Face Mask and Tear Film Stability: A Pilot Study of the Objective Measurement of Tear Break-Up Time
Abstract
:1. Introduction
2. Materials and Methods
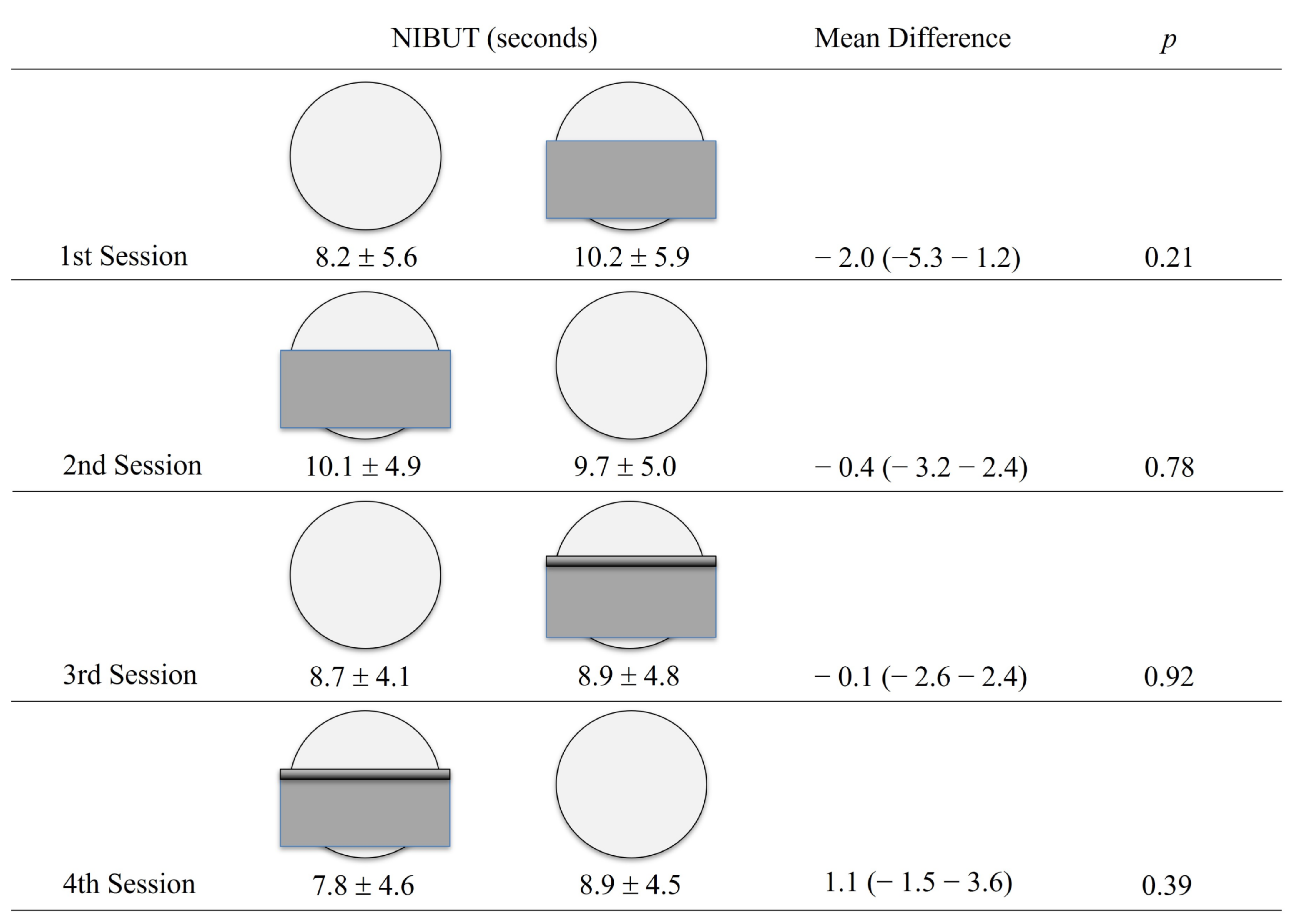
3. Results
4. Discussion
Supplementary Materials
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Conflicts of Interest
References
- WHO. Advice on the Use of Masks in the Context of COVID-19; WHO: Geneva, Switzerland, 2020; pp. 1–4. [Google Scholar]
- Patel, A.; Jernigan, D.B.; 2019-nCoV CDC Response Team. Initial Public Health Response and Interim Clinical Guidance for the 2019 Novel Coronavirus Outbreak—United States, December 31, 2019–February 4, 2020. MMWR Morb. Mortal Wkly. Rep. 2020, 69, 140–146. [Google Scholar] [CrossRef]
- Moshirfar, M.; West, W.B.; Marx, D.P. Face Mask-Associated Ocular Irritation and Dryness. Ophthalmol. Ther. 2020, 9, 397–400. [Google Scholar] [CrossRef]
- Boccardo, L. Self-reported symptoms of mask-associated dry eye: A survey study of 3605 people. Contact Lens Anterior Eye 2022, 45, 101408. [Google Scholar] [CrossRef]
- Pandey, S.; Sharma, V. Mask-associated dry eye disease and dry eye due to prolonged screen time: Are we heading towards a new dry eye epidemic during the COVID-19 era? Indian J. Ophthalmol. 2021, 69, 448. [Google Scholar] [CrossRef]
- Giannaccare, G.; Vaccaro, S.; Mancini, A.; Scorcia, V. Dry eye in the COVID-19 era: How the measures for controlling pandemic might harm ocular surface. Graefe’s Arch. Clin. Exp. Ophthalmol. 2020, 258, 2567–2568. [Google Scholar] [CrossRef]
- Krolo, I.; Blazeka, M.; Merdzo, I.; Vrtar, I.; Sabol, I.; Vickovic, I. Mask-Associated Dry Eye During COVID-19 Pandemic-How Face Masks Contribute to Dry Eye Disease Symptoms. Med. Arch. 2021, 75, 144. [Google Scholar] [CrossRef]
- Aksoy, M.; Simsek, M. Evaluation of Ocular Surface and Dry Eye Symptoms in Face Mask Users. Eye Contact Lens Sci. Clin. Pract. 2021, 47, 555–558. [Google Scholar] [CrossRef] [PubMed]
- Mastropasqua, L.; Lanzini, M.; Brescia, L.; D’Aloisio, R.; Nubile, M.; Ciancaglini, M.; D’Amario, C.; Agnifili, L.; Mastropasqua, R. Face Mask-Related Ocular Surface Modifications During COVID-19 Pandemic: A Clinical, In Vivo Confocal Microscopy, and Immune-Cytology Study. Transl. Vis. Sci. Technol. 2021, 10, 22. [Google Scholar] [CrossRef] [PubMed]
- Azzam, S.; Nama, A.; Badarni, H.; Asael, H.; Dahoud, W.; Mimouni, M.; Zayyad, H. Assessment of dry eye disease in N95 versus surgical face mask wearers during COVID-19. Indian J. Ophthalmol. 2022, 70, 995. [Google Scholar] [CrossRef] [PubMed]
- Nair, S.; Kaur, M.; Sah, R.; Titiyal, J.S. Impact of Taping The Upper Mask Edge On Ocular Surface Stability and Dry Eye Symptoms. Am. J. Ophthalmol. 2022, 238, 128–133. [Google Scholar] [CrossRef] [PubMed]
- Craig, J.P.; Nelson, J.D.; Azar, D.T.; Belmonte, C.; Bron, A.J.; Chauhan, S.K.; de Paiva, C.S.; Gomes, J.A.; Hammitt, K.M.; Jones, L.; et al. TFOS DEWS II Report Executive Summary. Ocul. Surf. 2017, 15, 802–812. [Google Scholar] [CrossRef] [PubMed]
- Chadwick, O.; Lockington, D. Addressing post-operative Mask-Associated Dry Eye (MADE). Eye 2021, 35, 1543–1544. [Google Scholar] [CrossRef] [PubMed]
- Silkiss, R.Z.; Paap, M.K.; Ugradar, S. Increased incidence of chalazion associated with face mask wear during the COVID-19 pandemic. Am. J. Ophthalmol. Case Rep. 2021, 22, 101032. [Google Scholar] [CrossRef] [PubMed]
- Bron, A.J.; de Paiva, C.S.; Chauhan, S.K.; Bonini, S.; Gabison, E.E.; Jain, S.; Knop, E.; Markoulli, M.; Ogawa, Y.; Perez, V.; et al. TFOS DEWS II pathophysiology report. Ocul. Surf. 2017, 15, 438–510. [Google Scholar] [CrossRef]
- Yokoi, N.; Georgiev, G.A. Tear Film–Oriented Diagnosis and Tear Film–Oriented Therapy for Dry Eye Based on Tear Film Dynamics. Investig. Opthalmol. Vis. Sci. 2018, 59, DES13. [Google Scholar] [CrossRef]
- Boulos, L.; Curran, J.A.; Gallant, A.; Wong, H.; Johnson, C.; Delahunty-Pike, A.; Saxinger, L.; Chu, D.; Comeau, J.; Flynn, T.; et al. Effectiveness of face masks for reducing transmission of SARS-CoV-2: A rapid systematic review. Philos. Trans. R. Soc. A Math. Phys. Eng. Sci. 2023, 381, 20230133. [Google Scholar] [CrossRef]
- Pan, X.; Li, X.; Kong, P.; Wang, L.; Deng, R.; Wen, B.; Xiao, L.; Song, H.; Sun, Y.; Zhou, H.; et al. Assessment of Use and Fit of Face Masks Among Individuals in Public During the COVID-19 Pandemic in China. JAMA Netw. Open 2021, 4, e212574. [Google Scholar] [CrossRef]
- Hayirci, E.; Yagci, A.; Palamar, M.; Basoglu, O.K.; Veral, A. The Effect of Continuous Positive Airway Pressure Treatment for Obstructive Sleep Apnea Syndrome on the Ocular Surface. Cornea 2012, 31, 604–608. [Google Scholar] [CrossRef]
- Singh, N.P.; Walker, R.J.E.; Cowan, F.; Davidson, A.C.; Roberts, D.N. Retrograde Air Escape via the Nasolacrimal System. Ann. Otol. Rhinol. Laryngol. 2014, 123, 321–324. [Google Scholar] [CrossRef]
- Maranhao, B.; Scott, A.W.; Scott, A.R.; Maeng, J.; Song, Z.; Baddigam, R.; King, C.R.; McCormick, M.; Kangrga, I.; Guffey, R. Probability of fit failure with reuse of N95 mask respirators. Br. J. Anaesth. 2020, 125, e322–e324. [Google Scholar] [CrossRef]
- Degesys, N.F.; Wang, R.C.; Kwan, E.; Fahimi, J.; Noble, J.A.; Raven, M.C. Correlation Between N95 Extended Use and Reuse and Fit Failure in an Emergency Department. JAMA 2020, 324, 94. [Google Scholar] [CrossRef]
- Karabagli, Y.; Kocman, E.A.; Kose, A.A.; Ozbayoglu, C.A.; Cetin, C. Adhesive Bands to Prevent Fogging of Lenses and Glasses of Surgical Loupes or Microscopes. Plast. Reconstr. Surg. 2006, 117, 718–719. [Google Scholar] [CrossRef]
- Bhardwaj, A.; Sharma, C.; Rajan, M.B. Simple solutions for the fogging of spectacles when wearing surgical masks. J. Am. Acad. Dermatol. 2021, 85, e237–e238. [Google Scholar] [CrossRef] [PubMed]
- Craig, J.P.; Nichols, K.K.; Akpek, E.K.; Caffery, B.; Dua, H.S.; Joo, C.K.; Liu, Z.; Nelson, J.D.; Nichols, J.J.; Tsubota, K.; et al. TFOS DEWS II Definition and Classification Report. Ocul. Surf. 2017, 15, 276–283. [Google Scholar] [CrossRef] [PubMed]
- Tsubota, K.; Yokoi, N.; Shimazaki, J.; Watanabe, H.; Dogru, M.; Yamada, M.; Kinoshita, S.; Kim, H.-M.; Tchah, H.-W.; Hyon, J.Y.; et al. New Perspectives on Dry Eye Definition and Diagnosis: A Consensus Report by the Asia Dry Eye Society. Ocul. Surf. 2017, 15, 65–76. [Google Scholar] [CrossRef] [PubMed]
- Mengher, L.S.; Bron, A.J.; Tonge, S.R.; Gilbert, D.J. A non-invasive instrument for clinical assessment of the pre-corneal tear film stability. Curr. Eye Res. 1985, 4, 1127–1128. [Google Scholar] [CrossRef] [PubMed]
- Sweeney, D.F.; Millar, T.J.; Raju, S.R. Tear film stability: A review. Exp. Eye Res. 2013, 117, 28–38. [Google Scholar] [CrossRef] [PubMed]
- Kim, J.; Kim, J.Y.; Seo, K.Y.; Kim, T.; Chin, H.S.; Jung, J.W. Location and pattern of non-invasive keratographic tear film break-up according to dry eye disease subtypes. Acta Ophthalmol. 2019, 97, E1089–E1097. [Google Scholar] [CrossRef]
- Alfaro-Juárez, A.; Caro-Magdaleno, M.; Montero-Iruzubieta, J.; Fernández-Palacín, A.; Muñoz-Morales, A.; Castilla-Martino, M.A.; de la Rúa, E.R. Keratograph 5M As A Useful And Objective Tool For Evaluating The Ocular Surface In Limbal Stem Cell Deficiency. Clin. Ophthalmol. 2019, 13, 2025–2033. [Google Scholar] [CrossRef]
- García-Montero, M.; Rico-del-Viejo, L.; Lorente-Velázquez, A.; Martínez-Alberquilla, I.; Hernández-Verdejo, J.L.; Madrid-Costa, D. Repeatability of Noninvasive Keratograph 5M Measurements Associated with Contact Lens Wear. Eye Contact Lens Sci. Clin. Pract. 2019, 45, 377–381. [Google Scholar] [CrossRef]
- Fernández, J.; Rodríguez-Vallejo, M.; Martínez, J.; Tauste, A.; García-Montesinos, J.; Piñero, D.P. Agreement and repeatability of objective systems for assessment of the tear film. Graefe’s Arch. Clin. Exp. Ophthalmol. 2018, 256, 1535–1541. [Google Scholar] [CrossRef]
- Vidas Pauk, S.; Petriček, I.; Jukić, T.; Popović-Suić, S.; Tomić, M.; Kalauz, M.; Jandroković, S.; Masnec, S. Noninvasive Tear Film Break-Up Time Assessment Using Handheld Lipid Layer Examination Instrument. Acta Clin. Croat. 2019, 58, 63–71. [Google Scholar] [CrossRef]
- Tian, L.; Qu, J.; Zhang, X.; Sun, X. Repeatability and Reproducibility of Noninvasive Keratograph 5M Measurements in Patients with Dry Eye Disease. J. Ophthalmol. 2016, 2016, 8013621. [Google Scholar] [CrossRef]
- Brissette, A.R.; Drinkwater, O.J.; Bohm, K.J.; Starr, C.E. The utility of a normal tear osmolarity test in patients presenting with dry eye disease like symptoms: A prospective analysis. Contact Lens Anterior Eye 2019, 42, 185–189. [Google Scholar] [CrossRef]
- Arriola-Villalobos, P.; Burgos-Blasco, B.; Vidal-Villegas, B.; Oribio-Quinto, C.; Ariño-Gutiérrez, M.; Diaz-Valle, D.; Benitez-Del-Castillo, J.M. Effect of Face Mask on Tear Film Stability in Eyes with Moderate-to-Severe Dry Eye Disease. Cornea 2021, 40, 1336–1339. [Google Scholar] [CrossRef]
- García-Marqués, J.V.; Martínez-Albert, N.; Talens-Estarelles, C.; García-Lázaro, S.; Cerviño, A. Repeatability of Non-invasive Keratograph Break-Up Time measurements obtained using Oculus Keratograph 5M. Int. Ophthalmol. 2021, 41, 2473–2483. [Google Scholar] [CrossRef]
- Sutphin, J.E.; Ying, G.S.; Bunya, V.Y.; Yu, Y.; Lin, M.C.; McWilliams, K.; Schmucker, E.; Kuklinski, E.J.; Asbell, P.A.; Maguire, M.G. Correlation of Measures from the OCULUS Keratograph and Clinical Assessments of Dry Eye Disease in the Dry Eye Assessment and Management Study. Cornea 2022, 41, 845–851. [Google Scholar] [CrossRef]
- Faul, F.; Erdfelder, E.; Buchner, A.; Lang, A.G. Statistical power analyses using G*Power 3.1: Tests for correlation and regression analyses. Behav. Res. Methods 2009, 41, 1149–1160. [Google Scholar]
- Nichols, K.K.; Nichols, J.J.; Mph, M.; Mitchell, G.L. The Lack of Association Between Signs and Symptoms in Patients with Dry Eye Disease. Cornea 2004, 23, 762–770. [Google Scholar] [CrossRef]
- Song, H.; Zhang, M.; Hu, X.; Li, K.; Jiang, X.; Liu, Y.; Lv, H.; Li, X. Correlation Analysis of Ocular Symptoms and Signs in Patients with Dry Eye. J. Ophthalmol. 2017, 2017, 1247138. [Google Scholar] [CrossRef]
- Scalinci, S.; Pacella, E.; Battagliola, E. Prolonged face mask use might worsen dry eye symptoms. Indian J. Ophthalmol. 2021, 69, 1508. [Google Scholar] [CrossRef]
- Esen Baris, M.; Guven Yilmaz, S.; Palamar, M. Impact of prolonged face mask wearing on tear break-up time and dry eye symptoms in health care professionals. Int. Ophthalmol. 2022, 42, 2141–2144. [Google Scholar] [CrossRef]
- Mbithi, F.; Worsley, P.R. Adhesives for medical application—Peel strength testing and evaluation of biophysical skin response. J. Mech. Behav. Biomed. Mater. 2023, 148, 106168. [Google Scholar] [CrossRef]
- Hou, J.; Zhang, N.; Li, X.; Wang, Z.; Wang, J. The Effects of Spectacles or Orthokeratology on the Tear Film in Children and Adolescents. Ophthalmol. Ther. 2023, 12, 1913–1927. [Google Scholar] [CrossRef]
- Fattoh, R.; Mounir, A.; Anbar, M.; Mohammed, O.A. Changes in Noncontact Meibography and Noninvasive Tear Break-Up Time Test with Contact Lenses Usage. Clin. Ophthalmol. 2022, 16, 1427–1437. [Google Scholar] [CrossRef]
- Maldonado-Codina, C.; Navascues-Cornago, M.; Plowright, A.J.; Mirza, A.; Smith, S.; Read, M.L.; Vega, J.; Orsborn, G.N.; Morgan, P.B. Using face masks with spectacles versus contact lenses. Contact Lens Anterior Eye 2022, 45, 101516. [Google Scholar] [CrossRef]
- Martinez-Perez, C.; Monteiro, B.; Soares, M.; Portugues, F.; Matos, S.; Ferreira, A.; Alvarez-Peregrina, C.; Sánchez-Tena, M. Influence of Face Masks on the Use of Contact Lenses. Int. J. Environ. Res. Public Health 2021, 18, 7407. [Google Scholar] [CrossRef]
| NIBUT Mean ± SD (Seconds) | |
|---|---|
| No face mask | 8.9 ± 3.7 |
| Face mask | 10.2 ± 4.1 |
| Tape-secured face mask | 8.4 ± 3.8 |
| Mean Dif. (95% CI); p | |
| No face mask vs. face mask | −1.2 (−3.4–0.9); p = 0.24 |
| No face mask vs. tape-secured face mask | 0.5 (−1.5–2.6); p = 0.91 |
| Face mask vs. tape-secured face mask | −1.8 (−4.0–0.3); p = 0.11 |
| Author. [Reference] | Year, Country | N=, Population | Evaluation | Key Comments and Findings |
|---|---|---|---|---|
| Moshirfar M. et al. [3] | 2020, USA | 0 | None | Face mask could produce ocular irritation and dryness |
| Boccardo L. et al. [4] | 2022, Italy | 3605, general population | Survey | 18.3% experienced MADE. Those with previous DED symptoms were more likely to have worsening of DED symptoms. |
| Chadwick O. et al. [5] | 2020, UK | 1 | Comment/ Case report | Ill-fitting face masks can cause exposure keratopathy in the setting of an anesthetized cornea |
| Giannaccare G. et al. [7] | 2020, Italy | 107, medical students | Survey/Letter to the editor | 24.3% used VDT in the last month for 6 h/day or more. 67.3% wore face mask > 6 h/day. 10.3% described appearance or worsening of ocular discomfort symptoms, 19.6% reported the need for daily use of tear substitutes. OSDI scored ≥ 15 (pathological) was 21, 57%. Mixed causes for DED were observed: DES and face mask use. |
| Pandey S. et al. [5] | 2021, India | 0 | Letter to the editor | Important to use face mask properly. Mixed component for the increase on DED in the pandemic, DES and face mask use. |
| Scalinci S. et al. [28] | 2021, Italy | 67, previous DED | Survey: OSDI | Retrospective comparison of OSDI scores in spring 2019 (pre pandemic) vs. spring 2020 (pandemic). Heavy face mask use (≥6 h/day, and ≥5 day/week, in the last 2 months, is associated with an increase in OSDI scores. |
| Krolo I. et al. [29] | 2021, Croatia | 203, patients attending eye clinic | Survey: Modified OSDI | Surgical face mask use 3–6 h/day had higher OSDI compared to <3 h/day use:15.3 (IQR = 8.3–47.7) vs. 8.3 (IQR = 0.0–35.1); p = 0.001). Prior DED had greater worsening of OSDI during face mask use (54.8% vs. 17.7%; p < 0.001). Approximately half experienced worsening of DED symptoms while wearing face mask. |
| Aksoy M. et al. [31] | 2021, Turkey | 52, outpatient | FBUT, OSDI, DED tests. | 3-layered face mask users >8 h/day had significant reduction in FBUT compared with the beginning of the day before face mask use. Taping down the mask improved FBUT. No control group. |
| Mastropasqua L. et al. [30] | 2021, Italy | 62 DED, 62 non-DED healthy | FBUT, DEQS, DED tests | The greater the use of surgical face mask, the more FBUT, symptoms and other DED parameters were reduced in healthy and DED patients. After 3 months of face mask use, only those using >6 h/day had significant FBUT reductions. No control group. |
| Nair S. et al. [36] | 2022, India | 50, Healthy workers | NIBUT, OSDI, other tests | N95 face mask. Taping of the upper face mask edge results in significantly better ocular surface stability and decrease in DED symptoms |
| Arriola-Villalobos P. et al. [33] | 2021, Spain | 31, DED | TBUT, and other tests | Removal of face mask for 10 min improves tear film stability in patients with moderate-to-severe DED. |
| Azzam S. et al. [34] | 2022, Israel | 30 surgical mask, 30 n95. Health-care workers | TBU, DED signs and symptoms | Cross-sectional study. Both types of face masks had reduced FBUT, but the N95 face mask users had greater reductions on TBUT (p < 0.042) and fluorescein staining (p < 0.038). |
| Esen Baris M. et al. [32] | 2022, Turkey | 66 eyes of 33 subjects | TBUT and other signs | Significant reduction in FBUT after 9 h of face mask use when compared to basal evaluation with face mask at the start of the day. |
| This study. Mohamed-Noriega. et al. | 2023, Mexico | 26 eyes, 26 health-care workers | NIBUT | No significant short-term differences were observed on NIBUT between using surgical face mask, after removal of face mask or after securing face mask with adhesive tape |
Disclaimer/Publisher’s Note: The statements, opinions and data contained in all publications are solely those of the individual author(s) and contributor(s) and not of MDPI and/or the editor(s). MDPI and/or the editor(s) disclaim responsibility for any injury to people or property resulting from any ideas, methods, instructions or products referred to in the content. |
© 2023 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Mohamed-Noriega, K.; Charles-Cantu, D.E.; Mohamed-Noriega, J.; Velasco-Sepúlveda, B.H.; Morales-Wong, F.; Villarreal-Méndez, G.; Mohamed-Hamsho, J. Face Mask and Tear Film Stability: A Pilot Study of the Objective Measurement of Tear Break-Up Time. J. Clin. Med. 2023, 12, 7727. https://doi.org/10.3390/jcm12247727
Mohamed-Noriega K, Charles-Cantu DE, Mohamed-Noriega J, Velasco-Sepúlveda BH, Morales-Wong F, Villarreal-Méndez G, Mohamed-Hamsho J. Face Mask and Tear Film Stability: A Pilot Study of the Objective Measurement of Tear Break-Up Time. Journal of Clinical Medicine. 2023; 12(24):7727. https://doi.org/10.3390/jcm12247727
Chicago/Turabian StyleMohamed-Noriega, Karim, David E. Charles-Cantu, Jibran Mohamed-Noriega, Braulio H. Velasco-Sepúlveda, Fernando Morales-Wong, Gerardo Villarreal-Méndez, and Jesús Mohamed-Hamsho. 2023. "Face Mask and Tear Film Stability: A Pilot Study of the Objective Measurement of Tear Break-Up Time" Journal of Clinical Medicine 12, no. 24: 7727. https://doi.org/10.3390/jcm12247727
APA StyleMohamed-Noriega, K., Charles-Cantu, D. E., Mohamed-Noriega, J., Velasco-Sepúlveda, B. H., Morales-Wong, F., Villarreal-Méndez, G., & Mohamed-Hamsho, J. (2023). Face Mask and Tear Film Stability: A Pilot Study of the Objective Measurement of Tear Break-Up Time. Journal of Clinical Medicine, 12(24), 7727. https://doi.org/10.3390/jcm12247727






