Ultrasound-Guided Bilateral Erector Spinae Plane Block vs. Ultrasound-Guided Bilateral Posterior Quadratus Lumborum Block for Postoperative Analgesia after Caesarean Section: An Observational Closed Mixed Cohort Study
Abstract
:1. Introduction
2. Materials and Methods
2.1. ESPB Group
2.2. pQLB Group
2.3. Outcomes
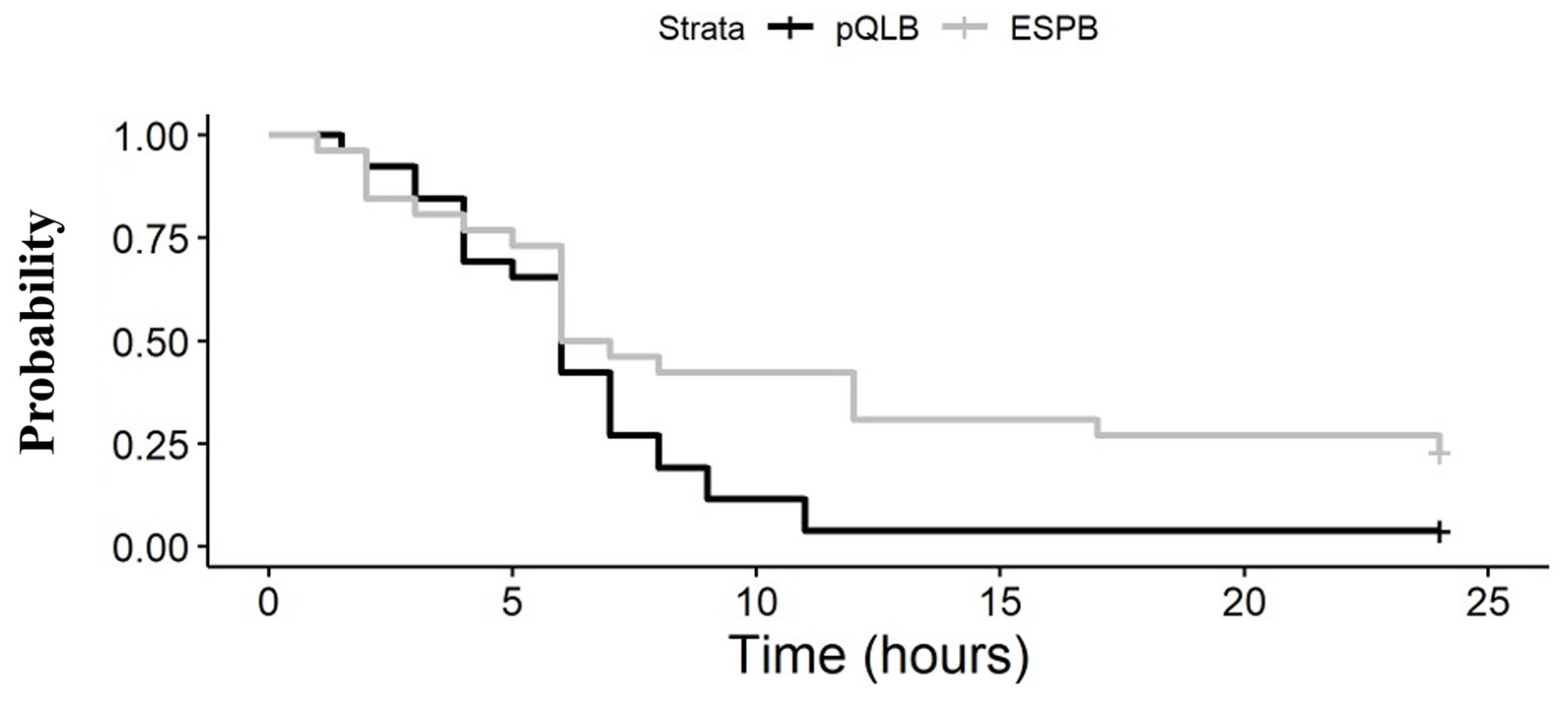
- Time to first opioid request (interval time between block and first opioid analgesic request);
- The relationship between the analgesic block performed and NPRS (ranging from 0, “no pain”, to 10, “the worst pain imaginable”), at rest and on movement at 0, 2, 6, 12 and 24 h from block performance;
- Differences in haemodynamic parameters;
- Any adverse event, like sedation, nausea and other complications, particularly signs of LA toxicity and the occurrence or persistence of motor weakness at the lower extremities after spinal anaesthesia recovery.
2.4. Statistical Analysis
3. Results
4. Discussion
5. Conclusions
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Conflicts of Interest
References
- Osterman, M.J.K.; Hamilton, B.E.; Martin, J.A.; Driscoll, A.K.; Valenzuela, C.P. Births: Final Data for 2020. Natl. Vital Stat. Rep. 2022, 70, 1–50. [Google Scholar] [CrossRef]
- Carvalho, B.; Cohen, S.E.; Lipman, S.S.; Fuller, A.; Mathusamy, A.D.; Macario, A. Patient Preferences for Anesthesia Outcomes Associated with Cesarean Delivery. Anesth. Analg. 2005, 101, 1182–1187. [Google Scholar] [CrossRef] [PubMed]
- Ortner, C.; Turk, D.; Theodore, B.; Siaulys, M.; Bollag, L.; Landau, R. The Short-Formmcgill Pain Questionnaire-Revised to Evaluate Persistent Pain and Surgery-Related Symptoms in Healthy Women Undergoing a Planned Cesarean Delivery. Reg. Anesth. Pain Med. 2014, 39, 478–486. [Google Scholar] [CrossRef] [PubMed]
- Gamez, B.H.; Habib, A.S. Predicting Severity of Acute Pain after Cesarean Delivery: A Narrative Review. Anesth. Analg. 2018, 126, 1606–1614. [Google Scholar] [CrossRef] [PubMed]
- Kainu, J.P.; Sarvela, J.; Tiippana, E.; Halmesmäki, E.; Korttila, K.T. Persistent Pain after Caesarean Section and Vaginal Birth: A Cohort Study. Int. J. Obstet. Anesth. 2010, 19, 4–9. [Google Scholar] [CrossRef] [PubMed]
- Yimer, H.; Woldie, H. Incidence and Associated Factors of Chronic Pain After Caesarean Section: A Systematic Review. J. Obstet. Gynaecol. Can. 2019, 41, 840–854. [Google Scholar] [CrossRef] [PubMed]
- Wong, C.A.; Girard, T. Undertreated or Overtreated? Opioids for Postdelivery Analgesia. Br. J. Anaesth. 2018, 121, 339–342. [Google Scholar] [CrossRef] [PubMed]
- Roofthooft, E.; Joshi, G.P.; Rawal, N.; Van de Velde, M. PROSPECT Guideline for Elective Caesarean Section: An Update. Anaesthesia 2023, 78, 1170–1171. [Google Scholar] [CrossRef]
- Forero, M.; Adhikary, S.D.; Lopez, H.; Tsui, C.; Chin, K.J. The Erector Spinae Plane Block a Novel Analgesic Technique in Thoracic Neuropathic Pain. Reg. Anesth. Pain Med. 2016, 41, 621–627. [Google Scholar] [CrossRef]
- Aygun, H.; Kavrut Ozturk, N.; Pamukcu, A.S.; Inal, A.; Kiziloglu, I.; Thomas, D.T.; Tulgar, S.; Nart, A. Comparison of Ultrasound Guided Erector Spinae Plane Block and Quadratus Lumborum Block for Postoperative Analgesia in Laparoscopic Cholecystectomy Patients; a Prospective Randomized Study. J. Clin. Anesth. 2020, 62, 109696. [Google Scholar] [CrossRef]
- Kendall, M.C.; Alves, L.; Traill, L.L.; De Oliveira, G.S. The Effect of Ultrasound-Guided Erector Spinae Plane Block on Postsurgical Pain: A Meta-Analysis of Randomized Controlled Trials. BMC Anesthesiol. 2020, 20, 99. [Google Scholar] [CrossRef] [PubMed]
- Tulgar, S.; Selvi, O.; Senturk, O.; Serifsoy, T.E.; Thomas, D.T. Ultrasound-Guided Erector Spinae Plane Block: Indications, Complications, and Effects on Acute and Chronic Pain Based on a Single-Center Experience. Cureus 2019, 11, e3815. [Google Scholar] [CrossRef] [PubMed]
- Kwon, H.M.; Kim, D.H.; Jeong, S.M.; Choi, K.T.; Park, S.; Kwon, H.J.; Lee, J.H. Does Erector Spinae Plane Block Have a Visceral Analgesic Effect?: A Randomized Controlled Trial. Sci. Rep. 2020, 10, 83–89. [Google Scholar] [CrossRef] [PubMed]
- Chin, K.J.; Adhikary, S.; Forero, M. Is the Erector Spinae Plane (ESP) Block a Sheath Block? A Reply. Anaesthesia 2017, 72, 916–917. [Google Scholar] [CrossRef] [PubMed]
- Hamilton, D.L.; Manickam, B.P. Is the Erector Spinae Plane (ESP) Block a Sheath Block? Anaesthesia 2017, 72, 915–916. [Google Scholar] [CrossRef] [PubMed]
- El-Boghdadly, K.; Wolmarans, M.; Stengel, A.D.; Albrecht, E.; Chin, K.J.; Elsharkawy, H.; Kopp, S.; Mariano, E.R.; Xu, J.L.; Adhikary, S.; et al. Standardizing Nomenclature in Regional Anesthesia: An ASRA-ESRA Delphi Consensus Study of Abdominal Wall, Paraspinal, and Chest Wall Blocks. Reg. Anesth. Pain Med. 2021, 46, 571–580. [Google Scholar] [CrossRef] [PubMed]
- Zhang, Z.; Zhu, R.L.; Yue, L.; Li, X.; Ma, J.H.; Kong, H.; Li, C.-d.; Zhang, H.; Wang, D.X. Bilateral Ultrasound-Guided Erector Spinae Plane Block versus Wound Infiltration for Postoperative Analgesia in Lumbar Spinal Fusion Surgery: A Randomized Controlled Trial. Eur. Spine J. 2023, 32, 301–312. [Google Scholar] [CrossRef] [PubMed]
- Blanco, R.; Ansari, T.; Girgis, E. Quadratus Lumborum Block for Postoperative Pain after Caesarean Section: A Randomised Controlled Trial. Eur. J. Anaesthesiol. 2015, 32, 812–818. [Google Scholar] [CrossRef]
- Zanfini, B.A.; Biancone, M.; Famele, M.; Catarci, S.; Lavalle, R.; Frassanito, L.; Draisci, G. Comparison of Ropivacaine Plasma Concentration after Posterior Quadratus Lumborum Block in Cesarean Section with Ropivacaine with Epinephrine vs. Plane. Minerva Anestesiol. 2021, 87, 979–986. [Google Scholar] [CrossRef]
- Aldrete, J.A. The Post-Anesthesia Recovery Score Revisited. J. Clin. Anesth. 1995, 7, 89–91. [Google Scholar] [CrossRef]
- Bakshi, A.; Srivastawa, S.; Jadon, A.; Mohsin, K.; Sinha, N.C.S. Comparison of the Analgesic Efficacy of Ultrasound-Guided Transmuscular Quadratus Lumborum Block versus Thoracic Erector Spinae Block for Postoperative Analgesia in Caesarean Section Parturients under Spinal Anaesthesia-A Randomised Study. Indian J. Anaesth. 2022, 66, S213–S219. [Google Scholar]
- Feilberg, V.L.; Rosenborg, D.; Christensen, C.B.; Mogensen, J.V. Excretion of Morphine in Human Breast Milk. Acta Anaesthesiol. Scand. 1989, 33, 426–428. [Google Scholar] [CrossRef] [PubMed]
- Priya, T.K.; Singla, D.; Talawar, P.; Sharma, R.S.; Goyal, S.; Purohit, G. Comparative Efficacy of Quadratus Lumborum Type-II and Erector Spinae Plane Block in Patients Undergoing Caesarean Section under Spinal Anaesthesia: A Randomised Controlled Trial. Int. J. Obstet. Anesth. 2023, 53, 103614. [Google Scholar] [CrossRef] [PubMed]
- Chin, K.J.; Lirk, P.; Hollmann, M.W.; Schwarz, S.K.W. Mechanisms of Action of Fascial Plane Blocks: A Narrative Review. Reg. Anesth. Pain Med. 2021, 46, 618–628. [Google Scholar] [CrossRef]
- Yamak Altinpulluk, E.; García Simón, D.; Fajardo-Pérez, M. Erector Spinae Plane Block for Analgesia after Lower Segment Caesarean Section: Case Report. Rev. Esp. Anestesiol. Reanim. 2018, 65, 284–286. [Google Scholar] [CrossRef] [PubMed]
- Tulgar, S.; Ahiskalioglu, A.; De Cassai, A.; Gurkan, Y. Efficacy of Bilateral Erector Spinae Plane Block in the Management of Pain: Current Insights. J. Pain Res. 2019, 12, 2597–2613. [Google Scholar] [CrossRef]
- Elsharkawy, H.; El-Boghdadly, K.; Barrington, M. Quadratus Lumborum Block: Anatomical Concepts, Mechanisms, and Techniques. Anesthesiology 2019, 130, 322–335. [Google Scholar] [CrossRef]
- Carline, L.; McLeod, G.A.; Lamb, C. A Cadaver Study Comparing Spread of Dye and Nerve Involvement after Three Different Quadratus Lumborum Blocks. Br. J. Anaesth. 2016, 117, 387–394. [Google Scholar] [CrossRef]
- Hu, J.; Chen, Q.; Xu, Q.; Song, Y.; Wei, K.L.X. Analgesic Effect of Ultrasound-Guided Erector Spinae Plane Block (Espb) in General Anesthesia for Cesarean Section: A Randomized Controlled Trial. BMC Anesthesiol. 2022, 22, 244. [Google Scholar] [CrossRef]
- Boules, M.L.; Goda, A.S.; Abdelhady, M.A.; Abu El, S.A.; El-Azeem, N.A.; Hamed, M.A. Comparison of Analgesic Effect between Erector Spinae Plane Block and Transversus Abdominis Plane Block after Elective Cesarean Section: A Prospective Randomized Single-Blind Controlled Study. J. Pain Res. 2020, 13, 1073–1080. [Google Scholar] [CrossRef]
- Malawat, A.; Verma, K.; Jethava, D.; Jethava, D. Erector Spinae Plane Block and Transversus Abdominis Plane Block for Postoperative Analgesia in Cesarean Section: A Prospective Randomized Comparative Study. J. Anaesthesiol. Clin. Pharmacol. 2020, 36, 201–206. [Google Scholar] [CrossRef] [PubMed]
- Hamed, M.A.; Yassin, H.M.; Botros, J.M.; Abdelhady, M.A. Analgesic Efficacy of Erector Spinae Plane Block Compared with Intrathecal Morphine after Elective Cesarean Section: A Prospective Randomized Controlled Study. J. Pain Res. 2020, 13, 597–604. [Google Scholar] [CrossRef] [PubMed]
- Cai, Q.; Liu, G.; Huang, L.; Yang, Z.; Gao, M.; Jing, R.; Liu, Z.; Pan, L. Effects of Erector Spinae Plane Block on Postoperative Pain and Side-Effects in Adult Patients Underwent Surgery: A Systematic Review and Meta-Analysis of Randomized Controlled Trials. Int. J. Surg. 2020, 80, 107–116. [Google Scholar] [CrossRef] [PubMed]
- Ribeiro Junior, I.d.V.; Carvalho, V.H.; Brito, L.G.O. Erector Spinae Plane Block for Analgesia after Cesarean Delivery: A Systematic Review with Meta-Analysis. Braz. J. Anesthesiol. 2022, 72, 506–515. [Google Scholar] [CrossRef] [PubMed]
- Xu, M.; Tang, Y.; Wang, J.; Yang, J. Quadratus Lumborum Block for Postoperative Analgesia after Cesarean Delivery: A Systematic Review and Meta-Analysis. Int. J. Obstet. Anesth. 2020, 42, 87–98. [Google Scholar] [CrossRef] [PubMed]
- Pangthipampai, P.; Dejarkom, S.; Poolsuppasit, S.; Luansritisakul, C.; Tangchittam, S. Bilateral Posterior Quadratus Lumborum Block for Pain Relief after Cesarean Delivery: A Randomized Controlled Trial. BMC Anesthesiol. 2021, 21, 90. [Google Scholar] [CrossRef] [PubMed]
- Salama, E.R. Ultrasound-Guided Bilateral Quadratus Lumborum Block vs. Intrathecal Morphine for Postoperative Analgesia after Cesarean Section: A Randomized Controlled Trial. Korean J. Anesthesiol. 2020, 73, 121–128. [Google Scholar] [CrossRef]
- Metin, K.M.; Güzel, I.; Oskovi, A.; Guzel, A.I. Chronic Subdural Hematoma Following Spinal Anesthesia for Cesarean Section. J. Exp. Ther. Oncol. 2015, 11, 97–99. [Google Scholar]
- D’Alfonso, A.; Serva, A.; Mascaretti, S.; Ludovisi, M.; Di Sibio, A.; Di Florio, C.; Guido, M. Case Report: Incomplete Cauda Equina Syndrome Following a Caesarean Section with Spinal Anaesthesia. Ital. J. Gynaecol. Obstet. 2022, 34, 293–301. [Google Scholar] [CrossRef]
- Zaphiratos, V.; McKeen, D.M.; Macaulay, B.; George, R.B. Persistent Paralysis after Spinal Anesthesia for Cesarean Delivery. J. Clin. Anesth. 2015, 27, 68–72. [Google Scholar] [CrossRef]
- Watson, S.E.; Richardson, A.L.; Lucas, D.N. Neuraxial and General Anaesthesia for Caesarean Section. Best Pract. Res. Clin. Anaesthesiol. 2022, 36, 53–68. [Google Scholar] [CrossRef] [PubMed]
- Devroe, S.; Van De Velde, M.; Rex, S. General Anesthesia for Caesarean Section. Curr. Opin. Anaesthesiol. 2015, 28, 240–246. [Google Scholar] [CrossRef] [PubMed]
- Santos, A.C.; DeArmas, P.I. Systemic Toxicity of Levobupivacaine, Bupivacaine, and Ropivacaine during Continuous Intravenous Infusion to Nonpregnant and Pregnant Ewes. Anesthesiology 2001, 95, 1256–1264. [Google Scholar] [CrossRef] [PubMed]
- Mock, N.D.; Griggs, K.M.; Mileto, L.A. Local Anesthetic Systemic Toxicity during Labor, Birth, and Immediate Postpartum: Clinical Review. MCN Am. J. Matern. Nurs. 2021, 46, 330–338. [Google Scholar] [CrossRef] [PubMed]
- Griffiths, J.D.; Barron, F.A.; Grant, S.; Bjorksten, A.R.; Hebbard, P.; Royse, C.F. Plasma Ropivacaine Concentrations after Ultrasound-Guided Transversus Abdominis Plane Block. Br. J. Anaesth. 2010, 105, 853–856. [Google Scholar] [CrossRef] [PubMed]
- Knudsen, K.; Beckman Suurküla, M.; Blomberg, S.; Sjövall, J.; Edvardsson, N. Central Nervous and Cardiovascular Effects of i.v. Infusions of Ropivacaine, Bupivacaine and Placebo in Volunteers. Br. J. Anaesth. 1997, 78, 507–514. [Google Scholar] [CrossRef] [PubMed]
- Abd Ellatif, S.E.; Abdelnaby, S.M. Ultrasound Guided Erector Spinae Plane Block versus Quadratus Lumborum Block for Postoperative Analgesia in Patient Undergoing Open Nephrectomy: A Randomized Controlled Study. Egypt. J. Anaesth. 2021, 37, 123–134. [Google Scholar] [CrossRef]
- Wikner, M. Unexpected Motor Weakness Following Quadratus Lumborum Block for Gynaecological Laparoscopy. Anaesthesia 2017, 72, 230–232. [Google Scholar] [CrossRef]


| Characteristics | ESPB (N = 26) | pQLB (N = 26) | |
|---|---|---|---|
| Age, y | 35 (6) | 34 (4) | 0.667 |
| Height, m | 1.63 (6) | 1.64 (6) | 0.512 |
| Weight, kg | 74 (67, 79) | 74 (64, 84) | 0.777 |
| Body mass index, kg/m2 | 28 (25, 29) | 28 (24, 30) | 0.843 |
| Medical history | |||
| Gestational diabetes | 4 (15) | 2 (7) | 0.333 |
| Hypothyroidism | 5 (19) | 0 (0) | 0.025 |
| Factor V Leiden mutation | 0 (0) | 2 (7) | 0.245 |
| ASA status 2 | 26 (100) | 26 (100) | >0.999 |
| Gestational weeks | 38 (38, 39) | 39 (38, 39) | 0.588 |
| Primipara | 20 (77) | 18 (69) | 0.531 |
| Neonatal outcomes | |||
| Neonatal weight, g | 3175 (374) | 3419 (346) | 0.053 |
| Apgar score at 1 min | 10 (9, 10) | 9 (9, 10) | 0.511 |
| Apgar score at 5 min | 10 (9, 10) | 10 (9, 10) | 0.954 |
| Surgery | |||
| Pfannenstiel incision | 25 (96) | 22 (84) | 0.158 |
| Joel Cohen incision | 0 (0) | 1 (4) | >0.999 |
| Length of surgery (minutes) | 59 (46, 72) | 67 (58, 80) | 0.025 |
Disclaimer/Publisher’s Note: The statements, opinions and data contained in all publications are solely those of the individual author(s) and contributor(s) and not of MDPI and/or the editor(s). MDPI and/or the editor(s) disclaim responsibility for any injury to people or property resulting from any ideas, methods, instructions or products referred to in the content. |
© 2023 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Zanfini, B.A.; Di Muro, M.; Biancone, M.; Catarci, S.; Piersanti, A.; Frassanito, L.; Ciancia, M.; Toni, F.; Santantonio, M.T.; Draisci, G. Ultrasound-Guided Bilateral Erector Spinae Plane Block vs. Ultrasound-Guided Bilateral Posterior Quadratus Lumborum Block for Postoperative Analgesia after Caesarean Section: An Observational Closed Mixed Cohort Study. J. Clin. Med. 2023, 12, 7720. https://doi.org/10.3390/jcm12247720
Zanfini BA, Di Muro M, Biancone M, Catarci S, Piersanti A, Frassanito L, Ciancia M, Toni F, Santantonio MT, Draisci G. Ultrasound-Guided Bilateral Erector Spinae Plane Block vs. Ultrasound-Guided Bilateral Posterior Quadratus Lumborum Block for Postoperative Analgesia after Caesarean Section: An Observational Closed Mixed Cohort Study. Journal of Clinical Medicine. 2023; 12(24):7720. https://doi.org/10.3390/jcm12247720
Chicago/Turabian StyleZanfini, Bruno A., Mariangela Di Muro, Matteo Biancone, Stefano Catarci, Alessandra Piersanti, Luciano Frassanito, Mariano Ciancia, Flavia Toni, Maria Teresa Santantonio, and Gaetano Draisci. 2023. "Ultrasound-Guided Bilateral Erector Spinae Plane Block vs. Ultrasound-Guided Bilateral Posterior Quadratus Lumborum Block for Postoperative Analgesia after Caesarean Section: An Observational Closed Mixed Cohort Study" Journal of Clinical Medicine 12, no. 24: 7720. https://doi.org/10.3390/jcm12247720





