Long-Term Survival of Neuroblastoma Patients Receiving Surgery, Chemotherapy, and Radiotherapy: A Propensity Score Matching Study
Abstract
1. Introduction
2. Materials and Methods
2.1. Data Source
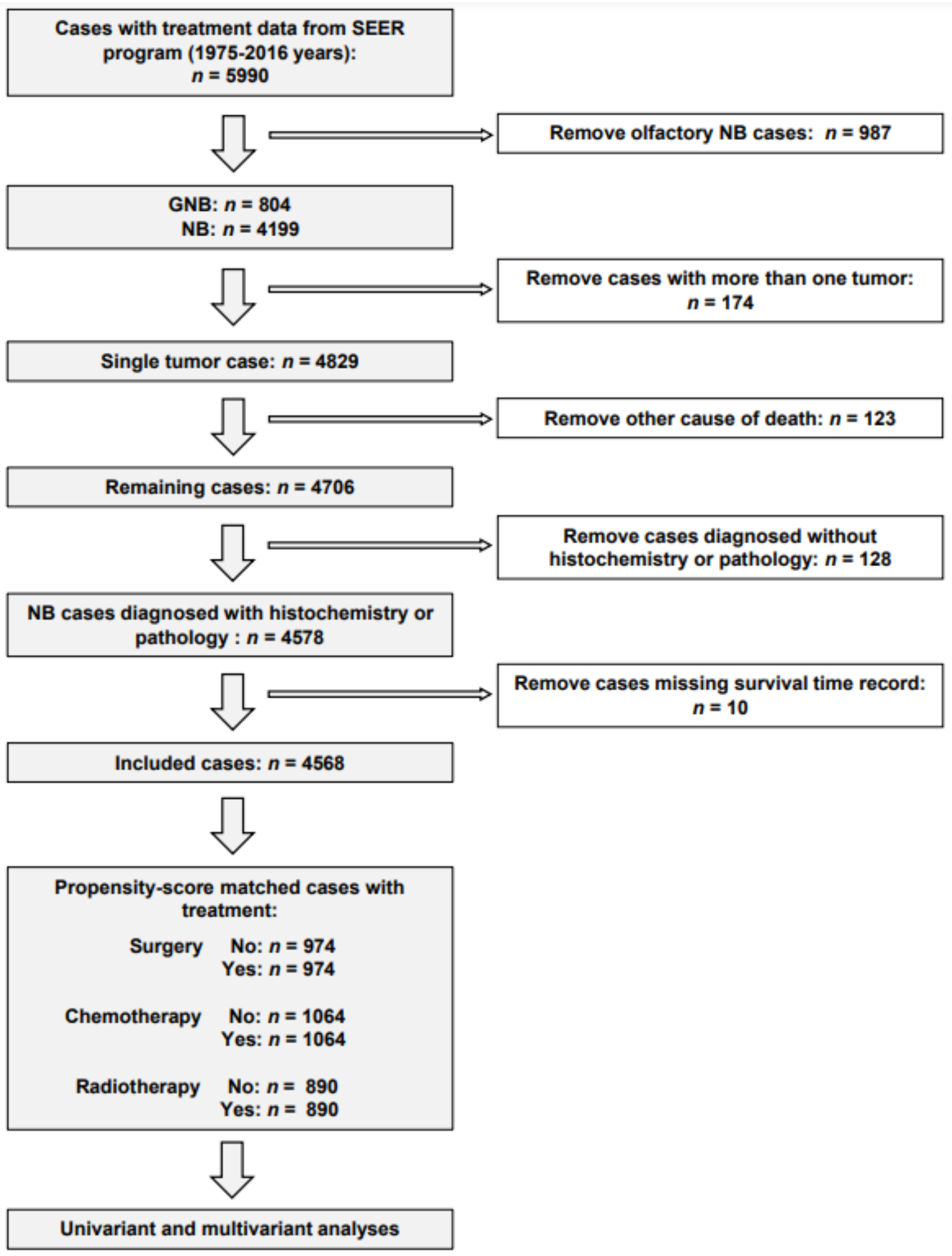
2.2. Patient Cohort
2.3. Survival Outcome and Study Variables
2.4. Propensity Score Matching Analysis
2.5. Statistical Analysis
3. Results
3.1. Characteristics of the Neuroblastoma Patients
3.2. Trends and Effects of Surgery, Chemotherapy, and Radiotherapy
3.3. Impact of Baseline Characteristics and Effects of Combinatorial Therapies on the Long-Term Survival of Neuroblastoma Patients Receiving Surgery
3.4. Trend of the Conventional Treatment Results with the Advancement of Time
4. Discussion
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Acknowledgments
Conflicts of Interest
References
- Qiu, B.; Matthay, K.K. Advancing therapy for neuroblastoma. Nat. Rev. Clin. Oncol. 2022, 198, 515–533. [Google Scholar] [CrossRef] [PubMed]
- Irwin, M.S.; Naranjo, A.; Zhang, F.F.; Cohn, S.L.; London, W.B.; Gastier-Foster, J.M.; Ramirez, N.C.; Pfau, R.; Reshmi, S.; Wagner, E.; et al. Revised Neuroblastoma Risk Classification System: A Report from the Children’s Oncology Group. J. Clin. Oncol. 2021, 3929, 3229–3241. [Google Scholar] [CrossRef] [PubMed]
- Luo, Y.B.; Cui, X.C.; Yang, L.; Zhang, D.; Wang, J.X. Advances in the Surgical Treatment of Neuroblastoma. Chin. Med. J. 2018, 13119, 2332–2337. [Google Scholar] [CrossRef] [PubMed]
- Twist, C.J.; Naranjo, A.; Schmidt, M.L.; Tenney, S.C.; Cohn, S.L.; Meany, H.J.; Mattei, P.; Adkins, E.S.; Shimada, H.; London, W.B.; et al. Defining Risk Factors for Chemotherapeutic Intervention in Infants with Stage 4S Neuroblastoma: A Report from Children’s Oncology Group Study ANBL0531. J. Clin. Oncol. 2019, 372, 115–124. [Google Scholar] [CrossRef]
- Berthold, F.; Spix, C.; Kaatsch, P.; Lampert, F. Incidence, Survival, and Treatment of Localized and Metastatic Neuroblastoma in Germany 1979–2015. Paediatr. Drugs 2017, 196, 577–593. [Google Scholar] [CrossRef] [PubMed]
- Ahmed, G.; Fawzy, M.; Elmenawi, S.; Elzomor, H.; Yosif, Y.; Elkinaai, N.; Refaat, A.; Hegazy, M.; El Shafiey, M. Role of surgery in localized initially unresectable neuroblastoma. J. Pediatr. Urol. 2018, 143, 231–236. [Google Scholar] [CrossRef]
- Varan, A.; Kesik, V.; Senocak, M.E.; Kale, G.; Akyuz, C.; Buyukpamukcu, M. The efficacy of delayed surgery in children with high-risk neuroblastoma. J. Cancer Res. Ther. 2015, 112, 268–271. [Google Scholar]
- Avanzini, S.; Pio, L.; Erminio, G.; Granata, C.; Holmes, K.; Gambart, M.; Buffa, P.; Castel, V.; Valteau Couanet, D.; Garaventa, A.; et al. Image-defined risk factors in unresectable neuroblastoma: SIOPEN study on incidence, chemotherapy-induced variation, and impact on surgical outcomes. Pediatr. Blood Cancer 2017, 64, 6411. [Google Scholar] [CrossRef]
- Desai, A.V.; Applebaum, M.A.; Karrison, T.G.; Oppong, A.; Yuan, C.; Berg, K.R.; MacQuarrie, K.; Sokol, E.; Hall, A.G.; Pinto, N.; et al. Efficacy of post-induction therapy for high-risk neuroblastoma patients with end-induction residual disease. Cancer 2022, 12815, 2967–2977. [Google Scholar] [CrossRef]
- Paraboschi, I.; Privitera, L.; Kramer-Marek, G.; Anderson, J.; Giuliani, S. Novel Treatments and Technologies Applied to the Cure of Neuroblastoma. Children 2021, 8, 86. [Google Scholar] [CrossRef]
- Peinemann, F.; Tushabe, D.A.; van Dalen, E.C.; Berthold, F. Rapid COJEC versus standard induction therapies for high-risk neuroblastoma. Cochrane Database Syst. Rev. 2015, 5, CD010774. [Google Scholar] [CrossRef] [PubMed]
- Morgenstern, D.A.; London, W.B.; Stephens, D.; Volchenboum, S.L.; Hero, B.; Di Cataldo, A.; Nakagawara, A.; Shimada, H.; Ambros, P.F.; Matthay, K.K.; et al. Metastatic neuroblastoma confined to distant lymph nodes (stage 4N) predicts outcome in patients with stage 4 disease: A study from the International Neuroblastoma Risk Group Database. J. Clin. Oncol. 2014, 3212, 1228–1235. [Google Scholar] [CrossRef] [PubMed]
- NCI. Surveillance, Epidemiology and End Result (SEER). 2020. Available online: https://seer.cancer.gov (accessed on 21 April 2020).
- Green, A.L.; Furutani, E.; Ribeiro, K.B.; Rodriguez Galindo, C. Death Within 1 Month of Diagnosis in Childhood Cancer: An Analysis of Risk Factors and Scope of the Problem. J. Clin. Oncol. 2017, 3512, 1320–1327. [Google Scholar] [CrossRef] [PubMed]
- Vo, K.T.; Matthay, K.K.; Neuhaus, J.; London, W.B.; Hero, B.; Ambros, P.F.; Nakagawara, A.; Miniati, D.; Wheeler, K.; Pearson, A.D.; et al. Clinical, biologic, and prognostic differences on the basis of primary tumor site in neuroblastoma: A report from the international neuroblastoma risk group project. J. Clin. Oncol. 2014, 3228, 3169–3176. [Google Scholar] [CrossRef] [PubMed]
- Strother, D.R.; London, W.B.; Schmidt, M.L.; Brodeur, G.M.; Shimada, H.; Thorner, P.; Collins, M.H.; Tagge, E.; Adkins, S.; Reynolds, C.P.; et al. Outcome after surgery alone or with restricted use of chemotherapy for patients with low-risk neuroblastoma: Results of Children’s Oncology Group study P9641. J. Clin. Oncol. 2012, 3015, 1842–1848. [Google Scholar] [CrossRef] [PubMed]
- Ryan, A.L.; Akinkuotu, A.; Pierro, A.; Morgenstern, D.A.; Irwin, M.S. The Role of Surgery in High-risk Neuroblastoma. J. Pediatr. Hematol. Oncol. 2020, 421, 1–7. [Google Scholar] [CrossRef]
- Tolbert, V.P.; Matthay, K.K. Neuroblastoma: Clinical and biological approach to risk stratification and treatment. Cell Tissue Res. 2018, 3722, 195–209. [Google Scholar] [CrossRef]
- Bansal, D.; Totadri, S.; Chinnaswamy, G.; Agarwala, S.; Vora, T.; Arora, B.; Prasad, M.; Kapoor, G.; Radhakrishnan, V.; Laskar, S.; et al. Management of Neuroblastoma: ICMR Consensus Document. Indian J. Pediatr. 2017, 846, 446–455. [Google Scholar] [CrossRef]
- Fischer, J.; Pohl, A.; Volland, R.; Hero, B.; Dübbers, M.; Cernaianu, G.; Berthold, F.; von Schweinitz, D.; Simon, T. Complete surgical resection improves outcome in INRG high-risk patients with localized neuroblastoma older than 18 months. BMC Cancer 2017, 171, 520. [Google Scholar] [CrossRef]
- Pohl, A.; Erichsen, M.; Stehr, M.; Hubertus, J.; Bergmann, F.; Kammer, B.; von Schweinitz, D. Image-defined Risk Factors Correlate with Surgical Radicality and Local Recurrence in Patients with Neuroblastoma. Klin. Padiatr. 2016, 2283, 118–123. [Google Scholar] [CrossRef]
- Yang, X.; Chen, J.; Wang, N.; Liu, Z.; Li, F.; Zhou, J.; Tao, B. Impact of extent of resection on survival in high-risk neuroblastoma: A systematic review and meta-analysis. J. Pediatr. Surg. 2019, 547, 1487–1494. [Google Scholar] [CrossRef] [PubMed]
- Simon, T.; Haberle, B.; Hero, B.; von Schweinitz, D.; Berthold, F. Role of surgery in the treatment of patients with stage 4 neuroblastoma age 18 months or older at diagnosis. J. Clin. Oncol. 2013, 316, 752–758. [Google Scholar] [CrossRef] [PubMed]
- Elzembely, M.M.; Park, J.R.; Riad, K.F.; Sayed, H.A.; Pinto, N.; Carpenter, P.A.; Baker, K.S.; El-Haddad, A. Acute Complications After High-Dose Chemotherapy and Stem-Cell Rescue in Pediatric Patients with High-Risk Neuroblastoma Treated in Countries with Different Resources. J. Glob. Oncol. 2018, 4, 1–12. [Google Scholar] [CrossRef] [PubMed]
- Valteau-Couanet, D.; Schleiermacher, G.; Sarnacki, S.; Pasqualini, C. High-risk neuroblastoma treatment strategy: The experience of the SIOPEN group. Bull. Cancer 2018, 10510, 918–924. [Google Scholar] [CrossRef] [PubMed]
- Davidoff, A.M. Neonatal Neuroblastoma. Clin. Perinatol. 2021, 481, 101–115. [Google Scholar] [CrossRef] [PubMed]
- Twist, C.J.; Schmidt, M.L.; Naranjo, A.; London, W.B.; Tenney, S.C.; Marachelian, A.; Shimada, H.; Collins, M.H.; Esiashvili, N.; Adkins, E.S.; et al. Maintaining Outstanding Outcomes Using Response- and Biology-Based Therapy for Intermediate-Risk Neuroblastoma: A Report from the Children’s Oncology Group Study ANBL0531. J. Clin. Oncol. 2019, 3734, 3243–3255. [Google Scholar] [CrossRef] [PubMed]
- Ferris, M.J.; Tian, S.; Switchenko, J.M.; Madden, N.A.; Eaton, B.R.; Esiashvili, N. Musculoskeletal outcomes and the effect of radiation to the vertebral bodies on growth trajectories for long-term survivors of high-risk neuroblastoma. J. Radiat. Oncol. 2018, 72, 187–193. [Google Scholar] [CrossRef] [PubMed]
- Wei, Z.; Li, J.; Jin, Y.; Liu, Y.; Wang, P.; Cao, Y.; Zhao, Q. The application and value of radiotherapy at the primary site in patients with high-risk neuroblastoma. Br. J. Radiol. 2022, 951134, 20211086. [Google Scholar] [CrossRef]
- Casey, D.L.; Kushner, B.H.; Cheung, N.K.; Modak, S.; LaQuaglia, M.P.; Wolden, S.L. Local Control with 21-Gy Radiation Therapy for High-Risk Neuroblastoma. Int. J. Radiat. Oncol. Biol. Phys. 2016, 962, 393–400. [Google Scholar] [CrossRef]
- Van Heerden, J.; Hendricks, M.; Geel, J.; Sartorius, B.; Hadley, G.P.; Du Plessis, J.; Buchner, A.; Naidu, G.; Van Emmenes, B.; Van Zyl, A.; et al. Overall survival for neuroblastoma in South Africa between 2000 and 2014. Pediatr. Blood Cancer 2019, 6611, e27944. [Google Scholar] [CrossRef]
- Bates, J.E.; Howell, R.M.; Liu, Q.; Yasui, Y.; Mulrooney, D.A.; Dhakal, S.; Smith, S.A.; Leisenring, W.M.; Indelicato, D.J.; Gibson, T.M.; et al. Therapy-Related Cardiac Risk in Childhood Cancer Survivors: An Analysis of the Childhood Cancer Survivor Study. J. Clin. Oncol. 2019, 3713, 1090–1101. [Google Scholar] [CrossRef] [PubMed]
- Zhao, Q.; Liu, Y.; Zhang, Y.; Meng, L.; Wei, J.; Wang, B.; Wang, H.; Xin, Y.; Dong, L.; Jiang, X. Role and toxicity of radiation therapy in neuroblastoma patients: A literature review. Crit. Rev. Oncol. Hematol. 2020, 149, 102924. [Google Scholar] [CrossRef] [PubMed]
- Anderson, J.; Majzner, R.G.; Sondel, P.M. Immunotherapy of Neuroblastoma: Facts and Hopes. Clin. Cancer Res. 2022, 2815, 3196–3206. [Google Scholar] [CrossRef] [PubMed]
- Yu, A.L.; Gilman, A.L.; Ozkaynak, M.F.; London, W.B.; Kreissman, S.G.; Chen, H.X.; Smith, M.; Anderson, B.; Villablanca, J.G.; Matthay, K.K.; et al. Anti-GD2 antibody with GM-CSF, interleukin-2, and isotretinoin for neuroblastoma. N. Engl. J. Med. 2010, 36314, 1324–1334. [Google Scholar] [CrossRef] [PubMed]
- Wienke, J.; Dierselhuis, M.P.; Tytgat, G.A.M.; Kunkele, A.; Nierkens, S.; Molenaar, J.J. The immune landscape of neuroblastoma: Challenges and opportunities for novel therapeutic strategies in pediatric oncology. Eur. J. Cancer 2021, 144, 123–150. [Google Scholar] [CrossRef]
- Richards, R.M.; Sotillo, E.; Majzner, R.G. CAR T Cell Therapy for Neuroblastoma. Front. Immunol. 2018, 9, 2380. [Google Scholar] [CrossRef]
- Matthay, K.K.; Maris, J.M.; Schleiermacher, G.; Nakagawara, A.; Mackall, C.L.; Diller, L.; Weiss, W.A. Neuroblastoma. Nat. Rev. Dis. Prim. 2016, 2, 16078. [Google Scholar] [CrossRef]
- Yu, E.Y.; Cheung, N.V.; Lue, N.F. Connecting telomere maintenance and regulation to the developmental origin and differentiation states of neuroblastoma tumor cells. J. Hematol. Oncol. 2022, 151, 117. [Google Scholar] [CrossRef]
- Pathania, A.S.; Prathipati, P.; Murakonda, S.P.; Murakonda, A.B.; Srivastava, A.; Avadhesh; Byrareddy, S.N.; Coulter, D.W.; Gupta, S.C.; Challagundla, K.B. Immune checkpoint molecules in neuroblastoma: A clinical perspective. Semin. Cancer Biol. 2022, 86, 247–258. [Google Scholar] [CrossRef]



| Unmatched | Matched | Unmatched | Matched | Unmatched | Matched | |||||||||||||
|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|
| SG (n = 1147) | Non-SG (n = 3363) | P | SG (n = 1147) | Non-SG (n = 3363) | p | CT (n = 2966) | Non-CT (n = 1602) | p | CT (n = 1064) | Non-CT (n = 1064) | p | RT (n = 1169) | Non-RT(n = 3354) | p | RT (n = 890) | Non-RT (n = 890) | p | |
| Gender | 0.328 | 0.158 | 0.039 | 0.516 | 0.087 | 0.924 | ||||||||||||
| Female (%) | 48.1 | 46.4 | 43.8 | 47.0 | 46.5 | 49.7 | 49.7 | 51.1 | 45.3 | 48.2 | 43.6 | 43.4 | ||||||
| male (%) | 51.9 | 53.6 | 56.2 | 53.0 | 53.5 | 50.3 | 50.3 | 48.9 | 54.7 | 51.8 | 56.4 | 56.6 | ||||||
| Grade | <0.001 | 0.063 | <0.001 | 0.485 | 0.545 | 0.682 | ||||||||||||
| I: well differentiated (%) | 3.3 | 1.2 | 0.8 | 1.3 | 54.2 | 62.5 | 59.0 | 60.2 | 1.4 | 3.3 | 1.3 | 1.3 | ||||||
| II: moderately differentiated (%) | 1.4 | 0.3 | 0.7 | 0.4 | 1.8 | 4.5 | 2.5 | 2.3 | 1.2 | 1.1 | 0.8 | 0.7 | ||||||
| III: poorly differentiated (%) | 31.8 | 23.7 | 29.0 | 26.0 | 0.6 | 2.1 | 0.8 | 0.9 | 27.3 | 30.1 | 26.9 | 28.1 | ||||||
| IV: undifferentiated (%) | 10.0 | 8.7 | 10.2 | 8.9 | 31.9 | 24.9 | 30 | 29.9 | 12.1 | 8.5 | 11.6 | 10.0 | ||||||
| Unknown (%) | 53.6 | 66.0 | 59.3 | 63.3 | 11.4 | 6.1 | 7.6 | 6.6 | 58.0 | 56.9 | 59.4 | 59.9 | ||||||
| Surgery | — | — | <0.001 | 0.532 | <0.001 | 0.692 | ||||||||||||
| No (%) | 0 | 100 | 0 | 100 | 32.1 | 12.1 | 17.5 | 16.4 | 20.9 | 26.6 | 23.1 | 24.4 | ||||||
| Yes (%) | 100 | 0 | 100 | 100 | 66.5 | 86.9 | 81.8 | 82.2 | 76.7 | 72.5 | 74.9 | 74.8 | ||||||
| Radiotherapy | <0.001 | 0.149 | <0.001 | 0.556 | — | — | ||||||||||||
| No (%) | 72.3 | 77.9 | 80.8 | 77.2 | 63.8 | 91.3 | 90.4 | 89.7 | 0 | 100 | 0 | 100 | ||||||
| Yes (%) | 26.7 | 21.3 | 19.2 | 21.7 | 34.9 | 8.4 | 9.2 | 10.3 | 100 | 0 | 100 | 100 | ||||||
| Chemotherapy | <0.001 | 0.864 | — | — | <0.001 | 0.258 | ||||||||||||
| No (%) | 41.4 | 16.9 | 19.7 | 19.4 | 0 | 100 | 0 | 100 | 11.5 | 43.6 | 13.8 | 12.0 | ||||||
| Yes (%) | 58.6 | 83.1 | 80.3 | 80.6 | 100 | 0 | 100 | 100 | 88.5 | 56.4 | 86.2 | 88.8 | ||||||
| Race | <0.001 | <0.001 | 0.002 | 0.600 | 0.022 | 0.510 | ||||||||||||
| White (%) | 78.8 | 76.5 | 73.6 | 80.0 | 77.0 | 81.0 | 82.2 | 81.6 | 75.5 | 79.3 | 79.3 | 80.6 | ||||||
| Black (%) | 12.7 | 13.3 | 13.1 | 11.4 | 13.6 | 11.1 | 10.8 | 10.0 | 16.3 | 11.6 | 13.0 | 12.4 | ||||||
| Others (%) | 8.5 | 10.2 | 13.2 | 8.6 | 9.4 | 7.9 | 7.0 | 8.5 | 8.1 | 9.1 | 7.6 | |||||||
| Age of diagnosis | <0.001 | 0.819 | <0.001 | 0.602 | <0.001 | 0.466 | ||||||||||||
| <1 (%) | 30.6 | 36.7 | 38.5 | 38.4 | 27.8 | 39.9 | 42.2 | 42.7 | 13.9 | 38.6 | 16.4 | 16.1 | ||||||
| 1–3 (%) | 43.2 | 41.2 | 40.3 | 41.5 | 47.8 | 33.3 | 37.0 | 37.9 | 50.3 | 40.1 | 53.6 | 55.6 | ||||||
| 4–6 (%) | 13.2 | 10.2 | 10.6 | 9.8 | 13.7 | 10.3 | 9.9 | 9.6 | 16.9 | 10.8 | 14.3 | 15.2 | ||||||
| 7–14 (%) | 7.7 | 5.6 | 4.7 | 5.5 | 6.5 | 8.4 | 5.0 | 4.9 | 8.8 | 6.5 | 7.8 | 7.4 | ||||||
| 15–18 (%) | 1.2 | 1.7 | 1.4 | 0.8 | 1.2 | 1.5 | 1.2 | 0.6 | 2.2 | 1.0 | 1.8 | 1.1 | ||||||
| >18 (%) | 4.1 | 4.6 | 4.4 | 4.0 | 3.0 | 6.7 | 4.7 | 4.4 | 7.8 | 3.0 | 6.2 | 4.6 | ||||||
| Year of Diagnosis | <0.001 | 0.873 | 0.001 | 0.622 | <0.001 | 0.884 | ||||||||||||
| 1975–1984 (%) | 14.8 | 9.2 | 11.3 | 11.7 | 9.6 | 14.5 | 11.2 | 12.4 | 19.3 | 8.5 | 16.7 | 16.0 | ||||||
| 1985–1994 (%) | 17.4 | 12.6 | 15.6 | 15.5 | 13.8 | 14.0 | 14.0 | 14.0 | 11.3 | 14.8 | 12.2 | 12.7 | ||||||
| 1995–2004 (%) | 24.0 | 26.9 | 26.4 | 26.3 | 26.5 | 24.7 | 26.0 | 25.3 | 22.2 | 27.1 | 22.8 | 24.2 | ||||||
| 2005–2016 (%) | 43.7 | 51.4 | 46.7 | 46.5 | 50.1 | 46.8 | 48.8 | 48.3 | 47.1 | 49.5 | 28.2 | 47.2 | ||||||
| Primary site | 0.047 | 0.101 | <0.001 | 0.805 | <0.001 | 0.124 | ||||||||||||
| Adrenal (%) | 43.4 | 39.9 | 44.8 | 41.8 | 49.2 | 29.4 | 33.7 | 35.1 | 51.4 | 39.0 | 51.2 | 53.9 | ||||||
| Retroperitoneum (%) | 11.8 | 12.3 | 11.8 | 10.8 | 12.6 | 11.1 | 13.2 | 11.7 | 10.4 | 12.8 | 9.1 | 10.8 | ||||||
| Others (%) | 44.8 | 47.8 | 43.4 | 47.8 | 38.2 | 59.5 | 53.1 | 53.2 | 38.2 | 48.2 | 39.7 | 35.3 | ||||||
| Patients | ||
|---|---|---|
| Characteristics | Number | % |
| Overall | 4568 | 100 |
| Age at diagnosis (years) | ||
| <1 | 1464 | 32.0 |
| 1–3 | 1951 | 42.7 |
| 4–6 | 570 | 12.5 |
| 7–14 | 327 | 7.2 |
| 15–18 | 60 | 1.3 |
| >18 | 196 | 4.3 |
| Gender | ||
| Female | 2175 | 47.6 |
| Male | 2393 | 52.4 |
| Race | ||
| Black | 582 | 12.7 |
| White | 3581 | 78.4 |
| Others | 405 | 8.9 |
| Year of diagnosis | ||
| 1975–1984 | 519 | 11.3 |
| 1985–1994 | 634 | 13.9 |
| 1995–2004 | 1181 | 25.9 |
| 2005–2016 | 2234 | 48.9 |
| Primary site | ||
| Adrenal gland | 1931 | 42.3 |
| Retroperitoneum | 552 | 12.1 |
| Others | 2085 | 45.6 |
| Grade | ||
| I: well differentiated | 126 | 2.8 |
| II: moderately differentiated | 52 | 1.1 |
| III: poorly differentiated | 1344 | 29.4 |
| IV: undifferentiated | 436 | 9.5 |
| Unknown | 2610 | 57.1 |
| Surgery | ||
| No | 1147 | 25.1 |
| Yes | 3363 | 73.6 |
| Unknown | 58 | 1.3 |
| Chemotherapy | ||
| No | 1602 | 35.1 |
| Yes | 2966 | 64.9 |
| Radiotherapy | ||
| No | 3354 | 73.4 |
| Yes | 1169 | 25.6 |
| Unknown | 45 | 1.0 |
| Univariate | Multivariate | |||||
|---|---|---|---|---|---|---|
| Variables | HR | 95% CI | p-Value | HR | 95% CI | p-Value |
| Gender | 1.178 | 1.058–1.313 | 0.003 | |||
| Grade | ||||||
| I: well differentiated | 1 (reference) | <0.001 | ||||
| II: moderately differentiated | 2.623 | 1.250–5.502 | 0.011 | 2.376 | 1.098–5.143 | 0.028 |
| III: poorly differentiated | 2.180 | 1.274–3.730 | 0.004 | 2.451 | 1.396–4.303 | 0.002 |
| IV: undifferentiated | 4.669 | 2.713–8.033 | <0.001 | 3.693 | 2.095–6.508 | <0.001 |
| Unknown | 3.416 | 2.014–5.792 | <0.001 | 2.304 | 1.329–3.996 | 0.003 |
| Radiotherapy | 2.269 | 2.034–2.532 | <0.001 | 1.353 | 1.201–1.524 | <0.001 |
| Surgery | 0.392 | 0.350–0.438 | <0.001 | 0.434 | 0.384–0.489 | <0.001 |
| Chemotherapy | 3.452 | 2.974–4.007 | <0.001 | 2.302 | 1.945–2.724 | <0.001 |
| Race | ||||||
| White | 1 (reference) | |||||
| Black | 1.233 | 1.059–1.435 | 0.007 | |||
| unknown | 1.141 | 0.945–1.375 | 0.171 | |||
| Age | ||||||
| <1 | 1 (reference) | |||||
| 1–3 | 3.927 | 3.296–4.678 | <0.001 | 3.712 | 3.091–4.459 | <0.001 |
| 4–6 | 4.278 | 3.478–5.261 | <0.001 | 4.103 | 3.303–5.097 | <0.001 |
| 7–14 | 4.554 | 3.613–5.740 | <0.001 | 5.222 | 4.104–6.645 | <0.001 |
| 15–18 | 6.135 | 4.191–8.980 | <0.001 | 6.080 | 4.124–8.962 | <0.001 |
| >18 | 8.490 | 6.699–10.760 | <0.001 | 9.783 | 7.589–12.612 | <0.001 |
| Year of Diagnosis | ||||||
| 1975–1984 | 1 (reference) | |||||
| 1985–1994 | 0.622 | 0.525–0.737 | <0.001 | 0.530 | 0.442–0.636 | <0.001 |
| 1995–2004 | 0.462 | 0.395–0.539 | <0.001 | 0.354 | 0.297–0.422 | <0.001 |
| 2005–2016 | 0.329 | 0.283–0.383 | <0.001 | 0.250 | 0.210–0.297 | <0.001 |
| Primary site | ||||||
| Adrenal | 1 (reference) | |||||
| Retroperitoneum | 0.843 | 0.714–0.995 | 0.043 | 0.741 | 0.623–0.882 | 0.01 |
| Others | 0.575 | 0.511–0.646 | <0.001 | 0.526 | 0.462–0.599 | <0.001 |
| Variables | Univariate | Multivariate | ||||
|---|---|---|---|---|---|---|
| HR | 95% CI | p-Value | HR | 95% CI | p-Value | |
| Gender | 1.190 | 0.932–1.520 | 0.162 | |||
| Grade | ||||||
| I: well differentiated | 1 (reference) | |||||
| II: moderately differentiated | 3.222 | 1.335–7.775 | 0.009 | 2.847 | 1.172–6.912 | 0.021 |
| III: poorly differentiated | 2.820 | 1.446–5.499 | 0.002 | 2.691 | 1.368–5.295 | 0.004 |
| IV: undifferentiated | 5.794 | 2.952–11.373 | <0.001 | 3.826 | 1.935–7.568 | <0.001 |
| Unknown | 3.100 | 1.602–6.001 | 0.001 | 2.326 | 1.198–4.516 | 0.013 |
| Radiotherapy | 1.916 | 1.473–2.491 | <0.001 | 1.362 | 1.169–1.587 | <0.001 |
| Chemotherapy | 2.714 | 1.798–4.098 | <0.001 | 2.309 | 1.784–4.423 | <0.001 |
| Race | ||||||
| White | 1 (reference) | |||||
| Black | 0.877 | 0.604–1.275 | 0.493 | |||
| Unknown | 1.405 | 1.007–1.962 | 0.046 | |||
| Age at diagnosis (years) | ||||||
| <1 | 1 (reference) | |||||
| 1–3 | 4.508 | 3.111–6.531 | <0.001 | 3.382 | 2.291–4.992 | <0.001 |
| 4–6 | 4.778 | 3.025–7.545 | <0.001 | 3.933 | 2.448–6.321 | <0.001 |
| 7–14 | 5.782 | 3.390–9.862 | <0.001 | 5.542 | 3.211–9.567 | <0.001 |
| 15–18 | 4.450 | 1.743–11.363 | <0.001 | 6.304 | 2.425–16.385 | <0.001 |
| >18 | 9.066 | 5.512–14.912 | <0.001 | 10.965 | 6.503–18.489 | <0.001 |
| Year of diagnosis | ||||||
| 1975–1984 | 1 (reference) | |||||
| 1985–1994 | 0.803 | 0.539–1.198 | 0.283 | 0.498 | 0.323–0.768 | 0.002 |
| 1995–2004 | 0.723 | 0.501–1.043 | 0.083 | 0.408 | 0.271–0.613 | <0.001 |
| 2005–2016 | 0.516 | 0.358–0.743 | <0.001 | 0.314 | 0.207–0.478 | <0.001 |
| Primary Site | ||||||
| Adrenal | 1 (reference) | |||||
| Retroperitoneum | 0.739 | 0.503–1.086 | 0.124 | 0.790 | 0.632–0.986 | 0.037 |
| Others | 0.445 | 0.340–0.584 | <0.001 | 0.443 | 0.370–0.530 | <0.001 |
Disclaimer/Publisher’s Note: The statements, opinions and data contained in all publications are solely those of the individual author(s) and contributor(s) and not of MDPI and/or the editor(s). MDPI and/or the editor(s) disclaim responsibility for any injury to people or property resulting from any ideas, methods, instructions or products referred to in the content. |
© 2023 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Li, Q.; Wang, J.; Cheng, Y.; Hu, A.; Li, D.; Wang, X.; Guo, Y.; Zhou, Y.; Chen, G.; Bao, B.; et al. Long-Term Survival of Neuroblastoma Patients Receiving Surgery, Chemotherapy, and Radiotherapy: A Propensity Score Matching Study. J. Clin. Med. 2023, 12, 754. https://doi.org/10.3390/jcm12030754
Li Q, Wang J, Cheng Y, Hu A, Li D, Wang X, Guo Y, Zhou Y, Chen G, Bao B, et al. Long-Term Survival of Neuroblastoma Patients Receiving Surgery, Chemotherapy, and Radiotherapy: A Propensity Score Matching Study. Journal of Clinical Medicine. 2023; 12(3):754. https://doi.org/10.3390/jcm12030754
Chicago/Turabian StyleLi, Qilan, Jianqun Wang, Yang Cheng, Anpei Hu, Dan Li, Xiaojing Wang, Yanhua Guo, Yi Zhou, Guo Chen, Banghe Bao, and et al. 2023. "Long-Term Survival of Neuroblastoma Patients Receiving Surgery, Chemotherapy, and Radiotherapy: A Propensity Score Matching Study" Journal of Clinical Medicine 12, no. 3: 754. https://doi.org/10.3390/jcm12030754
APA StyleLi, Q., Wang, J., Cheng, Y., Hu, A., Li, D., Wang, X., Guo, Y., Zhou, Y., Chen, G., Bao, B., Gao, H., Song, J., Du, X., Zheng, L., & Tong, Q. (2023). Long-Term Survival of Neuroblastoma Patients Receiving Surgery, Chemotherapy, and Radiotherapy: A Propensity Score Matching Study. Journal of Clinical Medicine, 12(3), 754. https://doi.org/10.3390/jcm12030754





