Shoulder Joint Hybrid Assistive Limb Treatment for Chronic Stroke Patients with Upper Limb Dysfunction
Abstract
:1. Introduction
2. Materials and Methods
2.1. Patients
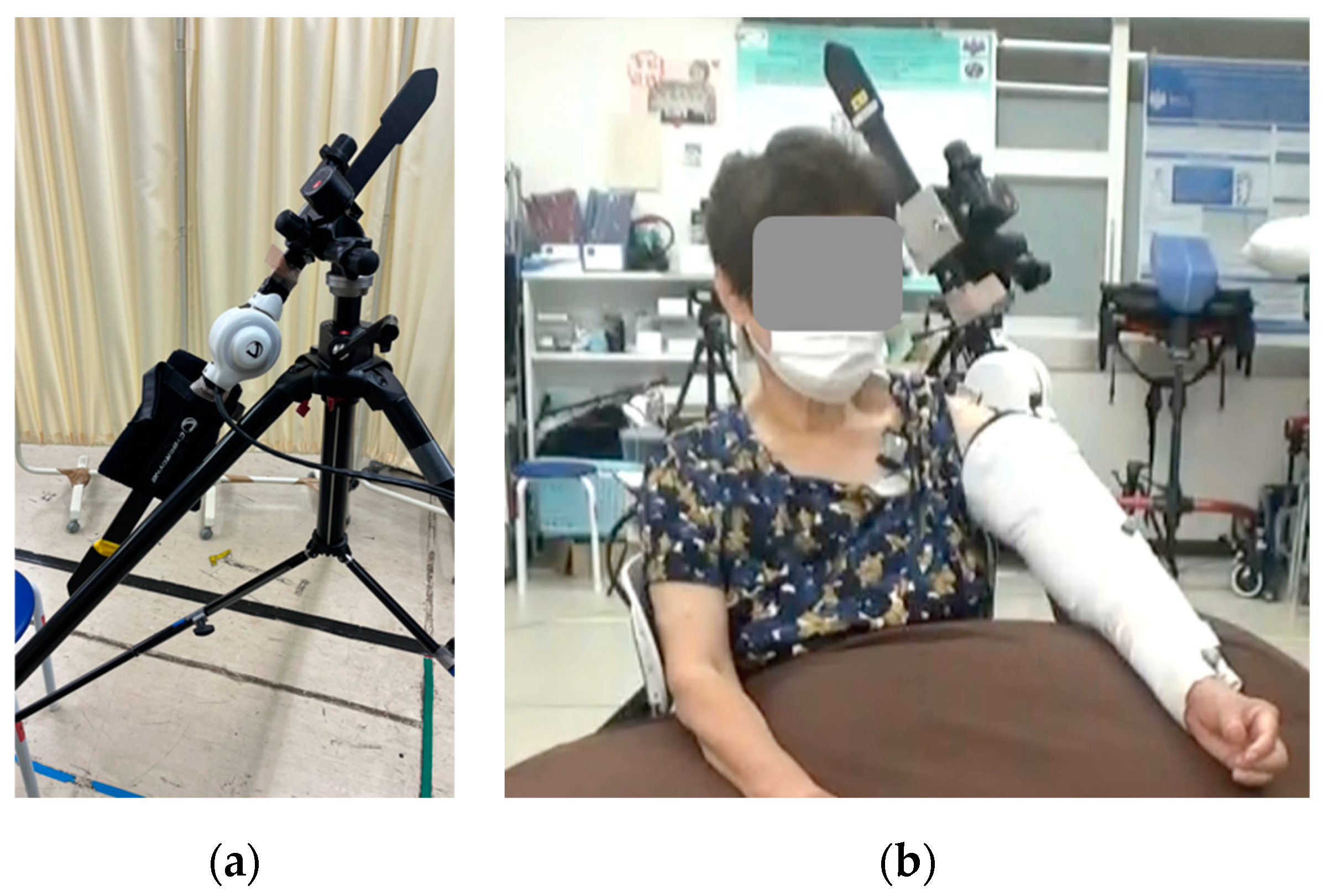
2.2. HAL Intervention
2.3. Assessments
2.3.1. Safety
2.3.2. Efficacy
Shoulder Joint Function
Surface Electromyography
Motion Analysis
Upper Limb Function and Activity
2.4. Statistical Analysis
3. Results
3.1. Safety
3.2. Efficacy
3.2.1. Shoulder Joint Function
3.2.2. Surface Electromyography
3.2.3. Motion Analysis
3.2.4. Upper Limb Function and Activity
4. Discussion
Limitations
5. Conclusions
Supplementary Materials
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Acknowledgments
Conflicts of Interest
References
- Lloyd-Jones, D.; Adams, R.J.; Brown, T.M.; Carnethon, M.; Dai, S.; De Simone, G.; Ferguson, T.B.; Ford, E.; Furie, K.; Gillespie, C.; et al. Executive summary: Heart disease and stroke statistics—2010 update: A report from the American Heart Association. Circulation 2010, 121, 948–954. [Google Scholar] [CrossRef]
- Broeks, J.G.; Lankhorst, G.J.; Rumping, K.; Prevo, A.J. The long-term outcome of arm function after stroke: Results of a follow-up study. Disabil. Rehabil. 1999, 21, 357–364. [Google Scholar] [CrossRef] [PubMed]
- Lai, C.H.; Sung, W.H.; Chiang, S.L.; Lu, L.H.; Lin, C.H.; Tung, Y.C.; Lin, C.H. Bimanual coordination deficits in hands following stroke and their relationship with motor and functional performance. J. Neuroeng. Rehabil. 2019, 16, 101. [Google Scholar] [CrossRef] [PubMed]
- Kwakkel, G.; Kollen, B.J.; van der Grond, J.; Prevo, A.J. Probability of regaining dexterity in the flaccid upper limb: Impact of severity of paresis and time since onset in acute stroke. Stroke 2003, 34, 2181–2186. [Google Scholar] [CrossRef] [PubMed]
- Marshall, R.S.; Perera, G.M.; Lazar, R.M.; Krakauer, J.W.; Constantine, R.C.; Delapaz, R.L. Evolution of cortical activation during recovery from corticospinal tract infarction. Stroke 2000, 31, 656–661. [Google Scholar] [CrossRef]
- Bertani, R.; Melegari, C.; De Cola, M.C.; Bramanti, A.; Bramanti, P.; Calabrò, R.S. Effects of robot-assisted upper limb rehabilitation in stroke patients: A systematic review with meta-analysis. Neurol. Sci. 2017, 38, 1561–1569. [Google Scholar] [CrossRef]
- Saita, K.; Morishita, T.; Arima, H.; Hyakutake, K.; Ogata, T.; Yagi, K.; Shiota, E.; Inoue, T. Biofeedback effect of hybrid assistive limb in stroke rehabilitation: A proof of concept study using functional near infrared spectroscopy. PLoS ONE 2018, 13, e0191361. [Google Scholar] [CrossRef]
- Okuno, T.; Takeuchi, T.; Takeda, E.; Izumi, Y.; Kaji, R. Clinical uses of a robot (hybrid-assisted limb or HAL™) in patients with post-stroke spasticity after botulinum toxin injections. J. Med. Investig. 2021, 68, 297–301. [Google Scholar] [CrossRef]
- Taketomi, M.; Shimizu, Y.; Kadone, H.; Hada, Y.; Yamazaki, M. Hybrid Assistive Limb Intervention for Hemiplegic Shoulder Dysfunction Due to Stroke. Cureus 2021, 13, e19827. [Google Scholar] [CrossRef]
- Kamkar, A.; Irrgang, J.J.; Whitney, S.L. Nonoperative management of secondary shoulder impingement syndrome. J. Orthop. Sports Phys. Ther. 1993, 17, 212–224. [Google Scholar] [CrossRef]
- Lindgren, I.; Lexell, J.; Jönsson, A.C.; Brogårdh, C. Left-sided hemiparesis, pain frequency, and decreased passive shoulder range of abduction are predictors of long-lasting poststroke shoulder pain. PMR 2012, 4, 561–568. [Google Scholar] [CrossRef]
- Olczak, A.; Truszczyńska-Baszak, A. Influence of the passive stabilization of the trunk and upper limb on selected parameters of the hand motor coordination, grip strength and muscle tension, in post-stroke patients. J. Clin. Med. 2021, 10, 2402. [Google Scholar] [CrossRef] [PubMed]
- Pong, Y.P.; Wang, L.Y.; Wang, L.; Leong, C.P.; Huang, Y.C.; Chen, Y.K. Sonography of the shoulder in hemiplegic patients undergoing rehabilitation after a recent stroke. J. Clin. Ultrasound 2009, 37, 199–205. [Google Scholar] [CrossRef] [PubMed]
- Ludewig, P.M.; Cook, T.M. Alterations in shoulder kinematics and associated muscle activity in people with symptoms of shoulder impingement. Phys. Ther. 2000, 80, 276–291. [Google Scholar] [CrossRef]
- Patel, R.M.; Gelber, J.D.; Schickendantz, M.S. The weight-bearing shoulder. J. Am. Acad. Orthop. Surg. 2018, 26, 3–13. [Google Scholar] [CrossRef] [PubMed]
- Puentes, S.; Kadone, H.; Watanabe, H.; Ueno, T.; Yamazaki, M.; Sankai, Y.; Marushima, A.; Suzuki, K. Reshaping of bilateral gait coordination in hemiparetic stroke patients after early robotic intervention. Front. Neurosci. 2018, 12, 719. [Google Scholar] [CrossRef]
- Shimizu, Y.; Kadone, H.; Kubota, S.; Ueno, T.; Sankai, Y.; Hada, Y.; Yamazaki, M. Voluntary elbow extension-flexion using single joint Hybrid Assistive Limb (HAL) for patients with spastic cerebral palsy: Two case reports. Front. Neurol. 2019, 10, 2. [Google Scholar] [CrossRef]
- Kubota, S.; Kadone, H.; Shimizu, Y.; Takahashi, H.; Koda, M.; Miura, K.; Watanabe, H.; Suzuki, K.; Hada, Y.; Sankai, Y.; et al. Robotic shoulder rehabilitation with the hybrid assistive limb in a patient with delayed recovery after postoperative C5 palsy: A case report. Front. Neurol. 2021, 12, 676352. [Google Scholar] [CrossRef]
- Lafitte, M.N.; Kadone, H.; Kubota, S.; Shimizu, Y.; Tan, C.K.; Koda, M.; Hada, Y.; Sankai, Y.; Suzuki, K.; Yamazaki, M. Alteration of muscle activity during voluntary rehabilitation training with single-joint Hybrid Assistive Limb (HAL) in patients with shoulder elevation dysfunction from cervical origin. Front. Neurosci. 2022, 16, 817659. [Google Scholar] [CrossRef]
- Tigrini, A.; Pettinari, L.A.; Verdini, F.; Fioretti, S.; Mengarelli, A. Shoulder Motion Intention Detection Through Myoelectric Pattern Recognition. IEEE Sens. Lett. 2021, 5, 1–4. [Google Scholar] [CrossRef]
- Tigrini, A.; Scattolini, M.; Mengarelli, A.; Fioretti, S.; Morettini, M.; Burattini, L.; Verdini, F. (Eds.) Role of the Window Length for Myoelectric Pattern Recognition in Detecting User Intent of Motion. In Proceedings of the 2022 IEEE International Symposium on Medical Measurements and Applications (MeMeA), Messing, Italy, 22–24 June 2022. [Google Scholar] [CrossRef]
- Rivela, D.; Scannella, A.; Pavan, E.E.; Frigo, C.A.; Belluco, P.; Gini, G. Analysis and Comparison of Features and Algorithms to Classify Shoulder Movements from sEMG Signals. IEEE Sens. J. 2018, 18, 3714–3721. [Google Scholar] [CrossRef]
- Rivela, D.; Scannella, A.; Pavan, E.E.; Frigo, C.A.; Belluco, P.; Gini, G. (Eds.) Processing of surface EMG through pattern recognition techniques aimed at classifying shoulder joint movements. In Proceedings of the 2015 37th Annual International Conference of the IEEE Engineering in Medicine and Biology Society (EMBC), Milan, Italy, 25–29 August 2015. [Google Scholar] [CrossRef]
- Sharba, G.K.; Wali, M.K.; Ai-Timemy, A.H. Real-time classification of shoulder girdle motions for multifunctional prosthetic hand control: A preliminary study. Int. J. Artif. Organs 2019, 42, 508–515. [Google Scholar] [CrossRef] [PubMed]
- Nsugbe, E.; Al-Timemy, A.H. Shoulder girdle recognition using electrophysiological and low frequency anatomical contraction signals for prosthesis control. CAAI Trans. Intell. Technol. 2022, 7, 81–94. [Google Scholar] [CrossRef]
- Makihara, T.; Kadone, H.; Onishi, S.; Kubota, S.; Hada, Y.; Shimizu, Y.; Kawamoto, H.; Sankai, Y.; Yamazaki, M. Shoulder motion assistance using a single-joint Hybrid Assistive Limb® robot: Evaluation of its safety and validity in healthy adults. J. Orthop. Surg. 2017, 25, 2309499017727951. [Google Scholar] [CrossRef] [PubMed]
- Nakayama, H.; Jørgensen, H.S.; Raaschou, H.O.; Olsen, T.S. Recovery of upper extremity function in stroke patients: The Copenhagen Stroke Study. Arch. Phys. Med. Rehabil. 1994, 75, 394–398. [Google Scholar] [CrossRef]
- Pollock, A.; Baer, G.; Campbell, P.; Choo, P.L.; Forster, A.; Morris, J.; Pomeroy, V.M.; Langhorne, P. Physical rehabilitation approaches for the recovery of function and mobility following stroke. Cochrane Database Syst. Rev. 2014, 2014, CD001920. [Google Scholar] [CrossRef]
- Hsieh, C.L.; Hsueh, I.P.; Chiang, F.M.; Lin, P.H. Inter-rater reliability and validity of the action research arm test in stroke patients. Age Ageing 1998, 27, 107–113. [Google Scholar] [CrossRef]
- Slota, G.P.; Enders, L.R.; Seo, N.J. Improvement of hand function using different surfaces and identification of difficult movement post stroke in the Box and Block Test. Appl. Ergon. 2014, 45, 833–838. [Google Scholar] [CrossRef]
- Jolkkonen, J.; Kwakkel, G. Translational hurdles in stroke recovery studies. Transl. Stroke Res. 2016, 7, 331–342. [Google Scholar] [CrossRef]







| Number | Age | Sex | Disease | Side | From Onset (Year) | Shoulder MMT | Grip Strength (kg) | ||
|---|---|---|---|---|---|---|---|---|---|
| Affected Side | Unaffected Side | Affected Side | Unaffected Side | ||||||
| 1 | 53 | Female | SAH | Rt | 1.98 | 2 | 5 | 0 | 17.8 |
| 2 | 84 | Male | ICH | Rt | 8.24 | 2 | 5 | 8.1 | 31.3 |
| 3 | 67 | Male | CI | Lt | 0.93 | 2 | 5 | 9.7 | 26.3 |
| 4 | 68 | Male | ICH | Rt | 8.65 | 2 | 5 | 0 | 33.4 |
| 5 | 71 | Male | CI | Lt | 1.60 | 2 | 5 | 6.7 | 30.3 |
| 6 | 68 | Male | CI | Lt | 4.57 | 2 | 5 | 15.7 | 35.1 |
| 7 | 67 | Male | ICH | Lt | 1.20 | 2 | 5 | 11 | 27.5 |
| 8 | 69 | Female | CI | Lt | 19.7 | 2 | 5 | 0 | - |
Disclaimer/Publisher’s Note: The statements, opinions and data contained in all publications are solely those of the individual author(s) and contributor(s) and not of MDPI and/or the editor(s). MDPI and/or the editor(s) disclaim responsibility for any injury to people or property resulting from any ideas, methods, instructions or products referred to in the content. |
© 2023 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Taketomi, M.; Shimizu, Y.; Kadone, H.; Kubota, S.; Kagai, Y.; Okamoto, Y.; Hada, Y.; Yamazaki, M. Shoulder Joint Hybrid Assistive Limb Treatment for Chronic Stroke Patients with Upper Limb Dysfunction. J. Clin. Med. 2023, 12, 1215. https://doi.org/10.3390/jcm12031215
Taketomi M, Shimizu Y, Kadone H, Kubota S, Kagai Y, Okamoto Y, Hada Y, Yamazaki M. Shoulder Joint Hybrid Assistive Limb Treatment for Chronic Stroke Patients with Upper Limb Dysfunction. Journal of Clinical Medicine. 2023; 12(3):1215. https://doi.org/10.3390/jcm12031215
Chicago/Turabian StyleTaketomi, Masakazu, Yukiyo Shimizu, Hideki Kadone, Shigeki Kubota, Yuta Kagai, Yoshitaka Okamoto, Yasushi Hada, and Masashi Yamazaki. 2023. "Shoulder Joint Hybrid Assistive Limb Treatment for Chronic Stroke Patients with Upper Limb Dysfunction" Journal of Clinical Medicine 12, no. 3: 1215. https://doi.org/10.3390/jcm12031215
APA StyleTaketomi, M., Shimizu, Y., Kadone, H., Kubota, S., Kagai, Y., Okamoto, Y., Hada, Y., & Yamazaki, M. (2023). Shoulder Joint Hybrid Assistive Limb Treatment for Chronic Stroke Patients with Upper Limb Dysfunction. Journal of Clinical Medicine, 12(3), 1215. https://doi.org/10.3390/jcm12031215






