Review of the Literature on Partial Resections of the Gallbladder, 1898–2022: The Outline of the Conception of Subtotal Cholecystectomy and a Suggestion to Use the Terms ‘Subtotal Open-Tract Cholecystectomy’ and ‘Subtotal Closed-Tract Cholecystectomy’
Abstract
1. Introduction
2. Materials and Methods
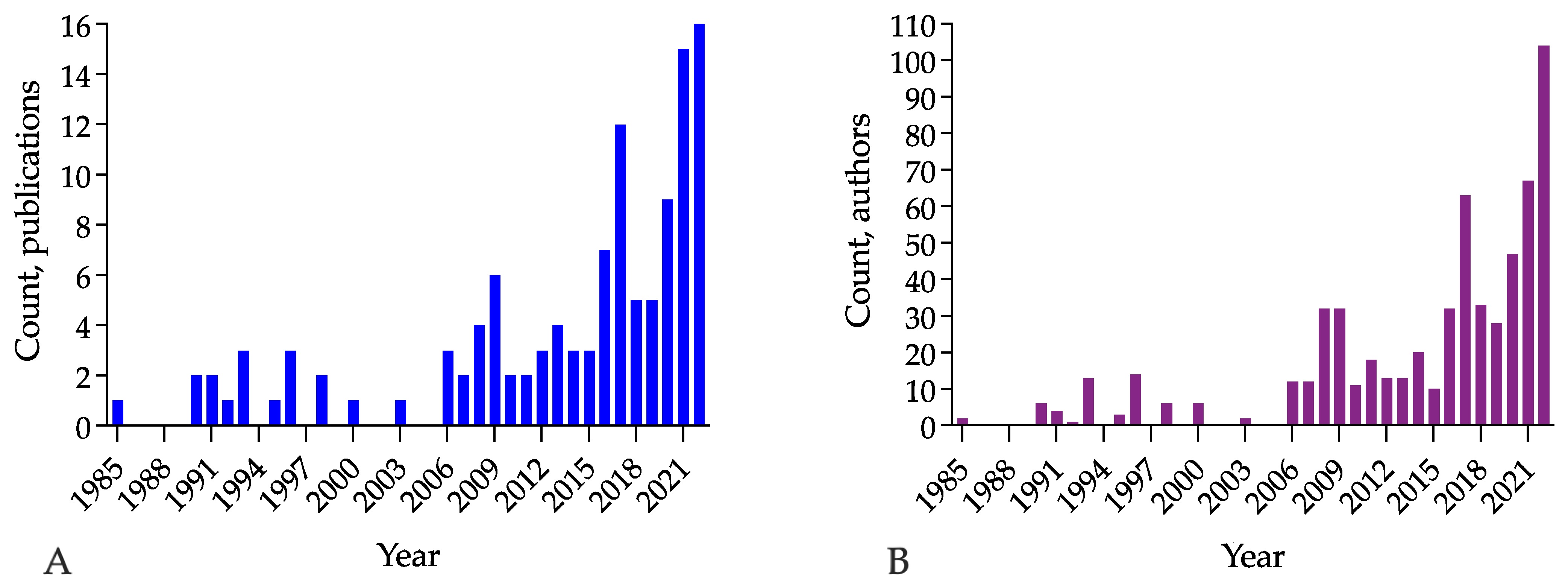
3. Results
3.1. General Overview
3.2. First Described Operations, 1898–1900: Hans Kehr, William J. Mayo, and Bertram C. Stevens
‘The gallbladder is not visible; it is intimately adherent to the inflamed omentum. It is possible only with difficulty to free the gallbladder, which is further adherent to the stomach and the greatest part of the posterior surface of the duodenum. In so doing, its thickened and soft wall tears. There appear in view a number of small to pea-sized roundish yellow stones with thick pus… The stones were removed with forceps. One intends to extirpate the gallbladder but finds the adhesions on the posterior surface separable only with great difficulty; besides, it is also evident that perforations have occurred and stones will lie behind the bladder in the adhesions; the removal of these is very difficult; on this account, one removes so much of the gallbladder wall that only in fact hardened posterior wall and the part of the bladder lying next to the cystic duct remains. With this, severe bleeding occurs from the cystic artery, which is controlled by ligature. Now there yet stick two stones in the cystic duct, which are removed with great difficulty. Then the bladder is sewn upon itself, some omental bands are ligated, a trip of gauze introduced down to the sutures, and the abdominal wall closed…’.
‘Separation of the stomach from the peritoneum; in so doing, the stomach tears, partial suture of the opening. The gallbladder stump is put in anastomosis with the stomach at the point of the tear in the stomach. Cystico-gastrostomy’.
‘Excision of the very fragile gallbladder at the level of the neck. Introduction of the tube into the stump, which is firmly sutured’.
‘A V-shaped portion of the margin of the liver and most of the gall bladder were removed, only a small portion of apparently healthy gall bladder being left… A tube was placed in the cystic duct, and what was left of the gall bladder was sewn firmly around the tube’.
3.3. Limited Resection of the Gallbladder to Reduce Mortality, 1920–1930
‘The gallbladder was dark blue and greatly distended but free of adhesions. As we attempted to lift it into view, it ruptured, revealing the fact that the tissues were exceedingly friable. An incision was made through its entire length, the redundant tissues removed, and bleeding points ligated. As no bile was escaping through the cystic duct, a cigar drain with the tube in the centre was sutured against the remaining mucous surface of the gall bladder. Twenty-four hours later, bile began to flow’.
‘The fundus was incised, a number of small stones were removed, and the mucosa dried and swabbed out with iodine. It was then split from the fundus to the cystic duct, and the redundant wall cut away almost to the liver attachment. A cigar drain was inserted and sutured in position; another was placed in the pouch below. This case has recovered from an operation, and I am very confident it will have no recurrence’.
3.4. Introduction of the Term ‘Partial Cholecystectomy’, 1931: The Series of W. L. Estes Papers
‘A short time later, I was confronted by a case of gangrenous cholecystitis with stones in which complete cholecystectomy was definitely indicated; because of inflammatory induration about the cystic duct; however, this method seemed technically inadvisable and probably dangerous. I therefore resorted to this same splitting of the gallbladder after removal of the stones but supplemented it by trimming off the excess portion of the gallbladder close to the fossa in the liver, attempting to obtain the effect of a complete cholecystectomy to permit drainage of the cystic duct and to avoid a two-stage operation, as is often necessary when only cholecystostomy is done. This partial cholecystectomy I have used in seven carefully selected cases. Convalescence has usually been uneventful; there have been no mortality and no evidence of peritonitis.’
3.5. H. P. Ritchie, 1937: A Technique of Cholecystectomy for the Complicated Case of Gallbladder Disease
‘When the landmarks are clouded, when the excision carries a risk of injury to the structures about the gallbladder, when the integrity of the gallbladder wall is uncertain’.
3.6. Partial Cholecystectomy, Middle of the 20th Century: The Trend in Surgery for Difficult Gallbladder
‘A partial resection of the gallbladder, leaving the portion attached to the liver undisturbed, is, in the presence of sepsis, a safer procedure than complete cholecystectomy, which leaves a denuded, raw gallbladder bed on the liver surface, which is prone to absorb the toxins in the region’.
‘This procedure is occasionally useful if the gallbladder is difficult to access, especially if it tends to be buried in the liver. Additionally, in cases of acute cholecystitis with partial gangrene of the gallbladder, removal of the free portion with coagulation of the part adherent to the liver is the method of choice’.
3.7. Substitutive Methods of Cholecystectomy: Adding the Value to Partial Cholecystectomy Theory
3.7.1. Cholecystectomy by M. Thorek
‘This (i.e., cystic) duct must be exposed and isolated; however, no clamp or ligature should be applied to what is supposed to be the cystic duct until the common hepatic duct, and the common bile duct are clearly observed. I freely admit that there are occasions when the surgeon cannot be satisfied with this anatomical disposition, but in such circumstances, the proper course is either to be content with a partial cholecystectomy, leaving the portion of the viscus just above the neck of the gallbladder, or cholecystostomy’.
3.7.2. Cholecystectomy by W. A. McElmoyle
3.8. The Changing Terminology: Subtotal Cholecystectomy
3.8.1. Morse and Barb, 1947: Introduction of the New Term
3.8.2. Bonilla Naar, 1954: Colombia
3.8.3. Madding, 1955: Subtotal Cholecystectomy as a Modification of Partial Cholecystectomy
‘An incision may then be made from the fundus to within 1 cm of the cystic duct and all stones removed, particularly the one creating the obstruction of the cystic duct. No attempt is made to isolate the cystic duct or artery in the presence of the brawny induration in the hepatoduodenal ligament. When, following the removal of all stones, the redundant flaps of the gallbladder are trimmed off at the liver bed attachment, the procedure has been designated in the literature as partial cholecystectomy, an operation first described in 1899. When the gallbladder is dissected in a retrograde fashion from the surface of the liver proper down to within 1 cm of the cystic duct, the method will be referred to as “subtotal cholecystectomy” and is the preferable procedure… A Penrose drain is then placed into the gallbladder stump, which remains; this gallbladder remanent usually not exceeding 1 cm in diameter. The cuff is then closed about the drain with interrupted catgut sutures. Other drains are placed, and these, in turn, are brought out the lateral angle of the wound where a subcostal type of incision has been used’.
3.8.4. Farrow’s Thesis on Subtotal Cholecystectomy, 1958–1959
3.9. New Wave Developing a Conception of Subtotal Cholecystectomy, 1985–1991: Techniques to Secure a Cystic Duct
3.10. Subtotal Cholecystectomy: Khan’s Modification, 1992
3.11. First Reports on Laparoscopic Subtotal Cholecystectomy, 1993
3.12. The Systematisation of Modalities of Subtotal Cholecystectomy, 1993–2022
3.12.1. Ibrarullah, 1993: Two Modalities of Partial Cholecystectomy
3.12.2. Crosthwaite, 1995, and Michalowski, 1998: Laparoscopic Surgery
3.12.3. Maudar, 1996: Classification of Resections of the Portions of the Gallbladder
3.12.4. Palanivelu, 2006, and Gode, 2014: Three Variants of Subtotal Cholecystectomy
3.12.5. Henneman, 2013: Four Methods of Partial Cholecystectomy
3.12.6. Strasberg, 2016, LeCompte 2020: Fenestrating and Reconstituting Subtypes
3.12.7. Tokyo Guidelines, 2007–2018: Acute Cholecystitis, Severity Grades, and the Surgical Alternatives
3.12.8. Lunevicius, 2020: Subtotal Cholecystectomy Resectional Variants and Subvariants
3.12.9. Purzner 2019, Deng 2022: Five Subtypes of Laparoscopic Subtotal Cholecystectomy
| Author, Year | Resection | Removal of the Gallbladder Wall | Extent of Resection * | Cystic Duct | Gallbladder Remnant | Procedure Completion, by Key Characteristic | ||
|---|---|---|---|---|---|---|---|---|
| Type/Variant/ Method | Subtype/ Subvariant | Peritoneal | Hepatic | |||||
| Ibrarullah, 1993 [46] | PC with retained Hartmann’s pouch (n = 17) | NA | Yes | Yes | 80–90% or more | Open | Closed | Closed-tract STC |
| PC with retained posterior wall (n = 12) | NA | Yes | No | 75% | Closed | Open | Closed-tract STC | |
| Crosthwaite, 1993 [47] | STC, open CD (n = 3) | NA | Removal | In situ | 75% | Open | Open | Open-tract STC |
| STC, closed CD (n = 2) | NA | Removal | In situ | 75% | Closed | Open | Closed-tract STC | |
| Maudar, 1996 [48] | PC (n = 5) | NA | Removal | Removal | 80–90% or more | Open | Closed | Closed-tract STC |
| STC (n = 21) | NA | Removal | In situ | 75% or less | NA | NA | NA | |
| Michalowski, 1996 [52] | STC with isolation and division of CD (n = 27) | NA | Removal | In situ | 75% | Closed | Open | Closed-tract STC |
| STC without isolation and division of CD (n = 2) | NA | Removal | In situ | 75% | Open | Open | Open-tract STC | |
| Palanivelu, 2006 [56] | LSC I (n = 62) | NA | Yes | No | 75% | Open | Open | Open-tract STC |
| LSC II (102) | NA | Yes | Yes | 90% | Open | Closed | Closed-tract STC | |
| LSC III (n = 42) | NA | Yes | No | 75% | Open | Closed | Closed-tract STC | |
| Gode, 2014 [83] | LSC I (n = 48) | NA | Yes | No | 75% | Closed | Closed | Closed-tract STC |
| LSC II (n = 591) | NA | Yes | Yes | 90% | Open | Closed | Closed-tract STC | |
| LSC III (n = 22) | NA | Yes | No | 75% | Open | Closed | Closed-tract STC | |
| Henneman, 2013 ** [159] | Method A | NA | Yes | No | 75% | Open | Open | Open-tract STC |
| Method B | NA | Yes | No | 75% | Open or closed | Closed | Closed-tract STC | |
| Method C | NA | Yes | Yes | 90% | Open | Closed | Closed-tract STC | |
| Method D | NA | Yes | Yes | 90% | Open | Open | Open-tract STC | |
| Strasberg, 2016 LeCompte 2020 [126,160] | NA | Reconstituting | Yes | Yes | 90% | Open | Closed | Closed-tract STC |
| NA | Fenestrating | Yes | No | 75% | Open or closed | Opened | Open-tract STC Closed-tract STC | |
| Lunevicius, 2021 [167] | STC-1 | STC-1A | Removal | Removal | 80–90% or more | Open | Open or Closed | Open-tract STC Closed-tract STC |
| STC-1B | Removal | Removal | 80–90% or more | Open | Open or Closed | Open-tract STC Closed-tract STC | ||
| STC-1C | Removal | Removal | 80–90% or more | Open | Open or Closed | Open-tract STC Closed-tract STC | ||
| STC-2 | STC-2A | Removal | In situ | 75% | Open | Open | Open-tract STC | |
| STC-2B | Removal | Partial | 75% or more | Closed | Open | Closed-tract STC | ||
| STC-3 (fundectomy) | NA | Fundus removal | NA | Fundectomy | Open | Open or Closed | Open-tract STC Closed-tract STC | |
| STC-4 | NA | Removal | In situ | Minimal | Open | Open | Open-tract STC | |
| Purzner, 2019 Deng, 2022 [113,143] | Reconstituting | LSC 1A | Excision | Excision | 80–90% or more | Open | Closed | Closed-tract STC |
| Reconstituting | LSC 1B | Excision | In situ | 75% | Open | Closed | Closed-tract STC | |
| Fenestrating | LSC 2A | Excision | Excision | 80–90% or more | Open | Open | Open-tract STC | |
| Fenestrating | LSC 2B | Excision | In situ | 75% | Open | Open | Open-tract STC | |
| Fenestrating | LSC 3 | Bilateral split | In situ | NA | Open | Open | Open-tract STC | |
4. Discussion
4.1. Historical Evolution and Current Trends
4.2. The Outline of a Conception of Subtotal Cholecystectomy
4.3. Limitations of the Review and Area That Needs Further Research
5. Conclusions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Conflicts of Interest
References
- Ellis, H. Chapter 9: Carl Langenbuch. The first cholecystectomy (1882). In Surgical Case-Histories from the Past; Royal Society of Medicine Press Limited: London, UK, 1994; pp. 57–61. [Google Scholar]
- Kim, Y.; Wima, K.; Jung, A.D.; Martin, G.E.; Dhar, V.K.; Shah, S.A. Laparoscopic subtotal cholecystectomy compared to total cholecystectomy: A matched national analysis. J. Surg. Res. 2017, 218, 316–321. [Google Scholar] [CrossRef] [PubMed]
- Sabour, A.F.; Matsushima, K.; Love, B.E.; Alicuben, E.T.; Schellenberg, M.A.; Inaba, K.; Demetriades, D. Nationwide trends in the use of subtotal cholecystectomy for acute cholecystitis. Surgery 2020, 167, 569–574. [Google Scholar] [CrossRef] [PubMed]
- Lunevicius, R.; Nzenwa, I.C.; Mesri, M. A nationwide analysis of gallbladder surgery in England between 2000 and 2019. Surgery 2022, 171, 276–284. [Google Scholar] [CrossRef] [PubMed]
- Ellis, H. Chapter 5: John Stough Bobbs. The first cholecystostomy for gall stones (1868). In Surgical Case-Histories from the Past; Royal Society of Medicine Press Limited: London, UK, 1994; pp. 31–37. [Google Scholar]
- Sims, J.M. Cholecystotomy for the removal of gall-stones in dropsy of the gall-bladder. Br. Med. J. 1878, 1, 811–815. [Google Scholar] [CrossRef]
- Lunevicius, R.; Haagsma, J.A. Supplementary Material to ‘Subtotal cholecystectomy: Results of a single-centre, registry-based retrospective cohort study of 180 adults in 2011–2018’. Mendeley Data 2020, V1, 85–89. [Google Scholar] [CrossRef]
- Nzenwa, I.C.; Mesri, M.; Lunevicius, R. Risks associated with subtotal cholecystectomy and the factors influencing them: A systematic review and meta-analysis of 85 studies published between 1985 and 2020. Surgery 2021, 170, 1014–1023. [Google Scholar] [CrossRef]
- Nzenwa, I.C.; Mesri, M.; Lunevicius, R. Supplementary Material to ‘Risks associated with subtotal cholecystectomy and the factors influencing them: A systematic review and meta-analysis of 85 studies published between 1985 and 2020’. Mendeley Data 2021, V1, 6–33. [Google Scholar] [CrossRef]
- Baethge, C.; Goldbeck-Wood, S.; Mertens, S. SANRA-a scale for the quality assessment of narrative review articles. Res. Integr. Peer Rev. 2019, 4, 5. [Google Scholar] [CrossRef]
- Kehr, H. Introduction to the Differential Diagnosis of the Separate Forms of Gallstone Disease: Based Upon His Own Experience Gained in 433 Laparotomies for Gallstones; P. Blakiston’s Son & Co.: Philadelphia, PA, USA, 1901; p. 370. [Google Scholar]
- Mayo, W.J. Some observations on the surgery of the gall-bladder and the bile-ducts. Ann. Surg. 1899, 30, 452–458. [Google Scholar] [CrossRef]
- Stevens, B.C. Cholecystectomy: Partial hepatectomy and pylorectomy: Recovery. Br. Med. J. 1901, 1, 878–879. [Google Scholar] [CrossRef]
- Martin, E.D. Complete cholecystostomy vs. cholecystectomy in cases of empyema of the gallbladder. South. M. J. 1926, 14, 198–201. [Google Scholar] [CrossRef]
- Estes, W.L., Jr. Partial cholecystectomy. Arch. Surg. 1931, 23, 119–128. [Google Scholar] [CrossRef]
- Estes, W.L. Acute gangrenous cholecystitis and the use of partial cholecystectomy in its treatment. Am. J. Surg. 1938, 40, 197–204. [Google Scholar] [CrossRef]
- Estes, W.L. Partial cholecystectomy. Arch. Surg. 1938, 36, 849–857. [Google Scholar] [CrossRef]
- Thorek, M. Electrosurgical obliteration of the gallbladder without surgical drainage: As a means of reducing mortality (report of 201 consecutive unselected patients). Am. J. Surg. 1936, 32, 417–434. [Google Scholar] [CrossRef]
- Thorek, M. Electrosurgical obliteration of the gallbladder without surgical drainage. Lancet 1938, 231, 15–20. [Google Scholar] [CrossRef]
- Thorek, M. Experience with electrosurgical obliteration of the gallbladder. JAMA 1954, 154, 738–740. [Google Scholar] [CrossRef]
- Judd, E.S.; Phillips, J.R. Acute cholecystic disease. Ann. Surg. 1933, 98, 771–779. [Google Scholar] [CrossRef]
- McKenty, J. Acute cholecystitis. Can. Med. Assoc. J. 1938, 38, 236–239. [Google Scholar]
- Ritchie, H.P. Suggestion in technic of cholecystectomy for complicated case of gallbladder disease. Surgery 1937, 1, 581–588. [Google Scholar]
- Love, R.M. Modern trends in biliary surgery. Br. J. Surg. 1952, 40, 214–222. [Google Scholar] [CrossRef] [PubMed]
- Turner, G.G. Injuries to the main bile-ducts. Lancet 1944, 13, 621–622. [Google Scholar] [CrossRef]
- Bailey, H.; Love, R.J.M. Electrosurgical obliteration of the gallbladder without drainage: Thoreks’ operation. Brit. Med. J. 1939, 30, 682–683. [Google Scholar] [CrossRef] [PubMed]
- Gurd, F.B. Gall-bladder surgery. Can. Med. Assoc. J. 1940, 43, 34–38. [Google Scholar]
- Morse, L.J.; Barb, J.S. Modified cholecystectomy in fulminating cholecystitis. Surg. Clin. N. Am. 1947, 27, 395–399. [Google Scholar] [CrossRef]
- Love, R.J.M. Diathermy dissection of the gall-bladder. Brit. Med. J. 1947, 5, 11–13. [Google Scholar] [CrossRef]
- Lerner, A. Partial cholecystectomy. Can. Med. Assoc. J. 1950, 63, 54–56. [Google Scholar]
- McElmoyle, W.A. Cholecystectomy: A method for the difficult gall-bladder. Lancet 1954, 266, 1320–1323. [Google Scholar] [CrossRef]
- Pribram, B.O. Mukoklase und drainagelose gallenchirurgie. Zentralbl. Chir. 1928, 55, 773–779. [Google Scholar]
- Pribram, B.O. The electrosurgical operation in gall-bladder diseases: Results of 13 years’ experience. Lancet 1939, 234, 927–929. [Google Scholar] [CrossRef]
- Bonilla Naar, A. Dos nuevas técnicas sobre vesícula y vías biliares: Colecistectomía subtotal, totalizable y endohepatofistulo-yeyunostomía. Prensa Med. Argent. 1954, 41, 1002–1006. [Google Scholar]
- Madding, G.F. Subtotal cholecystectomy in acute cholecystitis. Am. J. Surg. 1955, 89, 604–607. [Google Scholar] [CrossRef]
- Farrow, C.D., Jr. Subtotal cholecystectomy: Its rationale, technic, and postoperative evaluation. J. Am. Osteopath. Assoc. 1958, 58, 235–240. [Google Scholar]
- Farrow, C.D., Jr. Subtotal cholecystectomy; its rationale, technic, and postoperative evaluation. J. Am. Osteopath. Assoc. 1959, 58, 286–291. [Google Scholar]
- Bornman, P.C.; Terblanche, J. Subtotal cholecystectomy: For the difficult gallbladder in portal hypertension and cholecystitis. Surgery 1985, 98, 1–6. [Google Scholar]
- Douglas, P.; Ham, J. Partial cholecystectomy. ANZ J. Surg. 1990, 60, 595–597. [Google Scholar] [CrossRef]
- Bickel, A.; Lunsky, I.; Mizrahi, S.; Stamler, B. Modified subtotal cholecystectomy for high-risk patients. Can. J. Surg. 1990, 33, 13–14. [Google Scholar]
- Schein, M. Partial cholecystectomy. J. R. Coll. Surg. Edinb. 1991, 36, 295–297. [Google Scholar] [CrossRef]
- Cottier, D.J.; McKay, C.; Anderson, J.R. Subtotal cholecystectomy. Br. J. Surg. 1991, 78, 1326–1328. [Google Scholar] [CrossRef]
- Khan, T.F. Modified subtotal cholecystectomy: A procedure for the difficult gall bladder. Med. J. Malays. 1992, 47, 65–68. [Google Scholar]
- Schein, M.; Assalia, A.; Nitecki, S.; Kopelman, D.; Hashmonai, M. Subtotal cholecystectomy: An emergency procedure for the difficult gallbladder and high-risk patient. Harefuah 1993, 124, 191–193, 248. [Google Scholar] [PubMed]
- Bickel, A.; Shtamler, B. Laparoscopic subtotal cholecystectomy. J. Laparoendosc. Surg. 1993, 3, 365–376. [Google Scholar] [CrossRef] [PubMed]
- Ibralullah, M.D.; Kacker, L.K.; Sikora, S.S.; Saxena, R.; Kapoor, V.K.; Kaushik, S.P. Partial cholecystectomy—Safe and effective. HPB Surg. 1993, 7, 61–65. [Google Scholar] [CrossRef] [PubMed]
- Crosthwaite, G.; McKay, C.; Anderson, J.R. Laparoscopic subtotal cholecystectomy. J. R. Coll. Surg. Edinb. 1995, 40, 20–21. [Google Scholar]
- Maudar, K.K. Evaluation of surgical options in difficult gall bladder stone disease. J. Indian Med. Assoc. 1996, 94, 138–140. [Google Scholar]
- Subramaniasivan, N.; Ananthakrishnan, N.; Kate, V.; Smile, R.; Jagdish, S.; Srinivasan, K. Partial cholecystectomy in elective and emergency gall bladder surgery in the high risk patients—A viable and safe option in the ear of laparoscopic surgery. Trop. Gastroenterol. 1996, 17, 49–52. [Google Scholar]
- Katsohis, C.; Prousalidis, J.; Tzardinoglou, E.; Michalopoulos, A.; Fahandidis, E.; Apostolidis, S.; Aletras, H. Subtotal cholecystectomy. HPB Surg. 1996, 9, 133–136. [Google Scholar] [CrossRef]
- Ransom, K.J. Laparoscopic management of acute cholecystitis with subtotal cholecystectomy. Am. Surg. 1998, 64, 955–957. [Google Scholar]
- Michalowski, K.; Bornman, P.C.; Krige, J.E.; Gallagher, P.J.; Terblanche, J. Laparoscopic subtotal cholecystectomy in patients with complicated acute cholecystitis or fibrosis. Br. J. Surg. 1998, 85, 904–906. [Google Scholar] [CrossRef]
- Chowbey, P.K.; Sharma, A.; Khullar, R.; Mann, V.; Baijal, M.; Vashistha, A. Laparoscopic subtotal cholecystectomy: A review of 56 procedures. J. Laparoendosc. Adv. Surg. Tech. A 2000, 10, 31–34. [Google Scholar] [CrossRef]
- Beldi, G.; Glattli, A. Laparoscopic subtotal cholecystectomy for severe cholecystitis. Surg. Endosc. 2003, 17, 1437–1439. [Google Scholar] [CrossRef]
- Ji, W.; Li, L.T.; Li, J.S. Role of laparoscopic subtotal cholecystectomy in the treatment of complicated cholecystitis. Hepatobiliary Pancreat. Dis. Int. 2006, 5, 584–589. [Google Scholar]
- Palanivelu, C.; Rajan, P.S.; Jani, K.; Shetty, A.R.; Sendhilkumar, K.; Senthilnathan, P.; Parthasarthi, R. Laparoscopic cholecystectomy in cirrhotic patients: The role of subtotal cholecystectomy and its variants. J. Am. Coll. Surg. 2006, 203, 145–151. [Google Scholar] [CrossRef]
- Rohatgi, A.; Singh, K.K. Mirizzi syndrome: Laparoscopic management by subtotal cholecystectomy. Surg. Endosc. 2006, 20, 1477–1481. [Google Scholar] [CrossRef]
- Soleimani, M.; Mehrabi, A.; Mood, Z.A.; Fonouni, H.; Kashfi, A.; Buchler, M.W.; Schmidt, J. Partial cholecystectomy as a safe and viable option in the emergency treatment of complex acute cholecystitis: A case series and review of the literature. Am. Surg. 2007, 73, 498–507. [Google Scholar] [CrossRef]
- Sinha, I.; Smith, M.L.; Safranek, P.; Dehn, T.; Booth, M. Laparoscopic subtotal cholecystectomy without cystic duct ligation. Br. J. Surg. 2007, 94, 1527–1529. [Google Scholar] [CrossRef]
- Balakrishnan, S.; Samdani, T.; Singhal, T.; Hussain, A.; Grandy-Smith, S.; Nicholls, J.; El-Hasani, S. Patient experience with gallstone disease in a National Health Service district hospital. JSLS 2008, 12, 389–394. [Google Scholar]
- Philips, J.A.; Lawes, D.A.; Cook, A.J.; Arulampalam, T.H.; Zaborsky, A.; Menzies, D.; Motson, R.W. The use of laparoscopic subtotal cholecystectomy for complicated cholelithiasis. Surg. Endosc. 2008, 22, 1697–1700. [Google Scholar] [CrossRef]
- Horiuchi, A.; Watanabe, Y.; Doi, T.; Sato, K.; Yukumi, S.; Yoshida, M.; Yamamoto, Y.; Sugishita, H.; Kawachi, K. Delayed laparoscopic subtotal cholecystectomy in acute cholecystitis with severe fibrotic adhesions. Surg. Endosc. 2008, 22, 2720–2723. [Google Scholar] [CrossRef]
- Komatsu, S.; Hasegawa, H.; Shiroko, T.; Sakamoto, E.; Kurumiya, Y.; Norimizu, S.; Tabata, T.; Natsume, S.; Aoba, T. Safety and complications of laparoscopic subtotal cholecystectomy for severe cholecystitis. Jpn. J. Gastroenterol. Surg. 2008, 41, 1758–1764. (In Japanese) [Google Scholar] [CrossRef]
- Cakmak, A.; Genç, V.; Orozakunov, E.; Kepenekçi, I.; Cetinkaya, O.A.; Hazinedaroğlu, M.S. Partial cholecystectomy is a safe and efficient method. Chirurgia 2009, 104, 701–704. [Google Scholar] [PubMed]
- Tian, Y.; Wu, S.D.; Su, Y.; Kong, J.; Yu, K.; Fan, Y. Laparoscopic subtotal cholecystectomy as an alternative procedure designed to prevent bile duct injury: Experience of a hospital in Northern China. Surg. Today 2009, 39, 510–513. [Google Scholar] [CrossRef] [PubMed]
- Singhal, T.; Balakrishnan, S.; Hussain, A.; Nicholls, J.; Grandy-Smith, S.; El-Hasani, S. Laparoscopic subtotal cholecystectomy: Initial experience with laparoscopic management of difficult cholecystitis. Surgeon 2009, 7, 63–68. [Google Scholar] [CrossRef] [PubMed]
- Nakajima, J.; Sasaki, A.; Obuchi, T.; Baba, S.; Nitta, H.; Wakabayashi, G. Laparoscopic subtotal cholecystectomy for severe cholecystitis. Surg. Today 2009, 39, 870–875. [Google Scholar] [CrossRef]
- Di Carlo, I.; Pulvirenti, E.; Toro, A.; Corsale, G. Modified subtotal cholecystectomy: Results of a laparotomy procedure during the laparoscopic era. World J. Surg. 2009, 33, 520–525. [Google Scholar] [CrossRef]
- Sharp, C.F.; Garza, Z.R.; Mangram, A.J.; Dunn, E.L. Partial cholecystectomy in the setting of severe inflammation is an acceptable consideration with few long-term sequelae. Am. Surg. 2009, 75, 249–252. [Google Scholar] [CrossRef]
- Ukhanov, A.P.; Chakhmachev, S.R.; Ignatev, A.I.; Bolshakov, S.V.; Uvertkin, R.I.; Frumkin, B.B.; Yashina, A.S. Using laparoscopic cholecystectomy in treatment of destructive forms of acute cholecystitis. Vestn. Khirurgii Im. II Grek. 2010, 169, 15–19. (In Russian) [Google Scholar]
- Hubert, C.; Annet, L.; van Beers, B.E.; Gigot, J.F. The “inside approach of the gallbladder” is an alternative to the classic Calot’s triangle dissection for a safe operation in severe cholecystitis. Surg. Endosc. 2010, 24, 2626–2632. [Google Scholar] [CrossRef]
- Lica, I.; Lica, M.; Kinn, D.; Negoi, I.; Paun, S.; Beuran, M. Laparoscopic approach for difficult cholecystectomies. In Proceedings of the 12th European Congress on Trauma and Emergency Surgery ESTES, Milan, Italy, 27–30 April 2011; pp. 87–90. [Google Scholar]
- Jeong, I.O.; Kim, J.Y.; Choe, Y.M.; Choi, S.K.; Heo, Y.S.; Lee, K.Y.; Kim, S.J.; Cho, Y.U.; Ahn, S.I.; Hong, K.C.; et al. Efficacy and feasibility of laparoscopic subtotal cholecystectomy for acute cholecystitis. Korean J. Hepatobiliary Pancreat. Surg. 2011, 15, 225–230. [Google Scholar] [CrossRef]
- Tsukada, T.; Nakano, T.; Miyata, T.; Sasaki, S.; Ohta, T. Cholecystomucoclasis: Revaluation of safety and validity in aged populations. BMC Gastroenterol. 2012, 12, 113. [Google Scholar] [CrossRef]
- Memon, M.R.; Bozdar, A.G.; Mirani, S.H.; Arshad, S.; Shah, S.Q.A. Laparoscopic subtotal cholecystectomy without cystic duct clipping. Med. Channel 2012, 19, 103–106. [Google Scholar]
- Davis, B.; Castaneda, G.; Lopez, J. Subtotal cholecystectomy versus total cholecystectomy in complicated cholecystitis. Am. Surg. 2012, 78, 814–817. [Google Scholar] [CrossRef]
- Al-aubaidi, T.I.; Abid–AlKadhim, A.A.; Sbahi, K.R. Laparoscopic subtotal cholecystectomy in patients with acute cholecystitis. J. Fac. Med. Baghdad 2013, 55, 302–307. [Google Scholar]
- Lee, W. Experience with partial cholecystectomy in severe cholecystitis. Korean J. Hepatobiliary Pancreat. Surg. 2013, 17, 171–175. [Google Scholar] [CrossRef]
- Ghani, A.; Ahmed, W.; Baqai, F.U. Partial cholecystectomy: Indications and outcomes. J. Dow Uni. Health. Sci. 2013, 7, 107–111. [Google Scholar]
- Tamura, A.; Ishii, J.; Katagiri, T.; Maeda, T.; Kubota, Y.; Kaneko, H. Effectiveness of laparoscopic subtotal cholecystectomy: Perioperative and long-term postoperative results. Hepatogastroenterology 2013, 60, 1280–1283. [Google Scholar] [CrossRef]
- Kuwabara, J.; Watanabe, Y.; Kameoka, K.; Horiuchi, A.; Sato, K.; Yukumi, S.; Yoshida, M.; Yamamoto, Y.; Sugishita, H. Usefulness of laparoscopic subtotal cholecystectomy with operative cholangiography for severe cholecystitis. Surg. Today 2014, 44, 462–465. [Google Scholar] [CrossRef]
- Kaplan, D.; Inaba, K.; Chouliaras, K.; Low, G.M.; Benjamin, E.; Lam, L.; Grabo, D.; Demetriades, D. Subtotal cholecystectomy and open total cholecystectomy: Alternatives in complicated cholecystitis. Am. Surg. 2014, 80, 953–955. [Google Scholar] [CrossRef]
- Gode, D.; Palanivelu, C.; Syed, Z.Q. New variants of laparoscopic subtotal cholecystectomy in management of acute cholecystitis. Int. J. Med. Sci. Public Health 2014, 3, 397–400. [Google Scholar] [CrossRef]
- Mishra, A.; Mohanty, S.; Sahoo, S.; Behera, C.; Pal, A. Evaluation of usefulness of a subtotal cholecystectomy in cholecystitis. MedPulse Int. Med. J. 2015, 2, 342–345. [Google Scholar]
- Ebied, E.F.; Ebied, H. Subtotal cholecystectomy in difficult laparoscopic cholecystectomies: Is it safe? Egypt J. Surg. 2015, 34, 90–93. [Google Scholar] [CrossRef]
- Ali, L.; Bashir, T.; Bashir, S. Laparoscopic subtotal cholecystectomy in difficult cholecystitis—Our Experience. Pakistan J. Med. Health Sci. 2015, 9, 917–919. [Google Scholar]
- Yoon, P.D.; Pang, T.; Siriwardhane, M.; Richardson, A.; Hollands, M.; Pleass, H.; Johnston, E.; Yuen, L.; Lam, V. Laparoscopic partial cholecystectomy: A way of getting out of trouble. Int. J. Hepatobiliary Pancreat. Dis. 2016, 6, 68–75. [Google Scholar] [CrossRef]
- Shin, M.; Choi, N.; Yoo, Y.; Kim, Y.; Kim, S.; Mun, S. Clinical outcomes of subtotal cholecystectomy performed for difficult cholecystectomy. Ann. Surg. Treat. Res. 2016, 91, 226–232. [Google Scholar] [CrossRef]
- Kulen, F.; Tihan, D.; Duman, U.; Bayam, E.; Zaim, G. Laparoscopic partial cholecystectomy: A safe and effective alternative surgical technique in “difficult cholecystectomies”. Ulus Cerrahi Derg. 2016, 32, 185–190. [Google Scholar] [CrossRef]
- Dhannur, P.K.; Prasad, K.; Prasad, G. Laparoscopic subtotal cholecystectomy for complicated gall bladder surgeries: Experience at our setup. Int. J. Med. Res. Health Sci. 2016, 5, 13–16. [Google Scholar]
- Dissanaike, S. A step-by-step guide to laparoscopic subtotal fenestrating cholecystectomy: A damage control approach to the difficult gallbladder. J. Am. Coll. Surg. 2016, 223, e15–e18. [Google Scholar] [CrossRef]
- Harilingam, M.R.; Shrestha, A.K.; Basu, S. Laparoscopic modified subtotal cholecystectomy for difficult gall bladders: A single-centre experience. J. Minim. Access. Surg. 2016, 12, 325–329. [Google Scholar] [CrossRef]
- Shingu, Y.; Komatsu, S.; Norimizu, S.; Taguchi, Y.; Sakamoto, E. Laparoscopic subtotal cholecystectomy for severe cholecystitis. Surg. Endosc. 2016, 30, 526–531. [Google Scholar] [CrossRef]
- Jara, G.; Rosciano, J.; Barrios, W.; Vegas, L.; Rodríguez, O.; Sánchez, R.; Sánchez, A. Colecistectomía laparoscópica subtotal como alternativa quirúrgica segura en casos complejos. Cir. Esp. 2017, 95, 465–470. [Google Scholar] [CrossRef]
- Butt, I. Subtotal laparoscopic cholecystectomy: Our experience of 32 patients. Biomedica 2017, 33, 25–28. [Google Scholar]
- Abdelrahim, W.E.; Elsiddig, K.E.; Wahab, A.A.; Saad, M.; Saeed, H.; Khalil, E.A.G. Subtotal laparoscopic cholecystectomy influences the rate of conversion in patients with difficult laparoscopic cholecystectomy: Case series. Ann. Med. Surg. 2017, 19, 19–22. [Google Scholar] [CrossRef]
- Supit, C.; Supit, T.; Mazni, Y.; Basir, I. The outcomes of laparoscopic subtotal cholecystectomy in difficult cases—A case series. Int. J. Surg. Case Rep. 2017, 41, 311–314. [Google Scholar] [CrossRef]
- Al Matrafi, M.S. Subtotal cholecystectomy for the treatment of difficult gall bladder. EC Gastroenterol. Digest. Sys. 2017, 3, 56–61. [Google Scholar]
- Özçınar, B.; Memişoğlu, E.; Gök, A.F.K.; Ağcaoğlu, O.; Yanar, F.; İlhan, M.; Yanar, H.T.; Günay, K. Damage-control laparoscopic partial cholecystectomy with an endoscopic linear stapler. Turk. J. Surg. 2017, 33, 37–39. [Google Scholar] [CrossRef]
- Lidsky, M.E.; Speicher, P.J.; Ezekian, B.; Holt, E.W.; Nussbaum, D.P.; Castleberry, A.W.; Perez, A.; Pappas, T.N. Subtotal cholecystectomy for the hospital gallbladder: Failure to control the cystic duct results in significant morbidity. HPB 2017, 19, 547–556. [Google Scholar] [CrossRef]
- Hirajima, S.; Koh, T.; Sakai, T.; Imamura, T.; Kato, S.; Nishimura, Y.; Soga, K.; Nishio, M.; Oguro, A.; Nakagawa, N. Utility of laparoscopic subtotal cholecystectomy with or without cystic duct ligation for severe cholecystitis. Am. Surg. 2017, 83, 1209–1213. [Google Scholar] [CrossRef]
- Van Dijk, A.H.; Donkervoort, S.C.; Lameris, W.; de Vries, E.; Eijsbouts, Q.A.J.; Vrouenraets, B.C.; Busch, O.R.; Boermeester, M.A.; de Reuver, P.R. Short- and long-term outcomes after a reconstituting and fenestrating subtotal cholecystectomy. J. Am. Coll. Surg. 2017, 225, 371–379. [Google Scholar] [CrossRef]
- Peker, K.D.; Halil, A. Laparoscopic subtotal cholecystectomy could be an alternative to conversion. Med. J. Bakırköy 2017, 13, 113–117. [Google Scholar] [CrossRef]
- Abdallah, H.S. Laparoscopic subtotal cholecystectomy for difficult acute calculous cholecystitis. J. Surg. 2017, 5, 111–117. [Google Scholar] [CrossRef]
- Kirkwood, R.; Damon, L.; Wang, J.; Hong, E.; Kirkwood, K. Gangrenous cholecystitis: Innovative laparoscopic techniques to facilitate subtotal fenestrating cholecystectomy when a critical view of safety cannot be achieved. Surg. Endosc. 2017, 31, 5258–5266. [Google Scholar] [CrossRef] [PubMed]
- Matsumura, T.; Komatsu, S.; Komaya, K.; Ando, K.; Arikawa, T.; Ishiguro, S.; Saito, T.; Osawa, T.; Kurahashi, S.; Uchino, T.; et al. Closure of the cystic duct orifice in laparoscopic subtotal cholecystectomy for severe cholecystitis. Asian J. Endosc. Surg. 2018, 11, 206–211. [Google Scholar] [CrossRef]
- Shanker, M.C.R.S.; Shanker, K. Clinical outcome of stump closure techniques after subtotal cholecystectomy-our experience. J. Evol. Med. Dent. Sci. 2018, 7, 5232–5235. [Google Scholar]
- Gupta, V.; Karwal, V.; Singla, S.K.; Gupta, M. Clinical outcome of laparoscopic subtotal cholecystectomy in the treatment of complicated cholecystitis. J. Evol. Med. Dent. Sci. 2018, 7, 2534–2538. [Google Scholar] [CrossRef]
- Sormaz, İ.C.; Soytaş, Y.; Gök, A.F.K.; Özgür, İ.; Avtan, L. Fundus-first technique and partial cholecystectomy for difficult laparoscopic cholecystectomies. Ulus Travma Acil Cerrahi Derg. 2018, 24, 66–70. [Google Scholar] [CrossRef]
- Matsui, Y.; Hirooka, S.; Kotsuka, M.; Yamaki, S.; Yamamoto, T.; Kosaka, H.; Satoi, S. Use of a piece of free omentum to prevent bile leakage after subtotal cholecystectomy. Surgery 2018, 164, 419–423. [Google Scholar] [CrossRef]
- Sagiroglu, J.; Ozdemir, T.; Gapbarov, A.; Duman, E.; Kır, G.; Sermet, M.; Ekinci, O.; Alimoglu, O. Subtotal cholecystectomy for “difficult gallbladder”: Pearls and pitfalls. Chirurgia 2019, 32, 294–299. [Google Scholar] [CrossRef]
- Khan, H.M.; Manjunath, B.G.; Shenoy, V.G. Laparoscopic subtotal cholecystectomy: A safe approach in difficult cholecystectomy. Int. Surg. J. 2019, 6, 1767–1771. [Google Scholar] [CrossRef]
- Purzner, R.H.; Ho, K.B.; Al-Sukhni, E.; Jayaraman, S. Safe laparoscopic subtotal cholecystectomy in the face of severe inflammation in the cystohepatic triangle: A retrospective review and proposed management strategy for the difficult gallbladder. Can. J. Surg. 2019, 62, 402–411. [Google Scholar] [CrossRef]
- Roesch-Dietlen, F.; Pérez-Morales, A.G.; Martínez-Fernández, S.; Díaz-Roesch, F.; Gómez-Delgado, J.A.; Remes-Troche, J.M. Safety of laparoscopic subtotal cholecystectomy in acute cholecystitis. Experience in Southeast Mexico. Rev. Gastroenterol. Mex. 2019, 84, 461–466. [Google Scholar] [CrossRef]
- Kohga, A.; Suzuki, K.; Okumura, T.; Yamashita, K.; Isogaki, J.; Kawabe, A.; Kimura, T. Calculus left in remnant gallbladder cause long-term complications in patients undergoing subtotal cholecystectomy. HPB 2019, 21, 508–514. [Google Scholar] [CrossRef]
- Bairoliya, K.; Rajan, R.; Sindhu, R.S.; Natesh, B.; Mathew, J.; Raviram, S. Is a difficult gallbladder worth removing in its entirety?—Outcomes of subtotal cholecystectomy. J. Minim. Access Surg. 2020, 16, 323–327. [Google Scholar] [CrossRef]
- Kohn, J.F.; Trenk, A.; Denham, W.; Linn, J.G.; Haggerty, S.; Joehl, R.; Ujiki, M.B. Long-term outcomes after subtotal reconstituting cholecystectomy: A retrospective case series. Am. J. Surg. 2020, 220, 736–740. [Google Scholar] [CrossRef]
- Narasimhappa, R.; Thota, A. Laparoscopic subtotal cholecystectomy—A safe approach in difficult cholecystectomy. J. Evid. Based Med. Healthc. 2020, 7, 684–688. [Google Scholar] [CrossRef]
- Kuroki, T.; Kitasano, A.; Yamashita, M.; Noda, K.; Imai, R.; Kugiyama, T.; Hirayama, T.; Kobayashi, S.; Tokunaga, T.; Yamanouchi, K.; et al. Results of laparoscopic subtotal cholecystectomy by laparoscopic linear stapler in difficult cases with severe cholecystitis. Acta Med. Nagasaki 2020, 63, 55–59. [Google Scholar] [CrossRef]
- Waikar, K.V. Omentum piece for prevention of bile leakage after subtotal cholecystectomy. Int. J. Med. Biomed. Stud. 2020, 4, 95–98. [Google Scholar] [CrossRef]
- Tay, W.M.; Toh, Y.J.; Shelat, V.G.; Huey, C.W.; Junnarkar, S.P.; Woon, W.; Low, J.K. Subtotal cholecystectomy: Early and long-term outcomes. Surg. Endosc. 2020, 34, 4536–4542. [Google Scholar] [CrossRef]
- Porter, D.J.; Walter, A.; Lucocq, J.; Patil, P.; Alijani, A. Sub-total cholecystectomy—An audit of clinical practice in a tertiary referral hospital. World J. Surg. Surgical. Res. 2020, 3, 1190. [Google Scholar]
- Elhardello, O.; Miu, V.; Liu, C. Laparoscopic subtotal cholecystectomy is a safe rescue procedure: A DGH Experience. World J. Surg. Surgical. Res. 2020, 3, 1186. [Google Scholar]
- Shwaartz, C.; Pery, R.; Cordoba, M.; Gutman, M.; Rosin, D. Laparoscopic subtotal cholecystectomy for the difficult gallbladder: A safe alternative. Isr. Med. Assoc. J. 2020, 22, 538–541. [Google Scholar]
- Singh, S.K.; Shukla, D.; Singh, P.K.; Katyayan, I. Laparoscopic subtotal cholecystectomy a boon to difficult gall bladder. Int. Surg. J. 2021, 8, 215–219. [Google Scholar] [CrossRef]
- LeCompte, M.T.; Robbins, K.J.; Williams, G.A.; Sanford, D.E.; Hammill, C.W.; Fields, R.C.; Hawkins, W.G.; Strasberg, S.M. Less is more in the difficult gallbladder: Recent evolution of subtotal cholecystectomy in a single HPB unit. Surg. Endosc. 2021, 35, 3249–3257. [Google Scholar] [CrossRef] [PubMed]
- Ibrahim, R.; Abdalkoddus, M.; Mahendran, B.; Mownah, O.A.; Nawara, H.; Aroori, S. Subtotal cholecystectomy: Is it a safe option for difficult gallbladders? Ann. R. Coll. Surg. Engl. 2021. [Google Scholar] [CrossRef]
- Acar, N.; Acar, T.; Sür, Y.; Bağ, H.; Kar, H.; Yılmaz Bozok, Y.; Dilek, O.N. Is subtotal cholecystectomy safe and feasible? Short- and long-term results. J. Hepatobiliary Pancreat. Sci. 2021, 28, 263–271. [Google Scholar] [CrossRef] [PubMed]
- Slater, M.; Midya, S.; Booth, M. Re-interventions and re-admissions in a 13-year series following use of laparoscopic subtotal cholecystectomy. J. Minim. Access Surg. 2021, 17, 28–31. [Google Scholar] [CrossRef]
- Ie, M.; Katsura, M.; Kanda, Y.; Kato, T.; Sunagawa, K.; Mototake, H. Laparoscopic subtotal cholecystectomy after percutaneous transhepatic gallbladder drainage for grade II or III acute cholecystitis. BMC Surg. 2021, 21, 386. [Google Scholar] [CrossRef]
- Shimoda, M.; Udo, R.; Imasato, R.; Oshiro, Y.; Suzuki, S. What are the risk factors of conversion from total cholecystectomy to bailout surgery? Surg. Endosc. 2021, 35, 2206–2210. [Google Scholar] [CrossRef]
- Chávez-Villa, M.; Dominguez-Rosado, I.; Figueroa-Méndez, R.; De Los Santos-Pérez, A.; Mercado, M.A. Subtotal cholecystectomy after failed critical view of safety is an effective and safe bail out strategy. J. Gastrointest. Surg. 2021, 25, 2553–2561. [Google Scholar] [CrossRef]
- Toro, A.; Teodoro, M.; Khan, M.; Schembari, E.; Di Saverio, S.; Catena, F.; Di Carlo, I. Subtotal cholecystectomy for difficult acute cholecystitis: How to finalize safely by laparoscopy—A systematic review. World J. Emerg. Surg. 2021, 16, 45. [Google Scholar] [CrossRef]
- Tang, A.; Cohan, C.M.; Beattie, G.; Mooney, C.M.; Chiang, A.; Keeley, J.A. Factors that predict the need for subtotal cholecystectomy. Am. Surg. 2021, 87, 1245–1251. [Google Scholar] [CrossRef]
- Kohga, A.; Suzuki, K.; Okumura, T.; Yamashita, K.; Isogaki, J.; Kawabe, A.; Kimura, T. Does preoperative MRCP imaging predict risk for conversion to subtotal cholecystectomy in patients with acute cholecystitis? Surg. Endosc. 2021, 35, 6717–6723. [Google Scholar] [CrossRef]
- Srinivasa, S.; Hammill, C.W.; Strasberg, S.M. How to do laparoscopic subtotal fenestrating cholecystectomy. ANZ J. Surg. 2021, 91, 740–741. [Google Scholar] [CrossRef]
- Lunevicius, R.; Haagsma, J.A. Subtotal cholecystectomy: Results of a single-center, registry-based retrospective cohort study of 180 adults in 2011-2018. J. Laparoendosc. Adv. Surg. Tech. A 2021, 31, 1019–1033. [Google Scholar] [CrossRef]
- Mesri, M.; Nzenwa, I.C.; Lunevicius, R. Evaluating the patient and setting-specific factors that influenced the quality of informed consent in a retrospective cohort of subtotal cholecystectomy Patients. J. Laparoendosc. Adv. Surg. Tech. A 2021, 31, 77–84. [Google Scholar] [CrossRef]
- Loh, A.Y.H.; Chean, C.S.; Durkin, D.; Bhatt, A.; Athwal, T.S. Short and long term outcomes of laparoscopic fenestrating or reconstituting subtotal cholecystectomy versus laparoscopic total cholecystectomy in the management of acute cholecystitis. HPB 2022, 24, 691–699. [Google Scholar] [CrossRef]
- Byskosh, A.; Stocker, B.; Liu, D.Y.; Li, J.; Gastevich, B.; Devin, C.L.; Quach, G.; Weiss, H.; Posluszny, J. Subtotal fenestrating cholecystectomy: A safe and effective approach to the difficult gallbladder. J. Surg. Res. 2023, 282, 191–197. [Google Scholar] [CrossRef]
- Lucocq, J.; Hamilton, D.; Scollay, J.; Patil, P. Subtotal cholecystectomy results in high peri-operative morbidity and its risk-profile should be emphasised during consent. World J. Surg. 2022, 46, 2955–2962. [Google Scholar] [CrossRef]
- Braschi, C.; Tung, C.; Tang, A.; Delgado, C.; Uribe, L.; Senekjian, L.; Keeley, J.A. Early outcomes of subtotal vs total cholecystectomy for acute cholecystitis. JAMA Surg. 2022, 157, 1062–1064. [Google Scholar] [CrossRef]
- Deng, S.X.; Greene, B.; Tsang, M.E.; Jayaraman, S. Thinking your way through a difficult laparoscopic cholecystectomy: Technique for high-quality subtotal cholecystectomy. J. Am. Coll. Surg. 2022, 235, e8–e16. [Google Scholar] [CrossRef]
- Abe, T.; Oshita, A.; Fujikuni, N.; Hattori, M.; Kobayashi, T.; Hanada, K.; Noriyuki, T.; Ohdan, H.; Nakahara, M. Efficacy of bailout surgery for preventing intraoperative biliary injury in acute cholecystitis. Surg. Endosc. 2022. [Google Scholar] [CrossRef]
- Saavedra, G.C.; Segovia, D.R.; Centeno, R.H.; Pérez, N.J.F. Laparoscopic subtotal reconstituting cholecystectomy in type II & III Mirizzi syndrome: Case series of 5 patients. Int. J. Surg. Case Rep. 2022, 97, 107425. [Google Scholar] [CrossRef] [PubMed]
- Jenner, D.C.; Klimovskij, M.; Nicholls, M.; Bates, T. Occlusion of the cystic duct with cyanoacrylate glue at laparoscopic subtotal fenestrating cholecystectomy for a difficult gallbladder. Acta Chir. Belg. 2022, 122, 23–28. [Google Scholar] [CrossRef] [PubMed]
- Boyd, K.; Bradley, N.A.; Cannings, E.; Shearer, C.; Wadhawan, H.; Wilson, M.S.J.; Crumley, A. Laparoscopic subtotal cholecystectomy; change in practice over a 10-year period. HPB 2022, 24, 759–763. [Google Scholar] [CrossRef] [PubMed]
- Cremer, K.; Kloppenberg, F.W.H.; Vanhommerig, J.W.; Dijksman, L.M.; Bode, N.; Donkervoort, S.C. The effect of surgical strategy in difficult cholecystectomy cases on postoperative complications outcome: A value-based healthcare comparative study. Surg. Endosc. 2022, 36, 5293–5302. [Google Scholar] [CrossRef]
- Yoshida, M.C.; Ogami, T.; Ho, K.; Bui, E.X.; Khedr, S.; Chen, C.C. Patient and surgeon factors contributing to bailout cholecystectomies: A single-institutional retrospective analysis. Surg. Endosc. 2022, 36, 6696–6704. [Google Scholar] [CrossRef]
- Kurtulus, I.; Culcu, O.D.; Degerli, M.S. Which is more effective: Laparoscopic or open partial cholecystectomy? J. Laparoendosc. Adv. Surg. Tech. A 2022, 32, 476–484. [Google Scholar] [CrossRef]
- Tomihara, H.; Tomimaru, Y.; Hashimoto, K.; Fukuchi, N.; Yokoyama, S.; Mori, T.; Tanemura, M.; Sakai, K.; Takeda, Y.; Tsujie, M.; et al. Preoperative risk score to predict subtotal cholecystectomy after gallbladder drainage for acute cholecystitis: Secondary analysis of data from a multi-institutional retrospective study (CSGO-HBP-017B). Asian J. Endosc. Surg. 2022, 15, 555–562. [Google Scholar] [CrossRef]
- Yildirim, A.C., 4th; Zeren, S.; Ekici, M.F.; Yaylak, F.; Algin, M.C.; Arik, O. Comparison of fenestrating and reconstituting subtotal cholecystectomy techniques in difficult cholecystectomy. Cureus 2022, 14, e22441. [Google Scholar] [CrossRef]
- Kayapinar, A.K.; Sahin, H. Laparoscopic modified subtotal cholecystectomy is a safe method in the management of Mirizzi syndrome type I. Ann. Med. Res. 2022, 29, 604–609. [Google Scholar] [CrossRef]
- Worawanthanachai, T. Comparison between laparoscopic subtotal cholecystectomy and open conversion in difficult laparoscopic cholecystectomy. Thai J. Surg. 2022, 43, 78–85. [Google Scholar]
- Nada, H.; Sinha, A.; White, A.; Widlund, H.; Refalo, A.; Ebied, H. Predictive factors for subtotal cholecystectomy in delayed elective cholecystectomy after the acute presentation. Int. Surg. J. 2022, 10, 1–5. [Google Scholar] [CrossRef]
- Recent Literature: Introduction to the differential diagnosis of the separate forms of gallstone disease. By prof. Hans Kehr, Halberstadt. Authorised translation by William Watkins Seymour, M. D. (Yale), M.D. (Harvard), Surgeon to the Samaritan Hospital, Troy, N. Y., etc. pp. 370. Philadelphia: P. Blakiston’s Son & Co. 1901. Boston Med. Surg. J. 1901, 145, 285.
- Lahey, F.H. Strictures of the common and hepatic ducts. Ann. Surg. 1937, 105, 765–790. [Google Scholar] [CrossRef]
- Beye, H.L. Conditions necessitating surgery following cholecystectomy surgery. Gynecol. Obstet. 1936, 62, 191–202. [Google Scholar]
- Henneman, D.; da Costa, D.W.; Vrouenraets, B.C.; van Wagensveld, B.A.; Lagarde, S.M. Laparoscopic partial cholecystectomy for the difficult gallbladder: A systematic review. Surg. Endosc. 2013, 27, 315–358. [Google Scholar] [CrossRef]
- Strasberg, S.M.; Pucci, M.J.; Brunt, L.M.; Deziel, D.J. Subtotal cholecystectomy–‘fenestrating’ vs. ‘reconstituting’ subtypes and the prevention of bile duct injury: Definition of the optimal procedure in difficult operative conditions. J. Am. Coll. Surg. 2016, 222, 89–96. [Google Scholar] [CrossRef]
- Takada, T.; Kawarada, Y.; Nimura, Y.; Yoshida, M.; Mayumi, T.; Sekimoto, M.; Miura, F.; Wada, K.; Hirota, M.; Yamashita, Y.; et al. Background: Tokyo Guidelines for the management of acute cholangitis and cholecystitis. J. Hepatobiliary Pancreat. Surg. 2007, 14, 1–10. [Google Scholar] [CrossRef]
- Mayumi, T.; Takada, T.; Kawarada, Y.; Nimura, Y.; Yoshida, M.; Sekimoto, M.; Miura, F.; Wada, K.; Hirota, M.; Yamashita, Y.; et al. Results of the Tokyo Consensus Meeting Tokyo Guidelines. J. Hepatobiliary Pancreat. Surg. 2007, 14, 114–121. [Google Scholar] [CrossRef]
- Yamashita, Y.; Takada, T.; Kawarada, Y.; Nimura, Y.; Hirota, M.; Miura, F.; Mayumi, T.; Yoshida, M.; Strasberg, S.; Pitt, H.A.; et al. Surgical treatment of patients with acute cholecystitis: Tokyo Guidelines. J. Hepatobiliary Pancreat. Surg. 2007, 14, 91–97. [Google Scholar] [CrossRef]
- Okamoto, K.; Suzuki, K.; Takada, T.; Strasberg, S.M.; Asbun, H.J.; Endo, I.; Iwashita, Y.; Hibi, T.; Pitt, H.A.; Umezawa, A.; et al. Tokyo Guidelines 2018: Flowchart for the management of acute cholecystitis. J. Hepatobiliary Pancreat. Sci. 2018, 25, 55–72, Erratum in J. Hepatobiliary Pancreat. Sci. 2019, 26, 534. [Google Scholar] [CrossRef]
- Wakabayashi, G.; Iwashita, Y.; Hibi, T.; Takada, T.; Strasberg, S.M.; Asbun, H.J.; Endo, I.; Umezawa, A.; Asai, K.; Suzuki, K.; et al. Tokyo Guidelines 2018: Surgical management of acute cholecystitis: Safe steps in laparoscopic cholecystectomy for acute cholecystitis (with videos). J. Hepatobiliary Pancreat. Sci. 2018, 25, 73–86. [Google Scholar] [CrossRef] [PubMed]
- Iwashita, Y.; Hibi, T.; Ohyama, T.; Umezawa, A.; Takada, T.; Strasberg, S.M.; Asbun, H.J.; Pitt, H.A.; Han, H.S.; Hwang, T.L.; et al. Delphi consensus on bile duct injuries during laparoscopic cholecystectomy: An evolutionary cul-de-sac or the birth pangs of a new technical framework? J. Hepatobiliary Pancreat. Sci. 2017, 24, 591–602. [Google Scholar] [CrossRef] [PubMed]
- Lunevicius, R. Laparoscopic subtotal cholecystectomy: A classification, which encompasses the variants, technical modalities, and extent of resection of the gallbladder. Ann. R. Coll. Surg. Engl. 2020, 102, 315–317. [Google Scholar] [CrossRef] [PubMed]
- Mannino, M.; Toro, A.; Teodoro, M.; Di Carlo, I. Subtotal cholecystectomies during acute cholecystitis. An overview on different techniques. Surg. Gastroenterol. Oncol. 2018, 23, 405–407. [Google Scholar] [CrossRef]
- Lee, J.; Miller, P.; Kermani, R.; Dao, H.; O’Donnell, K. Gallbladder damage control: Compromised procedure for compromised patients. Surg. Endosc. 2012, 26, 2779–2783. [Google Scholar] [CrossRef]
- NHS Digital. Classifications browser OPCS—4.9. Available online: https://classbrowser.nhs.uk/#/book/OPCS-4.9 (accessed on 17 December 2022).
- Brunt, L.M.; Deziel, D.J.; Telem, D.A.; Strasberg, S.M.; Aggarwal, R.; Asbun, H.; Bonjer, J.; McDonald, M.; Alseidi, A.; Ujiki, M.; et al. Safe cholecystectomy multi-society practice guideline and state of the art consensus conference on prevention of bile duct injury during cholecystectomy. Ann. Surg. 2020, 272, 3–23. [Google Scholar] [CrossRef]
- Koo, J.G.A.; Chan, Y.H.; Shelat, V.G. Laparoscopic subtotal cholecystectomy: Comparison of reconstituting and fenestrating techniques. Surg. Endosc. 2021, 35, 1014–1024. [Google Scholar] [CrossRef]
- Eri, L.M.; Liavåg, I. Subtotal kolecystektomi. Et alternativ ved vanskelig kolecystektomi [Subtotal cholecystectomy. An alternative to a difficult cholecystectomy]. Tidsskr Nor Laegeforen 1987, 107, 467–468. (In Norwegian) [Google Scholar]

| Year | Author | Cases | Term | Resected Walls | Closure | Completion | |||
|---|---|---|---|---|---|---|---|---|---|
| Peritoneal | Hepatic | CD | Remnant | Open | Closed | ||||
| 1898 | Kehr [11] | 2 | None | + | + | − | + | − | + |
| 1899 | Mayo [12] | 3 | None | + | + | − | + | − | + |
| 1899 | Mayo [12] | 3 | None | NA | NA | − | + | − | + |
| 1901 | Stevens [13] | 1 | None | + | + | − | + | − | + |
| 1920 | Bengolea [17] * | NA | PC | NA | NA | − | − | − | − |
| 1923 | De Martel [17] * | 2 | None | + | − | + | − | − | + |
| 1924 | Zabala [17] * | 5 | PC | + | − | − | − | + | − |
| 1924 | Pauchet [17] * | NA | PC | + | − | − | − | + | − |
| 1926 | Martin [14] | 8 | None | + | − | − | − | + | − |
| 1927 | Gatch [17] * | NA | PC | + | − | − | − | + | − |
| 1927 | Zimmerman [17] * | NA | PC | + | − | − | − | + | − |
| 1930 | Haggard [17] * | NA | PC | + | − | − | + | − | + |
| 1931 | Estes [15] | 7 | PC | + | − | − | − | + | − |
| 1933 | Judd [21] | 149 | PC | + | − | − | − | + | − |
| 1935 | McKenty [17] * | NA | PC | + | − | + | − | − | + |
| 1936 | Thorek [18] | 201 | ESC | + | − | + | − | − | + |
| 1937 | Ritchie [23] | 16 | None | + | − | − | + | − | + |
| 1938 | McKenty [22] | 30 | PC | + | − | − | − | + | − |
| 1938 | Estes [16] | 48 | PC | + | − | − | − | + | − |
| 1938 | Thorek [19] | 342 | ESC | + | − | + | − | − | + |
| 1939 | Bailey [26] | 129 | ESC | + | − | + | − | − | + |
| 1940 | Gurd [27] | 6 | PC | + | − | − | − | + | − |
| 1947 | Morse [28] | 2 | STC | + | − | − | − | + | − |
| 1947 | Love [29] | 129 | ESC | + | − | + | − | − | + |
| 1950 | Lerner [30] | 2 | PC | + | − | − | − | + | − |
| 1953 | Meyer [36] ** | 28 | STC | + | − | − | − | + | − |
| 1954 | Thorek [20] | NA | ESC | + | − | + | − | − | + |
| 1954 | McElmoyle [31] | 23 | C | + | + | − | − | + | − |
| 1955 | Madding [35] | 4 | STC | + | + | − | + | − | + |
| 1959 | Farrow [37] | 24 | STC | + | − | − | − | + | − |
| 1985 | Bornman [38] | 18 | STC | + | − | + | − | − | + |
| 1990 | Douglas [39] | 11 | PC | + | − | + | − | − | + |
| 1991 | Schein [41] | 16 | PC | + | − | + | − | − | + |
| 1991 | Cottier [42] | 11 | STC | + | − | + | − | − | + |
| 1992 | Khan [43] | 43 | STC | + | + | − | + | − | + |
| 1993 | Schein [44] | 23 | STC | + | − | + | − | − | + |
| 1993 | Bickel [45] | 6 | STC | + | − | + | + | − | + |
| 1996 | Subramaniasivam [49] | 15 | PC | + | − | + | − | − | + |
| 1996 | Katsohis [50] | 34 | STC | + | − | + | − | − | + |
| 1998 | Ranson [51] | 8 | STC | + | − | + | − | − | + |
Disclaimer/Publisher’s Note: The statements, opinions and data contained in all publications are solely those of the individual author(s) and contributor(s) and not of MDPI and/or the editor(s). MDPI and/or the editor(s) disclaim responsibility for any injury to people or property resulting from any ideas, methods, instructions or products referred to in the content. |
© 2023 by the author. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Lunevicius, R. Review of the Literature on Partial Resections of the Gallbladder, 1898–2022: The Outline of the Conception of Subtotal Cholecystectomy and a Suggestion to Use the Terms ‘Subtotal Open-Tract Cholecystectomy’ and ‘Subtotal Closed-Tract Cholecystectomy’. J. Clin. Med. 2023, 12, 1230. https://doi.org/10.3390/jcm12031230
Lunevicius R. Review of the Literature on Partial Resections of the Gallbladder, 1898–2022: The Outline of the Conception of Subtotal Cholecystectomy and a Suggestion to Use the Terms ‘Subtotal Open-Tract Cholecystectomy’ and ‘Subtotal Closed-Tract Cholecystectomy’. Journal of Clinical Medicine. 2023; 12(3):1230. https://doi.org/10.3390/jcm12031230
Chicago/Turabian StyleLunevicius, Raimundas. 2023. "Review of the Literature on Partial Resections of the Gallbladder, 1898–2022: The Outline of the Conception of Subtotal Cholecystectomy and a Suggestion to Use the Terms ‘Subtotal Open-Tract Cholecystectomy’ and ‘Subtotal Closed-Tract Cholecystectomy’" Journal of Clinical Medicine 12, no. 3: 1230. https://doi.org/10.3390/jcm12031230
APA StyleLunevicius, R. (2023). Review of the Literature on Partial Resections of the Gallbladder, 1898–2022: The Outline of the Conception of Subtotal Cholecystectomy and a Suggestion to Use the Terms ‘Subtotal Open-Tract Cholecystectomy’ and ‘Subtotal Closed-Tract Cholecystectomy’. Journal of Clinical Medicine, 12(3), 1230. https://doi.org/10.3390/jcm12031230






