4]. In a retrospective study by Mazzella et al., nineteen adult patients with SRS showed that CRE led to a resolution of symptoms in the early post-operative period; however, the mid- to long-term follow-up showed symptom recurrence in 31% of patients. The main challenge of utilizing CRE is that it does not resolve the rib hypermobility, it only decreases how much rib is available to cause irritation [
15].
Laparoscopic CRE has also been studied. In 2020, Squillaro et al. performed a small, retrospective review of four pediatric patients with SRS comparing laparoscopic versus open CRE. The study showed laparoscopic CRE is a safe and effective technique. Three 5 mm ports are placed at the umbilicus, mid-epigastric, and mid-suprapubic. A laparoscopic hook cautery is used to open the peritoneal lining, dissect, and expose the cartilage; a Maryland or locking grasper helps provide traction. A pituitary rongeur is used to cut the cartilage and is removed via the umbilical port site. The peritoneal lining is laparoscopically closed. The average procedure time for laparoscopic CRE was 73 min; this was longer than the 57 min procedure time for open CRE. Within the laparoscopic CRE population, the average length of the cartilage resected was 2.3 cm with 1.3 cartilages resected. The length of stay was similar between both groups; 1.3 days with laparoscopic CRE versus 1 day with open CRE [
16].
Likely due to the continued rib hypermobility, there are high rates of recurrence in patients with SRS who undergo CRE. Gould et al. reports nearly a fourth of patients will experience recurrence of SRS after CRE, citing 26% requiring subsequent reoperation [
13]. Within the pediatric cohort in Fraser et al., 22% of patients had recurrence following CRE requiring reoperation with a median time to recurrence of 1.6 years. No anthropometric differences were found between patients who did and did not have recurrence requiring reoperation. However, patients with recurrence requiring reoperation were found to have residual cartilage and/or hypermobile ribs that slipped intra-operatively; Fraser et al. postulate this may be due to regrowth from repeated trauma in the pediatric SRS population [
4]. There are no long-term studies defining recurrence rates and risk factors in the adult SRS population.
Vertical rib plating has been shown to decrease recurrence rates. In a 2020 retrospective review of 85 patients by McMahon et. al, two cohorts of SRS patients who underwent cartilaginous rib excision were compared, those with and those without bioabsorbable vertical rib plating (VRP). Rib plating was utilized to reduce recurrence and reoperation if the surgeon was able to manually subluxate the affected rib over, under or into the adjacent rib during intra-operative evaluation. The BioBridge
TM bioabsorbable plate was utilized. Bioabsorbable plates have been used for other pathologies, such as facial fracture repair and clavicle fixation. They have an improved profile when compared to metal implants and have been shown to be safe in adult and pediatric populations. Over time, the plates are absorbed and leave behind scar tissue that serves as a stabilization for the ribs. A total of 17.1% of patients who were not plated experienced recurrence, versus 3.4% for patients who were plated, a significant reduction. Notably, in the plated patient cohort who presented with recurrence, both patients presented with clinical symptoms after a motor vehicle crash and a pedestrian struck by a motor vehicle crash. Of the 7 patients who were unplated and recurred, 6 patients underwent more than one reoperation to remove additional symptomatic rib or cartilage. Of the 41 patients within the cohort, three patients were unplated, recurred, and subsequently plated. Recurrence was defined as the return of clinical symptoms and confirmed with physical exam findings and positive dynamic ultrasounds. The median time to recurrence was six months. VRP significantly increased the intra-operative time (48 min in bilateral VRP,
p < 0.001) and length of stay (11 h,
p < 0.001). VRP did not increase the frequency of severe post-operative pain events. There were no major complications associated with VRP. Whilst vertical rib plating appears promising in the short-term, long-term data are still necessary to evaluate recurrence rates after the bioabsorbable plates have completely resorbed, which occurs by the second year of use. Within this study, the decision to utilize vertical rib plating was dependent on intra-operative subluxation of the affected ribs; further research is also needed to determine what criteria should be used when selecting patients who should or should not undergo VRP [
6].
Chest wall reconstruction is a challenging undertaking. The ideal reconstructive material restores skeletal integrity, is low risk, easy to use, and inexpensive. Reconstruction materials include synthetic and biomaterials. Synthetic meshes include polypropylene, polytetrafluoroethylene (PTFE), polyglactin, and polypropylene mesh-methyl methacrylate composite. However, they did not completely incorporate into tissue and are susceptible to infection; they require removal if infected. Biomaterials have more recently been introduced in thoracic skeleton reconstruction. In a retrospective review of 112 patients who underwent chest wall stabilization or reconstruction, 25 patients (22%) underwent reconstruction with biologic materials, a bovine pericardium patch and/or polylactic acid (PLA) bars (BioBridge™, Acute Innovations, Hillsboro, OR). In total, 68% of patients underwent chest wall resection and reconstruction for malignant disease, 44% underwent thoracic radiation pre-operatively, and 40% had pre-operatively infected reconstruction sites. Even within this population with a multitude of high-risk factors for chest wall reconstruction failure, only three patients required the removal of their biomaterials. In two patients, bovine pericardium was explanted during reoperation for partially necrotic muscle. In one patient, PLA bars were explanted for inflammatory reaction 3 months after a redo pectus repair. The median follow-up was 12 months; no patients with pre-operatively infected sites required biomaterial removal. No patients had a paradoxical respiratory motion of the thoracic skeleton, seroma formation, wound infection, or biomaterial infection [
17].
However, there have been reports of the failure of bioabsorbable plates used for chest wall reconstruction. Haslem et al. illustrates the case of a 66-year-old woman who underwent chest wall reconstruction for a radiation-induced wound with exposed ribs. Surgical resection and reconstruction included the excision of two ribs with a bony defect measuring 10 cm by 10 cm. Two BioBridge
TM bioabsorbable plates were used along with a biologic Strat Tice porcine tissue matrix as part of the reconstruction to provide chest wall stability and good cometic outcome. The soft tissue defect was covered with a myocutaneous latissimus dorsi flap. Six months after the index operation, the patient presented with a 2.5 cm superficial wound dehiscence and was found to have a 2 cm fragment of BioBridge™ plate which was extracted. On reoperation, the two BioBridge™ plates were fragmented in seven pieces, which were explanted. There was no plate resorption at six months. The authors postulated the structural failure of the BioBridge™ plates were likely contributory in the patient’s post-operative wound complication [
18]. BioBridge states the plates maintain their strength and durability for up to 6 months and resorption via hydrolysis occurs between 18 and 24 months.
In a 2019 retrospective review, Hansen et al. describes a minimally invasive slipped rib repair in 29 adult patients with SRS without cartilaginous rib excision. The authors stabilize the tenth rib costal insertion with two figure-of-eight stitches using an orthopedic tape suture (TigerTape) by fixing it superiorly and inferiorly. The sutures are carefully placed so as to avoid nerve entrapment. The incision is closed in multiple layers. The procedure is completed without entering the pleural cavity, so no thoracostomy tube is necessary. Patients were discharged the same day with an oral pain regimen. On post-operative follow-up, patients had a significant increase in function after slipped rib repair at one week, one month, and six months post-operatively (
p < 0.001). They also had a significant decrease in disability during the same time intervals (
p < 0.001) [
1].
The reports of combining CRE and VRP with using the patients’ own excised cartilage (from CRE) as spacers between the ribs are forthcoming. Utilizing CRE as spacers may help further stabilize the region and prevent nerve impingement if suture fixation of the affected ribs is performed. There may be utility in extending this rib fixation technique to the pediatric population; however, there may be challenges applying the procedure to growing children, in whom the rib cage is still undergoing somatic growth.
Pre-operative, intra-operative, and post-operative pain control in patients who undergo minimally invasive slipped rib repair is not well-understood. There is a paucity of literature studying pain management in this population. Macgregor et al. underscores the need for a multidisciplinary approach. There is also benefit in the implementation of a formal pathway that includes multiple specialties, including regional and pain anesthesiologists, physical therapy, and pain psychologists. This would allow patients to undergo a coordinated, monitored, and tailored non-operative management plan for symptom relief. This may be useful in selecting patients who are failing non-operative management and would benefit from surgical intervention [
1].
Most patients are taking either neural modulating medications, NSAIDs, or narcotics pre-operatively; many on a multi-modal analgesic regimen. Intercostal nerve blocks are utilized intra-operatively. Post-operatively, patients can be discharged the same day with a multi-modal pain regimen, often including narcotic medications and NSAIDs. In Hansen et al.’s cohort of 29 patients, a similar intra-operative and post-operative regimen was utilized. Median post-operative improvement in pain at 1 month and 6 months were 75% (
p < 0.001) and 80% (
p < 0.001). Among the patients who used pain medications pre-operatively, 100% of patients discontinued narcotics at 1 month, 86% discontinued neural modulators and 92% discontinued NSAIDs (all values
p < 0.001) [
1]. Burjek et al. reports on the successful use of an ambulatory erector spinae plane (ESP) block in a seventeen-year-old patient with a history of chronic pain and SRS after surgical intervention. The patient underwent intra-operative ESP placement at level T9 through T10. Post-operatively, she received a continuous nerve catheter infusion of 10.8 mL/h of ropivacaine 0.2% (0.125 mL/kg/h), as well as gabapentin 600 mg three times a day, ketorolac 30 mg every six hours, acetaminophen 650 mg every 6 h, diazepam 2.6 mg every 6 h as needed, and demand-only hydromorphone patient-controlled analgesia (PCA). She was discharged home on post-operative day one with an elastomeric pump and an oral regimen of gabapentin 600 mg three times a day, acetaminophen 650 mg every 6 h, ibuprofen 600 mg every 6 h, cyclobenzaprine 10 mg as needed, and oxycodone 5 mg as needed. The ESP catheter was removed at home on post-operative day four [
19]. Large studies have shown the use of peripheral nerve catheters in children is safe, with low failure and complication rates [
20]. In a randomized control trial, Gould et al. compared ESP and continuous thoracic epidural analgesia in adult cardiac surgery patients who underwent sternotomy and showed comparable outcomes, suggesting ESP is a safe and effective alternative [
21]. However, the use of ambulatory ESPs for acute post-operative surgical pain has not been studied in adult patients.
Intercostal nerve cryoablation has been used in the minimally invasive repair of pectus excavatum. Cryoablation (or cryo) involves the thoracoscopic (either intra- or extra-thoracically) delivery of extremely cold temperatures to temporarily stunt nerve function via a probe. This loss of function does not seem to have an effect on the motor function of breathing due to its locoregional delivery. A study of pediatric SRS patients by Lai et al. compared those who underwent CRE without cryo, those who underwent CRE with cryo, and those who underwent CRE with minimally invasive pectus excavatum repair and cryo. Of note, CRE was performed with vertical rib plating with a BioBridge™ absorbable plate. Within the CRE with cryo cohort of 20 patients, cryo was delivered extra-thoracically by tunnelling the problem below the intercostal muscle to provide temporary disruption of the intercostal nerve. The study reported there was a significant decrease of in-hospital opioid use and length of stay in patients who underwent cartilaginous rib excision and vertical rib plating with cryoablation (median LOS 1 day) versus cartilaginous rib excision without cryoablation (median LOS 2 days). Alternatively, the number of CREs performed, unilateral versus bilateral CRE, use of rib plating, age, sex, or BMI were not associated with in-hospital use. These data are corroborated by studies within the minimally invasive repair of the pectus excavatum population, which show decreased opioid use and length of stay in patients who undergo cryoablation versus those who do not [
5,
22]. No patients had post-operative abdominal wall laxity at a two-week follow-up. This is an important finding as the manufacturer warns against using cryoablation below the ninth rib as those nerves are contributory in motor innervation of the abdominal wall muscle [
23]. There is still further research to be conducted on the long-term utility of cryoablation in patients undergoing slipped rib repair and its long-term effects on post-operative pain control and possible complications, such as abdominal wall weakness or pneumothorax.