Incidence of Febrile Seizures in Children with COVID-19
Abstract
:1. Introduction
2. Methods
2.1. Patients
2.2. Data Collection
3. Results
3.1. Study Population
3.2. Clinical Manifestations in Children with COVID-19-Associated FS
3.3. Neurologic Manifestations of Patients with Prolonged FS during COVID-19
4. Discussion
5. Conclusions
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Acknowledgments
Conflicts of Interest
References
- Leung, A.K.; Hon, K.L.; Leung, T.N. Febrile seizures: An overview. Drugs Context 2018, 7, 212536. [Google Scholar] [CrossRef] [PubMed]
- Whelan, H.; Harmelink, M.; Chou, E.; Sallowm, D.; Khan, N.; Patil, R.; Sannagowdara, K.; Kim, J.H.; Chen, W.L.; Khalil, S.; et al. Complex febrile seizures-A systematic review. Disease-A-Month DM 2017, 63, 5–23. [Google Scholar] [CrossRef] [PubMed]
- Patel, A.D.; Vidaurre, J. Complex febrile seizures: A practical guide to evaluation and treatment. J. Child Neurol. 2013, 28, 762–767. [Google Scholar] [CrossRef]
- Graves, R.C.; Oehler, K.; Tingle, L.E. Febrile seizures: Risks, evaluation, and prognosis. Am. Fam. Physician 2012, 85, 149–153. [Google Scholar]
- Nilsson, G.; Lundström, S.; Fernell, E.; Gillberg, C. Neurodevelopmental problems in children with febrile seizures followed to young school age: A prospective longitudinal community-based study in Sweden. Acta Paediatr. 2022, 111, 586–592. [Google Scholar] [CrossRef]
- Delpisheh, A.; Veisani, Y.; Sayehmiri, K.; Fayyazi, A. Febrile seizures: Etiology, prevalence, and geographical variation. Iran. J. Child Neurol. 2014, 8, 30–37. [Google Scholar] [PubMed]
- Dubru, J.M.; Leroy, P.; Tomat, A.M.; Misson, J.P. Epidemiology and characteristics of febrile seizures in children. Rev. Med. Liege 2013, 68, 180–185. [Google Scholar]
- Berg, A.T.; Shinnar, S.; Shapiro, E.D.; Salomon, M.E.; Crain, E.F.; Hauser, W.A. Risk factors for a first febrile seizure: A matched case-control study. Epilepsia 1995, 36, 334–341. [Google Scholar] [CrossRef]
- Chung, B.; Wong, V. Relationship between five common viruses and febrile seizure in children. Arch. Dis. Child. 2007, 92, 589–593. [Google Scholar] [CrossRef] [Green Version]
- Pokorn, M.; Jevšnik, M.; Petrovec, M.; Steyer, A.; Mrvič, T.; Grosek, Š.; Lusa, L.; Strle, F. Respiratory and enteric virus detection in children: A prospective study comparing children with febrile seizures and healthy controls. J. Child Neurol. 2017, 32, 84–93. [Google Scholar] [CrossRef]
- Carman, K.B.; Calik, M.; Karal, Y.; Isikay, S.; Kocak, O.; Ozcelik, A.; Yazar, A.S.; Nuhoglu, C.; Sag, C.; Kilic, O.; et al. Viral etiological causes of febrile seizures for respiratory pathogens (EFES study). Hum. Vaccines Immunother. 2019, 15, 496–502. [Google Scholar] [CrossRef]
- Kukuruzovic, M. 391 Febrile convulsions and influenza A or B- are there differences? Arch. Dis. Child. 2021, 106, A164. [Google Scholar]
- Solomon, M.D.; McNulty, E.J.; Rana, J.S.; Leong, T.K.; Lee, C.; Sung, S.-H.; Ambrosy, A.P.; Sidney, S.; Go, A.S. The COVID-19 pandemic and the incidence of acute myocardial infarction. N. Engl. J. Med. 2020, 383, 691–693. [Google Scholar] [CrossRef]
- Chen, Y.T.; Shao, S.C.; Hsu, C.K.; Wu, I.W.; Hung, M.J.; Chen, Y.C. Incidence of acute kidney injury in COVID-19 infection: A systematic review and meta-analysis. Crit. Care 2020, 24, 1–4. [Google Scholar] [CrossRef]
- Gottesman, B.L.; Yu, J.; Tanaka, C.; Longhurst, C.A.; Kim, J.J. Incidence of new-onset type 1 diabetes among US children during the COVID-19 global pandemic. JAMA Pediatr. 2022, 176, 414–415. [Google Scholar] [CrossRef]
- Central Disease Control Headquaters. Weekly Updates for Countries with Major Outbreaks. Coronavirus (COVID-19). Republic of Korea. Available online: http://ncov.mohw.go.kr/en/ (accessed on 1 July 2022).
- Park, K.H.; Choe, Y.J.; Shim, Y.; Eun, B.L.; Byeon, J.H. Decrease in incidence of febrile seizure following social distancing measures: A national cohort study in South Korea. Pediatr. Infect. Vaccine 2021, 28, 144–148. [Google Scholar] [CrossRef]
- Cadet, K.; Boegner, J.; Ceneviva, G.D.; Thomas, N.J.; Krawiec, C. Evaluation of febrile seizure diagnoses associated with COVID-19. J. Child Neurol. 2022, 37, 410–415. [Google Scholar] [CrossRef] [PubMed]
- Angeles, D.K. Proposal for revised clinical and electroencephalographic classification of epileptic seizures. From the commission on classification and terminology of the international league against epilepsy. Epilepsia 1981, 22, 489–501. [Google Scholar]
- Seinfeld, S.; Shinnar, S.; Sun, S.; Hesdorffer, D.C.; Deng, X.; Shinnar, R.C.; O’Hara, K.; Nordli, D.R., Jr.; Frank, L.M.; Gallentine, W.; et al. Emergency management of febrile status epilepticus: Results of the FEBSTAT study. Epilepsia 2014, 55, 388–395. [Google Scholar] [CrossRef] [Green Version]
- Bassan, H.; Barzilay, M.; Shinnar, S.; Shorer, Z.; Matoth, I.; Gross-Tsur, V. Prolonged febrile seizures, clinical characteristics, and acute management. Epilepsia 2013, 54, 1092–1098. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Lee, J.J.; Choe, Y.J.; Jeong, H.; Kim, M.; Kim, S.; Yoo, H.; Park, K.; Kim, C.; Choi, S.; Sim, J.; et al. Importation and transmission of SARS-CoV-2 B.1.1.529 (omicron) variant of concern in Korea, November 2021. J. Korean Med. Sci. 2021, 36, e346. [Google Scholar] [CrossRef] [PubMed]
- Cloete, J.; Kruger, A.; Masha, M.; du Plessis, N.M.; Mawela, D.; Tshukudu, M.; Manyane, T.; Komane, L.; Venter, M.; Jassat, W.; et al. Rapid rise in paediatric COVID-19 hospitalisations during the early stages of the Omicron wave, Tshwane District, South Africa. medRxiv 2021. [Google Scholar] [CrossRef]
- Chiu, S.S.; Tse, C.Y.; Lau, Y.L.; Peiris, M. Influenza A infection is an important cause of febrile seizures. Pediatrics 2001, 108, E63. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Ward, K.N.; Gray, J.J. Primary human herpesvirus-6 infection is frequently overlooked as a cause of febrile fits in young children. J. Med. Virol. 1994, 42, 119–123. [Google Scholar] [CrossRef]
- Shrestha, D.; Dhakal, A.K.; Shakya, H.; Shakya, A.; Shah, S.C.; Mehata, S. Clinical characteristics of children with febrile seizure. J. Nepal Health Res. Counc. 2014, 12, 162–166. [Google Scholar]
- Forsgren, L.; Sidenvall, R.; Blomquist, H.K.S.; Heijbel, J. A prospective incidence study of febrile convulsions. Acta Paediatr. 1990, 79, 550–557. [Google Scholar] [CrossRef]
- Waruiru, C.; Appleton, R. Febrile seizures: An update. Arch. Dis. Child. 2004, 89, 751–756. [Google Scholar] [CrossRef] [Green Version]
- Hesdorffer, D.C.; Benn, E.K.; Bagiella, E.; Nordli, D.; Pellock, J.; Hinton, V.; Shinnar, S.; FEBSTAT Study Team. Distribution of febrile seizure duration and associations with development. Ann. Neurol. 2011, 70, 93–100. [Google Scholar] [CrossRef] [Green Version]
- Thongsing, A.; Eizadkhah, D.; Fields, C.; Ballaban-Gil, K. Provoked seizures and status epilepticus in the pediatric population with COVID-19 disease. Epilepsia 2022, 63, e86–e91. [Google Scholar] [CrossRef]
- Cha, T.; Choi, Y.J.; Oh, J.W.; Kim, C.R.; Park, D.W.; Seol, I.J.; Moon, J.H. Respiratory syncytial virus-associated seizures in Korean children, 2011–2016. Korean J. Pediatr. 2019, 62, 131–137. [Google Scholar] [CrossRef]
- Dantzer, R. Neuroimmune interactions: From the brain to the immune system and vice versa. Physiol. Rev. 2018, 98, 477–504. [Google Scholar] [CrossRef] [PubMed]
- Narula, N.; Joseph, R.; Katyal, N.; Daouk, A.; Acharya, S.; Avula, A.; Maroun, R. Seizure and COVID-19: Association and review of potential mechanism. Neurol. Psychiatry Brain Res. 2020, 38, 49–53. [Google Scholar] [CrossRef] [PubMed]
- Weil, A.A.; Luiten, K.G.; Casto, A.M.; Bennett, J.C.; O’Hanlon, J.; Han, P.D.; Gamboa, L.S.; McDermot, E.; Truong, M.; Gottlieb, G.S.; et al. Genomic surveillance of SARS-CoV-2 Omicron variants on a university campus. Nat. Commun. 2022, 13, 5240. [Google Scholar] [CrossRef] [PubMed]
- Hall, C.B.; Caserta, M.T.; Schnabel, K.C.; McDermott, M.P.; Lofthus, G.K.; Carnahan, J.A.; Gilbert, L.M.; Dewhurst, S. Characteristics and acquisition of human herpesvirus (HHV) 7 infections in relation to infection with HHV-6. J. Infect. Dis. 2006, 193, 1063–1069. [Google Scholar] [CrossRef]
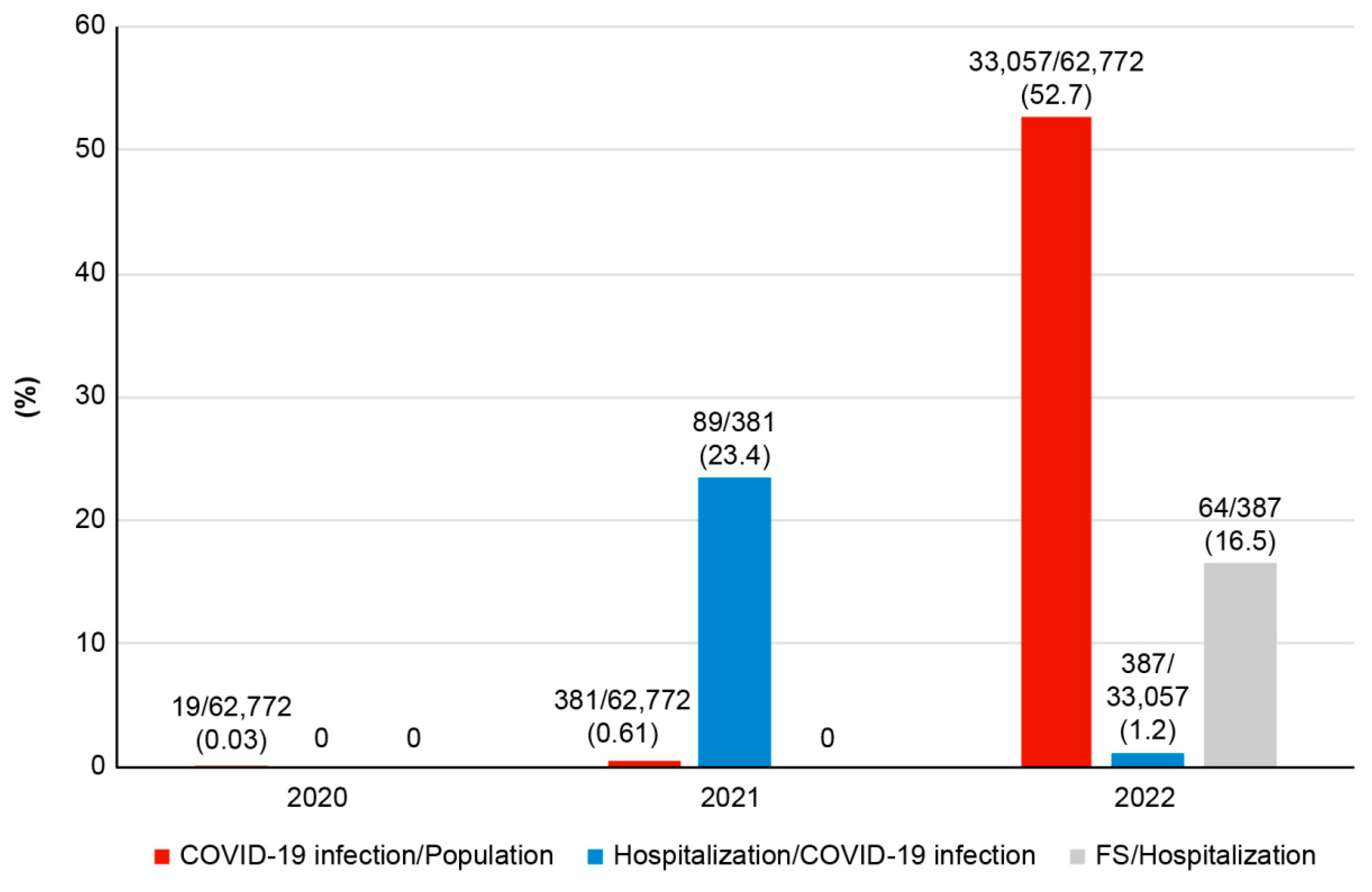

| COVID-19 Infection | Hospitalized COVID-19 (% *) | FS with COVID-19 (% **) | |
|---|---|---|---|
| Number (n) | |||
| 2020 | 0 | 0 | |
| 2021 | 89 (23.4) | 0 | |
| 2022 | 387 (1.2) | 64 (0.19) | |
| Total | 476 (1.4) | 64 (0.19) | |
| Sex distribution (M:F) | 0 | ||
| 2020 | 9:10 | 0 | 0 |
| 2021 | 186:195 | 47:42 | 0 |
| 2022 | 16,706:16,351 | 217:170 | 44:20 |
| Total | 16,901:16,556 | 264:212 | 44:20 |
| Age (months) | |||
| 2021 | 31.2 ± 16.7 | ||
| 2022 | 25.8 ± 18.6 | 36.7 ± 15.0 (6–60) | |
| Total | 26.9 ± 18.3 |
| Type of FS, n (%) | |
| Simple | 39 (60.9) |
| Complex | 24 (37.5) |
| FSE | 1 (1.6) |
| First FS, n (%) | 42 (65.6) |
| Recurrent FS, n (%) | 22 (34.4) |
| Average episode of seizure, n | 1.5 ± 1.2 |
| Duration of seizures, median, minutes | 3 (range 0.5–60) |
| Family history of FS, n (%) | 13 (20.3) |
| Hospitalization, day | 3.7 ± 2.7 |
| Ventilator care, n (%) | 1 (1.6) |
| ASM, n (%) | |
| 1st | 7 (10.9) |
| 2nd | 2 (3.1) |
| 3rd or more | 1 (1.6) |
| WBC, ×103/µL | 7.49 ± 2.71 |
| Differential lymphocyte, % | 22.5 ± 13.2 |
| CRP median, mg/L | 1.71 (range 0.2–36) |
| Sex | Age (Months) | Previous FS | Epi | Duration (min) | EEG | bMRI | Admission (Days) | ASM | Glucose (mg/dL) | Lactate (mmol/L) | |
|---|---|---|---|---|---|---|---|---|---|---|---|
| Pt 1 | M | 13 | 0 | 1 | 60 | Slow waves | n/s | 5 | 2nd | 232 | 3 |
| Pt 2 | M | 7 | 0 | 2 | 20 | - | - | 8 | 1st | 291 | 26 |
| Pt 3 | M | 28 | 0 | 1 | 15 | - | - | 1 | X | 78 | 0.9 |
| Pt 4 | M | 57 | 10 | 3 | 15 | Slow waves | n/s | 2 | X | 91 | 1 |
| Pt 5 | F | 37 | 0 | 2 | 20 | Slow waves | n/s | 3 | X | 95 | 1.33 |
| Pt 6 | M | 51 | 1 | 1 | 15 | n/s | n/s | 6 | X | 106 | 1.6 |
Disclaimer/Publisher’s Note: The statements, opinions and data contained in all publications are solely those of the individual author(s) and contributor(s) and not of MDPI and/or the editor(s). MDPI and/or the editor(s) disclaim responsibility for any injury to people or property resulting from any ideas, methods, instructions or products referred to in the content. |
© 2023 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Han, M.J.; Heo, J.H.; Hwang, J.S.; Jang, Y.-T.; Lee, M.; Kim, S.J. Incidence of Febrile Seizures in Children with COVID-19. J. Clin. Med. 2023, 12, 1076. https://doi.org/10.3390/jcm12031076
Han MJ, Heo JH, Hwang JS, Jang Y-T, Lee M, Kim SJ. Incidence of Febrile Seizures in Children with COVID-19. Journal of Clinical Medicine. 2023; 12(3):1076. https://doi.org/10.3390/jcm12031076
Chicago/Turabian StyleHan, Min Jeong, Jun Ho Heo, Ji Seong Hwang, Young-Taek Jang, Min Lee, and Sun Jun Kim. 2023. "Incidence of Febrile Seizures in Children with COVID-19" Journal of Clinical Medicine 12, no. 3: 1076. https://doi.org/10.3390/jcm12031076





