Short-Term and Long-Term Outcomes of Fetal Ventriculomegaly beyond Gestational 37 Weeks: A Retrospective Cohort Study
Abstract
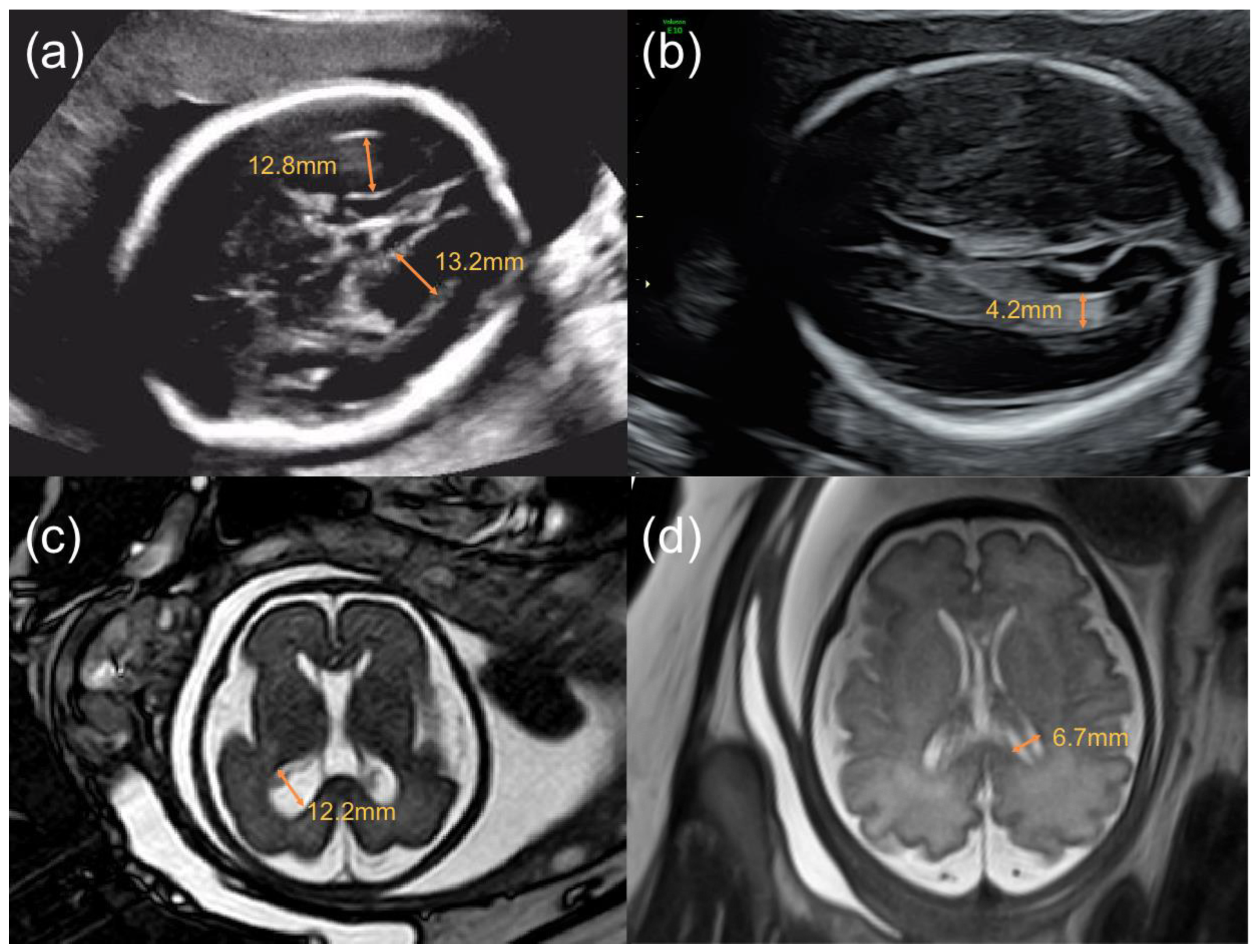
1. Introduction
2. Designs and Methods
3. Results
4. Discussion
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Acknowledgments
Conflicts of Interest
References
- Bloom, S.L.; Bloom, D.D.; Dellanebbia, C.; Martin, L.B.; Lucas, M.J.; Twickler, D.M. The developmental outcome of children with antenatal mild isolated ventriculomegaly. Obstet. Gynecol. 1997, 90, 93–97. [Google Scholar] [CrossRef] [PubMed]
- Zhao, X.M.; Li, X.; Li, W.; Li, S.S.; Chang, Y. Diagnostic Value of Magnetic Resonance Imaging in Fetal Lateral Ventriculomegaly and the Relationship Between the Degree of Isolated Lateral Ventriculomegaly and Neonatal Prognosis. Matern. Fetal Med. 2020, 2, 23–27. [Google Scholar] [CrossRef]
- Cardoza, J.D.; Goldstein, R.B.; Filly, R.A. Exclusion Of Fetal Ventriculomegaly With A Single Measurement—The Width Of The Lateral Ventricular Atrium. Radiology 1988, 169, 711–714. [Google Scholar] [CrossRef] [PubMed]
- Almog, B.; Gamzu, R.; Achiron, R.; Fainaru, O.; Zalel, Y. Fetal lateral ventricular width: What should be its upper limit? A prospective cohort study and reanalysis of the current and previous data. J. Ultrasound Med. 2003, 22, 39–43. [Google Scholar] [CrossRef]
- Mirsky, D.M.; Stence, N.V.; Powers, A.M.; Dingman, A.L.; Neuberger, I. Imaging of fetal ventriculomegaly. Pediatr. Radiol. 2020, 50, 1948–1958. [Google Scholar] [CrossRef]
- Gaglioti, P.; Oberto, M.; Todros, T. The significance of fetal ventriculomegaly: Etiology, short- and long-term outcomes. Prenatal Diagnosis 2009, 29, 381–388. [Google Scholar] [CrossRef]
- Tomic, K.; Schoenberger, H.; Weber, P.; Lapaire, O.; Manegold-Brauer, G. Significance of isolated borderline ventriculomegaly. Childs Nerv. Syst. 2020, 36, 393–399. [Google Scholar] [CrossRef]
- Thorup, E.; Jensen, L.N.; Bak, G.S.; Ekelund, C.K.; Greisen, G.; Jorgensen, D.S.; Hellmuth, S.G.; Wulff, C.; Petersen, O.B.; Pedersen, L.H.; et al. Neurodevelopmental disorder in children believed to have isolated mild ventriculomegaly prenatally. Ultrasound Obstet. Gynecol. 2019, 54, 182–189. [Google Scholar] [CrossRef]
- Oh, K.Y.; Gibson, T.J.; Pinter, J.D.; Pettersson, D.; Shaffer, B.L.; Selden, N.R.; Sohaey, R. Clinical outcomes following prenatal diagnosis of asymmetric ventriculomegaly, interhemispheric cyst, and callosal dysgenesis (AVID). Prenat. Diagn. 2019, 39, 26–32. [Google Scholar] [CrossRef]
- Parikh, L.I.; Reddy, U.M.; Mannisto, T.; Mendola, P.; Sjaarda, L.; Hinkle, S.; Chen, Z.; Lu, Z.; Laughon, S.K. Neonatal outcomes in early term birth. Am. J. Obstet. Gynecol. 2014, 211, 265.e1–265.e11. [Google Scholar] [CrossRef]
- Winkelhorst, D.; Kamphuis, M.M.; Steggerda, S.J.; Rijken, M.; Oepkes, D.; Lopriore, E.; van Klink, J.M.M. Perinatal Outcome and Long-Term Neurodevelopment after Intracranial Haemorrhage due to Fetal and Neonatal Alloimmune Thrombocytopenia. Fetal Diagn. Ther. 2019, 45, 184–191. [Google Scholar] [CrossRef]
- Burger, M.; Hoosain, M.; Einspieler, C.; Unger, M.; Niehaus, D. Maternal perinatal mental health and infant and toddler neurodevelopment—Evidence from low and middle-income countries. A systematic review. J. Affect. Disord. 2020, 268, 158–172. [Google Scholar] [CrossRef] [PubMed]
- Chimenea, A.; Garcia-Diaz, L.; Antinolo, G. Mode of delivery, perinatal outcome and neurodevelopment in uncomplicated monochorionic diamniotic twins: A single-center retrospective cohort study. BMC Pregnancy Childbirth 2022, 22, 89. [Google Scholar] [CrossRef] [PubMed]
- Carta, S.; Kaelin Agten, A.; Belcaro, C.; Bhide, A. Outcome of fetuses with prenatal diagnosis of isolated severe bilateral ventriculomegaly: Systematic review and meta-analysis. Ultrasound Obstet. Gynecol. 2018, 52, 165–173. [Google Scholar] [CrossRef] [PubMed]
- Pisapia, J.M.; Heuer, G.G. In reply to “Letter to the Editor: Fetal ventriculomegaly: Diagnosis, treatment, and future directions”. Childs Nerv. Syst. 2017, 33, 1865. [Google Scholar] [CrossRef]
- Movsas, T.Z.; Pinto-Martin, J.A.; Whitaker, A.H.; Feldman, J.F.; Lorenz, J.M.; Korzeniewski, S.J.; Levy, S.E.; Paneth, N. Autism Spectrum Disorder Is Associated with Ventricular Enlargement in a Low Birth Weight Population. J. Pediatr. 2013, 163, 73–78. [Google Scholar] [CrossRef]
- Kyriakopoulou, V.; Vatansever, D.; Elkommos, S.; Dawson, S.; McGuinness, A.; Allsop, J.; Molnar, Z.; Hajnal, J.; Rutherford, M. Cortical Overgrowth in Fetuses With Isolated Ventriculomegaly. Cereb. Cortex 2014, 24, 2141–2150. [Google Scholar] [CrossRef]
- Patel, M.D.; Filly, A.L.; Hersh, D.R.; Goldstein, R.B. Isolated mild fetal cerebral ventriculomegaly: Clinical course and outcome. Radiology 1994, 192, 759–764. [Google Scholar] [CrossRef]
- Nadel, A.S.; Benacerraf, B.R. Lateral ventricular atrium: Larger in male than female fetuses. Int. J. Gynaecol. Obstet. 1995, 51, 123–126. [Google Scholar] [CrossRef]
- Griffiths, P.D.; Jarvis, D.; Connolly, D.J.; Mooney, C.; Embleton, N.; Hart, A.R. Predicting neurodevelopmental outcomes in fetuses with isolated mild ventriculomegaly. Arch. Dis. Child Fetal Neonatal. Ed. 2022, 107, 431–436. [Google Scholar] [CrossRef]
- Patel, S.K.; Zamorano-Fernandez, J.; Nagaraj, U.; Bierbrauer, K.S.; Mangano, F.T. Not all ventriculomegaly is created equal: Diagnostic overview of fetal, neonatal and pediatric ventriculomegaly. Childs Nerv. Syst. 2020, 36, 1681–1696. [Google Scholar] [CrossRef] [PubMed]
- SMFM; Fox, N.S.; Monteagudo, A.; Kuller, J.A.; Craigo, S.; Norton, M.E. Mild fetal ventriculomegaly: Diagnosis, evaluation, and management. Am. J. Obstet. Gynecol. 2018, 219, B2–B9. [Google Scholar] [CrossRef] [PubMed]
- Chiu, T.H.; Haliza, G.; Lin, Y.H.; Hung, T.H.; Hsu, J.J.; Hsieh, T.T.; Lo, L.M. A retrospective study on the course and outcome of fetal ventriculomegaly. Taiwan. J. Obstet. Gynecol. 2014, 53, 170–177. [Google Scholar] [CrossRef] [PubMed]
- Bar-Yosef, O.; Barzilay, E.; Dorembus, S.; Achiron, R.; Katorza, E. Neurodevelopmental outcome of isolated ventriculomegaly: A prospective cohort study. Prenat. Diagn. 2017, 37, 764–768. [Google Scholar] [CrossRef] [PubMed]
- Guo, D.; He, D.; Shen, Q.; Lin, N.; He, S.; Dai, Y.; Li, Y.; Xu, L.; Wu, X. Comprehensive Assessment of Fetal Bilateral Ventriculomegaly Based on Genetic Disorders, Cytomegalovirus Infection, Extra Prenatal Imaging and Pregnancy Outcomes in a Tertiary Referral Center. Int. J. Gen. Med. 2021, 14, 7719–7728. [Google Scholar] [CrossRef]
- Kheiri, G.; Naderian, N.; Karami, S.; Habibi, Z.; Nejat, F. Prenatal ventriculomegaly: Natural course, survival, and neurodevelopmental status. J. Neurosurg. Pediatr. 2021, 27, 497–502. [Google Scholar] [CrossRef] [PubMed]

| Variable | VM Group (n = 179) | Control Group (n = 222) | p Value |
|---|---|---|---|
| Maternal age/(year) | 31.06 ± 4.05 | 31.30 ± 3.78 | 0.531 |
| Pre-BMI/(kg/m2) a | 20.63 ± 2.63 | 20.84 ± 2.69 | 0.447 |
| Gravidity | 2.34 ± 1.38 | 2.19 ± 1.43 | 0.302 |
| Parity | 1.36 ± 0.49 | 1.39 ± 0.53 | 0.564 |
| Pregnancy with complications (n./total n.) (%) | 97/179(54.19) | 103/222(46.40) | 0.121 |
| IVF-ET(n./total n.) (%) | 15/179(8.38) | 11/222(4.95) | 0.166 |
| Twin pregnancy(n./total n.) (%) | 7/179(3.91) | 14/222(6.31) | 0.284 |
| TORCH IgM positive of maternal serum (n./total n.) (%) b | 7/49(14.29) | 4/29(13.79) | 1.000 * |
| Abnormal chromosomal analysis of amniocentesis (n./total n.) (%) c | 8/92(8.70) | 2/45(4.44) | 0.497 * |
| Cesarean Section (n./total n.) (%) | 116/179(64.80) | 140/222(63.06) | 0.718 |
| Category | VM Group (n = 179) | Control Group (n = 222) | p Value |
|---|---|---|---|
| Gestational age at birth/(weeks) | 38.72 ± 1.05 | 38.73 ± 1.08 | 0.925 |
| Distribution(n./total n.) (%) | 0.902 | ||
| 37 0/7–38 6/7 weeks | 68/179(37.99) | 83/222(37.39) | |
| ≥39 0/7 weeks | 111/179(62.01) | 139/222(62.61) | |
| Male infant (n./total n.) (%) | 110/179(61.45) | 104/222(46.85) | 0.004 |
| Length at birth/mm a | 49.89 ± 2.01 | 49.32 ± 2.71 | 0.020 |
| Birth weight/g | 3382.99 ± 477.28 | 3233.18 ± 425.10 | 0.001 |
| Apgar at 1 min | 9.90 ± 0.38 | 9.95 ± 0.35 | 0.168 |
| Apgar at 5 min | 9.99 ± 0.08 | 9.99 ± 0.12 | 0.428 |
| Apgar at 10 min | 10.00 ± 0.00 | 10.00 ± 0.00 | 1.000 |
| NICU admission (n./total n.) (%) | 18/179(10.06) | 1/222 (0.45) | <0.001 |
| Abnormal neurodevelopment after birth (n./total n.) (%) | 26/179(14.53) | 5/222(2.25) | <0.001 |
| Factor | VM with Normal Neurodevelopment (n = 153) | VM with Abnormal Neurodevelopment (n = 26) | p Value |
|---|---|---|---|
| Maternal age/(year) | 31.07 ± 4.044 | 30.96 ± 4.142 | 0.898 |
| Pre-BMI/(kg/m2) | 20.78 ± 2.65 | 19.79 ± 2.36 | 0.078 |
| Gravidity | 2.30 ± 1.396 | 2.54 ± 1.272 | 0.417 |
| Parity | 1.35 ± 0.491 | 1.42 ± 0.504 | 0.464 |
| Pregnancy with complications (n./total n.) (%) | 71/153(46.41) | 12/26(46.15) | 0.981 |
| Twin pregnancy (n./total n.) (%) | 6/153(3.92) | 1/26(3.85) | 1.000 |
| IVF-ET (n./total n.) (%) | 15/153(9.80) | 0/26(0.00) | 0.132 * |
| Male infant (n./total n.) (%) | 98/153(64.05) | 12/26(46.15) | 0.083 |
| Abnormal chromosomal analysis of amniocentesis a | 7/79(8.86) | 1/13(7.69) | 1.000 * |
| Gestational age at birth (weeks) | 38.69 ± 1.053 | 38.85 ± 1.047 | 0.493 |
| Distribution (n./total n.) (%) | 0.209 | ||
| 37 0/7–38 6/7 weeks | 61/153(39.97) | 7/26(26.92) | |
| ≥ 39 0/7 weeks | 92/153(60.13) | 19/26(73.08) | |
| Cesarean section (n./total n.) (%) | 96/153(62.75) | 20/26(76.92) | 0.162 |
| NICU admission (n./total n.) (%) | 11/153(7.19) | 7/26(26.92) | 0.006 * |
| Non-isolated VM (n./total n.) (%) | 52/153(33.99) | 13/26(50.00) | 0.116 |
| Do MRI screen (n./total n.) (%) | 94/153(61.44) | 17/26(65.38) | 0.701 |
| Postnatal cranial ultrasound suggestive with VM b | 18/79(22.78) | 8/11(72.73) | 0.002 * |
| Bilateral VM (n./total n.) (%) | 37/153(24.18) | 9/26(34.62) | 0.260 |
| Gestational age at first diagnosis | |||
| ≥ 28 week (n./total n.) (%) | 79/153(51.63) | 14/26(53.85) | 0.853 |
| Progressing VM (n./total n.) (%) | 11/153(7.19) | 4/26(15.38) | 0.240 * |
| Peak width of lateral ventricles (mm) | 11.39 ± 1.046 | 12.25 ± 1.87 | 0.030 |
| Degrees (n./total n.) (%) | 0.029 ** | ||
| Mild | 122/153(79.74) | 15/26(57.69) | 0.070 c |
| Moderate | 31/153(20.26) | 9/26(34.62) | 0.064 d* |
| Severe | 0/153(0.00) | 2/26(7.69) | 0.014 e* |
| Factor | Category | B | S.E. | Wald | df | P | ExpB | 95%CI |
|---|---|---|---|---|---|---|---|---|
| Pregnancy with complications | Yes | −0.268 | 0.494 | 0.294 | 1 | 0.587 | 0.765 | 0.290–2.015 |
| Twin pregnancy | Yes | 0.063 | 1.281 | 0.002 | 1 | 0.961 | 1.065 | 0.087–13.102 |
| Male infant | Yes | −0.739 | 0.486 | 2.316 | 1 | 0.128 | 0.477 | 0.184–1.237 |
| Gestational age at first diagnosis (weeks) | / | −0.065 | 0.056 | 1.345 | 1 | 0.246 | 0.937 | 0.839–1.046 |
| Progressing VM | Yes | −0.157 | 0.829 | 0.036 | 1 | 0.850 | 0.855 | 0.168–4.342 |
| Non-isolated VM | Yes | 0.518 | 0.502 | 1.067 | 1 | 0.302 | 1.679 | 0.628–4.487 |
| Bilateral VM | Yes | −0.137 | 0.567 | 0.059 | 1 | 0.809 | 0.872 | 0.287–2.651 |
| Peak width of lateral ventricles (mm) | / | 0.357 | 0.217 | 2.714 | 1 | 0.099 | 1.429 | 0.935–2.185 |
| Gestational age at birth (weeks) | / | 0.216 | 0.231 | 0.875 | 1 | 0.350 | 1.242 | 0.789–1.954 |
| Cesarean section | Yes | 0.728 | 0.565 | 1.660 | 1 | 0.198 | 2.070 | 0.684–6.264 |
| NICU admission | Yes | 1.270 | 0.633 | 4.023 | 1 | 0.045 | 3.561 | 1.029–12.320 |
| Postnatal cranial ultrasound | No VM detected | / | / | 3.812 | 2 | 0.149 | / | / |
| VM detected | 1.590 | 0.818 | 3.780 | 1 | 0.052 | 4.903 | 0.987–24.350 | |
| Not carried out | 1.049 | 0.706 | 2.211 | 1 | 0.137 | 2.856 | 0.716–11.390 | |
| Constant | / | −13.766 | 9.454 | 2.120 | 1 | 0.145 | 0.000 | / |
Disclaimer/Publisher’s Note: The statements, opinions and data contained in all publications are solely those of the individual author(s) and contributor(s) and not of MDPI and/or the editor(s). MDPI and/or the editor(s) disclaim responsibility for any injury to people or property resulting from any ideas, methods, instructions or products referred to in the content. |
© 2023 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Chen, H.; Bai, P.; Yang, S.; Jia, M.; Tian, H.; Zou, J.; Xiao, X. Short-Term and Long-Term Outcomes of Fetal Ventriculomegaly beyond Gestational 37 Weeks: A Retrospective Cohort Study. J. Clin. Med. 2023, 12, 1065. https://doi.org/10.3390/jcm12031065
Chen H, Bai P, Yang S, Jia M, Tian H, Zou J, Xiao X. Short-Term and Long-Term Outcomes of Fetal Ventriculomegaly beyond Gestational 37 Weeks: A Retrospective Cohort Study. Journal of Clinical Medicine. 2023; 12(3):1065. https://doi.org/10.3390/jcm12031065
Chicago/Turabian StyleChen, Huiling, Peng Bai, Shuqi Yang, Mingzhu Jia, Huan Tian, Juan Zou, and Xue Xiao. 2023. "Short-Term and Long-Term Outcomes of Fetal Ventriculomegaly beyond Gestational 37 Weeks: A Retrospective Cohort Study" Journal of Clinical Medicine 12, no. 3: 1065. https://doi.org/10.3390/jcm12031065
APA StyleChen, H., Bai, P., Yang, S., Jia, M., Tian, H., Zou, J., & Xiao, X. (2023). Short-Term and Long-Term Outcomes of Fetal Ventriculomegaly beyond Gestational 37 Weeks: A Retrospective Cohort Study. Journal of Clinical Medicine, 12(3), 1065. https://doi.org/10.3390/jcm12031065







