Maxillary Antral Pseudocyst Drift after Osteotome Sinus Floor Elevation with Simultaneous Implant Placement: A Case Report and Literature Review
Abstract
1. Introduction
2. Case Report
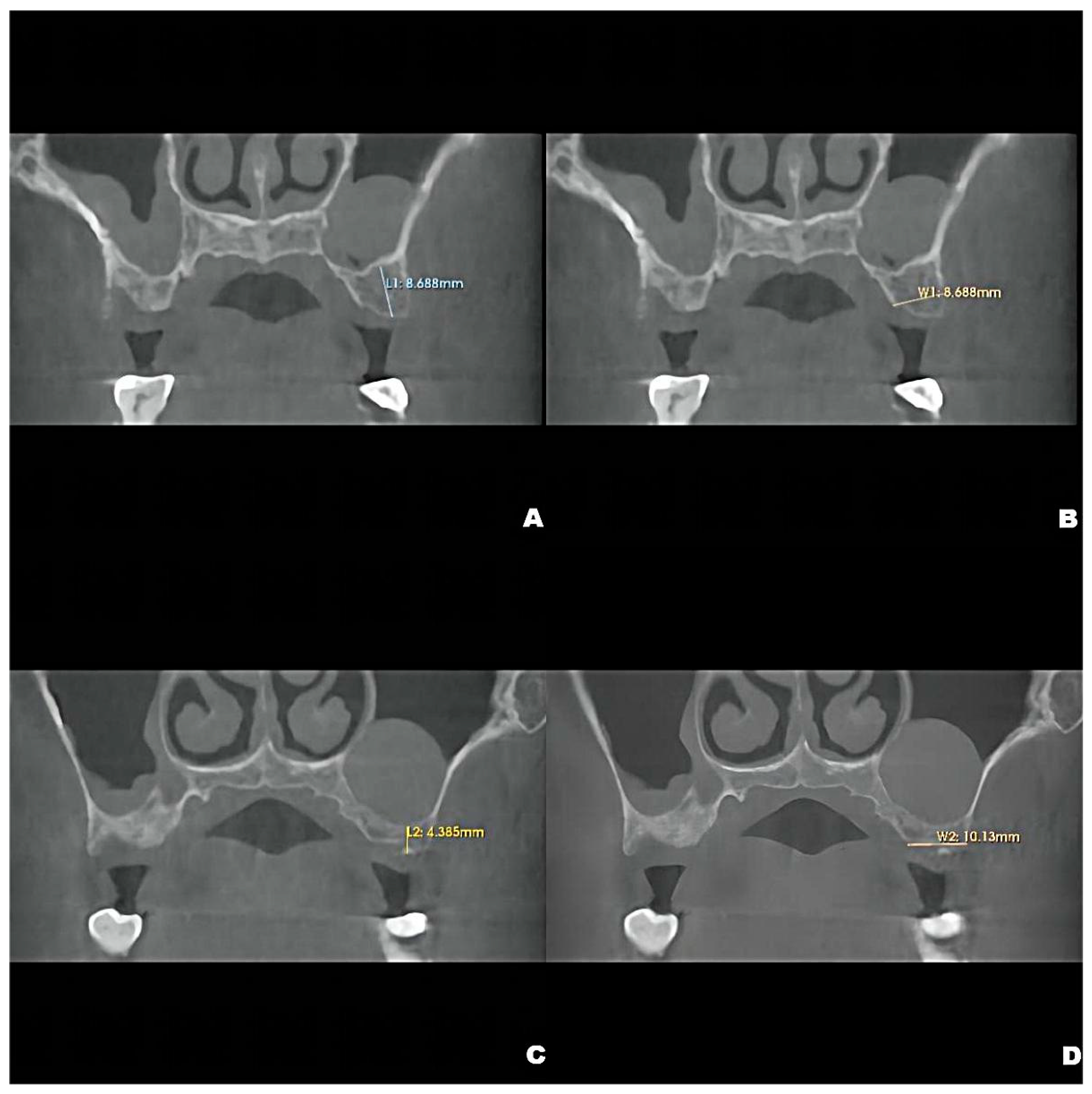
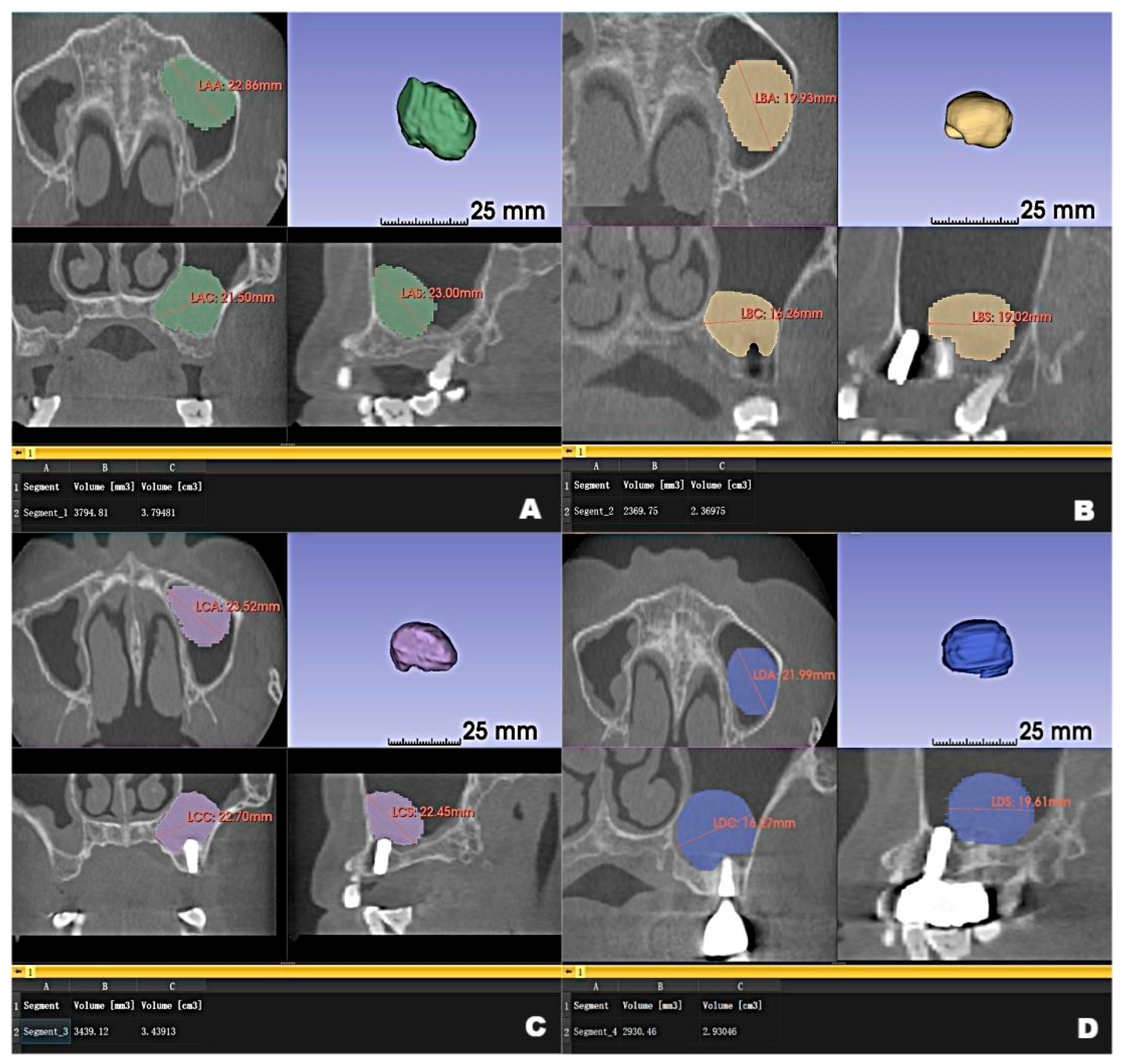
2.1. Preoperative Examinations
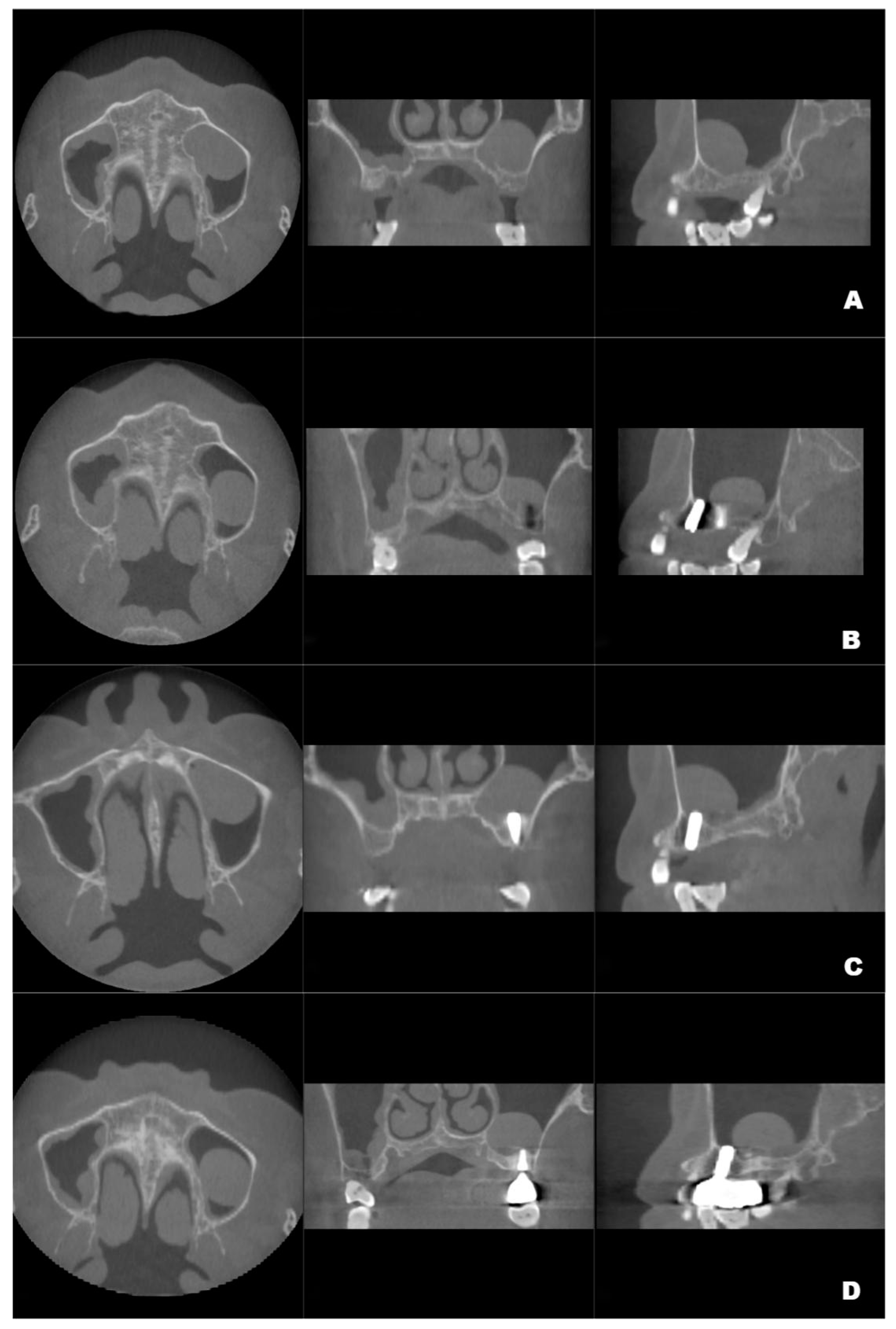
2.2. Surgical Procedures and Postoperative Management
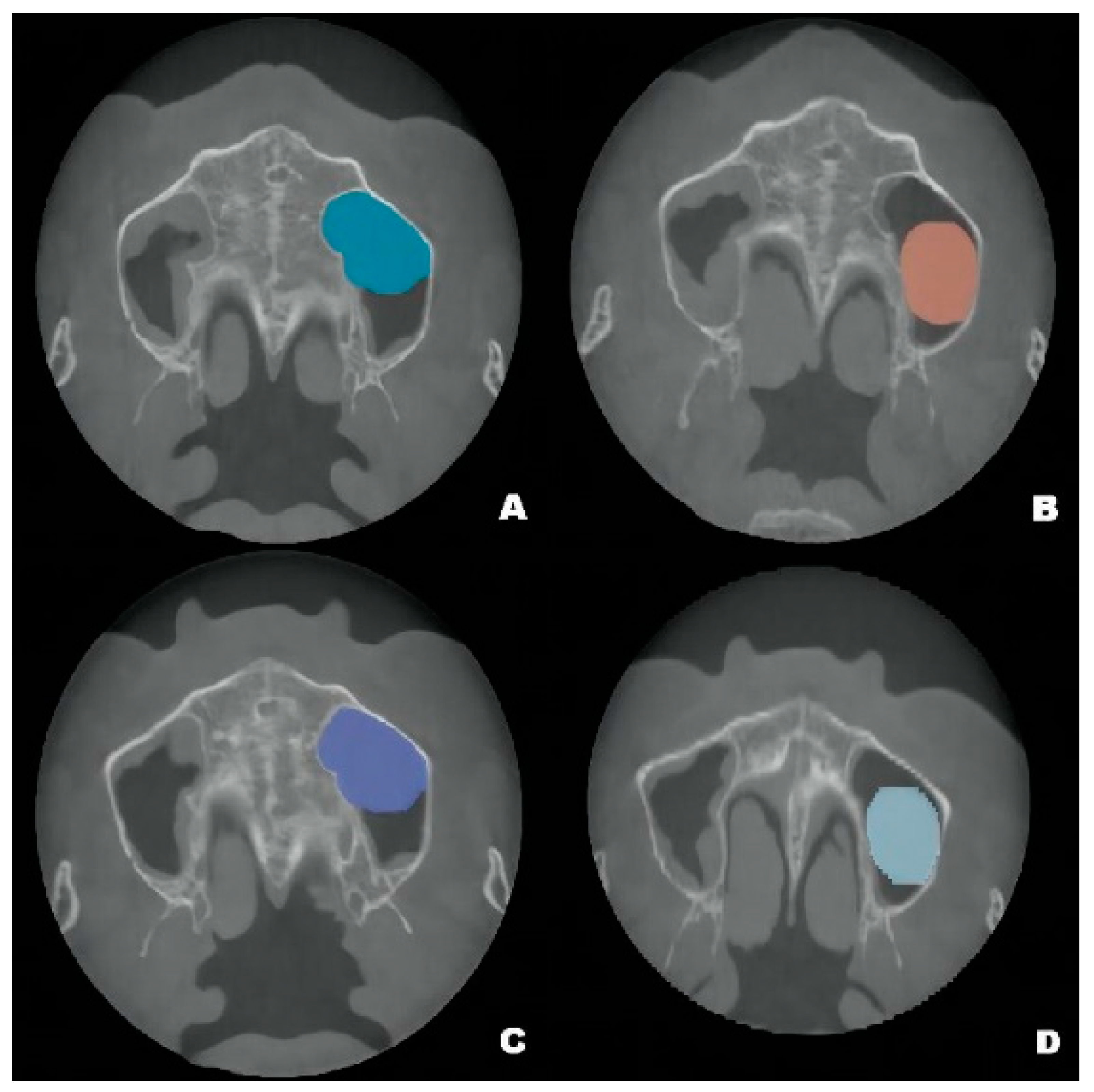
2.3. Postoperative Examinations
3. Discussion
4. Conclusions
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Acknowledgments
Conflicts of Interest
References
- Lana, J.P.; Carneiro, P.M.; Machado Vde, C.; de Souza, P.E.; Manzi, F.R.; Horta, M.C. Anatomic variations and lesions of the maxillary sinus detected in cone beam computed tomography for dental implants. Clin. Oral. Implants Res. 2012, 23, 1398–1403. [Google Scholar] [CrossRef] [PubMed]
- Xuran, W.; Yu, Z.; Ping, D.; Xi, J.; Ye, L. Anatomic variations and lesions of the maxillary sinus observed by CBCT before sinus augmentation in 666 sinuses of 589 patients. J. Pract. Stomatol. 2019, 35, 100–104. [Google Scholar]
- Kara, I.M.; Küçük, D.; Polat, S. Experience of maxillary sinus floor augmentation in the presence of antral pseudocysts. J. Oral. Maxillofac. Surg. 2010, 68, 1646–1650. [Google Scholar] [CrossRef] [PubMed]
- Carmeli, G.; Artzi, Z.; Kozlovsky, A.; Segev, Y.; Landsberg, R. Antral computerized tomography pre-operative evaluation: Relationship between mucosal thickening and maxillary sinus function. Clin. Oral. Implants Res. 2011, 22, 78–82. [Google Scholar] [CrossRef] [PubMed]
- Gong, T.; Hu, C.; Chen, Y.; Zhou, N.; Wu, H.; Man, Y. Raising the transcrestal sinus floor in the presence of antral pseudocysts, and in sinus floors with a normal Schneiderian membrane: A retrospective cohort study. Br. J. Oral. Maxillofac. Surg. 2019, 57, 466–472. [Google Scholar] [CrossRef]
- Anitua, E.; Alkhraisat, M.H.; Torre, A.; Eguia, A. Are mucous retention cysts and pseudocysts in the maxillary sinus a risk factor for dental implants? A systematic review. Med. Oral. Patol. Oral. Cir. Bucal. 2021, 26, e276–e283. [Google Scholar] [CrossRef]
- Beaumont, C.; Zafiropoulos, G.G.; Rohmann, K.; Tatakis, D.N. Prevalence of maxillary sinus disease and abnormalities in patients scheduled for sinus lift procedures. J. Periodontol. 2005, 76, 461–467. [Google Scholar] [CrossRef]
- Yu, H.; Qiu, L. Histological and clinical outcomes of lateral sinus floor elevation with simultaneous removal of a maxillary sinus pseudocyst. Clin. Implant. Dent. Relat. Res. 2019, 21, 94–100. [Google Scholar] [CrossRef]
- Mardinger, O.; Manor, I.; Mijiritsky, E.; Hirshberg, A. Maxillary sinus augmentation in the presence of antral pseudocyst: A clinical approach. Oral. Surg. Oral. Med. Oral. Pathol. Oral. Radiol. Endod. 2007, 103, 180–184. [Google Scholar] [CrossRef]
- Celebi, N.; Gonen, Z.B.; Kilic, E.; Etoz, O.; Alkan, A. Maxillary sinus floor augmentation in patients with maxillary sinus pseudocyst: Case report. Oral. Surg. Oral. Med. Oral. Pathol. Oral. Radiol. Endod. 2011, 112, e97–e102. [Google Scholar] [CrossRef]
- Gardner, D.G. Pseudocysts and retention cysts of the maxillary sinus. Oral. Surg. Oral. Med. Oral. Pathol. 1984, 58, 561–567. [Google Scholar] [CrossRef]
- Bhattacharyya, N. Do maxillary sinus retention cysts reflect obstructive sinus phenomena? Arch. Otolaryngol. Head Neck Surg. 2000, 126, 1369–1371. [Google Scholar] [CrossRef]
- Wang, J.H.; Jang, Y.J.; Lee, B.J. Natural course of retention cysts of the maxillary sinus: Long-term follow-up results. Laryngoscope 2007, 117, 341–344. [Google Scholar] [CrossRef] [PubMed]
- Liu, D.; Shi, L.; Dai, X.; Zhou, Q.; Yang, F.; Shen, M.; Yu, Y.; Wu, Y. Implants placed simultaneously with maxillary sinus floor augmentation in the presence of antral pseudocysts: Presentation of a case series. Quintessence Int. 2018, 49, 479–485. [Google Scholar] [PubMed]
- Giotakis, E.I.; Weber, R.K. Cysts of the maxillary sinus: A literature review. Int. Forum. Allergy Rhinol. 2013, 3, 766–771. [Google Scholar] [CrossRef] [PubMed]
- Tang, Z.H.; Wu, M.J.; Xu, W.H. Implants placed simultaneously with maxillary sinus floor augmentations in the presence of antral pseudocysts: A case report. Int. J. Oral. Maxillofac. Surg. 2011, 40, 998–1001. [Google Scholar] [CrossRef] [PubMed]
- Summers, R.B. A new concept in maxillary implant surgery: The osteotome technique. Compendium 1994, 15, 152, 154–156, 158 passim; quiz 162. [Google Scholar] [PubMed]
- Liu, H.; Liu, R.; Wang, M.; Yang, J. Immediate implant placement combined with maxillary sinus floor elevation utilizing the transalveolar approach and nonsubmerged healing for failing teeth in the maxillary molar area: A randomized controlled trial clinical study with one-year follow-up. Clin. Implant Dent. Relat. Res. 2019, 21, 462–472. [Google Scholar] [CrossRef]
- Fedorov, A.; Beichel, R.; Kalpathy-Cramer, J.; Finet, J.; Fillion-Robin, J.C.; Pujol, S.; Bauer, C.; Jennings, D.; Fennessy, F.; Sonka, M.; et al. 3D Slicer as an image computing platform for the Quantitative Imaging Network. Magn. Reson Imaging 2012, 30, 1323–1341. [Google Scholar] [CrossRef]
- Skoulakis, C.E.; Velegrakis, G.A.; Doxas, P.G.; Papadakis, C.E.; Bizakis, J.G.; Helidonis, E.S. Mucocele of the maxillary antrum in an eight-year-old boy. Int. J. Pediatr. Otorhinolaryngol. 1999, 47, 283–287. [Google Scholar] [CrossRef]
- Fu, M.; Jiang, Z.; Ren, L.; He, J.; Zhu, D.; Yang, G. Maxillary sinus floor augmentation comparing removing versus retaining antral pseudocyst: A retrospective cohort study. Clin. Oral. Implants Res. 2022, 33, 1098–1113. [Google Scholar] [CrossRef]
- Hu, Y.K.; Yang, C.; Qian, W.T. Endoscopic-Assisted Sinus Floor Augmentation Combined With Removal of an Antral Pseudocyst of the Ipsilateral Maxillary Sinus. J. Craniofac. Surg. 2017, 28, 1549–1551. [Google Scholar] [CrossRef]
- Oh, J.H.; An, X.; Jeong, S.M.; Choi, B.H. Crestal Sinus Augmentation in the Presence of an Antral Pseudocyst. Implant Dent. 2017, 26, 951–955. [Google Scholar] [CrossRef] [PubMed]
- Chiapasco, M.; Palombo, D. Sinus grafting and simultaneous removal of large antral pseudocysts of the maxillary sinus with a micro-invasive intraoral access. Int. J. Oral. Maxillofac. Surg. 2015, 44, 1499–1505. [Google Scholar] [CrossRef]
- Feng, Y.; Tang, Y.; Liu, Y.; Chen, F.; Li, D. Maxillary sinus floor elevation using the osteotome technique in the presence of antral pseudocysts: A retrospective study with an average follow-up of 27 months. Int. J. Oral. Maxillofac. Implants 2014, 29, 408–413. [Google Scholar] [CrossRef] [PubMed]
- Acocella, A.; Bertolai, R.; Nissan, J.; Ellis, E., 3rd; Sacco, R. Maxillary sinus lift using fresh frozen bone chips in presence of sinus cyst: Clinical and histological report. Cell Tissue Bank 2012, 13, 327–332. [Google Scholar] [CrossRef] [PubMed]
- Cortes, A.R.; Corrêa, L.; Arita, E.S. Evaluation of a maxillary sinus floor augmentation in the presence of a large antral pseudocyst. J. Craniofac. Surg. 2012, 23, e535–e537. [Google Scholar] [CrossRef]
- Kara, M.I.; Kirmali, O.; Ay, S. Clinical evaluation of lateral and osteotome techniques for sinus floor elevation in the presence of an antral pseudocyst. Int. J. Oral. Maxillofac. Implants 2012, 27, 1205–1210. [Google Scholar]
- Lin, Y.; Hu, X.; Metzmacher, A.R.; Luo, H.; Heberer, S.; Nelson, K. Maxillary sinus augmentation following removal of a maxillary sinus pseudocyst after a shortened healing period. J. Oral. Maxillofac. Surg. 2010, 68, 2856–2860. [Google Scholar] [CrossRef]
- Wang, M.; Yan, M.; Xia, H.; Zhao, Y. Sinus Elevation Through Transcrestal Window Approach and Delayed Implant Placement in 1- to 2-mm Residual Alveolar Bone: A Case Report. Implant Dent. 2016, 25, 866–869. [Google Scholar] [CrossRef]
| NO | Author (Year) | Number of Cases | Surgical Method of Maxillary Antral Floor Elevation | Management of Antral Pseudocysts | Implant Timing | Follow-Up | Outcome |
|---|---|---|---|---|---|---|---|
| 1 | Fu et al. [21] (2022) | 26 | LSFE | Removed in 13 cases | 1-Stage | 12-month, ~2 to 5 years | Failure in 1 case at 12 months, with higher bone graft volumetric stability after 6–12 months. |
| Preserved in 13 cases | 1-Stage | Failure in 2 cases at 12 months and 2~5-years follow-up, respectively. | |||||
| 2 | Gong et al. [5] | 17 | CSFE | Preserved | 1-Stage | 4–6 months | Osseointegration in all cases. |
| 3 | (2019) Yu and Qiu [8] (2019) | 15 | LSFE | Preserved | 1-Stage | 6 months | Failure in 1 implant before loading. |
| 4 | Liu et al. [14] (2018) | 14 | LSFE | Cystic fluid extraction | 1-Stage | 12 months | Osseointegration in all cases. |
| 5 | Hu et al. [22] (2017) | 1 | Endoscopic-Assisted LSFE | Removed | 2-Stage | 12 months | Osseointegration |
| 6 | Oh et al. [23] (2017) | 2 | CSFE | Cystic fluid extraction | 1-Stage | 6 months | Osseointegration in all cases. |
| 7 | Chiapasco and Palombo [24] (2015) | 12 | LSFE | Removed | 1-Stage in 7 cases | 12–96 months | Osseointegration in all cases. |
| 2-Stage in 5 cases | |||||||
| 8 | Feng et al. [25] (2014) | 21 | OSFE | Preserved | 1-Stage | Average of 27 months | Osseointegration in all cases. |
| 9 | Acocella et al. [26] (2012) | 1 | LSFE | Removed | 2-Stage | 2 years | Osseointegration |
| 10 | Cortes et al. [27] (2012) | 1 | LSFE | Removed | 1-Stage | 12 months | Osseointegration |
| 11 | Kara et al. [28] (2012) | 29 | LSFE in 17 cases | Preserved | 1-Stage | Average of 17 months | Osseointegration in all cases. |
| OSFE in 12 cases | 2-Stage | ||||||
| 12 | Celebi et al. [10] (2011) | 4 | LSFE in 2 cases | Preserved | 1-Stage | 6–8 months | Osseointegration in all cases. |
| CSFE in 2 cases | 2-Stage | ||||||
| 13 | Tang et al. [16] (2011) | 1 | LSFE | Preserved | 1-Stage | 12 months | Osseointegration |
| 14 | Lin et al. [29] (2010) | 11 | LSFE | Removed | 2-Stage | Average of 29.2 months after prosthetic loading | Osseointegration |
| 15 | Kara et al. [3] (2010) | 2 | LSFE in 1 case | Preserved | 2-Stage | 16 months | Osseointegration in all cases. |
| CSFE in 1 case | 13 months | ||||||
| 16 | Mardinger et al. [9] (2007) | 8 | LSFE | Preserved | 1-Stage in 7 cases | Average of 20 months | Osseointegration in all cases. |
| 2-Stage in 1 case |
Disclaimer/Publisher’s Note: The statements, opinions and data contained in all publications are solely those of the individual author(s) and contributor(s) and not of MDPI and/or the editor(s). MDPI and/or the editor(s) disclaim responsibility for any injury to people or property resulting from any ideas, methods, instructions or products referred to in the content. |
© 2023 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Wang, P.; Huang, N.; Ren, J.; Gong, P.; Long, J.; Huang, B. Maxillary Antral Pseudocyst Drift after Osteotome Sinus Floor Elevation with Simultaneous Implant Placement: A Case Report and Literature Review. J. Clin. Med. 2023, 12, 920. https://doi.org/10.3390/jcm12030920
Wang P, Huang N, Ren J, Gong P, Long J, Huang B. Maxillary Antral Pseudocyst Drift after Osteotome Sinus Floor Elevation with Simultaneous Implant Placement: A Case Report and Literature Review. Journal of Clinical Medicine. 2023; 12(3):920. https://doi.org/10.3390/jcm12030920
Chicago/Turabian StyleWang, Peihan, Nan Huang, Jiayin Ren, Ping Gong, Jie Long, and Bo Huang. 2023. "Maxillary Antral Pseudocyst Drift after Osteotome Sinus Floor Elevation with Simultaneous Implant Placement: A Case Report and Literature Review" Journal of Clinical Medicine 12, no. 3: 920. https://doi.org/10.3390/jcm12030920
APA StyleWang, P., Huang, N., Ren, J., Gong, P., Long, J., & Huang, B. (2023). Maxillary Antral Pseudocyst Drift after Osteotome Sinus Floor Elevation with Simultaneous Implant Placement: A Case Report and Literature Review. Journal of Clinical Medicine, 12(3), 920. https://doi.org/10.3390/jcm12030920





