The Negative Impact of Inflammation-Related Parameters in Prostate Cancer after Robot-Assisted Radical Prostatectomy: A Retrospective Multicenter Cohort Study in Japan (the MSUG94 Group)
Abstract
1. Introduction
2. Materials and Methods
2.1. Patient Population
2.2. Pathological Analysis
2.3. Follow-Up Schedule
2.4. Endpoints and Statistics
3. Results
3.1. Patient Characteristics
3.2. Oncological Outcomes
4. Discussion
5. Conclusions
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Conflicts of Interest
References
- Zhou, M.; Liang, J.; Hui, J.; Xu, J. Inflammation-related indicators have a potential to increase overall quality of the prostate cancer management: A narrative review. Transl. Androl. Urol. 2023, 12, 809–822. [Google Scholar] [CrossRef]
- Kawase, M.; Goto, T.; Ebara, S.; Tatenuma, T.; Sasaki, T.; Ishihara, T.; Ikehata, Y.; Nakayama, A.; Toide, M.; Yoneda, T.; et al. Nomogram Predicting Locally Advanced Prostate Cancer in Patients with Clinically Organ-Confined Disease Who Underwent Robot-Assisted Radical Prostatectomy: A Retrospective Multicenter Cohort Study in Japan (The MSUG94 Group). Ann. Surg. Oncol. 2023, 30, 6925–6933. [Google Scholar] [CrossRef] [PubMed]
- Hashine, K.; Yamashita, N.; Tachou, T.; Kan, M.; Yanagaki, T.; Oka, A.; Takeda, H.; Shirato, A.; Watanabe, U.; Noriyoshi Miura, N.; et al. Radical prostatectomy trends between 2010 and 2020 in Ehime, Japan, identified using data from the Medical Investigation Cancer Network (MICAN) study. Int. J. Urol. 2023, 30, 547–553. [Google Scholar] [CrossRef] [PubMed]
- Kawase, M.; Ebara, S.; Tatenuma, T.; Sasaki, T.; Ikehata, Y.; Nakayama, A.; Toide, M.; Yoneda, T.; Sakaguchi, K.; Ishihara, T.; et al. A Nomogram for Predicting Prostate Cancer with Lymph Node Involvement in Robot-Assisted Radical Prostatectomy Era: A Retrospective Multicenter Cohort Study in Japan (The MSUG94 Group). Diagnostics 2022, 12, 2545. [Google Scholar] [CrossRef] [PubMed]
- Goto, Y.; Utsumi, T.; Maruo, M.; Kurozumi, A.; Noro, T.; Tanaka, S.; Sugawara, S.; Chiba, K.; Miyazaki, K.; Inoue, A.; et al. Development and validation of novel nomogram to identify the candidates for extended pelvic lymph node dissection for prostate cancer patients in the robotic era. Int. J. Urol. 2023, 30, 659–665. [Google Scholar] [CrossRef] [PubMed]
- Tomioka-Inagawa, R.; Nakane, K.; Enomoto, T.; Tomioka, M.; Taniguchi, T.; Ishida, T.; Ozawa, K.; Takagi, K.; Ito, H.; Takeuchi, S.; et al. The Impact of Neutrophil-to-Lymphocyte Ratio after Two Courses of Pembrolizumab for Oncological Outcomes in Patients with Metastatic Urothelial Carcinoma. Biomedicines 2022, 10, 1609. [Google Scholar] [CrossRef] [PubMed]
- Iinuma, K.; Enomoto, T.; Kawada, K.; Fujimoto, S.; Ishida, T.; Takagi, K.; Nagai, S.; Ito, H.; Kawase, M.; Nakai, C.; et al. Utility of Neutrophil-to-Lymphocyte Ratio, Platelet-to-Lymphocyte Ratio, and Systemic Immune Inflammation Index as Prognostic, Predictive Biomarkers in Patients with Metastatic Renal Cell Carcinoma Treated with Nivolumab and Ipilimumab. J. Clin. Med. 2021, 10, 5325. [Google Scholar] [CrossRef]
- Samejima, H.; Kojima, K.; Fujiwara, A.; Tokunaga, T.; Okishio, K.; Yoon, H. The combination of PD-L1 expression and the neutrophil-to-lymphocyte ratio as a prognostic factor of postoperative recurrence in non-small-cell lung cancer: A retrospective cohort study. BMC Cancer 2023, 23, 1107. [Google Scholar] [CrossRef]
- Tacconi, F.; Mangiameli, G.; Voulaz, E.; Patirelis, A.; Carlea, F.; Rocca, E.; Tamburrini, A.; Vanni, G.; Ambrogi, V. Blood-Derived Systemic Inflammation Markers and Risk of Nodal Failure in Stage Ia Non-Small Cell Lung Cancer: A Multicentric Study. J. Clin. Med. 2023, 12, 4912. [Google Scholar] [CrossRef]
- Jadoon, S.K.; Soomro, R.; Ahsan, M.N.; Ijaz Khan, R.M.; Iqbal, S.; Yasmin, F.; Najeeb, H.; Saleem, N.; Cho, N.; Resham; et al. Association of neutrophil-to-lymphocyte ratio with clinical, pathological, radiological, laboratory features and disease outcomes of invasive breast cancer patients: A retrospective observational cohort study. Medicine 2023, 102, e33811. [Google Scholar] [CrossRef]
- Nakane, K.; Watanabe, H.; Naiki, T.; Takahara, K.; Yasui, T.; Miyake, H.; Shiroki, R.; Koie, T. Trends in the Use of Second-Generation Androgen Receptor Axis Inhibitors for Metastatic Hormone-Sensitive Prostate Cancer and Clinical Factors Predicting Biological Recurrence. Diagnostics 2023, 13, 1661. [Google Scholar] [CrossRef] [PubMed]
- Wang, S.; Yang, X.; Yu, Z.; Du, P.; Cao, Y.; Ji, Y.; Ma, J.; Yang, Y. The values of systemic immune-inflammation index and neutrophil-lymphocyte ratio in predicting testicular germ cell tumors: A retrospective clinical study. Front. Oncol. 2022, 12, 893877. [Google Scholar] [CrossRef] [PubMed]
- Lu, Y.; Huang, H.H.; Lau, W.K.O. Evaluation of neutrophil-to-lymphocyte ratio as a prognostic indicator in a Singapore cohort of patients with clinically localized prostate cancer treated with prostatectomy. World J. Urol. 2020, 38, 103–109. [Google Scholar] [CrossRef] [PubMed]
- Wang, S.; Ji, Y.; Ma, J.; Du, P.; Cao, Y.; Yang, X.; Yu, Z.; Yang, Y. Role of inflammatory factors in prediction of Gleason score and its upgrading in localized prostate cancer patients after radical prostatectomy. Front. Oncol. 2023, 12, 1079622. [Google Scholar] [CrossRef] [PubMed]
- Cao, Z.; Ji, J.; Zhang, C.; Wang, F.; Xu, H.; Yu, Y.; Sun, Y. The preoperative neutrophil-to-lymphocyte ratio is not a marker of prostate cancer characteristics but is an independent predictor of biochemical recurrence in patients receiving radical prostatectomy. Cancer Med. 2019, 8, 1004–1012. [Google Scholar] [CrossRef] [PubMed]
- Maeda, Y.; Kawahara, T.; Koizumi, M.; Ito, H.; Kumano, Y.; Ohtaka, M.; Kondo, T.; Mochizuki, T.; Hattori, Y.; Teranishi, J.; et al. Lack of an Association between Neutrophil-to-Lymphocyte Ratio and PSA Failure of Prostate Cancer Patients Who Underwent Radical Prostatectomy. Biomed. Res. Int. 2016, 2016, 6197353. [Google Scholar] [CrossRef] [PubMed][Green Version]
- Crusz, S.M.; Balkwill, F.R. Inflammation and cancer: Advances and new agents. Nat. Rev. Clin. Oncol. 2015, 12, 584–596. [Google Scholar] [CrossRef]
- Lu, G.; Cai, W.; Wang, X.; Huang, B.; Zhao, Y.; Shao, Y.; Wang, D. Identifying prognostic signatures in the microenvironment of prostate cancer. Transl. Androl. Urol. 2021, 10, 4206–4218. [Google Scholar] [CrossRef]
- Oken, M.M.; Creech, R.H.; Tormey, D.C.; Horton, J.; Davis, T.E.; McFadden, E.T.; Carbone, P.P. Toxicity and response criteria of the Eastern Cooperative Oncology Group. Am. J. Clin. Oncol. 1982, 5, 649–655. [Google Scholar] [CrossRef]
- Epstein, J.I.; Egevad, L.; Amin, M.B.; Delahunt, B.; Srigley, J.; Humphrey, P.A.; Committee, G. The 2014 International Society of Urological Pathology (ISUP) Consensus Conference on Gleason Grading of Prostatic Carcinoma: Definition of Grading Patterns and Proposal for a New Grading System. Am. J. Surg. Pathol. 2016, 40, 244–252. [Google Scholar] [CrossRef]
- Prostate Cancer. NCCN Guidelines®. 2022. Available online: https://www.nccn.org/guidelines/guidelines-process/transparency-process-and-recommendations/GetFileFromFileManager?fileManagerId=12813 (accessed on 6 November 2023).
- Buyyounouski, M.K.; Choyke, P.L.; McKenney, J.K.; Sartor, O.; Sandler, H.M.; Amin, M.B.; Kattan, M.W.; Lin, D.W. Prostate cancer—Major changes in the American Joint Committee on Cancer eighth edition cancer staging manual. CA Cancer J. Clin. 2017, 67, 245–253. [Google Scholar] [CrossRef] [PubMed]
- Perkins, N.J.; Schisterman, E.F. The inconsistency of “optimal” cutpoints obtained using two criteria based on the receiver operating characteristic curve. Am. J. Epidemiol. 2006, 163, 670–675. [Google Scholar] [CrossRef] [PubMed]
- Templeton, A.J.; McNamara, M.G.; Šeruga, B.; Vera-Badillo, F.E.; Aneja, P.; Ocaña, A.; Leibowitz-Amit, R.; Sonpavde, G.; Knox, J.J.; Tran, B.; et al. Prognostic role of neutrophil-to-lymphocyte ratio in solid tumors: A systematic review and meta-analysis. J. Natl. Cancer Inst. 2014, 106, dju124. [Google Scholar] [CrossRef] [PubMed]
- Salazar-Onfray, F.; López, M.N.; Mendoza-Naranjo, A. Paradoxical effects of cytokines in tumor immune surveillance and tumor immune escape. Cytokine Growth Factor Rev. 2007, 18, 171–182. [Google Scholar] [CrossRef] [PubMed]
- Shu, K.; Zheng, Y.; Chen, J.; Li, W.; Jiang, K. Prognostic value of selected preoperative inflammation-based scores in patients with high-risk localized prostate cancer who underwent radical prostatectomy. OncoTargets Ther. 2018, 11, 4551–4558. [Google Scholar] [CrossRef] [PubMed]
- Gregory, A.D.; Houghton, A.M. Tumor-associated neutrophils: New targets for cancer therapy. Cancer Res. 2011, 71, 2411–2416. [Google Scholar] [CrossRef] [PubMed]
- Cools-Lartigue, J.; Spicer, J.; McDonald, B.; Gowing, S.; Chow, S.; Giannias, B.; Bourdeau, F.; Kubes, P.; Ferri, L. Neutrophil extracellular traps sequester circulating tumor cells and promote metastasis. J. Clin. Investig. 2013, 123, 3446–3458. [Google Scholar] [CrossRef]
- Battinelli, E.M.; Markens, B.A.; Italiano, J.E., Jr. Release of angiogenesis regulatory proteins from platelet alpha granules: Modulation of physiologic and pathologic angiogenesis. Blood 2011, 118, 1359–1369. [Google Scholar] [CrossRef]
- Gay, L.J.; Felding-Habermann, B. Contribution of platelets to tumour metastasis. Nat. Rev. Cancer 2011, 11, 123–134. [Google Scholar] [CrossRef]
- Peng, H.; Luo, X. Prognostic significance of elevated pretreatment systemic inflammatory markers for patients with prostate cancer: A meta-analysis. Cancer Cell Int. 2019, 19, 70. [Google Scholar] [CrossRef]
- Zhang, G.M.; Zhu, Y.; Ma, X.C.; Qin, X.J.; Wan, F.N.; Dai, B.; Sun, L.J.; Ye, D.W. Pretreatment Neutrophil-to-Lymphocyte Ratio: A Predictor of Advanced Prostate Cancer and Biochemical Recurrence in Patients Receiving Radical Prostatectomy. Medicine 2015, 94, e1473. [Google Scholar] [CrossRef] [PubMed]
- Kwon, Y.S.; Han, C.S.; Yu, J.W.; Kim, S.; Modi, P.; Davis, R.; Park, J.H.; Lee, P.; Ha, Y.S.; Kim, W.J.; et al. Neutrophil and Lymphocyte Counts as Clinical Markers for Stratifying Low-Risk Prostate Cancer. Clin. Genitourin. Cancer 2016, 14, e1–e8. [Google Scholar] [CrossRef] [PubMed]

| Age (year, median, IQR) | 68 (64–72) |
| Body mass index (kg/m2, median, IQR) | 23.5 (21.7–25.5) |
| ECOG-PS (number, %) | |
| 0 | 2356 (97.0) |
| 1 | 73 (3.0) |
| Initial PSA (ng/mL, median, IQR) | 7.6 (5.6–11.3) |
| Prostate volume (mL, median, IQR) | 30 (23–40) |
| Biopsy Gleason grade group (number, %) | |
| 1 | 529 (21.8) |
| 2 | 770 (31.7) |
| 3 | 511 (21.0) |
| 4 | 468 (19.3) |
| 5 | 151 (6.2) |
| Clinical T stage (number, %) | |
| 1 | 494 (20.4) |
| 2 | 1769 (72.9) |
| 3 | 164 (6.8) |
| Unknown | 2 (0.08) |
| CRP (mg/dL, median, IQR) | 0.07 (0.03–0.11) |
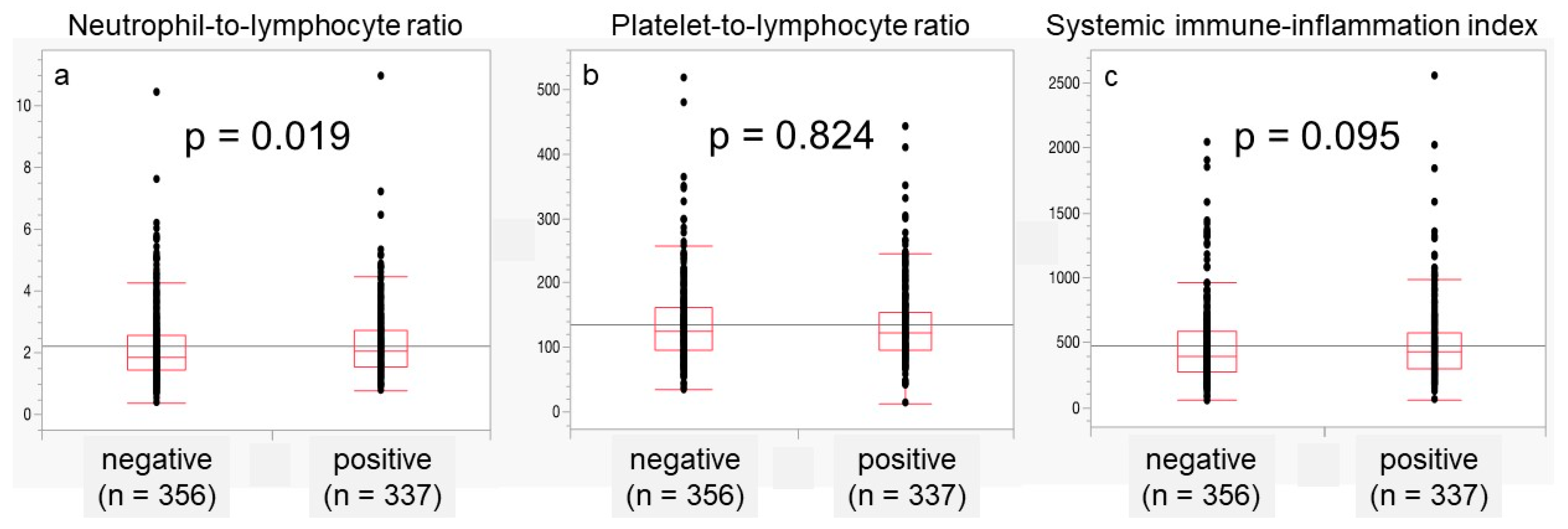
| NLR (median, IQR) | 2.01 (1.54–2.73) |
| PLR (median, IQR) | 129 (101–166) |
| SII (median, IQR) | 426 (306–587) |
| Pathological Gleason grade group (number, %) | |
| 1 | 188 (7.8) |
| 2 | 982 (40.6) |
| 3 | 788 (32.6) |
| 4 | 260 (10.7) |
| 5 | 201 (8.3) |
| Unknown | 10 (4.1) |
| Pathological T stage (number, %) | |
| 0 | 3 (0.1) |
| 2 | 1732 (71.3) |
| 3 | 688 (28.3) |
| 4 | 5 (0.2) |
| Unknown | 1 (0.04) |
| Pelvic lymphadenectomy (number, %) | |
| Not performed | 793 (32.6) |
| Performed | 1636 (67.4) |
| Unknown | 1 (0.04) |
| LVI (number, %) | 740 (30.5) |
| Follow-up period (months, median, IQR) | 25.1 (11.9–49.7) |
| NLR < 2.01 (n = 1211) | NLR ≥ 2.01 (n = 1218) | p-Value | |
|---|---|---|---|
| Age (year, median, IQR) | 68 (64–72) | 69 (65–73) | <0.001 |
| Body mass index (kg/m2, median, IQR) | 23.8 (22.0–25.8) | 23.3 (21.5–25.3) | <0.001 |
| ECOG-PS (number, %) | 0.420 | ||
| 0 | 1178 (97.3) | 1178 (96.7) | |
| 1 | 33 (2.7) | 40 (3.3) | |
| Initial PSA (ng/mL, median, IQR) | 7.5 (5.5–11.2) | 7.7 (5.7–11.3) | 0.107 |
| Prostate volume (mL, median, IQR) | 30 (22–39) | 30 (23–40) | 0.201 |
| Biopsy Gleason grade group (number, %) | 0.245 | ||
| 1 | 251 (20.7) | 278 (22.8) | |
| 2 | 397 (32.8) | 373 (30.6) | |
| 3 | 240 (19.8) | 271 (22.2) | |
| 4 | 247 (20.4) | 221 (18.1) | |
| 5 | 76 (6.3) | 75 (6.2) | |
| Clinical T stage (number, %) | 0.327 | ||
| 1 | 232 (19.2) | 262 (21.6) | |
| 2 | 894 (73.8) | 875 (72.0) | |
| 3 | 85 (7.0) | 79 (6.5) | |
| Unknown | 0 (0) | 2 (0.2) | |
| CRP (mg/dL, median, IQR) | 0.06 (0.03–0.10) | 0.07 (0.03–0.12) | 0.001 |
| PLR (median, IQR) | 107 (86–132) | 153 (125 –93) | < 0.001 |
| SII (median, IQR) | 310 (241–382) | 582 (475–747) | < 0.001 |
| Pathological Gleason grade group (number, %) | 0.294 | ||
| 1 | 94 (7.8) | 94(7.7) | |
| 2 | 498 (41.3) | 484 (39.9) | |
| 3 | 369 (30.6) | 419 (34.5) | |
| 4 | 137 (11.4) | 123 (10.1) | |
| 5 | 107 (8.9) | 94 (7.7) | |
| Unknown | 6 (0.5) | 4 (0.3) | |
| Pathological T stage (number, %) | 0.375 | ||
| 0 | 1 (0.1) | 2 (0.2) | |
| 2 | 846 (69.9) | 886 (72.7) | |
| 3 | 360 (29.8) | 328 (26.9) | |
| 4 | 3 (0.3) | 2 (0.2) | |
| Unknown | 1 (0.1) | 0 | |
| Pelvic lymphadenectomy (number, %) | 0.349 | ||
| Not performed | 386 (31.9) | 407 (33.4) | |
| Performed | 822 (67.9) | 810 (66.5) | |
| Unknown | 3 (0.2) | 1 (0.1) | |
| LVI (number, %) | 343 (28.3) | 397 (32.6) | 0.022 |
| BCR (number, %) | 148 (12.3) | 118 (9.7) | 0.037 |
| Radiological recurrence (number, %) | 14 (1.2) | 8 (0.7) | 0.199 |
| CRPC (number, %) | 7 (0.6) | 4 (0.3) | 0.365 |
| Follow-up period (months, median, IQR) | 26.0 (11.9–49.9) | 24.2 (11.8–49.5) | 0.220 |
| Variables | Univariate | Multivariate | ||
|---|---|---|---|---|
| OR (95%CI) | p-Value | OR (95%CI) | p-Value | |
| Clinical T stage (continuous) | 2.644 (2.065–3.386) | < 0.001 | 1.745 (1.350–2.256) | <0.001 |
| Biopsy Gleason grade group (continuous) | 1.655 (1.501–1.826) | < 0.001 | 1.498 (1.351–1.660) | <0.001 |
| Initial PSA (continuous) | 1.062 (1.048–1.077) | < 0.001 | 1.049 (1.034–1.064) | <0.001 |
| NLR (continuous) | 1.224 (1.029–1.455) | 0.022 | 1.204 (0.945–1.533) | 0.133 |
Disclaimer/Publisher’s Note: The statements, opinions and data contained in all publications are solely those of the individual author(s) and contributor(s) and not of MDPI and/or the editor(s). MDPI and/or the editor(s) disclaim responsibility for any injury to people or property resulting from any ideas, methods, instructions or products referred to in the content. |
© 2023 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Murase, K.; Kawase, M.; Ebara, S.; Tatenuma, T.; Sasaki, T.; Ikehata, Y.; Nakayama, A.; Toide, M.; Yoneda, T.; Sakaguchi, K.; et al. The Negative Impact of Inflammation-Related Parameters in Prostate Cancer after Robot-Assisted Radical Prostatectomy: A Retrospective Multicenter Cohort Study in Japan (the MSUG94 Group). J. Clin. Med. 2023, 12, 7732. https://doi.org/10.3390/jcm12247732
Murase K, Kawase M, Ebara S, Tatenuma T, Sasaki T, Ikehata Y, Nakayama A, Toide M, Yoneda T, Sakaguchi K, et al. The Negative Impact of Inflammation-Related Parameters in Prostate Cancer after Robot-Assisted Radical Prostatectomy: A Retrospective Multicenter Cohort Study in Japan (the MSUG94 Group). Journal of Clinical Medicine. 2023; 12(24):7732. https://doi.org/10.3390/jcm12247732
Chicago/Turabian StyleMurase, Kazumasa, Makoto Kawase, Shin Ebara, Tomoyuki Tatenuma, Takeshi Sasaki, Yoshinori Ikehata, Akinori Nakayama, Masahiro Toide, Tatsuaki Yoneda, Kazushige Sakaguchi, and et al. 2023. "The Negative Impact of Inflammation-Related Parameters in Prostate Cancer after Robot-Assisted Radical Prostatectomy: A Retrospective Multicenter Cohort Study in Japan (the MSUG94 Group)" Journal of Clinical Medicine 12, no. 24: 7732. https://doi.org/10.3390/jcm12247732
APA StyleMurase, K., Kawase, M., Ebara, S., Tatenuma, T., Sasaki, T., Ikehata, Y., Nakayama, A., Toide, M., Yoneda, T., Sakaguchi, K., Teishima, J., Makiyama, K., Inoue, T., Kitamura, H., Saito, K., Koga, F., Urakami, S., & Koie, T. (2023). The Negative Impact of Inflammation-Related Parameters in Prostate Cancer after Robot-Assisted Radical Prostatectomy: A Retrospective Multicenter Cohort Study in Japan (the MSUG94 Group). Journal of Clinical Medicine, 12(24), 7732. https://doi.org/10.3390/jcm12247732








