Incidence of Isolated Biliary Atresia during the COVID Lockdown in Europe: Results from a Collaborative Project by RARE-Liver
Abstract
:1. Introduction
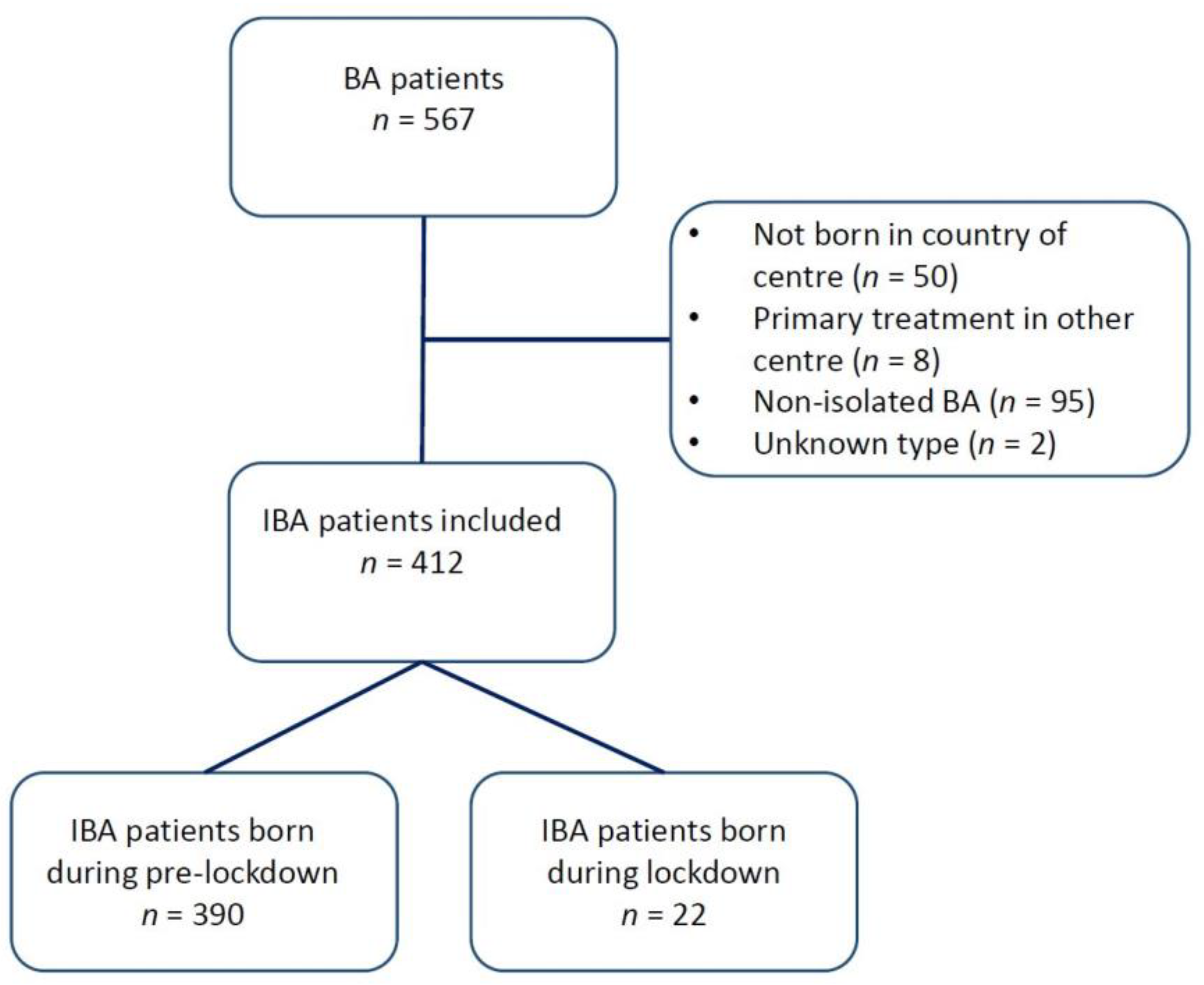
2. Materials and Methods
Statistical Analysis
3. Results
3.1. Number of IBA Patients before and during the Lockdown Period
3.2. Association between Patients Acquiring IBA and Strictness of Lockdown
3.3. Age at KPE
4. Discussion
5. Conclusions
Supplementary Materials
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Acknowledgments
Conflicts of Interest
References
- Mack, C.L.; Feldman, A.G.; Sokol, R.J. Clues to the Etiology of Bile Duct Injury in Biliary Atresia. Semin. Liver Dis. 2012, 32, 307–316. [Google Scholar] [CrossRef] [Green Version]
- Hartley, J.L.; Davenport, M.; Kelly, D.A. Biliary atresia. Lancet 2009, 374, 1704–1713. [Google Scholar] [CrossRef]
- Mohanty, S.K.; Donnelly, B.; Temple, H.; Tiao, G.M. A Rotavirus-Induced Mouse Model to Study Biliary Atresia and Neonatal Cholestasis. Methods Mol. Biol. 2019, 1981, 259–271. [Google Scholar] [CrossRef] [PubMed]
- Xu, Y.; Yu, J.; Zhang, R.; Yin, Y.; Ye, J.; Tan, L.; Xia, H. The Perinatal Infection of Cytomegalovirus Is an Important Etiology for Biliary Atresia in China. Clin. Pediatr. 2011, 51, 109–113. [Google Scholar] [CrossRef] [PubMed]
- Riepenhoff-Talty, M.; Gouvea, V.; Evans, M.J.; Svensson, L.; Hoffenberg, E.; Sokol, R.J.; Uhnoo, I.; Greenberg, S.J.; Schakel, K.; Zhaori, G.; et al. Detection of Group C Rotavirus in Infants with Extrahepatic Biliary Atresia. J. Infect. Dis. 1996, 174, 8–15. [Google Scholar] [CrossRef] [PubMed]
- Zani, A.; Quaglia, A.; Hadzić, N.; Zuckerman, M.; Davenport, M. Cytomegalovirus-associated biliary atresia: An aetiological and prognostic subgroup. J. Pediatr. Surg. 2015, 50, 1739–1745. [Google Scholar] [CrossRef] [PubMed]
- Fischler, B.; Ehrnst, A.; Forsgren, M.; Örvell, C.; Nemeth, A. The Viral Association of Neonatal Cholestasis in Sweden: A Possible Link Between Cytomegalovirus Infection and Extrahepatic Biliary Atresia. J. Craniofacial Surg. 1998, 27, 57–64. [Google Scholar] [CrossRef]
- Fischler, B.; Czubkowski, P.; Dezsofi, A.; Liliemark, U.; Socha, P.; Sokol, R.J.; Svensson, J.F.; Davenport, M. Incidence, Impact and Treatment of Ongoing CMV Infection in Patients with Biliary Atresia in Four European Centres. J. Clin. Med. 2022, 11, 945. [Google Scholar] [CrossRef]
- Davenport, M.; Muntean, A.; Hadzic, N. Biliary Atresia: Clinical Phenotypes and Aetiological Heterogeneity. J. Clin. Med. 2021, 10, 5675. [Google Scholar] [CrossRef]
- Sohrabi, C.; Alsafi, Z.; O’Neill, N.; Khan, M.; Kerwan, A.; Al-Jabir, A.; Iosifidis, C.; Agha, R. World Health Organization declares global emergency: A review of the 2019 novel coronavirus (COVID-19). Int. J. Surg. 2020, 76, 71–76. [Google Scholar] [CrossRef]
- World Health Organization (WHO). Coronavirus Disease (COVID-19) Advice for the Public. 2020. Available online: https://www.who.int/emergencies/diseases/novel-coronavirus-2019/advice-for-public (accessed on 18 September 2020).
- Kurgat, E.K.; Sexton, J.D.; Garavito, F.; Reynolds, A.; Contreras, R.D.; Gerba, C.P.; Leslie, R.A.; Edmonds-Wilson, S.L.; Reynolds, K.A. Impact of a hygiene intervention on virus spread in an office building. Int. J. Hyg. Environ. Health 2019, 222, 479–485. [Google Scholar] [CrossRef] [PubMed]
- Luangasanatip, N.; Hongsuwan, M.; Limmathurotsakul, D.; Lubell, Y.; Lee, A.S.; Harbarth, S.; Day, N.P.J.; Graves, N.; Cooper, B. Comparative efficacy of interventions to promote hand hygiene in hospital: Systematic review and network meta-analysis. BMJ 2015, 351, h3728. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Hooiveld, M.; Hendriksen, J.; Korevaar, J. Wekelijkse Surveillance Cijfers [Internet]. Nivel Zorgregistraties Eerste Lijn. 2020. Available online: www.nivel.nl/surveillance (accessed on 18 September 2020).
- Harris, P.A.; Taylor, R.; Thielke, R.; Payne, J.; Gonzalez, N.; Conde, J.G. Research electronic data capture (REDCap)—A metadata-driven methodology and workflow process for providing translational research informatics support. J. Biomed. Inform. 2009, 42, 377–381. [Google Scholar] [CrossRef] [Green Version]
- Hale, T.; Angrist, N.; Goldszmidt, R.; Kira, B.; Petherick, A.; Phillips, T.; Webster, S.; Cameron-Blake, E.; Hallas, L.; Majumdar, S.; et al. A global panel database of pandemic policies (Oxford COVID-19 Government Response Tracker). Nat. Hum. Behav. 2021, 5, 529–538. [Google Scholar] [CrossRef]
- Hale, T.; Angrist, N.; Hale, A.J.; Kira, B.; Majumdar, S.; Petherick, A.; Phillips, T.; Sridhar, D.; Thompson, R.N.; Webster, S.; et al. Government responses and COVID-19 deaths: Global evidence across multiple pandemic waves. PLoS ONE 2021, 16, e0253116. [Google Scholar] [CrossRef]
- Livesey, E.; Borja, M.C.; Sharif, K.; Alizai, N.; McClean, P.; Kelly, D.; Hadzic, N.; Davenport, M. Epidemiology of biliary atresia in England and Wales (1999–2006). Arch. Dis. Child. Fetal Neonatal Ed. 2009, 94, F451–F455. [Google Scholar] [CrossRef] [PubMed]
- Chardot, C.; Carton, M.; Spire-Bendelac, N.; Le Pommelet, C.; Golmard, J.-L.; Auvert, B. Epidemiology of biliary atresia in France: A national study 1986–96. J. Hepatol. 1999, 31, 1006–1013. [Google Scholar] [CrossRef] [PubMed]
- Nomden, M.; van Wessel, D.B.; Ioannou, S.; Verkade, H.J.; de Kleine, R.H.; Alizadeh, B.Z.; Bruggink, J.L.; Hulscher, J.B. A Higher Incidence of Isolated Biliary Atresia in Rural Areas: Results From an Epidemiological Study in The Netherlands. J. Craniofacial Surg. 2021, 72, 202–209. [Google Scholar] [CrossRef] [PubMed]
- Wildhaber, B.E.; Majno, P.; Mayr, J.; Zachariou, Z.; Hohlfeld, J.; Schwoebel, M.; Kistler, W.; Meuli, M.; Le Coultre, C.; Mentha, G.; et al. Biliary Atresia: Swiss National Study, 1994–2004. J. Craniofacial Surg. 2008, 46, 299–307. [Google Scholar] [CrossRef] [PubMed]
- Jimenez-Rivera, C.; Jolin-Dahel, K.S.; Fortinsky, K.J.; Gozdyra, P.; Benchimol, E.I. International incidence and outcomes of biliary atresia. J. Pediatr. Gastroenterol. Nutr. 2013, 56, 344–354. [Google Scholar] [CrossRef] [PubMed]
- Schreiber, R.A.; Harpavat, S.; Hulscher, J.B.F.; Wildhaber, B.E. Biliary Atresia in 2021: Epidemiology, Screening and Public Policy. J. Clin. Med. 2022, 11, 999. [Google Scholar] [CrossRef] [PubMed]
- Fischler, B.; Haglund, B.; Hjern, A. A population-based study on the incidence and possible pre- and perinatal etiologic risk factors of biliary atresia. J. Pediatr. 2002, 141, 217–222. [Google Scholar] [CrossRef] [PubMed]
- Strickland, A.D.; Shannon, K. Studies in the etiology of extrahepatic biliary atresia: Time-space clustering. J. Pediatr. 1982, 100, 749–753. [Google Scholar] [CrossRef] [PubMed]
- Lee, K.J.; Kim, J.W.; Moon, J.S.; Ko, J.S. Epidemiology of Biliary Atresia in Korea. J. Korean Med. Sci. 2017, 32, 656–660. [Google Scholar] [CrossRef] [PubMed]
- Yoon, P.W.; Bresee, J.S.; Olney, R.S.; James, L.M.; Khoury, M.J. Epidemiology of Biliary Atresia: A Population-based Study. Pediatrics 1997, 99, 376–382. [Google Scholar] [CrossRef]
- Caton, A.R.; Druschel, C.M.; McNutt, L.A. The epidemiology of extrahepatic biliary atresia in New York State, 1983–1998. Paediatr Perinat. Epidemiol. 2004, 18, 97–105. [Google Scholar] [CrossRef]
- Mysore, K.R.; Shneider, B.L.; Harpavat, S. Biliary Atresia as a Disease Starting In Utero: Implications for Treatment, Diagnosis, and Pathogenesis. J. Craniofacial Surg. 2019, 69, 396–403. [Google Scholar] [CrossRef]
- Bezerra, J.A. Potential etiologies of biliary atresia. Pediatr. Transplant. 2005, 9, 646–651. [Google Scholar] [CrossRef]
- Kilgore, A.; Mack, C.L. Update on investigations pertaining to the pathogenesis of biliary atresia. Pediatr. Surg. Int. 2017, 33, 1233–1241. [Google Scholar] [CrossRef] [Green Version]
- Yang, Y.; Wang, J.; Zhan, Y.; Chen, G.; Shen, Z.; Zheng, S.; Dong, R. The synthetic toxin biliatresone causes biliary atresia in mice. Lab. Investig. 2020, 100, 1425–1435. [Google Scholar] [CrossRef]
- Ullrich, A.; Schranz, M.; Rexroth, U.; Hamouda, O.; Schaade, L.; Diercke, M.; Boender, T.S. Impact of the COVID-19 pandemic and associated non-pharmaceutical interventions on other notifiable infectious diseases in Germany: An analysis of national surveillance data during week 1–2016—Week 32–2020. Lancet Reg. Health Eur. 2021, 6, 100103. [Google Scholar] [CrossRef] [PubMed]



| Centre | Number of BA Patients | ||
|---|---|---|---|
| IBA | Non-IBA (% of Total) | Overall | |
| Total | 412 (80) | 95(20) * | 486 |
| Groningen, the Netherlands | 43 (88) | 6 (12) | 49 |
| Geneva, Switzerland | 14 (78) | 4 (22) | 18 |
| Helsinki, Finland | 16 (70) | 7 (30) | 23 |
| London, England | 76 (78) | 21 (22) | 97 |
| Leeds, England | 59 (91) | 6 (9) | 65 |
| Birmingham, England | 47 (78) | 13 (22) | 60 |
| Copenhagen, Denmark | 17 (89) | 2 (11) | 19 |
| Stockholm, Sweden | 21 | NA | 21 * |
| Lyon, France | 29 (81) | 7 (19) | 36 |
| Padova, Italy | 13 (100) | 0 (0) | 13 |
| Hannover, Germany | 26 (53) | 23 (47) | 49 |
| Tübingen, Germany | 33 (87) | 5 (13) | 38 |
| Bergamo, Italy | 18 (95) | 1 (5) | 19 |
| Centre | Median Number of IBA Patients Born Per Month (Range) | ||||
|---|---|---|---|---|---|
| Pre-Lockdown | Lockdown | % Change | p-Value | Stringency | |
| Countries with national BA data | |||||
| Netherlands | 0.5 (0–3) | 0 (0–0) | −100 | 0.11 | 66.1 |
| United Kingdom * | 3 (0–11) | 1 (1–3) | −41.6 | 0.17 | 66.4 |
| Denmark | 0 (0–2) | 0 (0–1) | 26.9 | 0.66 | 56.2 |
| Finland | 0 (0–2) | 0 (0–1) | 37.5 | 0.69 | 51.0 |
| Switzerland | 0 (0–2) | 0 (0–1) | 57.1 | 0.57 | 57.5 |
| Overall national | 4 (1–13) | 3 (2–3) | −37.3 | 0.12 | |
| Centres with part of national BA data | |||||
| Lyon, France | 0 (0–2) | 0 (0–1) | −26.7 | 0.74 | 75.0 |
| Bergamo, Italy | 0 (0–3) | 0 (0–1) | 22.2 | 0.70 | 78.3 |
| Tübingen, Germany | 0 (0–3) | 1 (0–1) | 34 | 0.46 | 53.9 |
| Stockholm, Sweden | 0 (0–2) | 1 (1–1) | 244.8 | 0.01 | 46.8 |
| Hannover, Germany | 0 (0–3) | 0 (0–4) | 280 | 0.61 | 53.9 |
| Padova, Italy | 0 (0–1) | 1 (0–2) | 525 | 0.02 | 78.3 |
| Overall, partly national | 2 (0–7) | 4 (4–6) | 130 | 0.01 | |
| Overall | 6 (2–15) | 7 (6–9) | 16.6 | 0.36 | |
| Country | Odds Ratio (95% Confidence Interval) | Total IBA Patients | |||
|---|---|---|---|---|---|
| Stringency Index | Pre-Lockdown | Lockdown | p | n | |
| Overall | ref | 0.68 (0.33–1.35) | 0.27 | 272 | |
| The Netherlands | 66.1 | ref | 0.25 (0.01–4.03) | 0.33 | 43 |
| United Kingdom | 66.4 | ref | 0.64 (0.26–1.56) | 0.33 | 182 |
| Denmark | 56.2 | ref | 1.32 (0.18–9.98) | 0.79 | 17 |
| Finland | 51.0 | ref | 1.50 (0.20–11.35) | 0.70 | 16 |
| Switzerland | 57.5 | ref | 1.61 (0.21–12.30) | 0.65 | 14 |
| Median Age at KPE in Days (Range) | p-Value | ||
|---|---|---|---|
| Pre-Lockdown | Lockdown | ||
| Countries with national BA data | |||
| Groningen, The Netherlands | 55.5 (27–132) | NA | NA |
| Geneva, Switzerland | 58.5 (33–90) | 52 † | 0.59 |
| Helsinki, Finland | 64 (13–154) | 84 † | 0.45 |
| London, England | 49 (16–127) | 63 (62–64) | 0.09 |
| Leeds, England | 41 (9–145) | 53 (41–65) | 0.37 |
| Birmingham, England | 41.5 (22–115) | 32 † | 0.15 |
| Copenhagen, Denmark | 43 (16–148) | 45 † | 0.83 |
| Overall centralised | 48 (9–154) | 57 (32–84) | 0.29 |
| Countries with part of national BA data | |||
| Lyon, France | 51 (17–179) | 31 † | 0.34 |
| Padova, Italy | 79 (28–92) | 51 (35–126) | 0.64 |
| Hannover, Germany | 54 (29–142) | 59 (54–70) | 0.43 |
| Tübingen, Germany | 57 (24–107) | 23 (19–27) | 0.03 |
| Bergamo, Italy | 67 (41–101) | 105 † | 0.10 |
| Stockholm, Sweden * | |||
| Overall non-centralised | 57.5 (17–179) | 52.5 (19–126) | 0.43 |
| Overall | 51 (9–179) | 53 (19–126) | 0.73 |
Disclaimer/Publisher’s Note: The statements, opinions and data contained in all publications are solely those of the individual author(s) and contributor(s) and not of MDPI and/or the editor(s). MDPI and/or the editor(s) disclaim responsibility for any injury to people or property resulting from any ideas, methods, instructions or products referred to in the content. |
© 2023 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Nomden, M.; Alizai, N.K.; Betalli, P.; Bruggink, J.L.M.; Cananzi, M.; Christensen, V.B.; D’Antiga, L.; Davenport, M.; Fischler, B.; Hindemith, L.; et al. Incidence of Isolated Biliary Atresia during the COVID Lockdown in Europe: Results from a Collaborative Project by RARE-Liver. J. Clin. Med. 2023, 12, 775. https://doi.org/10.3390/jcm12030775
Nomden M, Alizai NK, Betalli P, Bruggink JLM, Cananzi M, Christensen VB, D’Antiga L, Davenport M, Fischler B, Hindemith L, et al. Incidence of Isolated Biliary Atresia during the COVID Lockdown in Europe: Results from a Collaborative Project by RARE-Liver. Journal of Clinical Medicine. 2023; 12(3):775. https://doi.org/10.3390/jcm12030775
Chicago/Turabian StyleNomden, Mark, Naved K. Alizai, Pietro Betalli, Janneke L. M. Bruggink, Mara Cananzi, Vibeke Brix Christensen, Lorenzo D’Antiga, Mark Davenport, Björn Fischler, Luise Hindemith, and et al. 2023. "Incidence of Isolated Biliary Atresia during the COVID Lockdown in Europe: Results from a Collaborative Project by RARE-Liver" Journal of Clinical Medicine 12, no. 3: 775. https://doi.org/10.3390/jcm12030775





