Computational Simulation Model to Predict Behavior Changes in Inflammatory Bowel Disease Patients during the COVID-19 Pandemic: Analysis of Two Regional Japanese Populations
Abstract
:1. Introduction
2. Materials and Methods
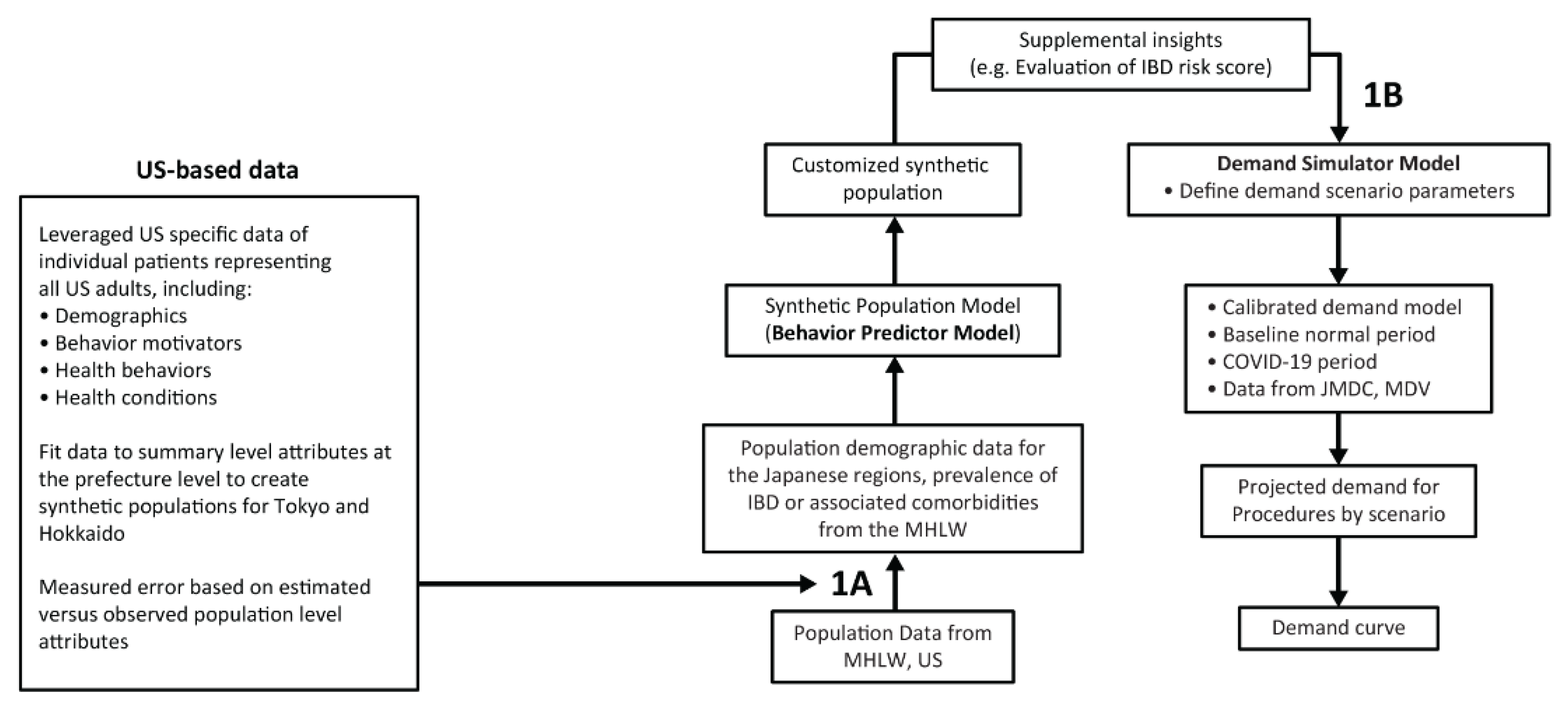
2.1. Synthetic IBD Population Model
2.2. Demand Simulation Model
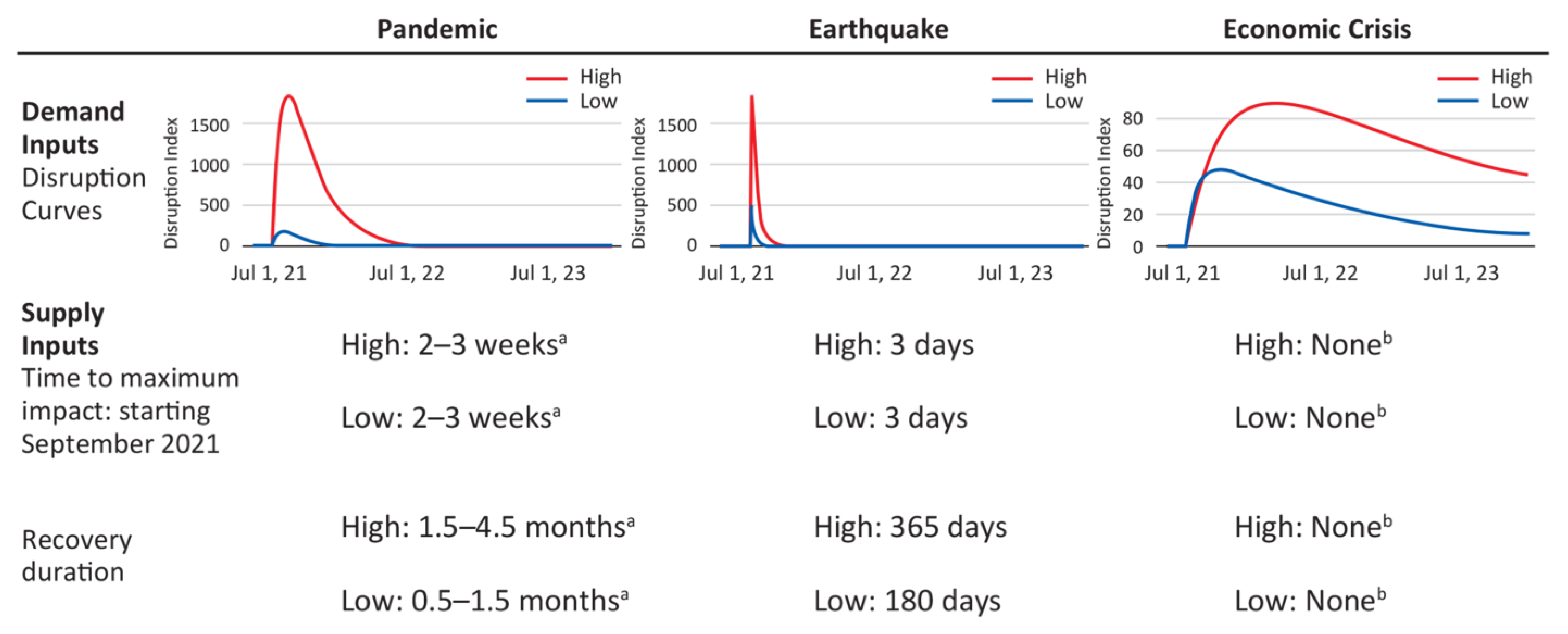
2.3. Simulation of Possible Future Crisis Scenarios for COVID-19 on Healthcare Demand
2.4. Interventions to Address the Impact of Disruptions
3. Results
3.1. Population Statistics
3.2. Calibration of Japanese Population of Patients with IBD
3.3. Impact of the COVID-19 Pandemic on Utilization of Medical Care for IBD
3.4. Interventions to Address the Impact of Disruptions
4. Discussion
5. Conclusions
Supplementary Materials
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Acknowledgments
Conflicts of Interest
References
- World Health Organization (WHO). Coronavirus COVID-19 Dashboard. Available online: https://covid19.who.int (accessed on 27 January 2022).
- Scaldaferri, F.; Pugliese, D.; Privitera, G.; Onali, S.; Lopetuso, L.R.; Rizzatti, G.; Settanni, C.R.; Pizzoferrato, M.; Schiavoni, E.; Turchini, L.; et al. Impact of COVID-19 pandemic on the daily management of biotechnological therapy in inflammatory bowel disease patients: Reorganisational response in a high-volume Italian inflammatory bowel disease centre. United Eur. Gastroenterol. J. 2020, 8, 775–781. [Google Scholar] [CrossRef] [PubMed]
- Kumric, M.; Kurir, T.T.; Martinovic, D.; Zivkovic, P.M.; Bozic, J. Impact of the COVID-19 pandemic on inflammatory bowel disease patients: A review of the current evidence. World J. Gastroenterol. 2021, 27, 3748–3761. [Google Scholar] [CrossRef] [PubMed]
- Moynihan, R.; Sanders, S.; Michaleff, Z.A.; Scott, A.M.; Clark, J.; To, E.J.; Jones, M.; Kitchener, E.; Fox, M.; Johansson, M.; et al. Impact of COVID-19 pandemic on utilisation of healthcare services: A systematic review. BMJ Open 2021, 11, e045343. [Google Scholar] [CrossRef]
- Ng, S.C.; Shi, H.Y.; Hamidi, N.; Underwood, F.E.; Tang, W.; Benchimol, E.I.; Panaccione, R.; Ghosh, S.; Wu, J.C.Y.; Chan, F.K.L.; et al. Worldwide incidence and prevalence of inflammatory bowel disease in the 21st century: A systematic review of population-based studies. Lancet 2018, 390, 2769–2778. [Google Scholar] [CrossRef] [PubMed]
- Fiorino, G.; Allocca, M.; Chaparro, M.; Coenen, S.; Fidalgo, C.; Younge, L.; Gisbert, P.G. ‘Quality of care’ standards in inflammatory bowel disease: A systematic review. J. Crohn’s Colitis 2019, 13, 127–137. [Google Scholar] [CrossRef]
- Siegel, C.A.; Melmed, G.Y.; McGovern, D.P.; Rai, V.; Krammer, F.; Rubin, D.T.; Abreu, M.T.; Dubinsky, M.C.; International Organization for the Study of Inflammatory Bowel Disease. SARS-CoV-2 vaccination for patients with inflammatory bowel diseases: Recommendations from an international consensus meeting. Gut 2021, 70, 635–640. [Google Scholar] [CrossRef]
- Pinto, S.; Loddo, E.; Paba, S.; Favale, A.; Chicco, F.; Onali, S.; Usai, P.; Fantini, M.C. Crohn’s disease and ulcerative colitis patient-reported outcomes signs and symptoms for the remote management of inflammatory bowel disease during the COVID-19 pandemic. J. Patient-Rep. Outcomes 2021, 5, 48. [Google Scholar] [CrossRef]
- Rubin, D.T.; Abreu, M.T.; Rai, V.; Siegel, C.A.; Ahuja, V.; Allez, M.; Ananthakrishnan, A.N.; Bernstein, C.N.; Braun, J.G.; Chowers, Y.; et al. Management of patients with Crohn’s disease and ulcerative colitis during the coronavirus disease-2019 pandemic: Results of an international meeting. Gastroenterology 2020, 159, 6–13.e6. [Google Scholar] [CrossRef]
- Nakase, H.; Matsumoto, T.; Matsuura, M.; Iijima, H.; Matsuoka, K.; Ohmiya, N.; Ishihara, S.; Hirai, F.; Wagatsuma, K.; Yokoyama, Y.; et al. Expert opinions on the current therapeutic management of inflammatory bowel disease during the COVID-19 pandemic: Japan IBD COVID-19 Taskforce, Intractable Diseases, the Health and Labor Sciences Research. Digestion 2020, 102, 814–822. [Google Scholar] [CrossRef]
- Kennedy, N.A.; Jones, G.-R.; Lamb, C.A.; Appleby, R.; Arnott, I.; Beattie, R.M.; Bloom, S.; Brooks, A.J.; Cooney, R.; Dart, R.J.; et al. British Society of Gastroenterology guidance for management of inflammatory bowel disease during the COVID-19 pandemic. Gut 2020, 69, 984–990. [Google Scholar] [CrossRef]
- Chebli, J.M.F.; Queiroz, N.S.F.; Damião, A.O.M.C.; Chebli, L.A.; Costa, M.H.D.M.; Parra, R.S. How to manage inflammatory bowel disease during the COVID-19 pandemic: A guide for the practicing clinician. World J. Gastroenterol. 2021, 27, 1022–1042. [Google Scholar] [CrossRef] [PubMed]
- Kubas, A.; Malecka-Wojciesko, E. COVID-19 vaccination in inflammatory bowel disease (IBD). J. Clin. Med. 2022, 11, 2676. [Google Scholar] [CrossRef] [PubMed]
- Lin, S.; Lau, L.H.; Chanchlani, N.; Kennedy, N.A.; Ng, S.C. Recent advances in clinical practice: Management of inflammatory bowel disease during the COVID-19 pandemic. Gut 2022, 71, 1426–1439. [Google Scholar] [CrossRef] [PubMed]
- Aziz, M.; Fatima, R.; Haghbin, H.; Lee-Smith, W.; Nawras, A. The incidence and outcomes of COVID-19 in IBD patients: A rapid review and meta-analysis. Inflamm. Bowel Dis. 2020, 26, e132–e133. [Google Scholar] [CrossRef]
- Brenner, E.J.; Ungaro, R.C.; Gearry, R.B.; Kaplan, G.G.; Kissous-Hunt, M.; Lewis, J.D.; Ng, S.C.; Rahier, J.-F.; Reinisch, W.; Ruemmele, F.M.; et al. Corticosteroids, but not TNF antagonists, are associated with adverse COVID-19 outcomes in patients with inflammatory bowel diseases: Results from an international registry. Gastroenterology 2020, 159, 481–491.e3. [Google Scholar] [CrossRef]
- Ungaro, R.C.; Brenner, E.J.; Agrawal, M.; Zhang, X.; Kappelman, M.D.; Colombel, J.-F.; Gearry, R.B.; Kaplan, G.G.; Kissous-Hunt, M.; Lewis, J.D.; et al. Impact of medications on COVID-19 outcomes in inflammatory bowel disease: Analysis of more than 6000 patients from an international registry. Gastroenterology 2022, 162, 316–319.e5. [Google Scholar] [CrossRef]
- Izadi, Z.; Brenner, E.J.; Mahil, S.K.; Dand, N.; Yiu, Z.Z.N.; Yates, M.; Ungaro, R.C.; Zhang, X.; Agrawal, M.; Colombel, J.-F.; et al. Association between tumor necrosis factor inhibitors and the risk of hospitalization or death among patients with immune-mediated inflammatory disease and COVID-19. JAMA Netw. Open 2021, 4, e2129639. [Google Scholar] [CrossRef]
- Satsangi, J.; Jewell, D.P.; Rosenberg, W.M.; Bell, J.I. Genetics of inflammatory bowel disease. Gut 1994, 35, 696–700. [Google Scholar] [CrossRef] [Green Version]
- Kumar, M.; Garand, M.; Al Khodor, S. Integrating omics for a better understanding of inflammatory bowel disease: A step towards personalized medicine. J. Transl. Med. 2019, 17, 419. [Google Scholar]
- Abegunde, A.T.; Muhammad, B.H.; Bhatti, O.; Ali, T. Environmental risk factors for inflammatory bowel diseases: Evidence based literature review. World J. Gastroenterol. 2016, 22, 6296–6317. [Google Scholar] [CrossRef]
- Tiongco, M.; Gonzales, C.; Cuyegkeng, M. Exploring the interdependencies of entrepreneurial ecosystems using feedback-guided analysis for social enterprise resilience. In Proceedings of the 2021 International Conference of the System Dynamics Society (ISDC), virtual, 25 July 2021. [Google Scholar]
- Dagan, N.; Barda, N.; Kepten, E.; Miron, O.; Perchik, S.; Katz, M.A.; Hernán, M.A.; Lipsitch, M.; Reis, B.; Balicer, R.D. BNT162b2 mRNA Covid-19 vaccine in a nationwide mass vaccination setting. N. Engl. J. Med. 2021, 384, 1412–1423. [Google Scholar] [CrossRef]
- Chudasama, Y.V.; Gillies, C.L.; Zaccardi, F.; Coles, B.; Davies, M.J.; Seidu, S.; Khunti, K. Impact of COVID-19 on routine care for chronic diseases: A global survey of views from healthcare professionals. Diabetes Metab. Syndr. Clin. Res. Rev. 2020, 14, 965–967. [Google Scholar] [CrossRef]
- Chenneville, T.; Gabbidon, K.; Hanson, P.; Holyfield, C. The impact of COVID-19 on HIV treatment and research: A call to action. Int. J. Environ. Res. Public Health 2020, 17, 4548. [Google Scholar] [CrossRef]
- Gregg, E.W.; Sophiea, M.K.; Weldegiorgis, M. Diabetes and COVID-19: Population impact 18 months into the pandemic. Diabetes Care 2021, 44, 1916–1923. [Google Scholar] [CrossRef]
- Sugawara, Y.; Iwagami, M.; Yoshida, Y.; Kikuchi, K.; Ando, R.; Shinoda, T.; Ryuzaki, M.; Nakamoto, H.; Sakai, K.; Hanafusa, N.; et al. Nationwide survey of the coronavirus disease 2019 prevention and treatment systems for kidney disease patients: A study of Japanese Society of Nephrology-certified educational facilities. Clin. Exp. Nephrol. 2021, 25, 996–1002. [Google Scholar] [CrossRef]
- Hisamatsu, T. Management of inflammatory bowel disease during the COVID-19 pandemic. Immunol. Med. 2022, 45, 128–135. [Google Scholar] [CrossRef]
- Shinohara, T.; Saida, K.; Tanaka, S.; Murayama, A. Do lifestyle measures to counter COVID-19 affect frailty rates in elderly community dwelling? Protocol for cross-sectional and cohort study. BMJ Open 2020, 10, e040341. [Google Scholar] [CrossRef]



| Intervention | Description | Impact of Intervention on Supply | Impact of Intervention on Demand | ||
|---|---|---|---|---|---|
| Physician outreach | Physicians message at a practice level to their patients (reach out to individual patients at risk) | N/A | 15% | Patients starting to seek care; biologic prescriptions; clinic visits | |
| System social signaling | Hospital systems reinforce confidence to their local area (targeted social media and local press efforts to a small footprint audience) | N/A | 40% | Patients starting to seek care; biologic prescriptions; clinic visits | |
| National confidence building | Government messages at a societal level, building confidence to stay engaged with care systems (broad scale media and high-level official communication efforts) | N/A | 60% | Patients starting to seek care; biologic prescriptions; clinic visits | |
| Simple navigation assistance | Education-focused initiatives on how best to navigate post-disruption (scheduling, where to go, who to see) | 5% | Access to continuous care; access to biologics; supply of procedures | 15% | Patients starting to seek care; biologic prescriptions; clinic visits |
| Barrier elimination | Partnership with government and/or private sector to subsidize transportation when regular channels are not available | 40% | Access to continuous care; access to biologics; supply of procedures | 40% | Patients starting to seek care; biologic prescriptions; clinic visits |
| Emergency response infrastructure | Infrastructure to provide emergency care on demand if the normal setting is disrupted | 60% | Access to continuous care; access to biologics; supply of procedures | 55% | Patients starting to seek care; biologic prescriptions; clinic visits |
Disclaimer/Publisher’s Note: The statements, opinions and data contained in all publications are solely those of the individual author(s) and contributor(s) and not of MDPI and/or the editor(s). MDPI and/or the editor(s) disclaim responsibility for any injury to people or property resulting from any ideas, methods, instructions or products referred to in the content. |
© 2023 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Suzuki, G.; Iwakiri, R.; Udagawa, E.; Ma, S.; Takayama, R.; Nishiura, H.; Nakamura, K.; Burns, S.P.; D’Alessandro, P.M.; Fernandez, J. Computational Simulation Model to Predict Behavior Changes in Inflammatory Bowel Disease Patients during the COVID-19 Pandemic: Analysis of Two Regional Japanese Populations. J. Clin. Med. 2023, 12, 757. https://doi.org/10.3390/jcm12030757
Suzuki G, Iwakiri R, Udagawa E, Ma S, Takayama R, Nishiura H, Nakamura K, Burns SP, D’Alessandro PM, Fernandez J. Computational Simulation Model to Predict Behavior Changes in Inflammatory Bowel Disease Patients during the COVID-19 Pandemic: Analysis of Two Regional Japanese Populations. Journal of Clinical Medicine. 2023; 12(3):757. https://doi.org/10.3390/jcm12030757
Chicago/Turabian StyleSuzuki, Gen, Ryuichi Iwakiri, Eri Udagawa, Sindy Ma, Ryoko Takayama, Hiroshi Nishiura, Koshi Nakamura, Samuel P. Burns, Paul Michael D’Alessandro, and Jovelle Fernandez. 2023. "Computational Simulation Model to Predict Behavior Changes in Inflammatory Bowel Disease Patients during the COVID-19 Pandemic: Analysis of Two Regional Japanese Populations" Journal of Clinical Medicine 12, no. 3: 757. https://doi.org/10.3390/jcm12030757
APA StyleSuzuki, G., Iwakiri, R., Udagawa, E., Ma, S., Takayama, R., Nishiura, H., Nakamura, K., Burns, S. P., D’Alessandro, P. M., & Fernandez, J. (2023). Computational Simulation Model to Predict Behavior Changes in Inflammatory Bowel Disease Patients during the COVID-19 Pandemic: Analysis of Two Regional Japanese Populations. Journal of Clinical Medicine, 12(3), 757. https://doi.org/10.3390/jcm12030757







