Percutaneous Ureteral Stent Insertion in Patients with Benign Uretero-Ileal Anastomosis Strictures Who Underwent Radical Cystectomy: Assessing Risk Factors for Stent Patency
Abstract
:1. Introduction
2. Materials and Methods
2.1. Patient Population
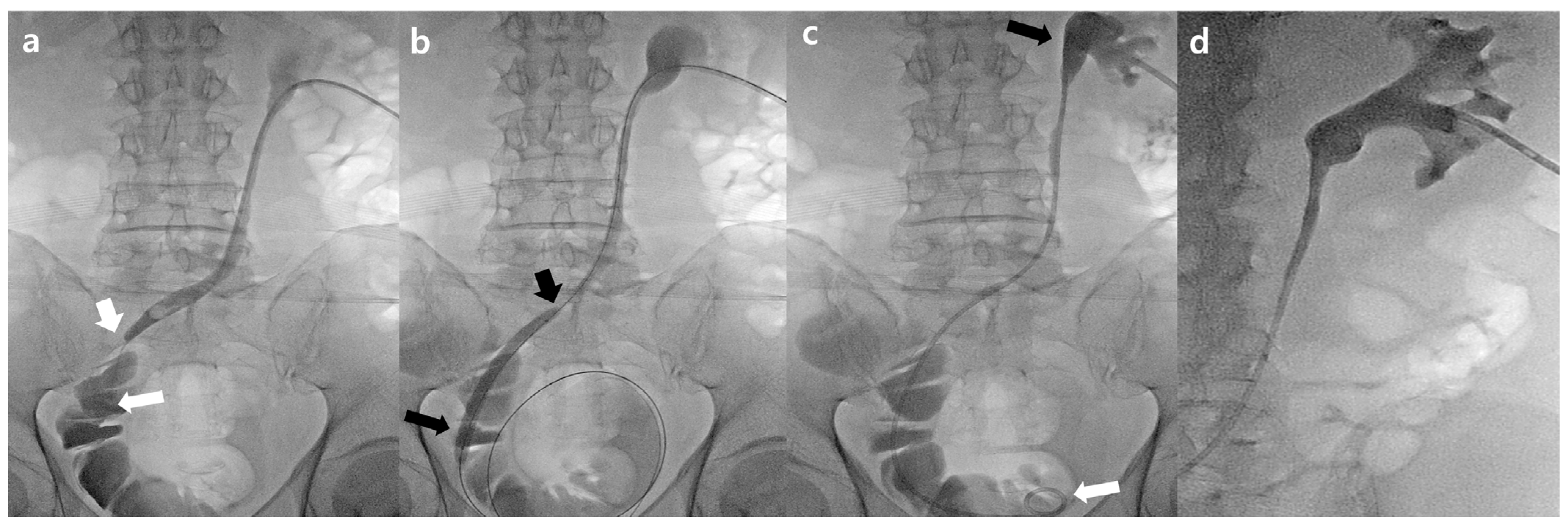
2.2. Procedure
2.3. Study Endpoints
2.4. Follow-Up
2.5. Statistical Analysis
3. Results
4. Discussion
5. Conclusions
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Conflicts of Interest
References
- Groeben, C.; Koch, R.; Baunacke, M.; Schmid, M.; Borkowetz, A.; Wirth, M.P.; Huber, J. Urinary diversion after radical cystectomy for bladder cancer: Comparing trends in the US and Germany from 2006 to 2014. Ann. Surg. Oncol. 2018, 25, 3502–3509. [Google Scholar] [CrossRef] [PubMed]
- Bachour, K.; Faiena, I.; Salmasi, A.; Lenis, A.T.; Johnson, D.C.; Pooli, A.; Drakaki, A.; Pantuck, A.J.; Chamie, K. Trends in urinary diversion after radical cystectomy for urothelial carcinoma. World J. Urol. 2018, 36, 409–416. [Google Scholar] [CrossRef] [PubMed]
- Micali, S.; De Carli, P.; Miano, R.; O’Sullivan, D.; Lamanna, L.; Micali, F. Double–J ureteral stents: An alternative to external urinary stents in orthotopic bladder substitution. Eur. Urol. 2001, 39, 575–579. [Google Scholar] [CrossRef] [PubMed]
- Varkarakis, I.M.; Delis, A.; Papatsoris, A.; Deliveliotis, C. Use of external ureteral catheters and internal double j stents in a modified ileal neobladder for continent diversion: A comparative analysis. Urol. Int. 2005, 75, 139–143. [Google Scholar] [CrossRef] [PubMed]
- Touiti, D.; Gelet, A.; Deligne, E.; Fassi-Fehri, H.; Benrais, H.; Martin, X.; Dubernard, J.-M. Treatment of uretero-intestinal and ureterovesical strictures by Acucise® balloon catheter. Eur. Urol. 2002, 42, 49–55. [Google Scholar] [CrossRef]
- De Sutter, T.; Akand, M.; Albersen, M.; Everaerts, W.; Van Cleynenbreugel, B.; De Ridder, D.; Goethuys, H.; Moris, L.; Milenkovic, U.; Van Poppel, H.; et al. The N-shaped orthotopic ileal neobladder: Functional outcomes and complication rates in 119 patients. SpringerPlus 2016, 5, 646. [Google Scholar] [CrossRef]
- Vickers, N.J. Animal communication: When I’m calling you, will you answer too? Curr. Biol. 2017, 27, R713–R715. [Google Scholar] [CrossRef]
- Pallwein, L.; Mitterberger, M.; Struve, P.; Pinggera, G.; Horninger, W.; Bartsch, G.; Aigner, F.; Lorenz, A.; Pedross, F.; Frauscher, F. Real-time elastography for detecting prostate cancer: Preliminary experience. BJU Int. 2007, 100, 42–46. [Google Scholar] [CrossRef]
- Lin, C.-M.; Tsai, T.-H.; Lin, T.-C.; Tang, S.-H.; Wu, S.-T.; Sun, G.-H.; Cha, T.-L. Holmium: Yttrium-aluminum-garnet laser endoureterotomy for benign ureteral strictures: A single-centre experience. Acta Chir. Belg. 2009, 109, 746–750. [Google Scholar] [CrossRef]
- Yu, H.-L.; Ye, L.-Y.; Lin, M.-H.; Yang, Y.; Miao, R.; Hu, X.-J. Treatment of benign ureteral stricture by double J stents using high-pressure balloon angioplasty. Chin. Med. J. 2011, 124, 943–946. [Google Scholar]
- Lucas, J.W.; Ghiraldi, E.; Ellis, J.; Friedlander, J.I. Endoscopic management of ureteral strictures: An update. Curr. Urol. Rep. 2018, 19, 24. [Google Scholar] [CrossRef] [PubMed]
- Zhao, P. Endoscopic management of ureteral stricture: NYU case of the month, August 2018. Rev. Urol. 2018, 20, 140. [Google Scholar] [PubMed]
- Wong, M.C.S.; Fung, F.D.H.; Leung, C.; Cheung, W.W.L.; Goggins, W.B.; Ng, C.F. The global epidemiology of bladder cancer: A joinpoint regression analysis of its incidence and mortality trends and projection. Sci. Rep. 2018, 8, 1129. [Google Scholar] [CrossRef] [PubMed]
- Onen, A. An alternative grading system to refine the criteria for severity of hydronephrosis and optimal treatment guidelines in neonates with primary UPJ-type hydronephrosis. J. Pediatr. Urol. 2007, 3, 200–205. [Google Scholar] [CrossRef] [PubMed]
- Sacks, D. Society of interventional radology clinical practice guidelines. J. Vasc. Interv. Radiol. 2003, 14, S199–S202. [Google Scholar] [CrossRef] [PubMed]
- Youn, S.Y.; Oh, J.S.; Lee, H.G.; Gil Choi, B.; Chun, H.J.; Kim, E.H. Primary and secondary percutaneous ureteral stent placement: Comparison of stent patency and clinical outcome. Cardiovasc. Interv. Radiol. 2018, 41, 130–136. [Google Scholar] [CrossRef]
- Liu, Z.; Zheng, B.; Hu, Y.; Li, H.; Qin, X.; Hu, X.; Wang, S.; Wang, H.; Zhang, P.; Wo, Q.; et al. The cause analysis of benign uretero-ileal anastomotic stricture after radical cystectomy and urinary diversion. Front. Oncol. 2022, 12, 1070141. [Google Scholar] [CrossRef]
- Large, M.C.; Cohn, J.A.; Kiriluk, K.J.; Dangle, P.; Richards, K.A.; Smith, N.D.; Steinberg, G.D. The impact of running versus interrupted anastomosis on ureterointestinal stricture rate after radical cystectomy. J. Urol. 2013, 190, 923–927. [Google Scholar] [CrossRef]
- Nassar, O.A.; Alsafa, M.E. Experience with ureteroenteric strictures after radical cystectomy and diversion: Open surgical revision. Urology 2011, 78, 459–465. [Google Scholar] [CrossRef]
- Lu, C.; Zhang, W.; Peng, Y.; Li, L.; Gao, X.; Liu, M.; Fang, Z.; Wang, Z.; Ming, S.; Dong, H.; et al. Endoscopic balloon dilatation in the treatment of benign ureteral strictures: A meta-analysis and systematic review. J. Endourol. 2019, 33, 255–262. [Google Scholar] [CrossRef]
- Peng, Y.; Li, X.; Li, X.; Zhang, C.; Yang, K.; Xiong, G.; Zhou, L.; Wang, G. Fluoroscopy-free minimally invasive ureteral stricture balloon dilatation: A retrospective safety and efficacy cohort study. Transl. Androl. Urol. 2021, 10, 2962–2969. [Google Scholar] [CrossRef] [PubMed]
- Yam, W.; Lim, S.; Teo, J.; Ng, K.; Ng, F. 130 Balloon dilatation of ureteric and ureteroileal strictures. Eur. Urol. Suppl. 2016, 15, e130. [Google Scholar] [CrossRef]
- Kuntz, N.J.; Neisius, A.; Tsivian, M.; Ghaffar, M.; Patel, N.; Ferrandino, M.N.; Sur, R.L.; Preminger, G.M.; Lipkin, M.E. Balloon dilation of the ureter: A contemporary review of outcomes and complications. J. Urol. 2015, 194, 413–417. [Google Scholar] [CrossRef] [PubMed]
- Li, J.; Chen, L.; Wang, X. Efficacy and safety of percutaneous renal access flexible ureteroscope plus balloon dilatation for patients with complex lower ureterostenosis. Zhonghua Yi Xue Za Zhi 2014, 94, 3642–3645. [Google Scholar] [PubMed]
- Hibi, H.; Yamada, Y.; Nonomura, H.; Hatano, Y.; Mitsui, K.; Taki, T.; Honda, N.; Fukatsu, H. Percutaneous ureteral incision with a small-caliber flexible ureteroscope. J. Soc. Laparoendosc. Surg. 2003, 7, 107–110. [Google Scholar]
- Lang, E.K. Factors influencing long-term results of transluminal dilatation or electrocautery incision with stenting of ureteral or ureteropelvic junction strictures. Minim. Invasive Ther. 1995, 4, 137–145. [Google Scholar] [CrossRef]
- Lang, E.K. Percutaneous ureterocystostomy and ureteroneocystostomy. Am. J. Roentgenol. 1988, 150, 1065–1068. [Google Scholar] [CrossRef]
- Richter, F.; Irwin, R.J.; A Watson, R.; Lang, E.K. Endourologic management of benign ureteral strictures with and without compromised vascular supply. Urology 2000, 55, 652–656. [Google Scholar] [CrossRef]
- Kunamneni, A.; Ravuri, B.; Saisha, V.; Ellaiah, P.; Prabhakhar, T. Urokinase-a very popular cardiovascular agent. Recent. Patents Cardiovasc. Drug Discov. 2008, 3, 45–58. [Google Scholar] [CrossRef]
- Lu, H.; Zheng, C.; Liang, B.; Xiong, B. Analysis of long-term effect of ureteral balloon dilatation combined with internal and external drainage tube in the treatment of benign ureteral stricture. BMC Urol. 2022, 22, 4. [Google Scholar] [CrossRef]
- Byun, S.S.; Kim, J.H.; Oh, S.J.; Kim, H.H. Simple retrograde balloon dilation for treatment of ureteral strictures: Etiology-based analysis. Yonsei Med. J. 2003, 44, 273–278. [Google Scholar] [CrossRef] [PubMed]
- Liu, J.S.; Hrebinko, R.L. The use of 2 ipsilateral ureteral stents for relief of ureteral obstruction from extrinsic compression. J. Urol. 1998, 159, 179–181. [Google Scholar] [CrossRef] [PubMed]
- Torre, L.A.; Bray, F.; Siegel, R.L.; Ferlay, J.; Lortet-Tieulent, J.; Jemal, A. Global cancer statistics, 2012. CA Cancer J. Clin. 2015, 65, 87–108. [Google Scholar] [CrossRef] [PubMed]




| Characteristics | N (%) |
|---|---|
| Sex (%) | |
| Male | 55 (87.3) |
| Female | 8 (12.7) |
| Age, years (range) | 68.8 ± 6.7 |
| ≤65 | 17 (27.0) |
| 66–75 | 34 (54.0) |
| >75 | 12 (19.0) |
| Hydronephrosis grade | |
| Mild | 15 (23.8) |
| Moderate | 35 (55.6) |
| Severe | 13 (20.6) |
| Blood clot retention grade | |
| 1 | 38 (60.3) |
| 2 | 18 (28.6) |
| 3 | 7 (11.1) |
| Direction of DJUS 1 | |
| Right | 24 (38.2) |
| Left | 39 (61.8) |
| Length of ureteral stricture | |
| Mild (<1 cm) | 18 (28.6) |
| Moderate (1–2 cm) | 15 (23.8) |
| Severe (>2 cm) | 30 (47.6) |
| Size of DJUS | |
| 6F | 29 (46.0) |
| 8F | 34 (54.0) |
| Type of DJUS | |
| Flexima | 15 (23.8) |
| Inlay Optima | 48 (76.2) |
| Balloon dilatation | |
| Yes | 30 (47.6) |
| No | 33 (52.4) |
| BUN before DJUS | 30.48 ± 15.27 |
| Cr before DJUS | 2.1 ± 1.4 |
| Characteristics | Univariate | Multivariate | ||
|---|---|---|---|---|
| OR (95% CI) | p | OR (95% CI) | p | |
| Sex | ||||
| Male | 2.000 (0.369–10.826) | 0.421 | ||
| Female | ||||
| Age | ||||
| ≤65 | 1 | 0.533 | ||
| 66–75 | 0.431 (0.062–3.012) | 0.396 | ||
| >75 | 0.333 (0.048–2.328) | 0.268 | ||
| Hydronephrosis | ||||
| Mild | 1 | 0.125 | ||
| Moderate | 0.600 (0.169–2.130) | 0.429 | ||
| Severe | 2.400 (0.524–10.992) | 0.259 | ||
| Blood clot retention grade | ||||
| 1 | 1 | 0.004 | 1 | 0.019 |
| 2 | 5.893 (1.727–20.106) | 0.005 | 6.922 (1.611–29.744) | 0.009 |
| 3 | 9.375 (1.525–57.621) | 0.016 | 5.543 (0.737–41.714) | 0.096 |
| Direction of DJUS | ||||
| Right | 0.960 (0.336–2.739) | 0.939 | ||
| Left | ||||
| Balloon dilatation | ||||
| Yes | 0.286 (0.097–0.850) | 0.024 | 0.186 (0.046–0.743) | 0.017 |
| No | ||||
| Length of ureteral stricture | ||||
| Mild (<1 cm) | 1 | 0.041 | 1 | 0.066 |
| Moderate (1–2 cm) | 7.000 (1.173–41.759) | 0.033 | 8.715 (1.164–65.226) | 0.035 |
| Severe (>2 cm) | 8.000 (1.560–41.033) | 0.013 | 7.646 (1.245–46.953) | 0.028 |
| Size of DJUS | ||||
| 6F | 0.752 (0.269–2.098) | 0.586 | ||
| 8F | ||||
| Type of DJUS | ||||
| Flexima | 1.596 (0.493–5.163) | 0.435 | ||
| Inlay Optima | ||||
| Characteristics | Univariate | Multivariate | ||
|---|---|---|---|---|
| OR (95% CI) | p | OR (95% CI) | p | |
| Sex | ||||
| Male | 1.927 (0.457–8.133) | 0.372 | ||
| Female | ||||
| Age | ||||
| ≤65 | 1 | 0.147 | ||
| 66–75 | 0.507 (0.226–1.134) | 0.098 | ||
| >75 | 0.390 (0.123–1.233) | 0.109 | ||
| Hydronephrosis | ||||
| Mild | 1 | 0.028 | 1 | 0.534 |
| Moderate | 0.936 (0.355–2.467) | 0.894 | 1.113 (0.415–2.989) | 0.831 |
| Severe | 2.869 (1.010–8.149) | 0.048 | 1.796 (0.578–5.578) | 0.311 |
| Blood clot retention grade | ||||
| 1 | 1 | <0.001 | 1 | <0.001 |
| 2 | 6.370 (2.732–14.852) | <0.001 | 6.044 (2.463–14.831) | <0.001 |
| 3 | 6.248 (1.868–20.902) | 0.003 | 6.330 (1.810–22.140) | 0.004 |
| Direction of DJUS | ||||
| Right | 0.646–1.413 | 0.820 | ||
| Left | ||||
| Balloon dilatation | ||||
| Yes | 0.836 (0.397–1.762) | 0.638 | ||
| No | ||||
| Length of ureteral stricture | ||||
| Mild (<1 cm) | 1 | 0.013 | 1 | 0.049 |
| Moderate (1–2 cm) | 4.386 (1.157–16.626) | 0.030 | 4.081 (1.054–15.798) | 0.042 |
| Severe (>2 cm) | 6.738 (1.889–24.032) | 0.003 | 5.518 (1.399–21.764) | 0.015 |
| Size of DJUS | ||||
| 6F | 0.900 (0.427–1.895) | 0.781 | ||
| 8F | ||||
| Type of DJUS | ||||
| Flexima | 1.783 (0.804–3.953) | 0.155 | ||
| Inlay Optima | ||||
Disclaimer/Publisher’s Note: The statements, opinions and data contained in all publications are solely those of the individual author(s) and contributor(s) and not of MDPI and/or the editor(s). MDPI and/or the editor(s) disclaim responsibility for any injury to people or property resulting from any ideas, methods, instructions or products referred to in the content. |
© 2023 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Kim, Y.; Oh, C.H.; Choi, S.L.; Kim, S. Percutaneous Ureteral Stent Insertion in Patients with Benign Uretero-Ileal Anastomosis Strictures Who Underwent Radical Cystectomy: Assessing Risk Factors for Stent Patency. J. Clin. Med. 2023, 12, 7721. https://doi.org/10.3390/jcm12247721
Kim Y, Oh CH, Choi SL, Kim S. Percutaneous Ureteral Stent Insertion in Patients with Benign Uretero-Ileal Anastomosis Strictures Who Underwent Radical Cystectomy: Assessing Risk Factors for Stent Patency. Journal of Clinical Medicine. 2023; 12(24):7721. https://doi.org/10.3390/jcm12247721
Chicago/Turabian StyleKim, Yebin, Chang Hoon Oh, Sang Lim Choi, and Sungwon Kim. 2023. "Percutaneous Ureteral Stent Insertion in Patients with Benign Uretero-Ileal Anastomosis Strictures Who Underwent Radical Cystectomy: Assessing Risk Factors for Stent Patency" Journal of Clinical Medicine 12, no. 24: 7721. https://doi.org/10.3390/jcm12247721
APA StyleKim, Y., Oh, C. H., Choi, S. L., & Kim, S. (2023). Percutaneous Ureteral Stent Insertion in Patients with Benign Uretero-Ileal Anastomosis Strictures Who Underwent Radical Cystectomy: Assessing Risk Factors for Stent Patency. Journal of Clinical Medicine, 12(24), 7721. https://doi.org/10.3390/jcm12247721






