Robustness of Breast Margins with Volumetric Modulated Arc Therapy without a Six-Degrees-of-Freedom Couch: A Dosimetric Evaluation
Abstract
1. Introduction
2. Materials and Methods
2.1. Patient Selection
2.2. Treatment Planning
2.3. Plan Analysis
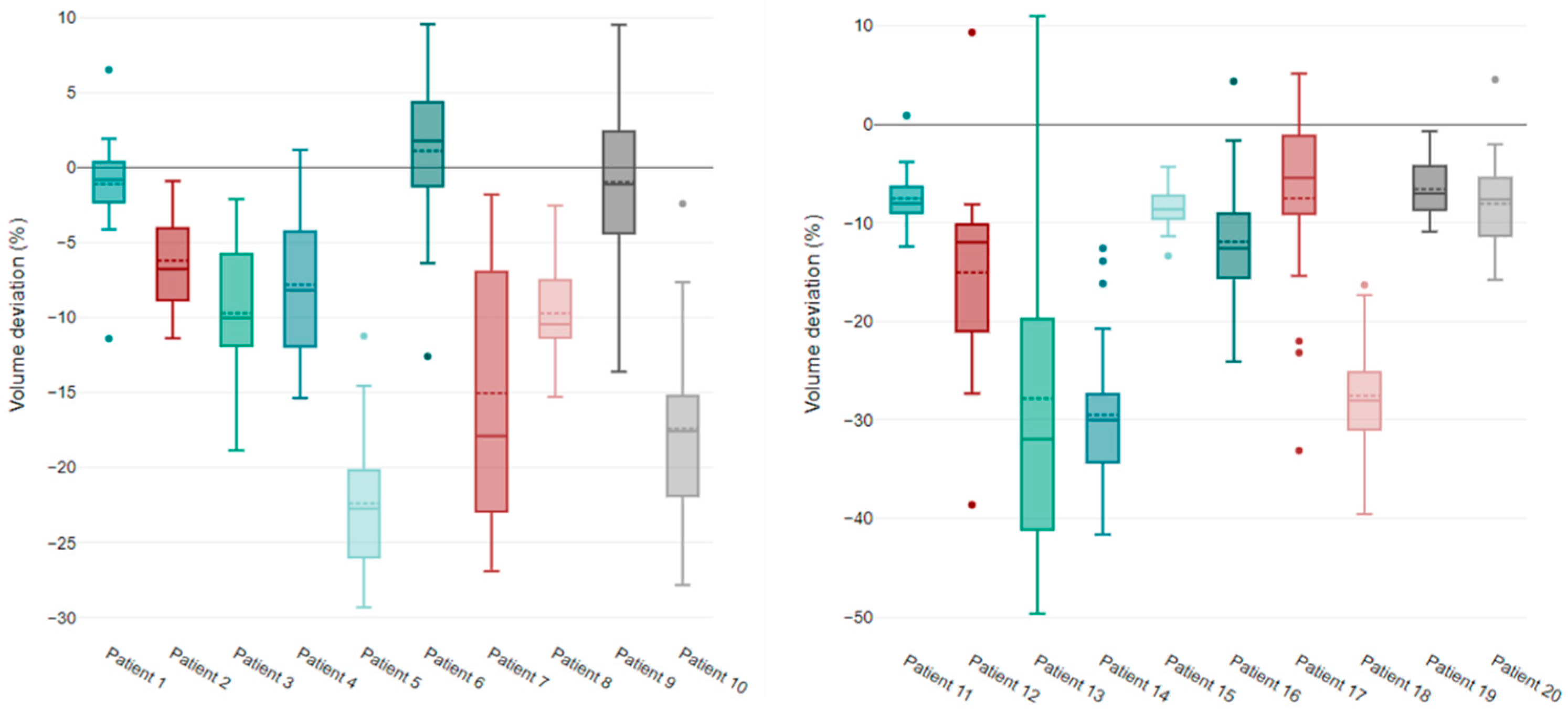
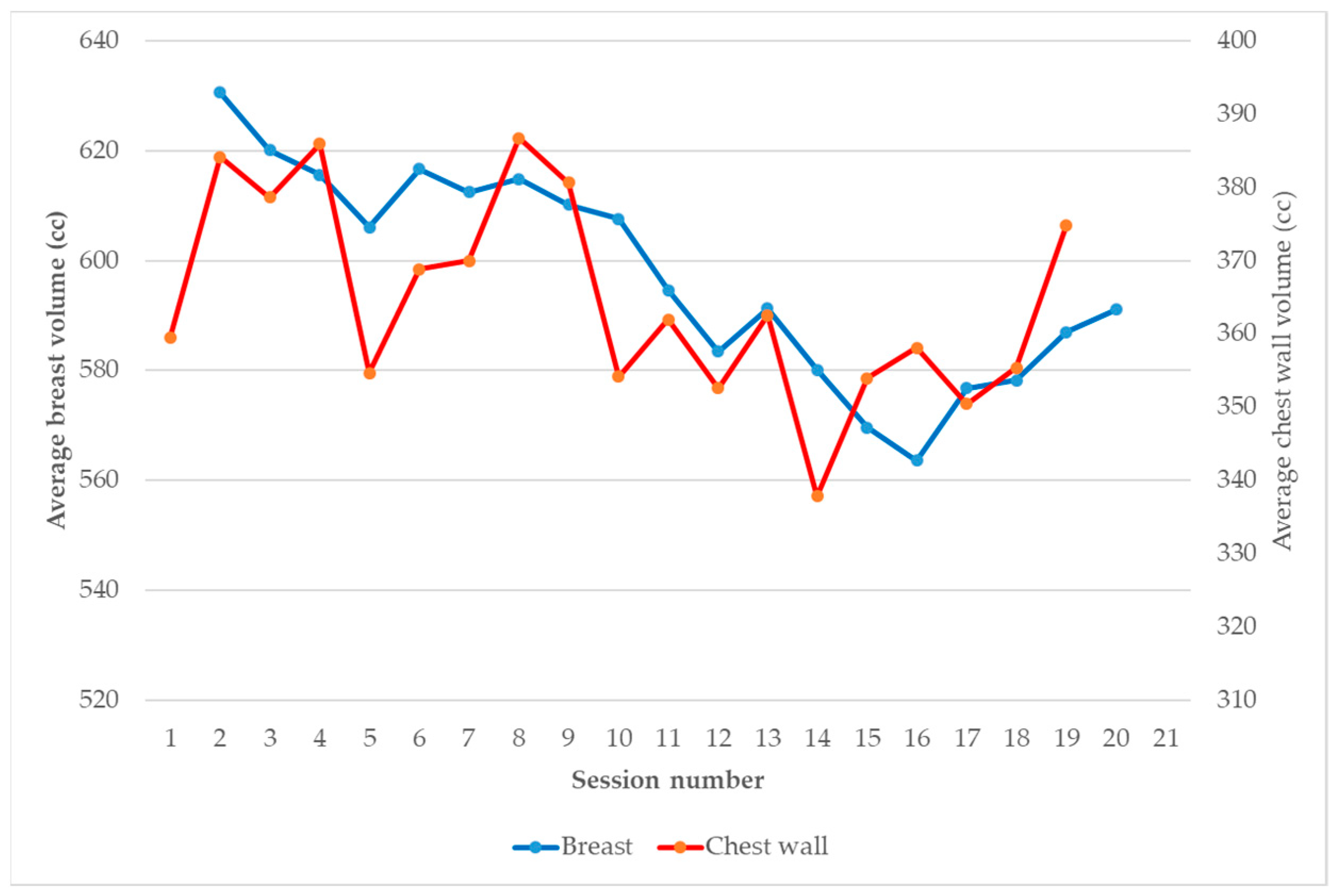
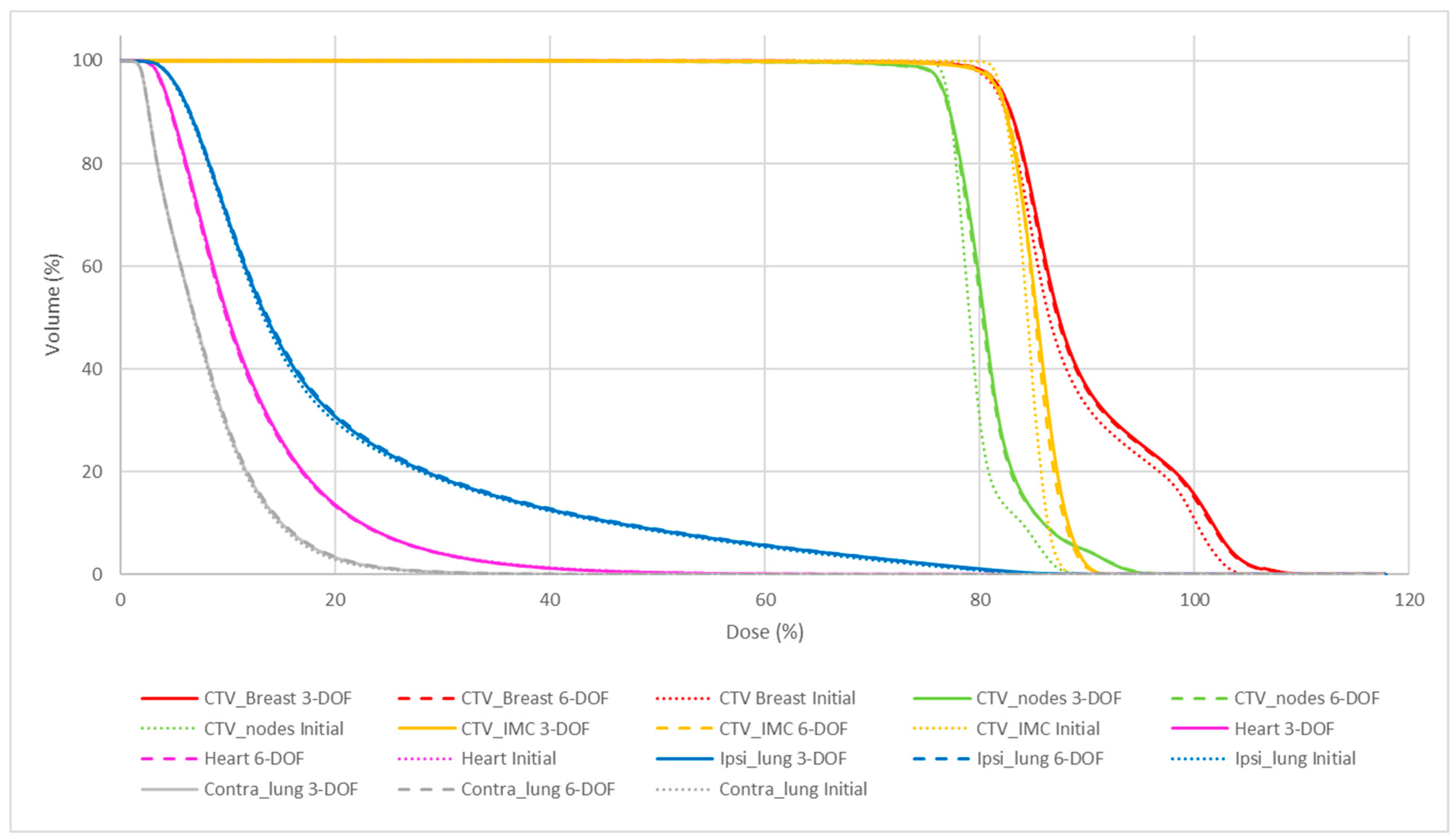
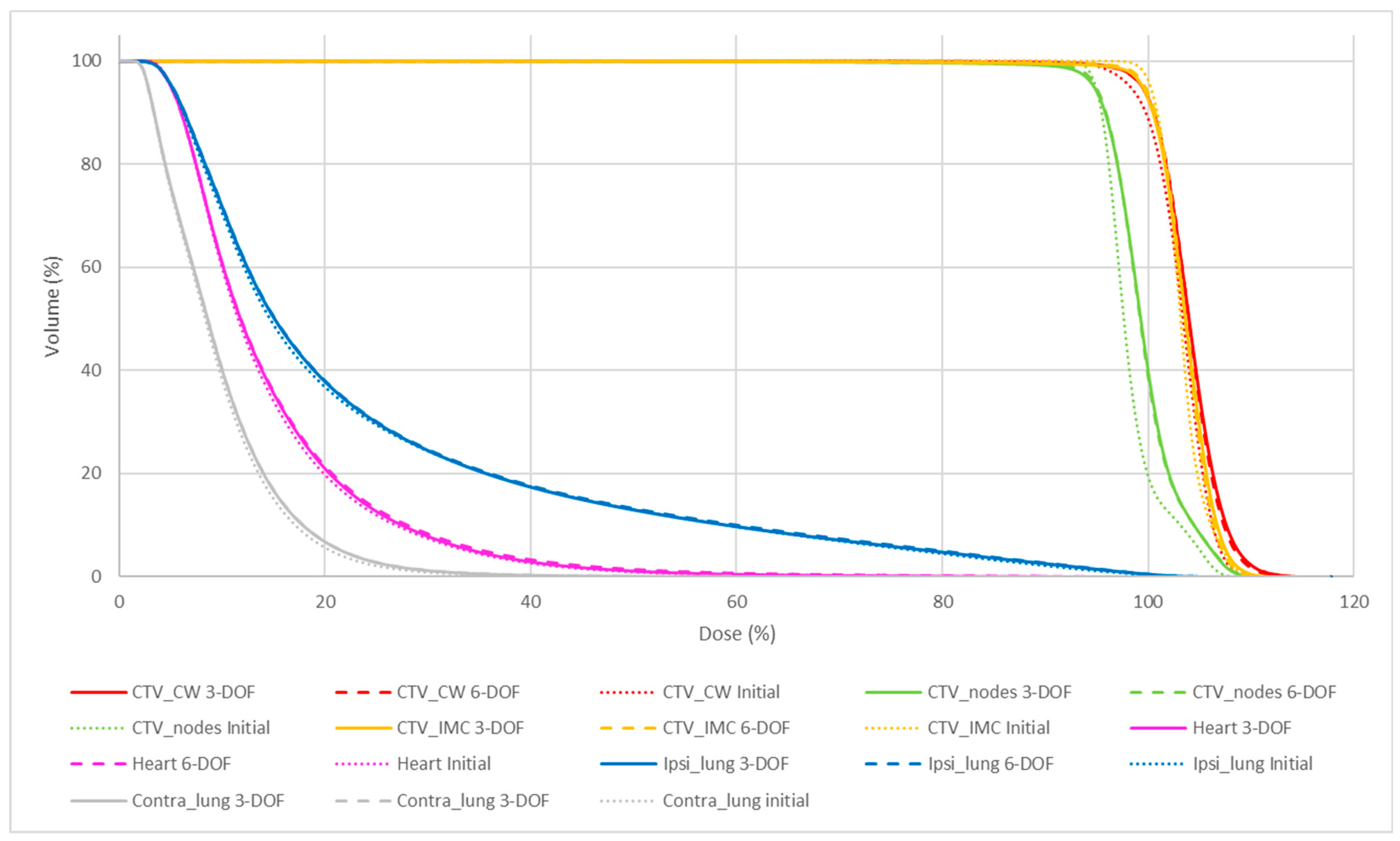
3. Results
4. Discussion
5. Conclusions
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Acknowledgments
Conflicts of Interest
References
- Mayles, W. Survey of the Availability and Use of Advanced Radiotherapy Technology in the UK. Clin. Oncol. 2010, 22, 636–642. [Google Scholar] [CrossRef] [PubMed]
- Cozzi, L.; Lohr, F.; Fogliata, A.; Franceschini, D.; De Rose, F.; Filippi, A.R.; Guidi, G.; Vanoni, V.; Scorsetti, M. Critical appraisal of the role of volumetric modulated arc therapy in the radiation therapy management of breast cancer. Radiat. Oncol. 2017, 12, 1–12. [Google Scholar] [CrossRef] [PubMed]
- Beckham, W.A.; Popescu, C.C.; Patenaude, V.V.; Wai, E.S.; Olivotto, I.A. Is Multibeam IMRT Better Than Standard Treatment for Patients with Left-Sided Breast Cancer? Int. J. Radiat. Oncol. 2007, 69, 918–924. [Google Scholar] [CrossRef] [PubMed]
- Iezzi, M.; Cusumano, D.; Piccari, D.; Menna, S.; Catucci, F.; D’Aviero, A.; Re, A.; Di Dio, C.; Quaranta, F.; Boschetti, A.; et al. Dosimetric Impact of Inter-Fraction Variability in the Treatment of Breast Cancer: Towards New Criteria to Evaluate the Appropriateness of Online Adaptive Radiotherapy. Front. Oncol. 2022, 12, 838039. [Google Scholar] [CrossRef] [PubMed]
- Sager, O.; Dincoglan, F.; Demiral, S.; Uysal, B.; Gamsiz, H.; Ozcan, F.; Colak, O.; Elcim, Y.; Gundem, E.; Dirican, B.; et al. Adaptive radiation therapy of breast cancer by repeated imaging during irradiation. World J. Radiol. 2020, 12, 68–75. [Google Scholar] [CrossRef] [PubMed]
- NCT01872975. A Randomized Phase III Clinical Trial Evaluating Postmastectomy Chestwall and Regional Nodal XRT and Post-Lumpectomy Regional Nodal XRT in Patients with Positive Axillary Nodes before Neoadjuvant Chemotherapy Who Convert to Pathologically Negative Axillary Nodes after Neoadjuvant Chemotherapy. Available online: https://clinicaltrials.gov/ct2/show/NCT01872975 (accessed on 9 May 2022).
- Seppälä, J.; Vuolukka, K.; Virén, T.; Heikkilä, J.; Honkanen, J.; Pandey, A.; Al-Gburi, A.; Shah, M.; Sefa, S.; Koivumäki, T. Breast deformation during the course of radiotherapy: The need for an additional outer margin. Phys. Medica 2019, 65, 1–5. [Google Scholar] [CrossRef]
- Luo, J.; Yin, Z.; Zhang, Z.; Guo, X.; Yu, X.; Wang, J. Does the protocol-required uniform margin around the CTV adequately account for setup inaccuracies in whole breast irradiation? Radiat. Oncol. 2021, 16, 143. [Google Scholar] [CrossRef]
- Rossi, M.; Boman, E.; Skyttä, T.; Haltamo, M.; Laaksomaa, M.; Kapanen, M. Dosimetric effects of anatomical deformations and positioning errors in VMAT breast radiotherapy. J. Appl. Clin. Med. Phys. 2018, 19, 506–516. [Google Scholar] [CrossRef]
- Garibaldi, C.; Piperno, G.; Ferrari, A.; Surgo, A.; Muto, M.; Ronchi, S.; Bazani, A.; Pansini, F.; Cremonesi, M.; Jereczek-Fossa, B.A.; et al. Translational and rotational localization errors in cone-beam CT based image-guided lung stereotactic radiotherapy. Phys. Medica 2016, 32, 859–865. [Google Scholar] [CrossRef]
- Gevaert, T.; Verellen, D.; Engels, B.; Depuydt, T.; Heuninckx, K.; Tournel, K.; Duchateau, M.; Reynders, T.; De Ridder, M. Clinical Evaluation of a Robotic 6-Degree of Freedom Treatment Couch for Frameless Radiosurgery. Int. J. Radiat. Oncol. 2012, 83, 467–474. [Google Scholar] [CrossRef]
- Mancosu, P.; Reggiori, G.; Gaudino, A.; Lobefalo, F.; Paganini, L.; Palumbo, V.; Stravato, A.; Tomatis, S.; Scorsetti, M. Are pitch and roll compensations required in all pathologies? A data analysis of 2945 fractions. Br. J. Radiol. 2015, 88, 20150468. [Google Scholar] [CrossRef] [PubMed]
- Offersen, B.V.; Boersma, L.J.; Kirkove, C.; Hol, S.; Aznar, M.C.; Sola, A.B.; Kirova, Y.M.; Pignol, J.-P.; Remouchamps, V.; Verhoeven, K.; et al. ESTRO consensus guideline on target volume delineation for elective radiation therapy of early stage breast cancer. Radiother. Oncol. 2015, 114, 3–10. [Google Scholar] [CrossRef]
- Offersen, B.V.; Boersma, L.J.; Kirkove, C.; Hol, S.; Aznar, M.C.; Sola, A.B.; Kirova, Y.M.; Pignol, J.-P.; Remouchamps, V.; Verhoeven, K.; et al. ESTRO consensus guideline on target volume delineation for elective radiation therapy of early stage breast cancer, version 1.1. Radiother. Oncol. 2016, 118, 205–208. [Google Scholar] [CrossRef] [PubMed]
- Noël, G.; Antoni, D.; Barillot, I.; Chauvet, B. Délinéation des organes à risque et contraintes dosimétriques. Cancer/Radiothérapie 2016, 20, S36–S60. [Google Scholar] [CrossRef] [PubMed]
- Ung, M.; Rouyar-Nicolas, A.; Limkin, E.; Petit, C.; Sarrade, T.; Carre, A.; Auzac, G.; Lombard, A.; Ullman, E.; Bonnet, N.; et al. Improving Radiotherapy Workflow Through Implementation of Delineation Guidelines & AI-Based Annotation. Int. J. Radiat. Oncol. 2020, 108, e315. [Google Scholar] [CrossRef]
- Jiang, P.; Liu, Z.; Jiang, W.; Qu, A.; Sun, H.; Wang, J. Detection of setup errors with a body-surface laser-scanning system for whole-breast irradiation after breast-conserving surgery. J. Appl. Clin. Med. Phys. 2022, 23, e13578. [Google Scholar] [CrossRef]
- Alderliesten, T.; Hollander, S.D.; Yang, T.-I.J.; Elkhuizen, P.H.; van Mourik, A.M.; Hurkmans, C.; Remeijer, P.; van Vliet-Vroegindeweij, C. Dosimetric impact of post-operative seroma reduction during radiotherapy after breast-conserving surgery. Radiother. Oncol. 2011, 100, 265–270. [Google Scholar] [CrossRef]
- Zegers, C.M.L.; Baeza, J.A.; Van Elmpt, W.; Murrer, L.H.P.; Verhoeven, K.; Boersma, L.; Verhaegen, F.; Nijsten, S.M.J.J.G. Three-dimensional dose evaluation in breast cancer patients to define decision criteria for adaptive radiotherapy. Acta Oncol. 2017, 56, 1487–1494. [Google Scholar] [CrossRef]
- Gleeson, I. Comparing the robustness of different skin flash approaches using wide tangents, manual flash VMAT, and simulated organ motion robust optimization VMAT in breast and nodal radiotherapy. Med. Dosim. 2022, 47, 264–272. [Google Scholar] [CrossRef]
- Struikmans, H.; Wárlám-Rodenhuis, C.; Stam, T.; Stapper, G.; Tersteeg, R.J.; Bol, G.H.; Raaijmakers, C.P. Interobserver variability of clinical target volume delineation of glandular breast tissue and of boost volume in tangential breast irradiation. Radiother. Oncol. 2005, 76, 293–299. [Google Scholar] [CrossRef]
- Song, Y.-C.; Yan, X.-N.; Tang, Y.; Jing, H.; Zhang, N.; Zhang, J.; Zhong, Y.-H.; Dong, L.-H.; Wu, H.-F.; Tie, J.; et al. Variability of Target Volumes and Organs at Risk Delineation in Breast Cancer Radiation Therapy: Quality Assurance Results of the Pretrial Benchmark Case for the POTENTIAL Trial. Pract. Radiat. Oncol. 2022, 12, 397–408. [Google Scholar] [CrossRef] [PubMed]
- Oh, K.S.; Kong, F.-M.; Griffith, K.A.; Yanke, B.; Pierce, L.J. Planning the breast tumor bed boost: Changes in the excision cavity volume and surgical scar location after breast-conserving surgery and whole-breast irradiation. Int. J. Radiat. Oncol. 2006, 66, 680–686. [Google Scholar] [CrossRef] [PubMed]
- Prendergast, B.; Indelicato, D.J.; Grobmyer, S.R.; Saito, A.I.; Lightsey, J.L.; Snead, F.E.; Morris, C.G.; Copeland, E.M.; Mendenhall, N.P. The Dynamic Tumor Bed: Volumetric Changes in the Lumpectomy Cavity During Breast-Conserving Therapy. Int. J. Radiat. Oncol. 2009, 74, 695–701. [Google Scholar] [CrossRef] [PubMed]
- Giacometti, V.; King, R.B.; Agnew, C.E.; Irvine, D.M.; Jain, S.; Hounsell, A.R.; McGarry, C.K. An evaluation of techniques for dose calculation on cone beam computed tomography. Br. J. Radiol. 2019, 92, 20180383. [Google Scholar] [CrossRef]


| Patient | Laterality | Type | CTV Breast/Chest Wall Volume (cc) |
|---|---|---|---|
| 1 | Right | Conserving surgery | 802.5 |
| 2 | Right | Conserving surgery | 489.7 |
| 3 | Right | Conserving surgery | 904.6 |
| 4 | Right | Conserving surgery | 501.2 |
| 5 | Right | Conserving surgery | 381.5 |
| 6 | Left | Conserving surgery | 575.0 |
| 7 | Left | Conserving surgery | 754.2 |
| 8 | Left | Conserving surgery | 692.5 |
| 9 | Left | Conserving surgery | 870.3 |
| 10 | Left | Conserving surgery | 475.4 |
| 11 | Right | Mastectomy | 415.9 |
| 12 | Right | Mastectomy | 274.0 |
| 13 | Right | Mastectomy | 527.8 |
| 14 | Right | Mastectomy | 250.3 |
| 15 | Right | Mastectomy | 516.1 |
| 16 | Left | Mastectomy | 384.5 |
| 17 | Left | Mastectomy | 237.6 |
| 18 | Left | Mastectomy | 368.5 |
| 19 | Left | Mastectomy | 621.1 |
| 20 | Left | Mastectomy | 623.6 |
| Breast | Chest Wall | |||
|---|---|---|---|---|
| CTV Breast | V95% (%) | Initial | 99.07 ± 0.15 | 99.06 ± 0.17 |
| 6-DOF | 99.26 ± 0.75 | 99.17 ± 0.61 | ||
| 3-DOF | 99.17 ± 1.00 | 99.28 ± 0.53 | ||
| V110% (%) | Initial | 27.53 ± 13.10 | 0.10 ± 0.13 | |
| 6-DOF | 30.07 ± 13.85 | 1.71 ± 4.37 | ||
| 3-DOF | 30.49 ± 14.26 | 2.15 ± 5.47 | ||
| CTV_IMC | V95% (%) | Initial | 100 ± 0.00 | 100 ± 0.00 |
| 6-DOF | 99.27 ± 1.08 | 99.35 ± 0.65 | ||
| 3-DOF | 99.06 ± 1.39 | 99.11 ± 1.03 | ||
| V110% (%) | Initial | 0 ± 0.00 | 0.11 ± 0.27 | |
| 6-DOF | 0.56 ± 1.12 | 0.28 ± 0.40 | ||
| 3-DOF | 0.39 ± 0.59 | 0.59 ± 1.48 | ||
| CTV_Nodes | V95% (%) | Initial | 100 ± 0.00 | 100 ± 0.00 |
| 6-DOF | 99.37 ± 0.61 | 99.43 ± 0.56 | ||
| 3-DOF | 99.54 ± 0.55 | 99.21 ± 0.88 | ||
| V110% (%) | Initial | 6 ± 13.50 | 2.79 ± 6.67 | |
| 6-DOF | 9.40 ± 24.23 | 6.16 ± 8.98 | ||
| 3-DOF | 9.24 ± 23.54 | 5.79 ± 8.34 | ||
| Heart | Dmean (Gy) | Initial | 7.58 ± 1.05 | 7.65 ± 1.22 |
| 6-DOF | 7.51 ± 1.15 | 7.92 ± 1.48 | ||
| 3-DOF | 7.58 ± 1.09 | 7.84 ± 1.20 | ||
| Ipsi_Lung | Dmean (Gy) | Initial | 12.47 ± 1.31 | 12.54 ± 1.06 |
| 6-DOF | 12.76 ± 1.23 | 12.79 ± 1.27 | ||
| 3-DOF | 12.71 ± 1.48 | 12.83 ± 1.17 | ||
| D10% (Gy) | Initial | 28.75 ± 3.03 | 31.18 ± 2.23 | |
| 6-DOF | 29.50 ± 2.72 | 31.59 ± 2.41 | ||
| 3-DOF | 29.31 ± 3.80 | 31.79 ± 2.93 | ||
| D20% (Gy) | Initial | 17.94 ± 2.37 | 18.77 ± 1.93 | |
| 6-DOF | 18.16 ± 1.92 | 18.82 ± 2.17 | ||
| 3-DOF | 18.07 ± 2.55 | 19.03 ± 2.32 | ||
| D80% (Gy) | Initial | 5.17 ± 1.03 | 4.43 ± 0.95 | |
| 6-DOF | 5.23 ± 1.03 | 4.55 ± 1.00 | ||
| 3-DOF | 5.21 ± 1.05 | 4.55 ± 0.98 | ||
| Contra_lung | Dmean (Gy) | Initial | 5.00 ± 0.57 | 5.04 ± 0.37 |
| 6-DOF | 5.09 ± 0.57 | 5.23 ± 0.43 | ||
| 3-DOF | 5.06 ± 0.61 | 5.12 ± 0.41 |
| Initial vs. 6-DOF | Initial vs. 3-DOF | 6-DOF vs. 3-DOF | ||
|---|---|---|---|---|
| CTV Breast/Chest wall | V95% | 0.326 | 0.381 | 0.951 |
| V110% | 0.014 | 0.015 | 0.071 | |
| CTV_Nodes | V95% | 0.0002 | 0.013 | 0.925 |
| V110% | 0.126 | 0.150 | 0.274 | |
| CTV_IMC | V95% | 0.003 | 0.004 | 0.400 |
| V110% | 0.067 | 0.052 | 0.801 | |
| Heart | Dmean | 0.363 | 0.284 | 0.955 |
| Ipsi_lung | Dmean | 0.052 | 0.148 | 0.972 |
| D10% | 0.193 | 0.383 | 0.996 | |
| D20% | 0.678 | 0.640 | 0.839 | |
| D80% | 0.011 | 0.034 | 0.284 | |
| Contra_lung | Dmean | 0.053 | 0.094 | 0.240 |
Disclaimer/Publisher’s Note: The statements, opinions and data contained in all publications are solely those of the individual author(s) and contributor(s) and not of MDPI and/or the editor(s). MDPI and/or the editor(s) disclaim responsibility for any injury to people or property resulting from any ideas, methods, instructions or products referred to in the content. |
© 2023 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Prunaretty, J.; Mir, N.; Tilhac, A.; Gouillou, M.; Azria, D.; Fenoglietto, P.; Bourgier, C. Robustness of Breast Margins with Volumetric Modulated Arc Therapy without a Six-Degrees-of-Freedom Couch: A Dosimetric Evaluation. J. Clin. Med. 2023, 12, 862. https://doi.org/10.3390/jcm12030862
Prunaretty J, Mir N, Tilhac A, Gouillou M, Azria D, Fenoglietto P, Bourgier C. Robustness of Breast Margins with Volumetric Modulated Arc Therapy without a Six-Degrees-of-Freedom Couch: A Dosimetric Evaluation. Journal of Clinical Medicine. 2023; 12(3):862. https://doi.org/10.3390/jcm12030862
Chicago/Turabian StylePrunaretty, Jessica, Nicolas Mir, Anaïs Tilhac, Maureen Gouillou, David Azria, Pascal Fenoglietto, and Céline Bourgier. 2023. "Robustness of Breast Margins with Volumetric Modulated Arc Therapy without a Six-Degrees-of-Freedom Couch: A Dosimetric Evaluation" Journal of Clinical Medicine 12, no. 3: 862. https://doi.org/10.3390/jcm12030862
APA StylePrunaretty, J., Mir, N., Tilhac, A., Gouillou, M., Azria, D., Fenoglietto, P., & Bourgier, C. (2023). Robustness of Breast Margins with Volumetric Modulated Arc Therapy without a Six-Degrees-of-Freedom Couch: A Dosimetric Evaluation. Journal of Clinical Medicine, 12(3), 862. https://doi.org/10.3390/jcm12030862





