Two-Years Follow-Up of Symptoms and Return to Work in Complex Post-COVID-19 Patients
Abstract
1. Introduction
2. Population and Methods
2.1. Population and Study Design
2.2. Statistical Analysis
3. Results
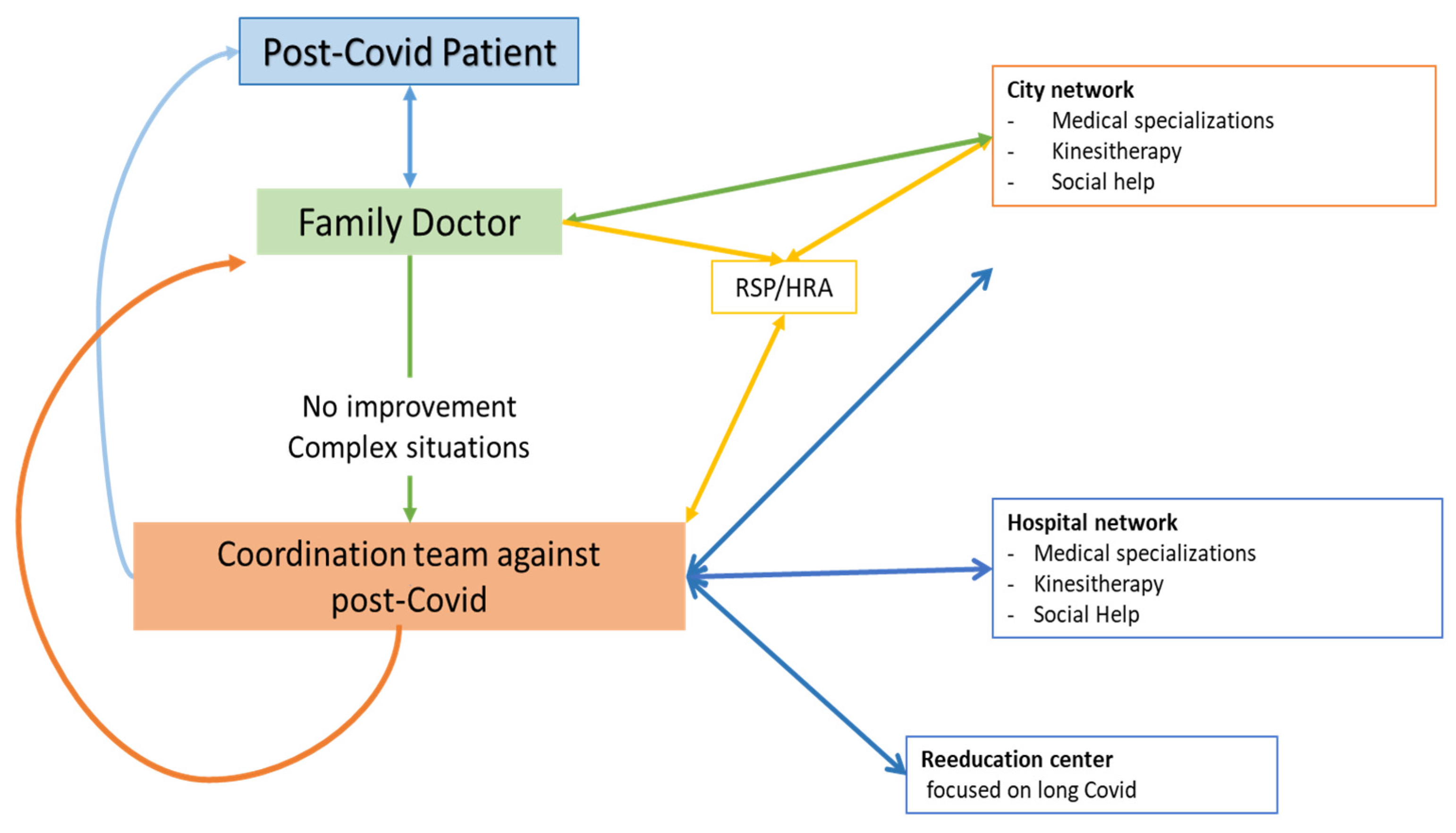
3.1. Flow Chart of the Study
3.2. Means of Contact of the Coordination Team
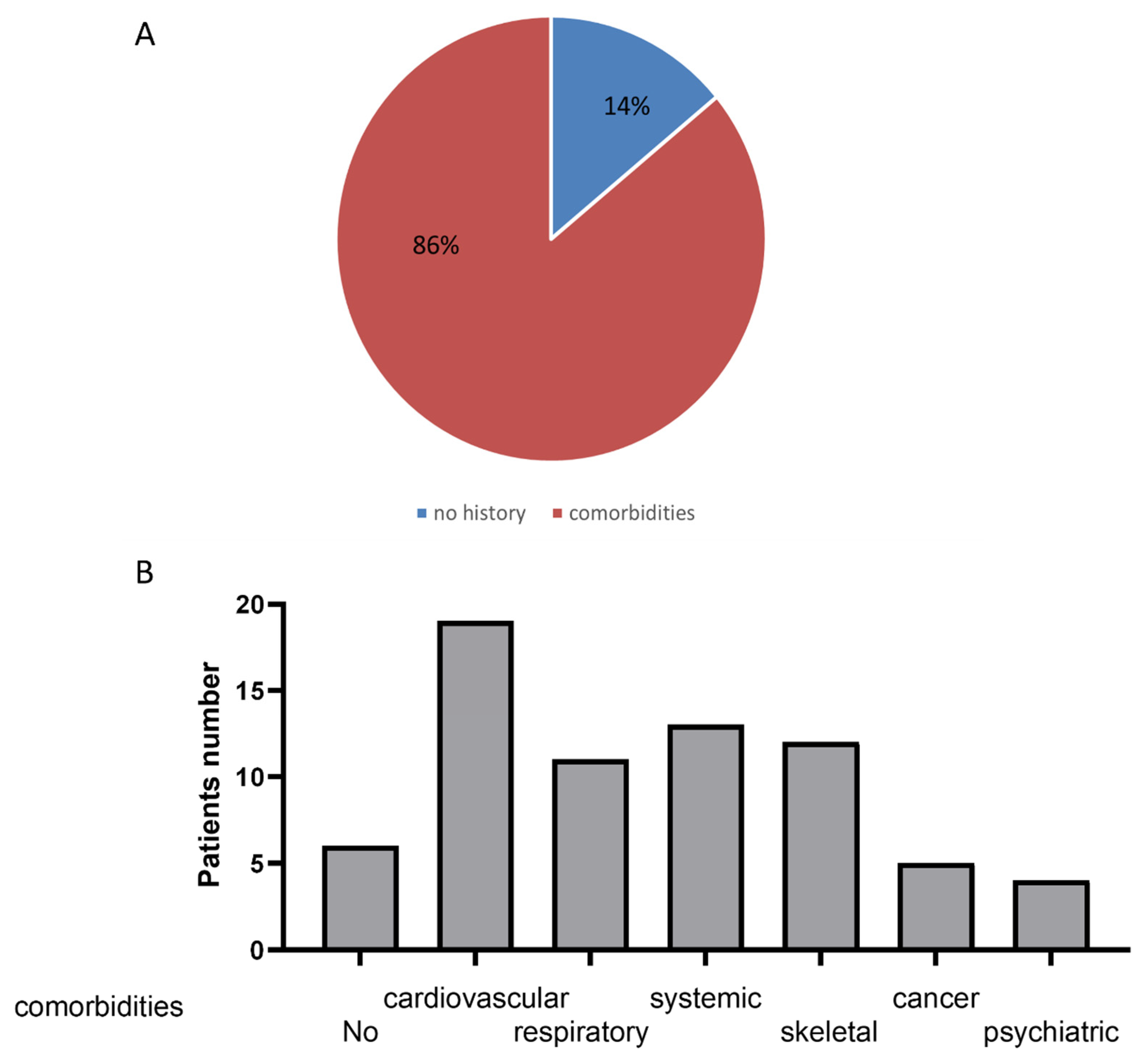
3.3. Population Characteristics
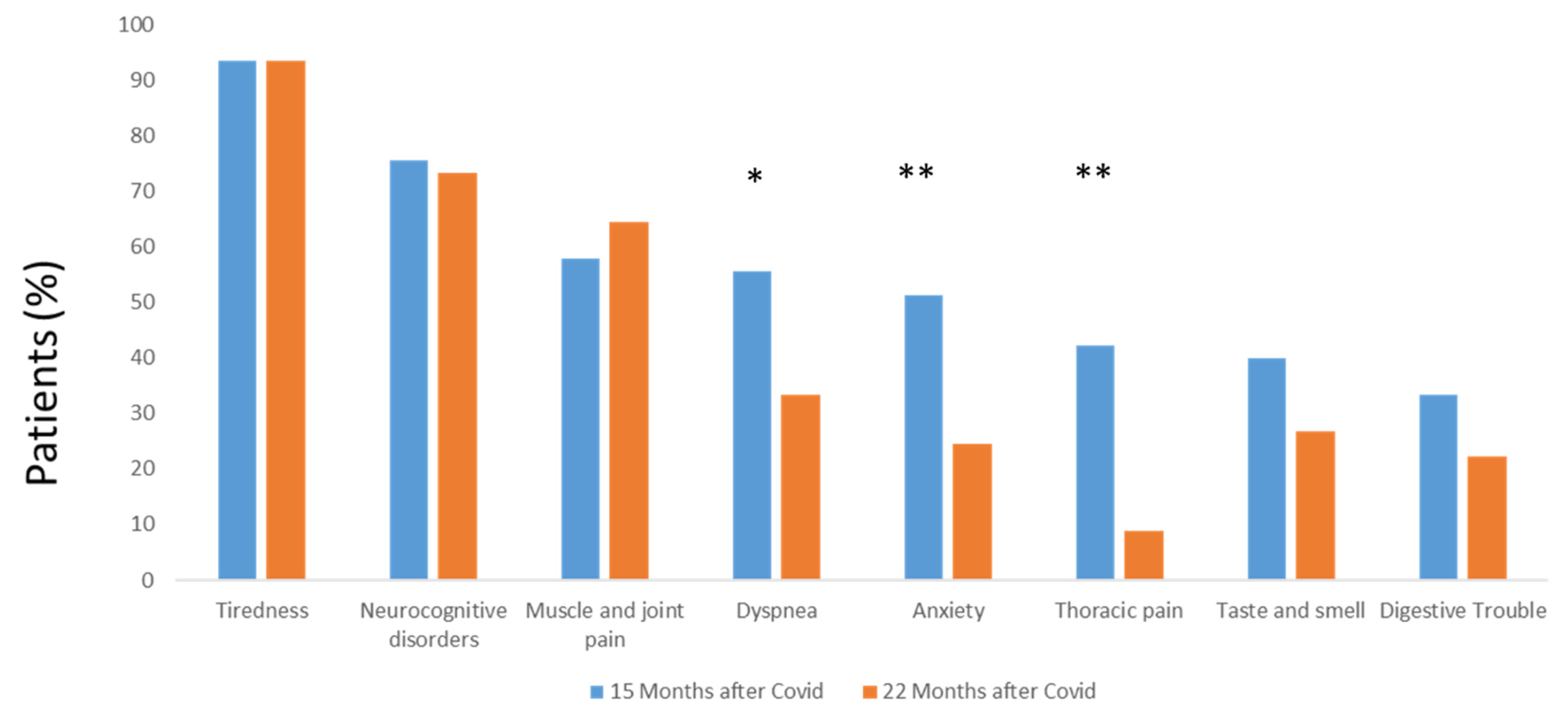
3.4. Post-COVID-19 Symptom Evolution
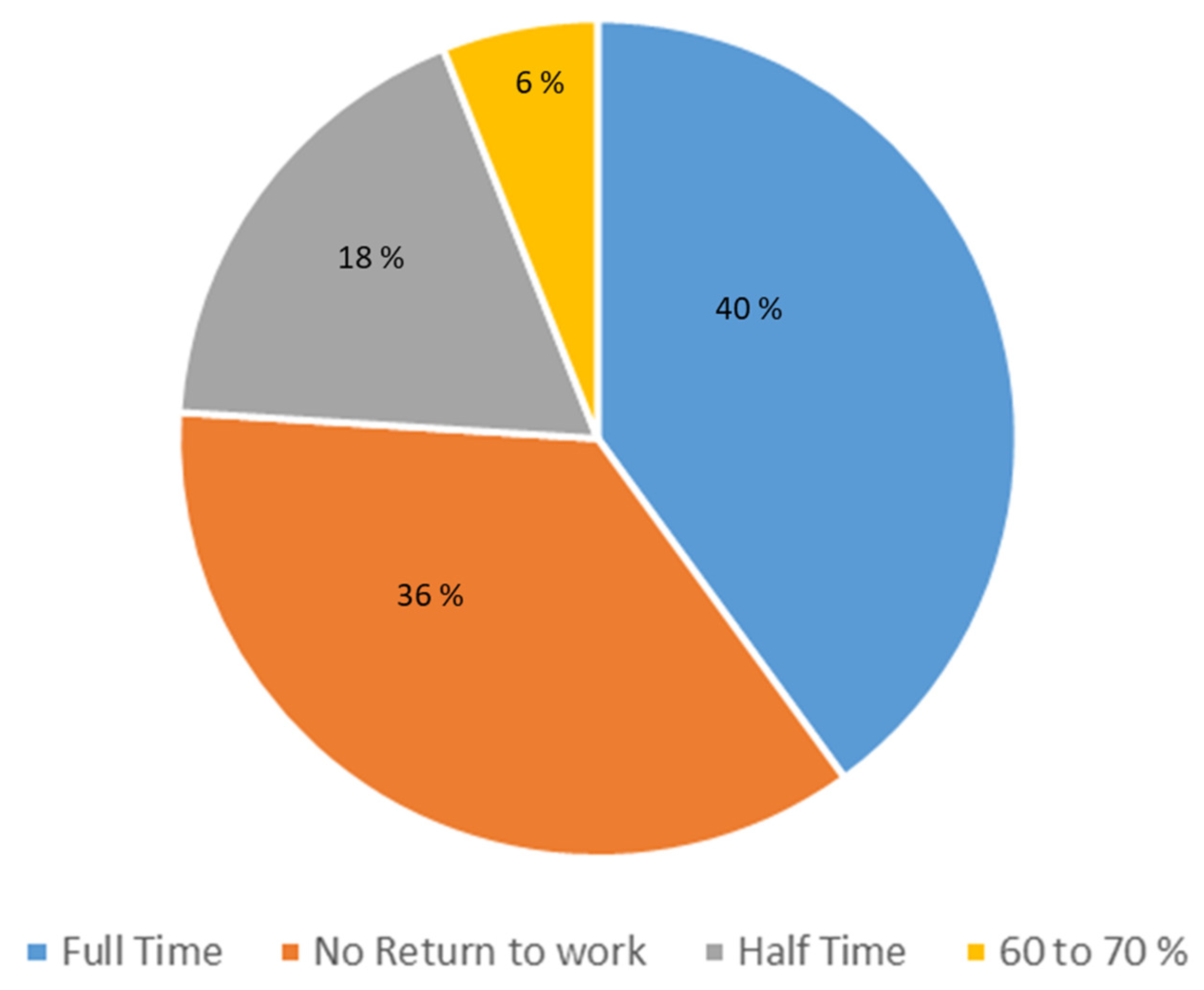
3.5. Patients’ Perceived Improvement and Ability to Return to Work
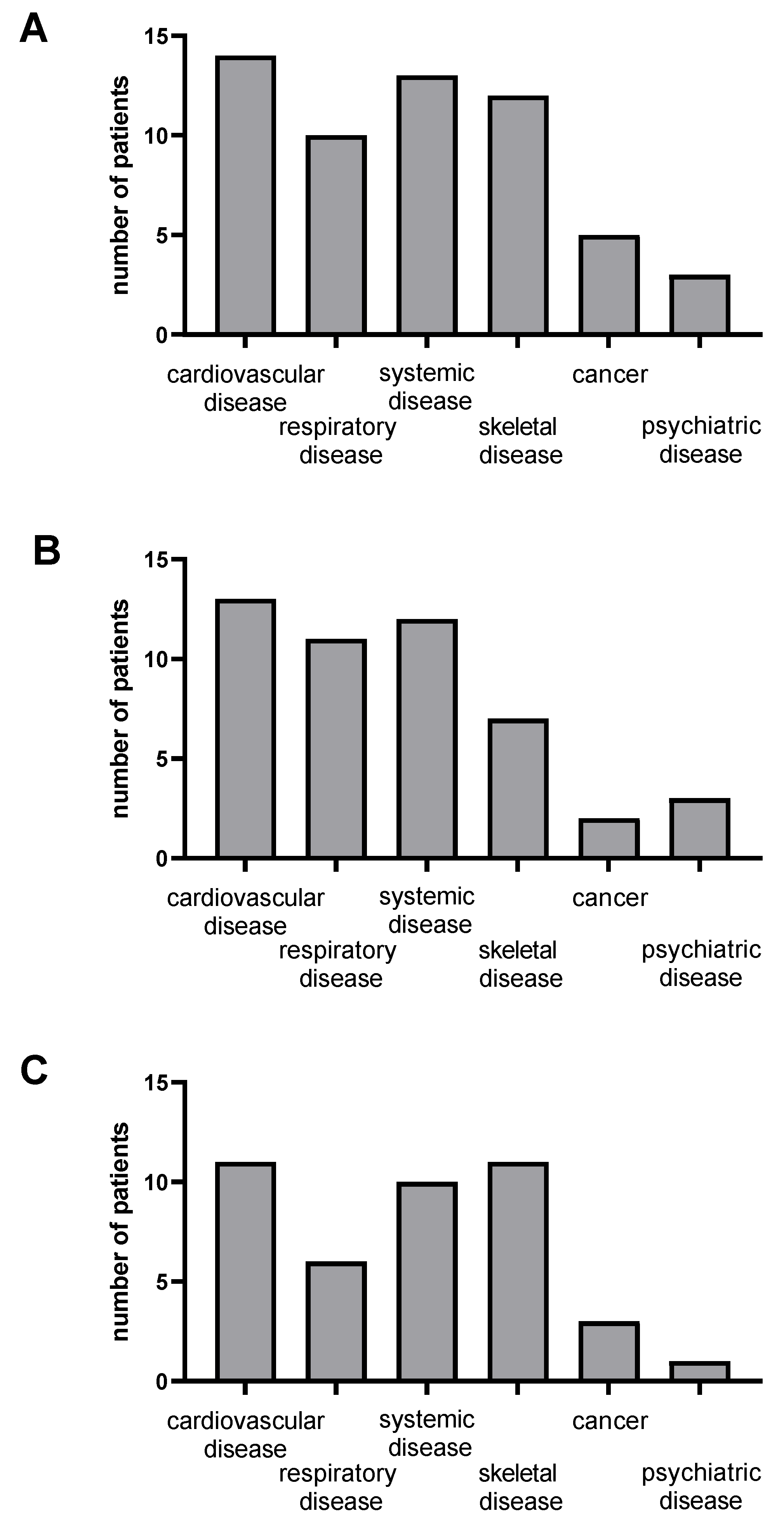
3.6. Potential Links between Patients’ Symptoms, Pre-Existing Pathologies and Back-to-Work Occurrence
4. Discussion
4.1. Post-COVID Patients Addressing and Characteristics
4.2. Therapeutic Proposals and Perceived Efficacy of the Support
4.3. Limitations of the Study
5. Conclusions
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Acknowledgments
Conflicts of Interest
References
- WHO. A Clinical Case Definition of Post COVID-19 Condition by a Delphi Consensus. Available online: https://www.who.int/publications/i/item/WHO-2019-nCoV-Post_COVID-19_condition-Clinical_case_definition-2021.1 (accessed on 15 November 2022).
- Whitaker, M.; Elliott, J.; Chadeau-Hyam, M.; Riley, S.; Darzi, A.; Cooke, G.; Ward, H.; Elliott, P. Persistent COVID-19 symptoms in a community study of 606,434 people in England. Nat. Commun. 2022, 13, 1957. [Google Scholar] [CrossRef] [PubMed]
- Pavli, A.; Theodoridou, M.; Maltezou, H.C. Post-COVID Syndrome: Incidence, Clinical Spectrum, and Challenges for Primary Healthcare Professionals. Arch. Med. Res. 2021, 52, 575–581. [Google Scholar] [CrossRef] [PubMed]
- Tarazona, V.; Kirouchena, D.; Clerc, P.; Pinsard-Laventure, F.; Bourrion, B. Quality of Life in COVID-19 Outpatients: A Long-Term Follow-Up Study. J. Clin. Med. 2022, 11, 6478. [Google Scholar] [CrossRef]
- Grant, M.C.; Geoghegan, L.; Arbyn, M.; Mohammed, Z.; McGuinness, L.; Clarke, E.L.; Wade, R.G. The prevalence of symptoms in 24,410 adults infected by the novel coronavirus (SARS-CoV-2; COVID-19): A systematic review and meta-analysis of 148 studies from 9 countries. PLoS ONE 2020, 15, e0234765. [Google Scholar] [CrossRef]
- Davis, H.E.; Assaf, G.S.; McCorkell, L.; Wei, H.; Low, R.J.; Re’em, Y.; Redfield, S.; Austin, J.P.; Akrami, A. Characterizing long COVID in an international cohort: 7 months of symptoms and their impact. EClinicalMedicine 2021, 38, 101019. [Google Scholar] [CrossRef] [PubMed]
- Nikolic Turnic, T.; Vasiljevic, I.; Stanic, M.; Jakovljevic, B.; Mikerova, M.; Ekkert, N.; Reshetnikov, V.; Jakovljevic, V. Post-COVID-19 Status and Its Physical, Nutritional, Psychological, and Social Effects in Working-Age Adults-A Prospective Questionnaire Study. J. Clin. Med. 2022, 11, 6668. [Google Scholar] [CrossRef] [PubMed]
- Levy, D.; Giannini, M.; Oulehri, W.; Riou, M.; Marcot, C.; Pizzimenti, M.; Debrut, L.; Charloux, A.; Geny, B.; Meyer, A. Long Term Follow-Up of Sarcopenia and Malnutrition after Hospitalization for COVID-19 in Conventional or Intensive Care Units. Nutrients 2022, 14, 912. [Google Scholar] [CrossRef]
- Ghanem, J.; Passadori, A.; Severac, F.; Dieterlen, A.; Geny, B.; Andrès, E. Effects of Rehabilitation on Long-COVID-19 Patient’s Autonomy, Symptoms and Nutritional Observance. Nutrients 2022, 14, 3027. [Google Scholar] [CrossRef]
- Riou, M.; Oulehri, W.; Momas, C.; Rouyer, O.; Lebourg, F.; Meyer, A.; Enache, I.; Pistea, C.; Charloux, A.; Marcot, C.; et al. Reduced Flow-Mediated Dilatation Is Not Related to COVID-19 Severity Three Months after Hospitalization for SARS-CoV-2 Infection. J. Clin. Med. 2021, 10, 1318. [Google Scholar] [CrossRef] [PubMed]
- Rubin, R. As Their Numbers Grow, COVID-19 “Long Haulers” Stump Experts. JAMA 2020, 324, 1381. [Google Scholar] [CrossRef]
- Kingstone, T.; Taylor, A.K.; O’Donnell, C.A.; Atherton, H.; Blane, D.N.; Chew-Graham, C.A. Finding the ‘right’ GP: A qualitative study of the experiences of people with long-COVID. BJGP Open 2020, 4, 1143. [Google Scholar] [CrossRef] [PubMed]
- Fernandez-de-Las-Penas, C.; Martin-Guerrero, J.D.; Pellicer-Valero, O.J.; Navarro-Pardo, E.; Gomez-Mayordomo, V.; Cuadrado, M.L.; Arias-Navalon, J.A.; Cigaran-Mendez, M.; Hernandez-Barrera, V.; Arendt-Nielsen, L. Female Sex Is a Risk Factor Associated with Long-Term Post-COVID Related-Symptoms but Not with COVID-19 Symptoms: The LONG-COVID-EXP-CM Multicenter Study. J. Clin. Med. 2022, 11, 413. [Google Scholar] [CrossRef]
- Zheng, Y.Y.; Ma, Y.T.; Zhang, J.Y.; Xie, X. COVID-19 and the cardiovascular system. Nat. Rev. Cardiol. 2020, 17, 259–260. [Google Scholar] [CrossRef] [PubMed]
- Luers, J.C.; Rokohl, A.C.; Loreck, N.; Wawer Matos, P.A.; Augustin, M.; Dewald, F.; Klein, F.; Lehmann, C.; Heindl, L.M. Olfactory and Gustatory Dysfunction in Coronavirus Disease 2019 (COVID-19). Clin. Infect. Dis. 2020, 71, 2262–2264. [Google Scholar] [CrossRef]
- Taneri, P.E.; Gómez-Ochoa, S.A.; Llanaj, E.; Raguindin, P.F.; Rojas, L.Z.; Roa-Díaz, Z.M.; Salvador, D., Jr.; Groothof, D.; Minder, B.; Kopp-Heim, D.; et al. T. Anemia and iron metabolism in COVID-19: A systematic review and meta-analysis. Eur. J. Epidemiol. 2020, 35, 763–773. [Google Scholar] [CrossRef] [PubMed]
- Fugazzaro, S.; Contri, A.; Esseroukh, O.; Kaleci, S.; Croci, S.; Massari, M.; Facciolongo, N.C.; Besutti, G.; Iori, M.; Salvarani, C.; et al. Rehabilitation Interventions for Post-Acute COVID-19 Syndrome: A Systematic Review. Int. J. Environ. Res. Public Health 2022, 19, 5185. [Google Scholar] [CrossRef]
- Chen, H.; Shi, H.; Liu, X.; Sun, T.; Wu, J.; Liu, Z. Effect of pulmonary rehabilitation for patients with post-COVID-19: A systemic review and meta-analysis. Front. Med. 2022, 9, 837420. [Google Scholar] [CrossRef]
- Zeng, B.; Chen, D.; Qiu, Z.; Zhang, M. Expert consensus on protocol of rehabilitation for COVID-19 patients using framework and approaches of WHO International Family Clasifications. Aging Med. 2020, 3, 82–94. [Google Scholar] [CrossRef]
- Važgėlienė, D.; Kubilius, R.; Bileviciute-Ljungar, I. Do Comorbidities and Daily Medication before SARS-CoV-2 Infection Play a Role in Self-Reported Post-Infection Symptoms? J. Clin. Med. 2022, 11, 6278. [Google Scholar] [CrossRef]
- Townsend, L.; Dyer, A.H.; Jones, K.; Dunne, J.; Mooney, A.; Gaffney, F.; O’Connor, L.; Leavy, D.; O’Brien, K.; Dowds, J.; et al. Persistent fatigue following SARS-CoV-2 infection is common and independent of severity of initial infection. PLoS ONE 2020, 15, e0240784. [Google Scholar] [CrossRef]
- Dellino, M.; Cascardi, E.; Vinciguerra, M.; Lamanna, B.; Malvasi, A.; Scacco, S.; Acquaviva, S.; Pinto, V.; Di Vagno, G.; Cormio, G.; et al. Nutrition as Personalized Medicine against SARS-CoV-2 Infections: Clinical and Oncological Options with a Specific Female Groups Overview. Int. J. Mol. Sci. 2022, 23, 9136. [Google Scholar] [CrossRef] [PubMed]
- Ackermann, M.; Verleden, S.E.; Kuehnel, M.; Haverich, A.; Welte, T.; Laenger, F.; Vanstapel, A.; Werlein, C.; Stark, H.; Tzankov, A.; et al. Pulmonary Vascular Endothelialitis, Thrombosis, and Angiogenesis in COVID-19. N. Engl. J. Med. 2020, 383, 120–128. [Google Scholar] [CrossRef] [PubMed]
- Giannini, M.; Ohana, M.; Nespola, B.; Zanframundo, G.; Geny, B.; Meyer, A. Similarities between COVID-19 and anti-MDA5 syndrome: What can we learn for better care ? Eur. Respir. J. 2020, 56, 2001618. [Google Scholar] [CrossRef] [PubMed]


| Mean ± SD | |||
|---|---|---|---|
| Clinical characteristics | Age, years | 49.6 ± 11.2 | |
| BMI, kg/m2 | 25.8 ± 5.6 | ||
| Number n = 45 | Percentage | ||
| Female | 28 | 62.2% | |
| Male | 17 | 37.8% | |
| Main risk factors | Hypertension | 13 | 28.9% |
| Obesity | 10 | 22.2% | |
| Smoker | 8 | 17.8% | |
| Hyperlipidemia | 4 | 8.9% | |
| Diabetes | 3 | 6.7% | |
Disclaimer/Publisher’s Note: The statements, opinions and data contained in all publications are solely those of the individual author(s) and contributor(s) and not of MDPI and/or the editor(s). MDPI and/or the editor(s) disclaim responsibility for any injury to people or property resulting from any ideas, methods, instructions or products referred to in the content. |
© 2023 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Van Wambeke, E.; Bezler, C.; Kasprowicz, A.-M.; Charles, A.-L.; Andres, E.; Geny, B. Two-Years Follow-Up of Symptoms and Return to Work in Complex Post-COVID-19 Patients. J. Clin. Med. 2023, 12, 741. https://doi.org/10.3390/jcm12030741
Van Wambeke E, Bezler C, Kasprowicz A-M, Charles A-L, Andres E, Geny B. Two-Years Follow-Up of Symptoms and Return to Work in Complex Post-COVID-19 Patients. Journal of Clinical Medicine. 2023; 12(3):741. https://doi.org/10.3390/jcm12030741
Chicago/Turabian StyleVan Wambeke, Erika, Cécile Bezler, Anne-Marie Kasprowicz, Anne-Laure Charles, Emmanuel Andres, and Bernard Geny. 2023. "Two-Years Follow-Up of Symptoms and Return to Work in Complex Post-COVID-19 Patients" Journal of Clinical Medicine 12, no. 3: 741. https://doi.org/10.3390/jcm12030741
APA StyleVan Wambeke, E., Bezler, C., Kasprowicz, A.-M., Charles, A.-L., Andres, E., & Geny, B. (2023). Two-Years Follow-Up of Symptoms and Return to Work in Complex Post-COVID-19 Patients. Journal of Clinical Medicine, 12(3), 741. https://doi.org/10.3390/jcm12030741







