Epidermolysis Bullosa Acquisita—Current and Emerging Treatments
Abstract
:1. Introduction
1.1. The Classical Form of EBA
1.2. The Inflammatory Form of EBA Has Four Clinical Presentations
1.2.1. Bullous Pemphigoid-Like Variant
1.2.2. Mucose Membrane Pemphigoid-Like Variant
1.2.3. Linear IgA Disease-Like Variant
1.2.4. Brunsting-Perry Pemphigoid-Like Variant
2. Diagnostic Methods
3. Treatment
3.1. Systemic Corticosteroids
3.2. Corticosteroid Sparing Agents
3.3. High-Dose Intravenous Immunoglobulin (IVIG) Therapy
3.4. Rituximab (RTX)
3.5. Immunoadsorption (IA)
3.6. Extracorporeal Photochemotherapy (ECP)
3.7. Daclizumab
3.8. Minocycline
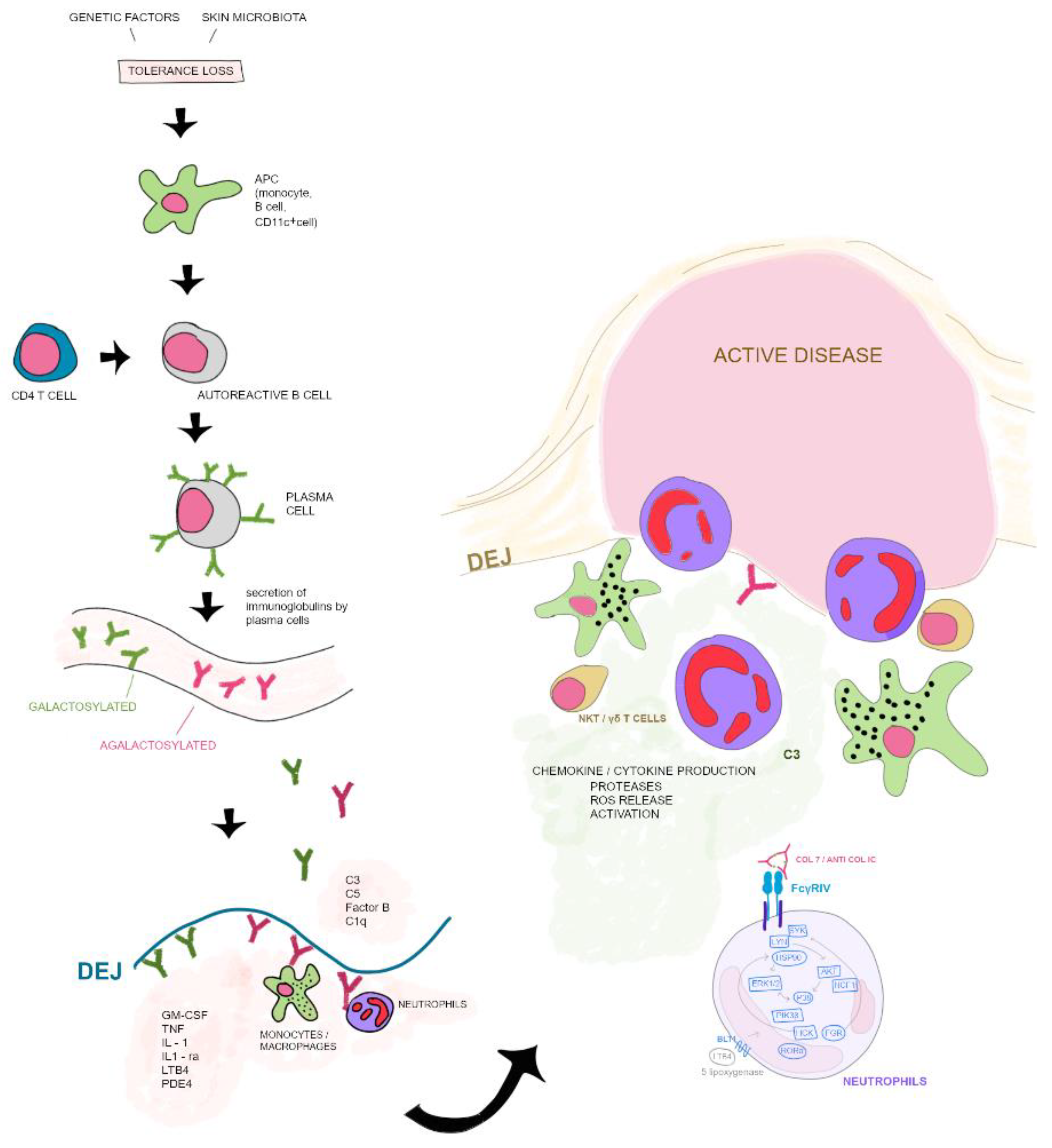
4. Pathogenesis
4.1. Induction Phase
4.2. Autoantibody Phase
4.3. Effector Phase
5. Novel Therapeutic Implications (Table 2)
| Anti-Hsp90 Treatment | Modulating induction phase |
| Monoclonal antibodies against CD3, CD4, IL-2R and CD 40 L | |
| Antigen-specific immunoadsorption | Modulating autoantibody maintenance |
| Saturation of neonatal Fc receptor binding sites | |
| Endoglycosidase (EndoS) | Modulating the effector phase |
| Anti-CM-CSF antibody | |
| IL-1 receptor blocker anakinra | |
| Targeting retinoid related orphan receptor α/Akt, Src, P13Kβ, Erk1/2,p38 | |
| Soluble FcγRIIB (CD32) | |
| Anti-Flii antibody |
5.1. Modulating Induction Phase
5.2. Modulating Autoantibody Maintenance
5.3. Modulating the Effector Phase
6. Conclusions
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Conflicts of Interest
References
- Buijsrogge, J.; Diercks, G.; Pas, H.; Jonkman, M. The many faces of epidermolysis bullosa acquisita after serration pattern analysis by direct immunofluorescence microscopy. Br. J. Dermatol. 2011, 165, 92–98. [Google Scholar] [CrossRef] [PubMed]
- Kim, S.; Kim, J.; Kim, Y. Epidermolysis Bullosa Acquisita: A Retrospective Clinical Analysis of 30 Cases. Acta Derm. Venereol. 2011, 91, 307–312. [Google Scholar] [CrossRef] [PubMed]
- Woodley, D.T.; Briggaman, R.A.; Gammon, W.T. Review and update of epidermolysis bullosa acquisita. Semin. Dermatol. 1988, 7, 111–122. [Google Scholar] [PubMed]
- Alexandre, M.; Brette, M.-D.; Pascal, F.; Tsianakas, P.; Fraitag, S.; Doan, S.; Caux, F.; Dupuy, A.; Heller, M.; Lièvre, N.; et al. A Prospective Study of Upper Aerodigestive Tract Manifestations of Mucous Membrane Pemphigoid. Medicine 2006, 85, 239–252. [Google Scholar] [CrossRef]
- Kasperkiewicz, M.; Sadik, C.D.; Bieber, K.; Ibrahim, S.; Manz, R.A.; Schmidt, E.; Zillikens, D.; Ludwig, R. Epidermolysis Bullosa Acquisita: From Pathophysiology to Novel Therapeutic Options. J. Investig. Dermatol. 2016, 136, 24–33. [Google Scholar] [CrossRef]
- Woodley, D.T.; Burgeson, R.E.; Lunstrum, G.; Bruckner-Tuderman, L.; Reese, M.J.; Briggaman, R.A. Epidermolysis bullosa acquisita antigen is the globular carboxyl terminus of type VII procollagen. J. Clin. Investig. 1988, 81, 683–687. [Google Scholar] [CrossRef]
- Licarete, E.; Ganz, S.; Recknagel, M.J.; Di Zenzo, G.; Hashimoto, T.; Hertl, M.; Zambruno, G.; Hundorfean, G.; Mudter, J.; Neurath, M.F.; et al. Prevalence of collagen VII-specific autoantibodies in patients with autoimmune and inflammatory diseases. BMC Immunol. 2012, 13, 16. [Google Scholar] [CrossRef]
- Hübner, F.; Recke, A.; Zillikens, D.; Linder, R.; Schmidt, E. Prevalence and Age Distribution of Pemphigus and Pemphigoid Diseases in Germany. J. Investig. Dermatol. 2016, 136, 2495–2498. [Google Scholar] [CrossRef]
- Iwata, H.; Vorobyev, A.; Koga, H.; Recke, A.; Zillikens, D.; Prost-Squarcioni, C.; Ishii, N.; Hashimoto, T.; Ludwig, R.J. Meta-analysis of the clinical and immunopathological characteristics and treatment outcomes in epidermolysis bullosa acquisita patients. Orphanet J. Rare Dis. 2018, 13, 153. [Google Scholar] [CrossRef]
- Bertram, F.; Brãcker, E.-B.; Zillikens, D.; Schmidt, E. Prospective analysis of the incidence of autoimmune bullous disorders in Lower Franconia, Germany. JDDG J. Dtsch. Dermatol. Ges. 2009, 7, 434–439. [Google Scholar] [CrossRef]
- Milinković, M.V.; Janković, S.; Medenica, L.; Nikolić, M.; Reljić, V.; Popadić, S.; Janković, J. Incidence of autoimmune bullous diseases in Serbia: A 20-year retrospective study. J. Dtsch. Dermatol. Ges. 2016, 14, 995–1005. [Google Scholar] [CrossRef] [PubMed]
- Bernard, P.; Vaillant, L.; Labeille, B.; Bedane, C.; Arbeille, B.; Denoeux, J.P.; Lorette, G.; Bonnetblanc, J.M.; Prost, C. Incidence and distribution of subepidermal autoimmune bullous skin diseases in three French regions. Bullous Diseases French Study Group. Arch. Dermatol. 1995, 131, 48–52. [Google Scholar] [CrossRef] [PubMed]
- Hashimoto, T.; Jin, Z.; Ishii, N. Clinical and immunological studies for 105 Japanese seropositive patients of epidermolysis bullosa acquisita examined at Kurume University. Expert Rev. Clin. Immunol. 2016, 12, 895–902. [Google Scholar] [CrossRef] [PubMed]
- Lee, C.W. Prevalences of subacute cutaneous lupus erythematosus and Epidermolysis bullosa acquisita among Korean/Oriental populations. Dermatology 1998, 197, 187. [Google Scholar] [PubMed]
- Ludwig, R.J. Clinical Presentation, Pathogenesis, Diagnosis, and Treatment of Epidermolysis Bullosa Acquisita. ISRN Dermatol. 2013, 2013, 812029. [Google Scholar] [CrossRef]
- Ishii, N.; Hamada, T.; Dainichi, T.; Karashima, T.; Nakama, T.; Yasumoto, S.; Zillikens, D.; Hashimoto, T. Epidermolysis bullosa acquisita: What’s new? J. Dermatol. 2010, 37, 220–230. [Google Scholar] [CrossRef]
- Chen, M.; Kim, G.H.; Prakash, L.; Woodley, D.T. Epidermolysis bullosa acquisita: Autoimmunity to anchoring fibril collagen. Autoimmunity 2011, 45, 91–101. [Google Scholar] [CrossRef]
- Schulze, F.; Neumann, K.; Recke, A.; Zillikens, D.; Linder, R.; Schmidt, E. Malignancies in Pemphigus and Pemphigoid Diseases. J. Investig. Dermatol. 2015, 135, 1445–1447. [Google Scholar] [CrossRef]
- Delbaldo, C.; Chen, M.; Friedli, A.; Prins, C.; Desmeules, J.; Saurat, J.-H.; Woodley, D.T.; Borradori, L. Drug-induced epidermolysis bullosa acquisita with antibodies to type VII collagen. J. Am. Acad. Dermatol. 2002, 46, S161–S164. [Google Scholar] [CrossRef]
- Jappe, U.; Zillikens, D.; Bonnekoh, B.; Gollnick, H. Epidermolysis bullosa acquisita with ultraviolet radiation sensitivity. Br. J. Dermatol. 2000, 142, 517–520. [Google Scholar] [CrossRef]
- Baican, A.; Chiriac, G.; Baican, C.; Macovei, V.; Ciuce, D.; Fritsch, A.; Sitaru, C. Metal sensitization precipitates skin blistering in epidermolysis bullosa acquisita. J. Dermatol. 2010, 37, 280–282. [Google Scholar] [CrossRef]
- Wakelin, S.H.; Allen, J.; Zhou, S.; Wojnarowska, F. Drug-induced linear IgA disease with antibodies to collagen VII. Br. J. Dermatol. 1998, 138, 310–314. [Google Scholar] [CrossRef]
- Roenigk, H.H., Jr.; Ryan, J.G.; Bergfeld, W.F. Epidermolysis bullosa acquisita. Report of three cases and review of all published cases. Arch. Dermatol. 1971, 103, 1–10. [Google Scholar] [CrossRef]
- Gammon, W.R.; Briggaman, R.A.; Woodley, D.T.; Heald, P.W.; Wheeler, C.E., Jr. Epidermolysis bullosa acquisita—A pemphigoid-like disease. J. Am. Acad. Dermatol. 1984, 11, 820–832. [Google Scholar] [CrossRef]
- Kurzhals, G.; Stolz, W.; Meurer, M.; Kunze, J.; Braun-Falco, O.; Krieg, T. Acquired epidermolysis bullosa with the clinical feature of Brunsting-Perry cicatricial bullous pemphigoid. Arch. Dermatol. 1991, 127, 391–395. [Google Scholar] [CrossRef]
- Zambruno, G.; Manca, V.; Kanitakis, J.; Cozzani, E.; Nicolas, J.-F.; Giannetti, A. Linear IgA bullous dermatosis with autoantibodies to a 290 kd antigen of anchoring fibrils. J. Am. Acad. Dermatol. 1994, 31, 884–888. [Google Scholar] [CrossRef]
- Dahl, M.G. Epidermolysis bullosa acquisita–a sign of cicatricial pemphigoid? Br. J. Dermatol. 1979, 101, 475. [Google Scholar] [CrossRef]
- Vorobyev, A.; Ludwig, R.J.; Schmidt, E. Clinical features and diagnosis of epidermolysis bullosa acquisita. Expert Rev. Clin. Immunol. 2016, 13, 157–169. [Google Scholar] [CrossRef]
- Koga, H.; Prost-Squarcioni, C.; Iwata, H.; Jonkman, M.F.; Ludwig, R.J.; Bieber, K. Epidermolysis Bullosa Acquisita: The 2019 Update. Front. Med. 2019, 5, 362. [Google Scholar] [CrossRef] [PubMed]
- Schmidt, E.; Della Torre, R.; Borradori, L. Clinical features and practical diagnosis of bullous pemphigoid. Immunol. Allergy Clin. 2012, 32, 217–232. [Google Scholar] [CrossRef] [PubMed]
- Gammon, W.R.; Briggaman, R.A.; Wheeler, C.E. Epidermolysis bullosa acquisita presenting as an inflammatory bullous disease. J. Am. Acad. Dermatol. 1982, 7, 382–387. [Google Scholar] [CrossRef] [PubMed]
- Chan, L.S.; Ahmed, A.R.; Anhalt, G.J.; Bernauer, W.; Cooper, K.D.; Elder, M.J.; Fine, J.D.; Foster, C.S.; Ghohestani, R.; Hashimoto, T.; et al. The first international consensus on mucous membrane pemphigoid: Definition, diagnostic criteria, pathogenic factors, medical treatment, and prognostic indicators. Arch. Dermatol. 2002, 138, 370–379. [Google Scholar] [CrossRef]
- Luke, M.C.; Darling, T.N.; Hsu, R.; Summers, R.M.; Smith, J.A.; Solomon, B.I.; Thomas, G.R.; Yancey, K.B. Mucosal Morbidity in Patients With Epidermolysis Bullosa Acquisita. Arch. Dermatol. 1999, 135, 954–959. [Google Scholar] [CrossRef]
- Letko, E.; Bhol, K.; Anzaar, F.; Perez, V.L.; Ahmed, A.R.; Foster, C.S. Chronic Cicatrizing Conjunctivitis in a Patient With Epidermolysis Bullosa Acquisita. Arch. Ophthalmol. 2006, 124, 1615. [Google Scholar] [CrossRef]
- Lang, P.G., Jr.; Tapert, M.J. Severe ocular involvement in a patient with epidermolysis bullosa acquisita. J. Am. Acad. Dermatol. 1987, 16, 439–443. [Google Scholar] [CrossRef]
- Briggaman, R.A.; Gammon, W.R.; Woodley, D.T. Epidermolysis Bullosa Acquisita of the Immunopathological Type (Dermolytic Pemphigoid). J. Investig. Dermatol. 1985, 85, S79–S84. [Google Scholar] [CrossRef]
- Delgado, L.; Aoki, V.; Santi, C.; Gabbi, T.; Sotto, M.; Maruta, C. Clinical and immunopathological evaluation of epidermolysis bullosa acquisita. Clin. Exp. Dermatol. 2010, 36, 12–18. [Google Scholar] [CrossRef]
- Kiniwa, Y.; Ashida, A.; Ohashi, A.; Kitoh, R.; Fukuda, S.; Hashimoto, T.; Okuyama, R. A Case of Epidermolysis Bullosa Acquisita Associated with Laryngeal Stenosis. Acta Dermato-Venereologica 2012, 92, 93–94. [Google Scholar] [CrossRef]
- Benton, E.C.; Bhogal, B.; Oakley, R.; Groves, R.W. Beware the blistering patient with dysphonia. Clin. Exp. Dermatol. 2013, 38, 691–692. [Google Scholar] [CrossRef]
- Poirier, E.; Soued, I.; Alexandre, M.; Boussoura, S.; Lamberto, C.; Uzunhan, Y.; Gharbi, N.; Pascal, F.; Doan, S.; Brillet, P.-Y.; et al. Pemphigoide des muqueuses avec sténose laryngée ou trachéale. Annales de Dermatologie et de Vénéréologie 2014, 141, S262. [Google Scholar] [CrossRef]
- Vodegel, R.M.; de Jong, M.C.; Pas, H.H.; Jonkman, M.F. IgA-mediated epidermolysis bullosa acquisita: Two cases and review of the literature. J. Am. Acad. Dermatol. 2002, 47, 919–925. [Google Scholar] [CrossRef]
- Bauer, J.W.; Schaeppi, H.; Metze, D.; Muss, W.; Pohla-Gubo, G.; Hametner, R.; Ruckhofer, J.; Grabner, G.; Hintner, H. Ocular involvement in IgA-epidermolysis bullosa acquisita. Br. J. Dermatol. 1999, 141, 887–892. [Google Scholar] [CrossRef] [PubMed]
- Hashimoto, T.; Ishiko, A.; Shimizu, H.; Tanaka, T.; Dodd, H.J.; Bhogal, B.S.; Black, M.M.; Nishikawa, T. A case of linear IgA bullous dermatosis with IgA anti-type VII collagen autoantibodies. Br. J. Dermatol. 1996, 134, 336–339. [Google Scholar] [CrossRef] [PubMed]
- Brunsting, L.A.; Perry, H.O. Benign pemphigoid; a report of seven cases with chronic, scarring, herpetiform plaques about the head and neck. AMA Arch. Derm. 1957, 75, 489–501. [Google Scholar] [CrossRef]
- Gupta, R.; Woodley, D.T.; Chen, M. Epidermolysis bullosa acquisita. Clin. Dermatol. 2012, 30, 60–69. [Google Scholar] [CrossRef]
- Joly, P.; Roujeau, J.-C.; Benichou, J.; Delaporte, E.; D’Incan, M.; Dreno, B.; Bedane, C.; Sparsa, A.; Gorin, I.; Picard, C.; et al. A Comparison of Two Regimens of Topical Corticosteroids in the Treatment of Patients with Bullous Pemphigoid: A Multicenter Randomized Study. J. Investig. Dermatol. 2009, 129, 1681–1687. [Google Scholar] [CrossRef]
- Murrell, D.F.; Daniel, B.S.; Joly, P.; Borradori, L.; Amagai, M.; Hashimoto, T.; Caux, F.; Marinovic, B.; Sinha, A.A.; Hertl, M.; et al. Definitions and outcome measures for bullous pemphigoid: Recommendations by an international panel of experts. J. Am. Acad. Dermatol. 2011, 66, 479–485. [Google Scholar] [CrossRef]
- Murrell, D.F.; Marinovic, B.; Caux, F.; Prost, C.; Ahmed, R.; Wozniak, K.; Amagai, M.; Bauer, J.; Beissert, S.; Borradori, L.; et al. Definitions and outcome measures for mucous membrane pemphigoid: Recommendations of an international panel of experts. J. Am. Acad. Dermatol. 2014, 72, 168–174. [Google Scholar] [CrossRef]
- Prost-Squarcioni, C.; Caux, F.; Schmidt, E.; Jonkman, M.F.; Vassileva, S.; Kim, S.C.; Iranzo, P.; Daneshpazhooh, M.; Terra, J.; Bauer, J.; et al. International Bullous Diseases Group: Consensus on diagnostic criteria for epidermolysis bullosa acquisita. Br. J. Dermatol. 2018, 179, 30–41. [Google Scholar] [CrossRef]
- Schmidt, E.; Goebeler, M.; Hertl, M.; Sárdy, M.; Sitaru, C.; Eming, R.; Hofmann, S.C.; Hunzelmann, N.; Kern, J.S.; Kramer, H.; et al. S2k guideline for the diagnosis of pemphigus vulgaris/foliaceus and bullous pemphigoid. JDDG J. Dtsch. Dermatol. Ges. 2015, 13, 713–727. [Google Scholar] [CrossRef]
- Vodegel, R.; Jonkman, M.; Pas, H.; De Jong, M. U-serrated immunodeposition pattern differentiates type VII collagen targeting bullous diseases from other subepidermal bullous autoimmune diseases. Br. J. Dermatol. 2004, 151, 112–118. [Google Scholar] [CrossRef] [PubMed]
- Terra, J.; Meijer, J.; Jonkman, M.; Diercks, G. The n- vs. u-serration is a learnable criterion to differentiate pemphigoid from epidermolysis bullosa acquisita in direct immunofluorescence serration pattern analysis. Br. J. Dermatol. 2013, 169, 100–105. [Google Scholar] [CrossRef] [PubMed]
- Terra, J.; Pas, H.; Hertl, M.; Dikkers, F.; Kamminga, N.; Jonkman, M. Immunofluorescence serration pattern analysis as a diagnostic criterion in antilaminin-332 mucous membrane pemphigoid: Immunopathological findings and clinical experience in 10 Dutch patients. Br. J. Dermatol. 2011, 165, 815–822. [Google Scholar] [CrossRef]
- Woodley, D.; Sauder, D.; Talley, M.J.; Silver, M.; Grotendorst, G.; Qwarnstrom, E. Localization of Basement Membrane Components After Dermal-Epidermal Junction Separation. J. Investig. Dermatol. 1983, 81, 149–153. [Google Scholar] [CrossRef] [PubMed]
- Gammon, W.R.; Briggaman, R.A.; Inman, A.O., III; Queen, L.L.; Wheeler, C.E. Differentiatinganti-lamina lucida and anti-sublamina densa anti-BMZ antibodies by indirect immunofluorescence on 1.0 M sodium chloride-separated skin. J. Investig. Dermatol. 1984, 82, 139–144. [Google Scholar] [CrossRef]
- Logan, R.A.; Bhogal, B.; Das, A.K.; McKee, P.M.; Black, M.M. Localization of bullous pem-phigoid antibody–an indirect immunofluorescence study of 228 cases using a split-skin technique. Br. J. Dermatol. 1987, 117, 471–478. [Google Scholar] [CrossRef]
- Lazarova, Z.; Yancey, K.B. Reactivity of autoantibodies from patients with defined subepidermal bullous diseases against 1 mol/L salt-split skin: Specificity, sensitivity, and practical considerations. J. Am. Acad. Dermatol. 1996, 35, 398–403. [Google Scholar] [CrossRef]
- Schmidt, E.; Groves, R. Immunobullous diseases. In Rook’s Textbook of Dermatology, Part 3, Chapter 50, 9th ed.; Griffith, C., Barker, J., Chalmers, R., Bleiker, T., Creamer, D., Eds.; Wiley-Blackwell: Chichester, UK, 2016; Volume 50, pp. 1–56. [Google Scholar]
- Goletz, S.; Hashimoto, T.; Zillikens, D.; Schmidt, E. Anti-p200 pemphigoid. J. Am. Acad. Dermatol. 2014, 71, 185–191. [Google Scholar] [CrossRef]
- Bruins, S.; De Jong, M.C.; Heeres, K.; Wilkinson, M.; Jonkman, M.F.; Van Der Meer, J.B. Fluorescence overlay antigen mapping of the epidermal basement membrane zone: III. Topographic staining and effective resolution. J. Histochem. Cytochem. 1995, 43, 649–656. [Google Scholar] [CrossRef]
- De Jong, M.C.; Bruins, S.; Heeres, K.; Jonkman, M.F.; Nieboer, C.; Boorsma, D.M.; Pas, H.H.; van der Meer, J.B. Bullous pemphigoid and epidermolysis bullosa acquisita. Differentiation by fluorescence overlay antigen mapping. Arch. Dermatol. 1996, 132, 151–157. [Google Scholar] [CrossRef]
- Wozniak, K.; Kazama, T.; Kowalewski, C. A practical technique for differentiation of subepidermal bullous diseases: Localization of in vivo-bound IgG by laser scanning confocal microscopy. Arch. Dermatol. 2003, 139, 1007–1011. [Google Scholar] [CrossRef]
- Jonkman, M.F.; Schuur, J.; Dijk, F.; Heeres, K.; De Jong, M.C.J.M.; Van Der Meer, J.B.; Yancey, K.B.; Pas, H.H. Inflammatory Variant of Epidermolysis Bullosa Acquisita With IgG Autoantibodies Against Type VII Collagen and Laminin α3. Arch. Dermatol. 2000, 136, 227–231. [Google Scholar] [CrossRef]
- Vodegel, R.M.; Kiss, M.; Cjm De Jong, M.; Altmayer, A.; Molnar, K.; Sándor, H.U.S.Z.; Jonkman, M.F. The use of skin substrates deficient in basement membrane molecules for the diagnosis of subepidermal autoimmune bullous disease. Eur. J. Dermatol. 1998, 8, 83–85. [Google Scholar] [CrossRef]
- Prost-Squarcioni, C. Electron microscopy and immunoelectronmicroscopy. In Blistering Diseases: Clinical Features, Pathogenesis, Treatment; Murrell, D., Ed.; Springer: New York, NY, USA, 2015; pp. 213–237. [Google Scholar]
- Saleh, M.A.; Ishii, K.; Kim, Y.-J.; Murakami, A.; Ishii, N.; Hashimoto, T.; Schmidt, E.; Zillikens, D.; Shirakata, Y.; Hashimoto, K.; et al. Development of NC1 and NC2 domains of Type VII collagen ELISA for the diagnosis and analysis of the time course of epidermolysis bullosa acquisita patients. J. Dermatol. Sci. 2011, 62, 169–175. [Google Scholar] [CrossRef]
- Seta, V.; Aucouturier, F.; Bonnefoy, J.; Le Roux-Villet, C.; Pendaries, V.; Alexandre, M.; Grootenboer-Mignot, S.; Heller, M.; Lièvre, N.; Laroche, L.; et al. Comparison of 3 type VII collagen (C7) assays for serologic diagnosis of epidermolysis bullosa acquisita (EBA). J. Am. Acad. Dermatol. 2016, 74, 1166–1172. [Google Scholar] [CrossRef]
- van Beek, N.; Dähnrich, C.; Johannsen, N.; Lemcke, S.; Goletz, S.; Hübner, F.; Di Zenzo, G.; Dmochowski, M.; Drenovska, K.; Geller, S.; et al. Prospective studies on the routine use of a novel multivariant enzyme-linked immunosorbent assay for the diagnosis of autoimmune bullous diseases. J. Am. Acad. Dermatol. 2017, 76, 889–894. [Google Scholar] [CrossRef]
- Komorowski, L.; Müller, R.; Vorobyev, A.; Probst, C.; Recke, A.; Jonkman, M.F.; Hashimoto, T.; Kim, S.C.; Groves, R.; Ludwig, R.J.; et al. Sensitive and specificassays for routine serological diagnosis of epidermolysis bullosaacquisita. J. Am. Acad. Dermatol. 2013, 68, e89–e95. [Google Scholar] [CrossRef]
- Marzano, A.V.; Cozzani, E.; Biasin, M.; Russo, I.; Alaibac, M. The use of Biochip immunofluorescence microscopy for the serological diagnosis of epidermolysis bullosa acquisita. Arch. Dermatol. Res. 2016, 308, 273–276. [Google Scholar] [CrossRef]
- Lapiere, J.C.; Woodley, D.T.; Parente, M.G.; Iwasaki, T.; Wynn, K.C.; Christiano, A.M.; Uitto, J. Epitope mapping of type VII collagen. Identification of discrete peptide sequences recognized by sera from patients with acquired epidermolysis bullosa. J. Clin. Investig. 1993, 92, 1831–1839. [Google Scholar] [CrossRef]
- Chen, M.; O’Toole, E.A.; Sanghavi, J.; Woodley, D.T.; Mahmud, N.; Kelleher, D.; Weir, D.; Fairley, J.A. The epidermolysis bullosa acquisita antigen (type VII collagen) is present in human colon and patients with crohn’s disease have autoantibodies to type VII collagen. J. Investig. Dermatol. 2002, 118, 1059–1064. [Google Scholar] [CrossRef] [Green Version]
- Chan, L.S.; Lapiere, J.-C.; Chen, M.; Traczyk, T.; Mancini, A.J.; Paller, A.S.; Woodley, D.T.; Marinkovich, M.P. Bullous systemic lupus erythematosus with autoantibodies recognizing multiple skin basement membrane components, bullous pemphigoid antigen 1, laminin-5, laminin-6, and type VII collagen. Arch. Dermatol. 1999, 135, 569–573. [Google Scholar] [CrossRef] [PubMed]
- Barton, D.D.; Fine, J.-D.; Gammon, W.R.; Sams, W.M. Bullous systemic lupus erythematosus: An unusual clinical course and detectable circulating autoantibodies to the epidermolysis bullosa acquisita antigen. J. Am. Acad. Dermatol. 1986, 15, 369–373. [Google Scholar] [CrossRef] [PubMed]
- Terra, J.B.; Jonkman, M.F.; Diercks, G.F.H.; Pas, H.H. Low sensitivity of typeVII collagen enzyme-linked immunosorbent assay in epidermolysisbullosa acquisita: Serration pattern analysis on skin biopsy isrequired for diagnosis. Br. J. Dermatol. 2013, 169, 164–167. [Google Scholar] [CrossRef]
- Woodley, D.T.; Gammon, W.R.; Briggaman, R.A. Epidermolysis bullosa acquisita. In Dermatology in General Medicine, 4th ed.; Fitzpatrick, T.B., Eisen, A.Z., Wolff, K., Freedberg, I.M., Austen, K.F., Eds.; McGrawHill: New York, NY, USA, 1998; Volume 1–2, pp. 702–709. [Google Scholar]
- Kofler, H.; Wambacher-Gasser, B.; Topar, G.; Weinlich, G.; Schuler, G.; Hintner, H.; Romani, N.; Fritsch, P. Intravenous immunoglobulin treatment in therapy-resistant epidermolysis bullosa acquisita. J. Am. Acad. Dermatol. 1997, 36, 331–335. [Google Scholar] [CrossRef] [PubMed]
- Furue, M.; Iwata, M.; Yoon, H.I.; Kubota, Y.; Ohto, H.; Kawashima, M.; Tsuchida, T.; Oohara, K.; Tamaki, K.; Kukita, A. Epidermolysis bullosa acquisita: Clinical response to plasma exchange therapy and circulating anti-BMZ antibody titre. J. Am. Acad. Dermatol. 1986, 14, 873–878. [Google Scholar] [CrossRef] [PubMed]
- Gordon, K.B.; Chan, L.S.; Woodley, D.T. Treatment of refractory epidermolysis bullosa acquisita with extracorporeal photochemotherapy. Br. J. Dermatol. 1997, 136, 415–420. [Google Scholar] [CrossRef]
- Camara, A.; Bécherel, P.A.; Bussel, A.; Lagrange, S.; Chosidow, O.; Joly, P.; Piette, J.C.; Francès, C. Resistant acquired bullous epidermolysis with severe ocular involvement: The success of extracorporeal photochemotherapy. Ann. Dermatol. Venereol. 1999, 126, 612–615. [Google Scholar]
- Bloching, M.; Dippel, E.; Jovanovic, S.; Hess, M.; Zouboulis, C.C. Manifestation of epidermolysis bullosa acquisita (EBA) in the ENT area. HNO 1999, 47, 497–501. [Google Scholar] [CrossRef]
- Schmidt, E.; Zillikens, D. Pemphigoid diseases. Lancet 2013, 381, 320–332. [Google Scholar] [CrossRef]
- Tanaka, N.; Dainichi, T.; Ohyama, B.; Yasumoto, S.; Oono, T.; Iwatsuki, K.; Elfert, S.; Fritsch, A.; Bruckner-Tuderman, L.; Hashimoto, T. A case of epidermolysis bullosa acquisita with clinical features of Brunsting-Perry pemphigoid showing an excellent response to colchicine. J. Am. Acad. Dermatol. 2009, 61, 715–719. [Google Scholar] [CrossRef]
- Adachi, A.; Komine, M.; Suzuki, M.; Murata, S.; Hirano, T.; Ishii, N.; Hashimoto, T.; Ohtsuki, M. Oral colchicine monotherapy for epidermolysis bullosa acquisita: Mechanism of action and efficacy. J. Dermatol. 2016, 43, 1389–1391. [Google Scholar] [CrossRef] [PubMed]
- Megahed, M.; Scharffetter-Kochanek, K. Epidermolysis bullosa acquisita–successful treatment with colchicine. Arch. Dermatol. Res. 1994, 286, 35–46. [Google Scholar] [CrossRef]
- Russo, I.; Ferrazzi, A.; Zanetti, I.; Alaibac, M. Epidermolysis bullosa acquisita in a 17- year-old boy with Crohn’s disease. BMJ Case Rep. 2015, 2015, bcr2015210210. [Google Scholar] [CrossRef]
- Gürcan, H.M.; Ahmed, A.R. Current concepts in the treatment of epidermolysis bullosa acquisita. Expert Opin. Pharmacother. 2011, 12, 1259–1268. [Google Scholar] [CrossRef]
- Hughes, A.P.; Callen, J.P. Epidermolysis bullosa acquisita responsive to dapsone therapy. J. Cutan. Med. Surg. 2001, 5, 397–399. [Google Scholar] [CrossRef]
- Zhu, Y.; Stiller, M.J. Dapsone and sulfones in dermatology: Overview and update. J. Am. Acad. Dermatol. 2001, 45, 420–434. [Google Scholar] [CrossRef]
- Gürcan, H.; Ahmed, A.R. Analysis of current data on the use of methotrexate in the treatment of pemphigus and pemphigoid. Br. J. Dermatol. 2009, 161, 723–731. [Google Scholar] [CrossRef]
- Sticherling, M.; Franke, A.; Aberer, E.; Gläser, R.; Hertl, M.; Pfeiffer, C.; Rzany, B.; Schneider, S.; Shimanovich, I.; Werfel, T.; et al. An open, multicentre, randomized clinical study in patients with bullous pemphigoid comparing methylprednisolone and azathioprine with methylprednisolone and dapsone. Br. J. Dermatol. 2017, 177, 1299–1305. [Google Scholar] [CrossRef]
- Fraser, A.G.; Orchard, T.R.; Jewell, D.P. The efficacy of azathioprine for the treatment of inflammatory bowel disease: A 30 year review. Gut 2002, 50, 485. [Google Scholar] [CrossRef]
- Ryan, C.; Amor, K.T.; Menter, A. The use of cyclosporine in dermatology: Part II. J. Am. Acad. Dermatol. 2010, 63, 949–972. [Google Scholar] [CrossRef]
- Allison, A.C.; Eugui, E.M. Mycophenolate mofetil and its mechanisms of action. Immunopharmacology 2000, 47, 85–118. [Google Scholar] [CrossRef] [PubMed]
- Allison, A.C. Mechanisms of action of mycophenolate mofetil. Lupus 2005, 14 (Suppl. S1), 2–8. [Google Scholar] [CrossRef] [PubMed]
- Beissert, S.; Mimouni, D.; Kanwar, A.J.; Solomons, N.; Kalia, V.; Anhalt, G.J. Treating Pemphigus Vulgaris with Prednisone and Mycophenolate Mofetil: A Multicenter, Randomized, Placebo-Controlled Trial. J. Investig. Dermatol. 2010, 130, 2041–2048. [Google Scholar] [CrossRef]
- Tran, M.M.; Anhalt, G.J.; Barrett, T.; Cohen, B.A. Childhood IgA-mediated epidermolysis bullosa acquisita responding to mycophenolate mofetil as a corticosteroid-sparing agent. J. Am. Acad. Dermatol. 2006, 54, 734–736. [Google Scholar] [CrossRef]
- Sami, N. Mycophenolate mofetil (MMF) in the treatment of epidermolysis bullosa acquisita (EBA) long-term follow-up. JAAD Case Rep. 2015, 1, 321–323. [Google Scholar] [CrossRef]
- Ahmed, A.; Gürcan, H. Treatment of epidermolysis bullosa acquisita with intravenous immunoglobulin in patients non-responsive to conventional therapy: Clinical outcome and post-treatment long-term follow-up. J. Eur. Acad. Dermatol. Venereol. 2011, 26, 1074–1083. [Google Scholar] [CrossRef]
- Amagai, M.; Ikeda, S.; Hashimoto, T.; Mizuashi, M.; Fujisawa, A.; Ihn, H.; Matsuzaki, Y.; Ohtsuka, M.; Fujiwara, H.; Furuta, J.; et al. A randomized double-blind trial of intravenous immunoglobulin for bullous pemphigoid. J. Dermatol. Sci. 2016, 85, 77–84. [Google Scholar] [CrossRef]
- Schmidt, E.; Goebeler, M.; Zillikens, D. Rituximab in Severe Pemphigus. Ann. N. Y. Acad. Sci. 2009, 1173, 683–691. [Google Scholar] [CrossRef]
- Kim, J.H.; Kim, S.C. Epidermolysis bullosa acquisita. J. Eur. Acad. Dermatol. Venereol. 2013, 27, 1204–1213. [Google Scholar] [CrossRef]
- Joly, P.; Maho-Vaillant, M.; Prost-Squarcioni, C.; Hebert, V.; Houivet, E.; Calbo, S.; Caillot, F.; Golinski, M.L.; Labeille, B.; Picard-Dahan, C.; et al. First-line rituximab combined with short-term prednisone versus prednisone alone for the treatment of pemphigus (Ritux 3): A prospective, multicentre, parallel-group, open-label randomised trial. Lancet 2017, 389, 2031–2040. [Google Scholar] [CrossRef]
- Lamberts, A.; Euverman, H.I.; Terra, J.B.; Jonkman, M.F.; Horváth, B. Effectiveness and safety of rituximab in recalcitrant pemphigoid diseases. Front. Immunol. 2018, 9, 248. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Bevans, S.L.; Sami, N. The use of rituximab in treatment of epidermolysis bullosa acquisita: Three new cases and a review of the literature. Dermatol. Ther. 2018, 31, e12726. [Google Scholar] [CrossRef]
- Niedermeier, A.; Eming, R.; Pfütze, M.; Neumann, C.R.; Happel, C.; Reich, K.; Hertl, M. Clinical Response of Severe Mechanobullous Epidermolysis Bullosa Acquisita to Combined Treatment With Immunoadsorption and Rituximab (Anti-CD20 Monoclonal Antibodies). Arch. Dermatol. 2007, 143, 192–198. [Google Scholar] [CrossRef]
- Oktem, A.; Akay, B.N.; Boyvat, A.; Kundakci, N.; Erdem, C.; Bostanci, S.; Sanli, H.; Kocyigit, P. Long-term results of rituximab–intravenous immunoglobulin combination therapy in patients with epidermolysis bullosa acquisita resistant to conventional therapy. J. Dermatol. Treat. 2016, 28, 50–54. [Google Scholar] [CrossRef]
- Mendes, S.R.; Coutinho, I.; Cardoso, J.C. Epidermolysis bullosa acquisita treated with rituximab. BMJ Case Rep. 2021, 14, e243432. [Google Scholar] [CrossRef]
- Schmidt, E.; Klinker, E.; Opitz, A.; Herzog, S.; Sitaru, C.; Goebeler, M.; Taleghoni, B.M.; Brocker, E.-B.; Zillikens, D. Protein A immunoadsorption: A novel and effective adjuvant treatment of severe pemphigus. Br. J. Dermatol. 2003, 148, 1222–1229. [Google Scholar] [CrossRef]
- Kolesnik, M.; Becker, E.; Reinhold, D.; Ambach, A.; Heim, M.; Gollnick, H.; Bonnekoh, B. Treatment of severe autoimmune blistering skin diseases with combination of protein A immunoadsorption and rituximab: A protocol without initial high dose or pulse steroid medication. J. Eur. Acad. Dermatol. Venereol. 2013, 28, 771–780. [Google Scholar] [CrossRef]
- Kubisch, I.; Diessenbacher, P.; Schmidt, E.; Gollnick, H.; Leverkus, M. Premonitory epidermolysis bullosa acquisita mimicking eyelid dermatitis: Successful treatment with rituximab and protein A immunoapheresis. Am. J. Clin. Dermatol. 2010, 11, 289–293. [Google Scholar] [CrossRef]
- Woodley, D.T.; Remington, J.; Chen, M. Autoimmunity to Type VII Collagen: Epidermolysis Bullosa Acquisita. Clin. Rev. Allergy Immunol. 2007, 33, 78–84. [Google Scholar] [CrossRef]
- Baroudjian, B.; Le Roux-Villet, C.; Bréchignac, S.; Alexandre, M.; Caux, F.; Prost-Squarcioni, C.; Laroche, L. Long-term efficacy of extracorporeal photochemotherapy in a patient with refractory epidermolysis bullosa acquisita. Eur. J. Dermatol. 2012, 22, 795–797. [Google Scholar] [CrossRef]
- Miller, J.; Stricklin, G.; Fine, J.; King, L.; Arzubiaga, M.D.C.; Ellis, D. Remission of severe epidermolysis bullosa acquisita induced by extracorporeal photochemotherapy. Br. J. Dermatol. 1995, 133, 467–471. [Google Scholar] [CrossRef] [PubMed]
- Egan, C.; Brown, M.; White, J.; Yancey, K. Treatment of Epidermolysis Bullosa Acquisita with the Humanized Anti-Tac mAb Daclizumab. Clin. Immunol. 2001, 101, 146–151. [Google Scholar] [CrossRef]
- Kawase, K.; Oshitani, Y.; Mizutani, Y.; Shu, E.; Fujine, E.; Seishima, M. Inflammatory Epidermolysis Bullosa Acquisita Effectively Treated with Minocycline. Acta Derm. Venereol. 2014, 94, 615–616. [Google Scholar] [CrossRef]
- Gammon, W.R.; Heise, E.R.; Burke, W.A.; Fine, J.-D.; Woodley, D.T.; Briggaman, R.A. Increased Frequency of HLA-DR2 in Patients with Autoantibodies to Epidermolysis Bullosa Acquisita Antigen: Evidence that the Expression of Autoimmunity to Type VII Collagen Is HLA Class II Allele Associated. J. Investig. Dermatol. 1988, 91, 228–232. [Google Scholar] [CrossRef] [PubMed]
- Zumelzu, C.; Le Roux-Villet, C.; Loiseau, P.; Busson, M.; Heller, M.; Aucouturier, F.; Pendaries, V.; Lièvre, N.; Pascal, F.; Brette, M.-D.; et al. Black Patients of African Descent and HLA-DRB1*15:03 Frequency Overrepresented in Epidermolysis Bullosa Acquisita. J. Investig. Dermatol. 2011, 131, 2386–2393. [Google Scholar] [CrossRef]
- Iwata, H.; Bieber, K.; Tiburzy, B.; Chrobok, N.; Kalies, K.; Shimizu, A.; Leineweber, S.; Ishiko, A.; Vorobyev, A.; Zillikens, D.; et al. B Cells, Dendritic Cells, and Macrophages Are Required To Induce an Autoreactive CD4 Helper T Cell Response in Experimental Epidermolysis Bullosa Acquisita. J. Immunol. 2013, 191, 2978–2988. [Google Scholar] [CrossRef]
- Sitaru, C.; Mihai, S.; Otto, C.; Chiriac, M.T.; Hausser, I.; Dotterweich, B.; Saito, H.; Rose, C.; Ishiko, A.; Zillikens, D. Induction of dermal-epidermal separation in mice by passive transfer of antibodies specific to type VII collagen. J. Clin. Investig. 2005, 115, 870–878. [Google Scholar] [CrossRef]
- Müller, R.; Dahler, C.; Möbs, C.; Wenzel, E.; Eming, R.; Messer, G.; Niedermeier, A.; Hertl, M. T and B cells target identical regions of the non-collagenous domain 1 of type VII collagen in epidermolysis bullosa acquisita. Clin. Immunol. 2010, 135, 99–107. [Google Scholar] [CrossRef]
- Sitaru, A.G.; Sesarman, A.; Mihai, S.; Chiriac, M.T.; Zillikens, D.; Hultman, P.; Solbach, W.; Sitaru, C. T cells are required for the production of blister-inducing autoantibodies in experimental epidermolysis bullosa acquisita. J. Immunol. 2010, 184, 1596–1603. [Google Scholar] [CrossRef]
- Hammers, C.M.; Bieber, K.; Kalies, K.; Banczyk, D.; Ellebrecht, C.T.; Ibrahim, S.M.; Zillikens, D.; Ludwig, R.J.; Westermann, J. Complement-Fixing Anti-Type VII Collagen Antibodies Are Induced in Th1-Polarized Lymph Nodes of Epidermolysis Bullosa Acquisita-Susceptible Mice. J. Immunol. 2011, 187, 5043–5050. [Google Scholar] [CrossRef]
- Chen, L.; Peterson, J.D.; Zheng, W.-Y.; Lin, S.-X.; Chan, L.S. Autoimmunity to type VII collagen in SKH1 mice is independent of regulatory T cells. Clin. Exp. Immunol. 2006, 145, 322–331. [Google Scholar] [CrossRef] [PubMed]
- Samavedam, U.K.S.R.L.; Iwata, H.; Müller, S.; Schulze, F.S.; Recke, A.; Schmidt, E.; Zillikens, D.; Ludwig, R.J. GM-CSF Modulates Autoantibody Production and Skin Blistering in Experimental Epidermolysis Bullosa Acquisita. J. Immunol. 2014, 192, 559–571. [Google Scholar] [CrossRef] [PubMed]
- Tiburzy, B.; Szyska, M.; Iwata, H.; Chrobok, N.; Kulkarni, U.; Hirose, M.; Ludwig, R.J.; Kalies, K.; Westermann, J.; Wong, D.; et al. Persistent Autoantibody-Production by Intermediates between Short-and Long-Lived Plasma Cells in Inflamed Lymph Nodes of Experimental Epidermolysis Bullosa Acquisita. PLoS ONE 2013, 8, e83631. [Google Scholar] [CrossRef]
- Schmidt, E.; Bröcker, E.-B.; Goebeler, M. Rituximab in Treatment-Resistant Autoimmune Blistering Skin Disorders. Clin. Rev. Allergy Immunol. 2007, 34, 56–64. [Google Scholar] [CrossRef]
- Kasperkiewicz, M.; Hirose, M.; Recke, A.; Schmidt, E.; Zillikens, D.; Ludwig, R. Clearance rates of circulating and tissue-bound autoantibodies to type VII collagen in experimental epidermolysis bullosa acquisita. Br. J. Dermatol. 2010, 162, 1064–1070. [Google Scholar] [CrossRef]
- Challa, D.K.; Velmurugan, R.; Ober, R.J.; Ward, E.S. FcRn: From Molecular Interactions to Regulation of IgG Pharmacokinetics and Functions. Fc Recept. 2014, 382, 249–272. [Google Scholar] [CrossRef]
- Sesarman, A.; Mihai, S.; Chiriac, M.; Olaru, F.; Sitaru, A.; Thurman, J.; Zillikens, D.; Sitaru, C. Binding of avian IgY to type VII collagen does not activate complement and leucocytes and fails to induce subepidermal blistering in mice. Br. J. Dermatol. 2008, 158, 463–471. [Google Scholar] [CrossRef]
- Chiriac, M.; Roesler, J.; Sindrilaru, A.; Scharffetter-Kochanek, K.; Zillikens, D.; Sitaru, C. NADPH oxidase is required for neutrophil-dependent autoantibody-induced tissue damage. J. Pathol. 2007, 212, 56–65. [Google Scholar] [CrossRef]
- Hirose, M.; Brandolini, L.; Zimmer, D.; Götz, J.; Westermann, J. The allosteric CXCR1/2 inhibitor DF2156A improves experimental epidermolysis bullosa acquisita. J. Genet. Syndr. Gene Ther. S 2013, 3, 2. [Google Scholar]
- Sadeghi, H.; Lockmann, A.; Hund, A.-C.; Samavedam, U.K.S.R.L.; Pipi, E.; Vafia, K.; Hauenschild, E.; Kalies, K.; Pas, H.H.; Jonkman, M.F.; et al. Caspase-1–Independent IL-1 Release Mediates Blister Formation in Autoantibody-Induced Tissue Injury through Modulation of Endothelial Adhesion Molecules. J. Immunol. 2015, 194, 3656–3663. [Google Scholar] [CrossRef]
- Samavedam, U.K.S.; Kalies, K.; Scheller, J.; Sadeghi, H.; Gupta, Y.; Jonkman, M.F.; Schmidt, E.; Westermann, J.; Zillikens, D.; Rose-John, S.; et al. Recombinant IL-6 treatment protects mice from organ specific autoimmune disease by IL-6 classical signalling-dependent IL-1ra induction. J. Autoimmun. 2013, 40, 74–85. [Google Scholar] [CrossRef] [PubMed]
- Kasperkiewicz, M.; Nimmerjahn, F.; Wende, S.; Hirose, M.; Iwata, H.; Jonkman, M.F.; Samavedam, U.; Gupta, Y.; Möller, S.; Rentz, E.; et al. Genetic identification and functional validation of FcgRIV as key molecule in autoantibody-induced tissue injury. J. Pathol. 2012, 228, 8–19. [Google Scholar] [CrossRef]
- Hellberg, L.; Samavedam, U.K.; Holdorf, K.; Hänsel, M.; Recke, A.; Beckmann, T.; Steinhorst, K.; Boehncke, W.-H.; Kirchner, T.; Möckel, N.; et al. Methylprednisolone Blocks Autoantibody-Induced Tissue Damage in Experimental Models of Bullous Pemphigoid and Epidermolysis Bullosa Acquisita through Inhibition of Neutrophil Activation. J. Investig. Dermatol. 2013, 133, 2390–2399. [Google Scholar] [CrossRef]
- Kulkarni, S.; Sitaru, C.; Jakus, Z.; Anderson, K.E.; Damoulakis, G.; Davidson, K.; Hirose, M.; Juss, J.; Oxley, D.; Chessa, T.A.; et al. PI3Kb plays a critical role in neutrophil activation by immune complexes. Sci. Signal. 2011, 4, ra23. [Google Scholar] [CrossRef]
- Sadeghi, H.; Gupta, Y.; Möller, S.; Samavedam, U.K.; Behnen, M.; Kasprick, A.; Bieber, K.; Müller, S.; Kalies, K.; Marques, A.D.C.; et al. The retinoid-related orphan receptor alpha is essential for the end-stage effector phase of experimental epidermolysis bullosa acquisita. J. Pathol. 2015, 237, 111–122. [Google Scholar] [CrossRef]
- Kopecki, Z.; Cowin, A. Flightless I: An actin-remodelling protein and an important negative regulator of wound repair. Int. J. Biochem. Cell Biol. 2008, 40, 1415–1419. [Google Scholar] [CrossRef]
- Kopecki, Z.; Arkell, R.M.; Strudwick, X.L.; Hirose, M.; Ludwig, R.J.; Kern, J.S.; Bruckner-Tuderman, L.; Zillikens, D.; Murrell, D.F.; Cowin, A.J. Overexpression of the Flii gene increases dermal-epidermal blistering in an autoimmune ColVII mouse model of epidermolysis bullosa acquisita. J. Pathol. 2011, 225, 401–413. [Google Scholar] [CrossRef]
- Kopecki, Z.; Ruzehaji, N.; Turner, C.; Iwata, H.; Ludwig, R.J.; Zillikens, D.; Murrell, D.F.; Cowin, A.J. Topically Applied Flightless I Neutralizing Antibodies Improve Healing of Blistered Skin in a Murine Model of Epidermolysis Bullosa Acquisita. J. Investig. Dermatol. 2013, 133, 1008–1016. [Google Scholar] [CrossRef]
- Ujiie, H.; Shimizu, H. Evidence for pathogenicity of autoreactive T cells in autoimmune bullous diseases shown by animal disease models. Exp. Dermatol. 2012, 21, 901–905. [Google Scholar] [CrossRef]
- Kasperkiewicz, M.; Müller, R.; Manz, R.; Magens, M.; Hammers, C.; Somlai, C.; Westermann, J.; Schmidt, E.; Zillikens, D.; Ludwig, R.; et al. Heat-shock protein 90 inhibition in autoimmunity to type VII collagen: Evidence that nonmalignant plasma cells are not therapeutic targets. Blood 2011, 117, 6135–6142. [Google Scholar] [CrossRef]
- Sola’rova’, Z.; Mojzis, J.; Sola’r, P. Hsp90 inhibitor as a sensitizer of cancer cells to different therapies (review). Int. J. Oncol. 2015, 46, 907–926. [Google Scholar]
- Collins, C.B.; Aherne, C.M.; Yeckes, A.; Pound, K.; Eltzschig, H.K.; Jedlicka, P.; de Zoeten, E.F. Inhibition of N-terminal ATPase on HSP90 attenuates colitis through enhanced Treg function. Mucosal. Immunol. 2013, 6, 960–971. [Google Scholar] [CrossRef] [PubMed]
- de Zoeten, E.F.; Wang, L.; Butler, K.; Beier, U.H.; Akimova, T.; Sai, H.; Bradner, J.E.; Mazitschek, R.; Kozikowski, A.P.; Matthias, P.; et al. Histone deacetylase 6 and heat shock protein 90 control the functions of Foxp3(þ) T-regulatory cells. Mol. Cell. Biol. 2011, 31, 2066–2078. [Google Scholar] [CrossRef] [Green Version]
- Tukaj, S.; Tiburzy, B.; Manz, R.; Marques, A.D.C.; Orosz, A.; Ludwig, R.J.; Zillikens, D.; Kasperkiewicz, M. Immunomodulatory effects of heat shock protein 90 inhibition on humoral immune responses. Exp. Dermatol. 2014, 23, 585–590. [Google Scholar] [CrossRef]
- Tukaj, S.; Zillikens, D.; Kasperkiewicz, M. Inhibitory effects of heat shock protein 90 blockade on proinflammatory human Th1 and Th17 cell subpopulations. J. Inflamm. 2014, 11, 10. [Google Scholar] [CrossRef]
- Tukaj, S.; Grüner, D.; Zillikens, D.; Kasperkiewicz, M. Hsp90 blockade modulates bullous pemphigoid IgG-induced ILe8 production by keratinocytes. Cell Stress Chaperones. 2014, 19, 887–894. [Google Scholar] [CrossRef]
- Tukaj, S.; Hellberg, L.; Ueck, C.; Hänsel, M.; Samavedam, U.; Zillikens, D.; Ludwig, R.J.; Laskay, T.; Kasperkiewicz, M. Heat shock protein 90 is required for ex vivo neutrophil-driven autoantibody-induced tissue damage in experimental epidermolysis bullosa acquisita. Exp. Dermatol. 2015, 24, 471–473. [Google Scholar] [CrossRef]
- Tukaj, S.; Zillikens, D.; Kasperkiewicz, M. Heat shock protein 90: A pathophysiological factor and novel treatment target in autoimmune bullous skin diseases. Exp. Dermatol. 2015, 24, 567–571. [Google Scholar] [CrossRef]
- Schwab, I.; Mihai, S.; Seeling, M.; Kasperkiewicz, M.; Ludwig, R.J.; Nimmerjahn, F. Broad requirement for terminal sialic acid residues and FcgRIIB for the preventive and therapeutic activity of intravenous immunoglobulins in vivo. Eur. J. Immunol. 2014, 44, 1444–1453. [Google Scholar] [CrossRef]
- Washburn, N.; Schwab, I.; Ortiz, D.; Bhatnagar, N.; Lansing, J.C.; Medeiros, A.; Tyler, S.; Mekala, D.; Cochran, E.; Sarvaiya, H.; et al. Controlled tetra-Fc sialylation of IVIg results in a drug candidate with consistent enhanced anti-inflammatory activity. Proc. Natl. Acad. Sci. USA 2015, 112, E1297–E1306. [Google Scholar] [CrossRef]
- Iwata, H.; Pipi, E.; Möckel, N.; Sondermann, P.; Vorobyev, A.; van Beek, N.; Zillikens, D.; Ludwig, R.J. Recombinant Soluble CD32 Suppresses Disease Progression in Experimental Epidermolysis Bullosa Acquisita. J. Investig. Dermatol. 2015, 135, 916–919. [Google Scholar] [CrossRef] [PubMed]
- Kasprick, A.; Hofrichter, M.; Smith, B.; Ward, P.; Bieber, K.; Shock, A.; Ludwig, R.J.; Schmidt, E. Treatment with anti-neonatal Fc receptor (FcRn) antibody ameliorates experimental epidermolysis bullosa acquisita in mice. Br. J. Pharmacol. 2020, 177, 2381–2392. [Google Scholar] [CrossRef]
- Hiroyasu, S.; Zeglinski, M.R.; Zhao, H.; Pawluk, M.A.; Turner, C.T.; Kasprick, A.; Tateishi, C.; Nishie, W.; Burleigh, A.; Lennox, P.A.; et al. Granzyme B inhibition reduces disease severity in autoimmune blistering diseases. Nat. Commun. 2021, 12, 302. [Google Scholar] [CrossRef]
| 1. | Systemic Corticosteroid Therapy |
| 2. | Corticosteroid sparing agents:  colchicine colchicine diaminodiphenyl sulfone (dapsone) diaminodiphenyl sulfone (dapsone) methotrexate (MTX) methotrexate (MTX) azathioprine (AZA) azathioprine (AZA) cyclosporine (CSA) cyclosporine (CSA) mycophenolate mofetil (MMF) mycophenolate mofetil (MMF) cyclophosphamide (CPA) cyclophosphamide (CPA) |
| 3. | High-dose intravenous immunoglobulin (IVIG) therapy |
| 4. | Rituximab (RTX) |
| 5. | Immunoadsorption (IA) |
| 6. | Extracorporeal photochemotherapy (ECP) |
| 7. | Daclizumab |
| 8. | Minocycline |
Disclaimer/Publisher’s Note: The statements, opinions and data contained in all publications are solely those of the individual author(s) and contributor(s) and not of MDPI and/or the editor(s). MDPI and/or the editor(s) disclaim responsibility for any injury to people or property resulting from any ideas, methods, instructions or products referred to in the content. |
© 2023 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Tešanović Perković, D.; Bukvić Mokos, Z.; Marinović, B. Epidermolysis Bullosa Acquisita—Current and Emerging Treatments. J. Clin. Med. 2023, 12, 1139. https://doi.org/10.3390/jcm12031139
Tešanović Perković D, Bukvić Mokos Z, Marinović B. Epidermolysis Bullosa Acquisita—Current and Emerging Treatments. Journal of Clinical Medicine. 2023; 12(3):1139. https://doi.org/10.3390/jcm12031139
Chicago/Turabian StyleTešanović Perković, Deša, Zrinka Bukvić Mokos, and Branka Marinović. 2023. "Epidermolysis Bullosa Acquisita—Current and Emerging Treatments" Journal of Clinical Medicine 12, no. 3: 1139. https://doi.org/10.3390/jcm12031139
APA StyleTešanović Perković, D., Bukvić Mokos, Z., & Marinović, B. (2023). Epidermolysis Bullosa Acquisita—Current and Emerging Treatments. Journal of Clinical Medicine, 12(3), 1139. https://doi.org/10.3390/jcm12031139






