Effect of Supplemental Oxygen on von Willebrand Factor Activity and Ristocetin Cofactor Activity in Patients at Risk for Cardiovascular Complications Undergoing Moderate-to High-Risk Major Noncardiac Surgery—A Secondary Analysis of a Randomized Trial
Abstract
:1. Introduction
2. Materials and Methods
3. Results
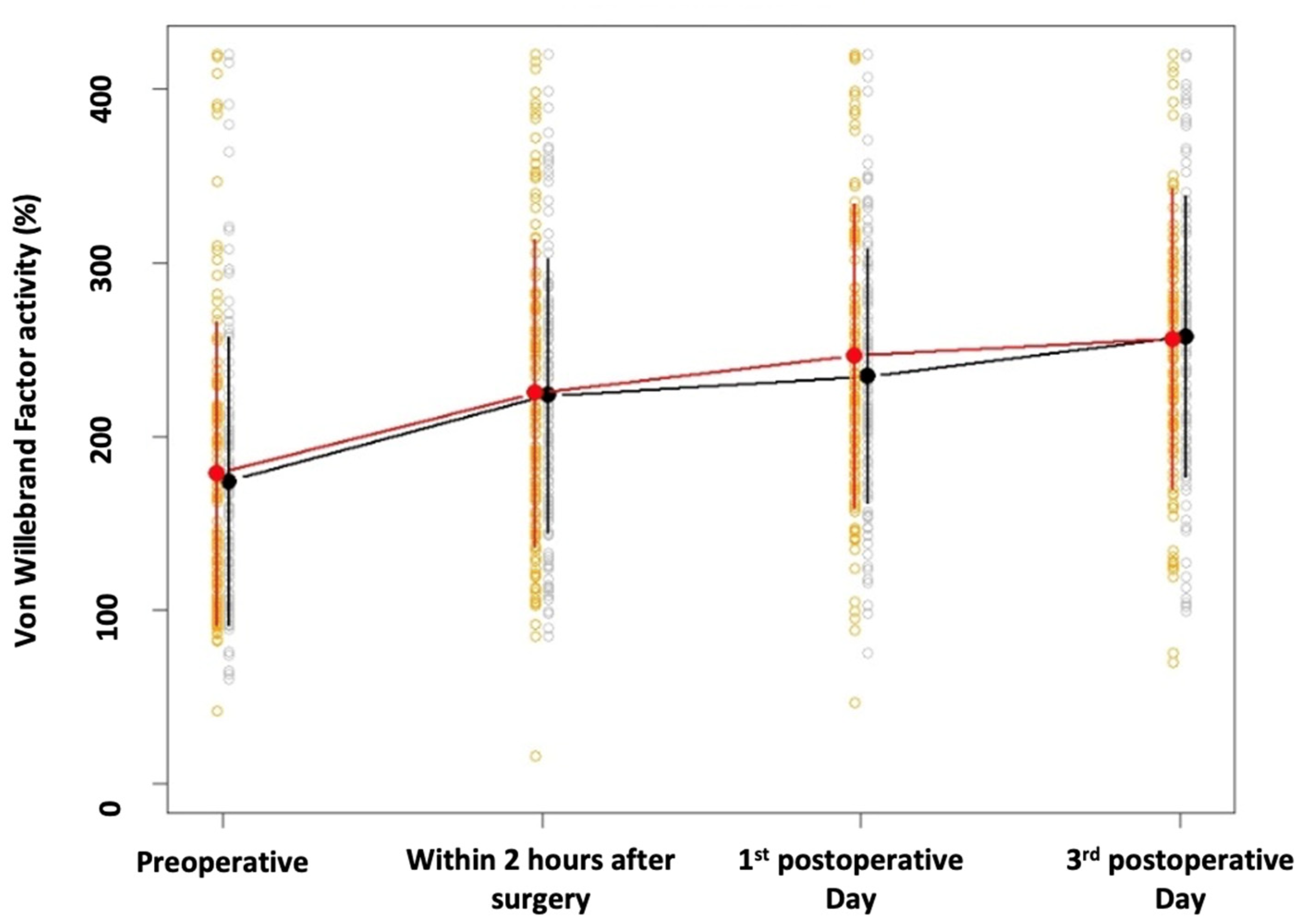
3.1. Primary Outcome
3.2. Secondary Outcome: Ristocetin Cofactor Activity
3.3. Analyses of Possible Confounding Factors
3.3.1. Von Willebrand Factor Activity
3.3.2. Ristocetin Cofactor Activity
3.3.3. vWF Activity and SORP
4. Discussion
5. Conclusions
Supplementary Materials
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Conflicts of Interest
References
- Heit, J.A. Epidemiology of venous thromboembolism. Nat. Rev. Cardiol. 2015, 12, 464–474. [Google Scholar] [CrossRef] [PubMed]
- Stevens, J.L.; Feelisch, M.; Martin, D.S. Perioperative Oxidative Stress: The Unseen Enemy. Anesth. Analg. 2019, 129, 1749–1760. [Google Scholar] [CrossRef] [PubMed]
- Williams, M.; Azcutia, V.; Newton, G.; Alcaide, P. Emerging mechanisms of neutrophil recruitment across endothelium. Trends Immunol. 2011, 32, 461–469. [Google Scholar] [CrossRef] [PubMed]
- Ley, K.; Laudanna, C.; Cybulsky, M.I.; Nourshargh, S. Getting to the site of inflammation: The leukocyte adhesion cascade updated. Nat. Rev. Immunol. 2007, 7, 678–689. [Google Scholar] [CrossRef]
- Randi, A.M.; Laffan, M.A. Von Willebrand factor and angiogenesis: Basic and applied issues. J. Thromb. Haemost. 2017, 15, 13–20. [Google Scholar] [CrossRef]
- Kawecki, C.; Lenting, P.J.; Denis, C.V. von Willebrand factor and inflammation. J. Thromb. Haemost. 2017, 15, 1285–1294. [Google Scholar] [CrossRef]
- Bierings, R.; Voorberg, J. Up or out: Polarity of VWF release. Blood 2016, 128. [Google Scholar] [CrossRef]
- Ikeda, M.; Iwamoto, S.I.; Imamura, H.; Furukawa, H.; Kawasaki, T. Increased platelet aggregation and production of platelet-derived microparticles after surgery for upper gastrointestinal malignancy. J. Surg. Res. 2003, 115, 174–183. [Google Scholar] [CrossRef]
- Marc Samama, C.; Thiry, D.; Elalamy, I.; Diaby, M.; Guillosson, J.J.; Kieffer, E.; Coriat, P. Perioperative activation of hemostasis in vascular surgery patients. Anesthesiology 2001, 94, 74–78. [Google Scholar] [CrossRef]
- D’Amore, P.A.; Sweet, E. Effects of hyperoxia on microvascular cells in vitro. Vitr. Cell. Dev. Biol. 1987, 23, 123–128. [Google Scholar] [CrossRef]
- Junod, A.F.; Jornot, L.; Petersen, H. Differential effects of hyperoxia and hydrogen peroxide on DNA damage, polyadenosine diphosphate-ribose polymerase activity, and nicotinamide adenine dinucleotide and adenosine triphosphate contents in cultured endothelial cells and fibroblasts. J. Cell Physiol. 1989, 140, 177–185. [Google Scholar] [CrossRef] [PubMed]
- Singer, M.; Young, P.J.; Laffey, J.G.; Asfar, P.; Taccone, F.S.; Skrifvars, M.B.; Meyhoff, C.S.; Radermacher, P. Dangers of hyperoxia. Crit. Care 2021, 25, 440. [Google Scholar] [CrossRef]
- Allegranzi, B.; Zayed, B.; Bischoff, P.; Kubilay, N.Z.; de Jonge, S.; de Vries, F.; Gomes, S.M.; Gans, S.; Wallert, E.D.; Wu, X.; et al. New WHO recommendations on intraoperative and postoperative measures for surgical site infection prevention: An evidence-based global perspective. Lancet Infect. Dis. 2016, 16, e288–e303. [Google Scholar] [CrossRef] [PubMed]
- Kurz, A.; Kopyeva, T.; Suliman, I.; Podolyak, A.; You, J.; Lewis, B.; Vlah, C.; Khatib, R.; Keebler, A.; Reigert, R.; et al. Supplemental oxygen and surgical-site infections: An alternating intervention controlled trial. Br. J. Anaesth. 2018, 120, 117–126. [Google Scholar] [CrossRef]
- Meyhoff, C.S.; Wetterslev, J.; Jorgensen, L.N.; Henneberg, S.W.; Høgdall, C.; Lundvall, L.; Svendsen, P.E.; Mollerup, H.; Lunn, T.H.; Simonsen, I.; et al. Effect of High Perioperative Oxygen Fraction on Sugical Site Infection and Pilmonary Complications After abdominal Surgery. JAMA 2009, 302, 1543–1550. [Google Scholar] [CrossRef]
- Kabon, B.; Kurz, A. Optimal perioperative oxygen administration. Curr. Opin. Anaesthesiol. 2006, 19, 11–18. [Google Scholar] [CrossRef]
- Reiterer, C.; Kabon, B.; von Sonnenburg, M.F.; Starlinger, P.; Taschner, A.; Zotti, O.; Goshin, J.; Drlicek, G.; Fleischmann, E. The effect of supplemental oxygen on perioperative brain natriuretic peptide concentration in cardiac risk patients—A protocol for a prosprective randomized clinical trial. Trials 2020, 21, 400. [Google Scholar] [CrossRef] [PubMed]
- Zheng, H.; Ma, H.P.; Chen, L.; Zhan, H.T.; Guo, H. Prethrombotic state and cardiac events in patients with coronary heart disease during noncardiac surgery. Clin. Appl. Thromb. Hemost. 2014, 20, 84–90. [Google Scholar] [CrossRef]
- Reiterer, C.; Kabon, B.; Taschner, A.; von Sonnenburg, M.F.; Graf, A.; Adamowitsch, N.; Starlinger, P.; Goshin, J.; Fraunschiel, M.; Fleischmann, E. Perioperative supplemental oxygen and NT-proBNP concentrations after major abdominal surgery—A prospective randomized clinical trial. J. Clin. Anesth. 2021, 73, 110379. [Google Scholar] [CrossRef]
- Taschner, A.; Kabon, B.; Falkner von Sonnenburg, M.; Graf, A.; Adamowitsch, N.; Fraunschiel, M.; Fleischmann, E.; Reiterer, C. Perioperative Supplemental Oxygen and Plasma Catecholamine Concentrations after Major Abdominal Surgery—Secondary Analysis of a Randomized Clinical Trial. J. Clin. Med. 2022, 11, 1767. [Google Scholar] [CrossRef]
- Taschner, A.; Kabon, B.; Graf, A.; Adamowitsch, N.; Falkner von Sonnenburg, M.; Fraunschiel, M.; Horvath, K.; Fleischmann, E.; Reiterer, C. Perioperative Supplemental Oxygen and Postoperative Copeptin Concentration in Cardiac-Risk Patients Undergoing Major Abdominal Surgery—A Secondary analysis of a Randomized Clinical Trail. J. Clin. Med. 2022, 11, 2085. [Google Scholar] [CrossRef] [PubMed]
- Reiterer, C.; Fleischmann, E.; Taschner, A.; Adamowitsch, N.; von Sonnenburg, M.F.; Graf, A.; Fraunschiel, M.; Starlinger, P.; Goschin, J.; Kabon, B. Perioperative supplemental oxygen and oxidative stress in patients undergoing moderate- to high-risk major abdominal surgery—A subanalysis of randomized clinical trial. J. Clin. Anesth. 2022, 77, 110614. [Google Scholar] [CrossRef] [PubMed]
- Holse, C.; Aasvang, E.K.; Vester-Andersen, M.; Rasmussen, L.S.; Wetterslev, J.; Christensen, R.; Jorgensen, L.N.; Pedersen, S.S.; Loft, F.C.; Troensegaard, H.; et al. Hyperoxia and Antioxidants for Myocardial Injury in Noncardiac Surgery: A 2 × 2 Factorial, Blinded, Randomized Clinical Trial. Anesthesiology 2022, 136, 408–419. [Google Scholar] [CrossRef] [PubMed]
- Jiang, Q.; Kurz, A.; Zhang, X.; Liu, L.; Yang, D.; Sessler, D.I. Supplemental Intraoperative Oxygen and Long-term Mortality: Subanalysis of a Multiple Crossover Cluster Trial. Anesthesiology 2021, 134, 709–721. [Google Scholar] [CrossRef]
- Devereaux, P.J.; Goldman, L.; Cook, D.J.; Gilbert, K.; Leslie, K.; Guyatt, G.H. Perioperative cardiac events in patients undergoing noncardiac surgery: A review of the magnitude of the problem, the pathophysiology of the events and methods to estimate and communicate risk. Cmaj 2005, 173, 627–634. [Google Scholar] [CrossRef]
- Kalinin, R.E.; Suchkov, I.A.; Mzhavanadze, N.D.; Zhurina, O.N.; Klimentova, E.A.; Povarov, V.O. Coagulation factor activity and hemostatic markers of endothelial dysfunction in patients with peripheral arterial disease. Vasc. Spec. Int. 2021, 37, 26. [Google Scholar] [CrossRef]
- Obradovic, M.; Kurz, A.; Kabon, B.; Roth, G.; Kimberger, O.; Zotti, O.; Bayoumi, A.; Reiterer, C.; Stift, A.; Fleischmann, E. The effect of intraoperative goal-directed crystalloid versus colloid administration on perioperative inflammatory markers- Asubstudy of a randomized controlled trial. BMC Anesthesiol. 2020, 20, 210. [Google Scholar] [CrossRef]
- Noblett, S.E.; Snowden, C.P.; Shenton, B.K.; Horgan, A.F. Randomized clinical trial assessing the effect of Doppler-optimized fluid management on outcome after elective colorectal resection. Br. J. Surg. 2006, 93, 1069–1076. [Google Scholar] [CrossRef]
- Pagano, A.; Barazzone-Argiroffo, C. Alveolar Cell Death in Hypoeroxia-Induces Lung Injury. Ann. N Y Acad. Sci. 2003, 1010, 405–416. [Google Scholar] [CrossRef]
- Hafner, C.; Wu, J.; Tiboldi, A.; Hess, M.; Mitulovic, G.; Kaun, C.; Krychtiuk, K.A.; Wojta, J.; Ullrich, R.; Tretter, E.V.; et al. Hyperoxia induces inflammation and cytotoxicity in human adult cardiac monocytes. Shock 2017, 47, 436–444. [Google Scholar] [CrossRef]
- Patmore, S.; Dhami, S.P.S.; O’Sullivan, J.M. Von Willebrand factor and cancer; metastasis and coagulopathies. J. Thromb. Haemost. 2020, 18, 2444–2456. [Google Scholar] [CrossRef]
- Wun, T.; White, R.H. Epidemiology of cancer-related venous thromboembolism. Best Pract. Res. Clin. Haematol. 2009, 22, 9–23. [Google Scholar] [CrossRef] [PubMed]
- Narula, N.; Olin, J.W.; Narula, N. Pathologic Disparities between Peripheral Artery Disease and Coronary Artery Disease. Arterioscler. Thromb. Vasc. Biol. 2020, 40, 1982–1989. [Google Scholar] [CrossRef] [PubMed]
- Makin, A.J.; Chung, N.A.Y.; Silverman, S.H.; Lip, G.Y.H. Alterations of thrombogenesis, endothelial damage and oxidative stress with reperfusion during femoral artery bypass surgery for peripheral vascular disease. Pathophysiol. Haemost. Thromb. 2002, 32, 158–164. [Google Scholar] [CrossRef] [PubMed]
- Blann, A.D.; Seigneur, M.; Steiner, M.; Boisseau, M.R.; Mccollum, C.N. Circulating endothelial cell markers in peripheral vascular disease: Relationship to the location and extent of atherosclerotic disease. Eur. J. Clin. Investig. 1997, 27, 916–921. [Google Scholar] [CrossRef] [PubMed]
- Heeschen, C.; Dimmeler, S.; Hamm, C.W.; van den Brand, M.J.; Boersma, E.; Zeiher, A.M.; Simoons, M.L. Soluble CD40 Ligand in Acute Coronary Syndromes. N. Engl. J. Med. 2003, 348, 1104–1111. [Google Scholar] [CrossRef]
- Touyz, R.M. Molecular and cellular mechanisms in vascular injury in hypertension: Role of angiotensin II. Curr. Opin. Nephrol. Hypertens. 2005, 14, 125–131. [Google Scholar] [CrossRef]
- Jenkins, P.V.; O’Donnell, J.S. ABO blood group determines plasma von Willebrand factor levels: A biologic function after all? Transfusion 2006, 46, 1836–1844. [Google Scholar] [CrossRef]
- Ward, S.E.; O’Sullivan, J.M.; O’Donnell, J.S. The relationship between ABO blood group, von Willebrand factor, and primary hemostasis. Blood 2020, 136, 2864–2874. [Google Scholar] [CrossRef]
- Jick, H.; Westerholm, B.; Vessey, M.; Lewis, G.; Slone, D.; Inman, W.W.; Shapiro, S.; Worcester, J. Venous thromboembolic disease and abo blood type. A cooperative study. Obstet. Gynecol. Surv. 1969, 24, 539–542. [Google Scholar] [CrossRef]
- Wiggins, K.L.; Smith, N.L.; Glazer, N.L.; Rosendaal, F.R.; Heckbert, S.R.; Psaty, B.M.; Rice, K.M.; Lumley, T. ABO genotype and risk of thrombotic events and hemorrhagic stroke. J. Thromb. Haemost. 2009, 7, 263–269. [Google Scholar] [CrossRef] [PubMed]
- Carpeggiani, C.; Coceani, M.; Landi, P.; Michelassi, C.; L’Abbate, A. ABO blood group alleles: A risk factor for coronary artery disease. An angiographic study. Atherosclerosis 2010, 211, 461–466. [Google Scholar] [CrossRef] [PubMed]
- Sari, I.; Ozer, O.; Davutoglu, V.; Gorgulu, S.; Eren, M.; Aksoy, M. ABO blood group distribution and major cardiovascular risk factors in patients with acute myocardial infarction. Blood Coagul. Fibrinolysis 2008, 19, 231–234. [Google Scholar] [CrossRef] [PubMed]
- Cassar, K.; Bachoo, P.; Ford, I.; Greaves, M.; Brittenden, J. Markers of coagulation activation, endothelial stimulation and inflammation in patients with peripheral arterial disease. Eur. J. Vasc. Endovasc. Surg. 2005, 29, 171–176. [Google Scholar] [CrossRef] [Green Version]
| 80% Oxygen | 30% Oxygen | p-Value | |||
|---|---|---|---|---|---|
| vWF activity, % | |||||
| Baseline | 156.5 | [112.75; 212.5] | 155.5 | [119; 200.75] | 0.78 |
| 2 h postoperative | 211 | [160; 274.5] | 214 | [163; 266] | 0.85 |
| Postoperative day 1 | 228 | [180; 315.75] | 219.5 | [186; 279.5] | 0.45 |
| Postoperative day 3 | 244 | [199.5; 302] | 256 | [193; 317] | 0.82 |
| Ristocetin cofactor activity, % | |||||
| Baseline | 142.5 | [113.75; 208.75] | 152 | [116.5; 199.5] | 0.88 |
| 2 h postoperative | 227.5 | [164.25; 306.25] | 247 | [198; 315] | 0.19 |
| Postoperative day 1 | 255.5 | [190; 359.75] | 245 | [201; 286] | 0.56 |
| Postoperative day 3 | 247.5 | [199.25; 311] | 270 | [203.5; 340] | 0.36 |
| Variable | Comparison | Effect | Lower CL | Upper CL | p-Value |
|---|---|---|---|---|---|
| Time | Overall Trend Test | 19.264 | 17.040 | 21.488 | <0.001 |
| pre vs. 2 h post | −46.672 | −55.050 | −38.295 | <0.001 | |
| pre vs. POD 1 | −62.434 | −70.973 | −53.894 | <0.001 | |
| pre vs. POD 3 | −80.874 | −89.720 | −72.028 | <0.001 | |
| Time × Group | Overall Trend Test | 0.297 | −4.154 | 4.749 | 0.896 |
| Group 30% vs. 80% pre | −2.964 | −23.547 | 17.619 | 0.777 | |
| Group 30% vs. 80% 2 h post | 0.099 | −20.528 | 20.726 | 0.993 | |
| Group 30% vs. 80% POD 1 | −11.570 | −32.475 | 9.335 | 0.277 | |
| Group 30% vs. 80% POD 3 | 0.507 | −20.852 | 21.866 | 0.963 | |
| Group 30% pre vs. 2 h post | −48.180 | −59.995 | −36.365 | <0.001 | |
| Group 30% pre vs. POD 1 | −57.891 | −70.157 | −45.625 | <0.001 | |
| Group 30% pre vs. POD 3 | −82.617 | −95.187 | −70.048 | <0.001 | |
| Group 80% pre vs. 2 h post | −45.117 | −57.009 | −33.224 | <0.001 | |
| Group 80% pre vs. POD 1 | −66.497 | −78.401 | −54.584 | <0.001 | |
| Group 80%: pre vs. POD 3 | −79.146 | −91.610 | −66.682 | <0.001 | |
| Type of surgery | Laparoscopic vs. Open | −48.264 | −66.232 | −30.297 | <0.001 |
| Time × Type of surgery | Overall Trend Test | 1.523 | −3.171 | 6.216 | 0.524 |
| Liver | Yes vs. No | 10.534 | −19.790 | 40.858 | 0.495 |
| Colorectal | Yes vs. No | −11.296 | −31.163 | 13.330 | 0.431 |
| Pancreatic | Yes vs. No | 55.257 | 29.981 | 80.534 | <0.001 |
| Renal | Yes vs. No | −38.300 | −62.435 | −14.166 | 0.002 |
| Prostatectomy | Yes vs. No | −36.031 | −64.046 | −8.017 | 0.012 |
| Cystectomy | Yes vs. No | −17.482 | −48.574 | 13.610 | 0.269 |
| Gynecological | Yes vs. No | 27.488 | −19.689 | 74.660 | 0.252 |
| Other | Yes vs. No | 3.228 | −26.021 | 32.477 | 0.828 |
| Age | 1.059 | −0.134 | 2.252 | 0.082 | |
| BMI | 0.301 | −1.552 | 2.154 | 0.750 | |
| Sex | Female vs. Male | 19.584 | 0.561 | 38.607 | 0.044 |
| ASA | 3,4 vs. 1,2 | 15.168 | −4.580 | 34.916 | 0.132 |
| History of Coronary Artery Disease | Yes vs. No | 2.912 | −18.077 | 23.901 | 0.785 |
| History of Peripheral Artery Disease | Yes vs. No | 26.660 | 1.698 | 51.622 | 0.036 |
| History of stroke | Yes vs. No | −2.287 | −34.760 | 30.186 | 0.890 |
| History of Heart failure | Yes vs. No | 8.693 | −26.490 | 43.875 | 0.627 |
| Diabetes | Yes vs. No | −0.345 | −20.530 | 19.839 | 0.973 |
| History of Hypertension | Yes vs. No | −26.494 | −61.876 | 8.889 | 0.142 |
| Blood type | 0 vs. A,B,AB | 51.242 | 32.961 | 69.523 | <0.001 |
| pre ADAMTS | 0.002 | −0.100 | 0.105 | 0.962 | |
| Type of surgery | Laparoscopic vs. Open | −48.264 | −66.232 | −30.297 | <0.001 |
| Blood Loss | 0.007 | −0.007 | 0.021 | 0.345 |
| Variable | Comparison | Effect | Lower CL | Upper CL | p-Value |
|---|---|---|---|---|---|
| Time | pre vs. 2 h post | −45.736 | −54.239 | −37.233 | <0.001 |
| pre vs. POD 1 | −61.587 | −70.243 | −52.931 | <0.001 | |
| pre vs. POD 3 | −80.248 | −80.305 | −89.272 | <0.001 | |
| Type of surgery | Laparoscopic vs. Open | −30.367 | −50.177 | −10.557 | 0.003 |
| Sex | Female vs. Male | 18.570 | 1.194 | 35.946 | 0.036 |
| History of Peripheral Artery Disease | Yes vs. No | 26.305 | 4.018 | 48.592 | 0.021 |
| Blood type | 0 vs. A,B,AB | 55.529 | 38.568 | 72.489 | <0.001 |
| Pancreatic | Yes vs. No | 28.625 | 5.024 | 52.225 | 0.018 |
| Renal | Yes vs. No | −16.297 | −41.125 | 8.531 | 0.197 |
| Prostatectomy | Yes vs. No | −25.026 | −52.736 | 2.685 | 0.077 |
Disclaimer/Publisher’s Note: The statements, opinions and data contained in all publications are solely those of the individual author(s) and contributor(s) and not of MDPI and/or the editor(s). MDPI and/or the editor(s) disclaim responsibility for any injury to people or property resulting from any ideas, methods, instructions or products referred to in the content. |
© 2023 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Horvath, K.; Taschner, A.; Adamowitsch, N.; Falkner von Sonnenburg, M.; Fleischmann, E.; Kabon, B.; Fraunschiel, M.; Reiterer, C.; Graf, A. Effect of Supplemental Oxygen on von Willebrand Factor Activity and Ristocetin Cofactor Activity in Patients at Risk for Cardiovascular Complications Undergoing Moderate-to High-Risk Major Noncardiac Surgery—A Secondary Analysis of a Randomized Trial. J. Clin. Med. 2023, 12, 1222. https://doi.org/10.3390/jcm12031222
Horvath K, Taschner A, Adamowitsch N, Falkner von Sonnenburg M, Fleischmann E, Kabon B, Fraunschiel M, Reiterer C, Graf A. Effect of Supplemental Oxygen on von Willebrand Factor Activity and Ristocetin Cofactor Activity in Patients at Risk for Cardiovascular Complications Undergoing Moderate-to High-Risk Major Noncardiac Surgery—A Secondary Analysis of a Randomized Trial. Journal of Clinical Medicine. 2023; 12(3):1222. https://doi.org/10.3390/jcm12031222
Chicago/Turabian StyleHorvath, Katharina, Alexander Taschner, Nikolas Adamowitsch, Markus Falkner von Sonnenburg, Edith Fleischmann, Barbara Kabon, Melanie Fraunschiel, Christian Reiterer, and Alexandra Graf. 2023. "Effect of Supplemental Oxygen on von Willebrand Factor Activity and Ristocetin Cofactor Activity in Patients at Risk for Cardiovascular Complications Undergoing Moderate-to High-Risk Major Noncardiac Surgery—A Secondary Analysis of a Randomized Trial" Journal of Clinical Medicine 12, no. 3: 1222. https://doi.org/10.3390/jcm12031222
APA StyleHorvath, K., Taschner, A., Adamowitsch, N., Falkner von Sonnenburg, M., Fleischmann, E., Kabon, B., Fraunschiel, M., Reiterer, C., & Graf, A. (2023). Effect of Supplemental Oxygen on von Willebrand Factor Activity and Ristocetin Cofactor Activity in Patients at Risk for Cardiovascular Complications Undergoing Moderate-to High-Risk Major Noncardiac Surgery—A Secondary Analysis of a Randomized Trial. Journal of Clinical Medicine, 12(3), 1222. https://doi.org/10.3390/jcm12031222






