Urinary Continence Recovery after Robotic Radical Prostatectomy without Anterior or Posterior Reconstruction: Experience from a Tertiary Referral Center
Abstract
:1. Introduction
2. Materials and Methods
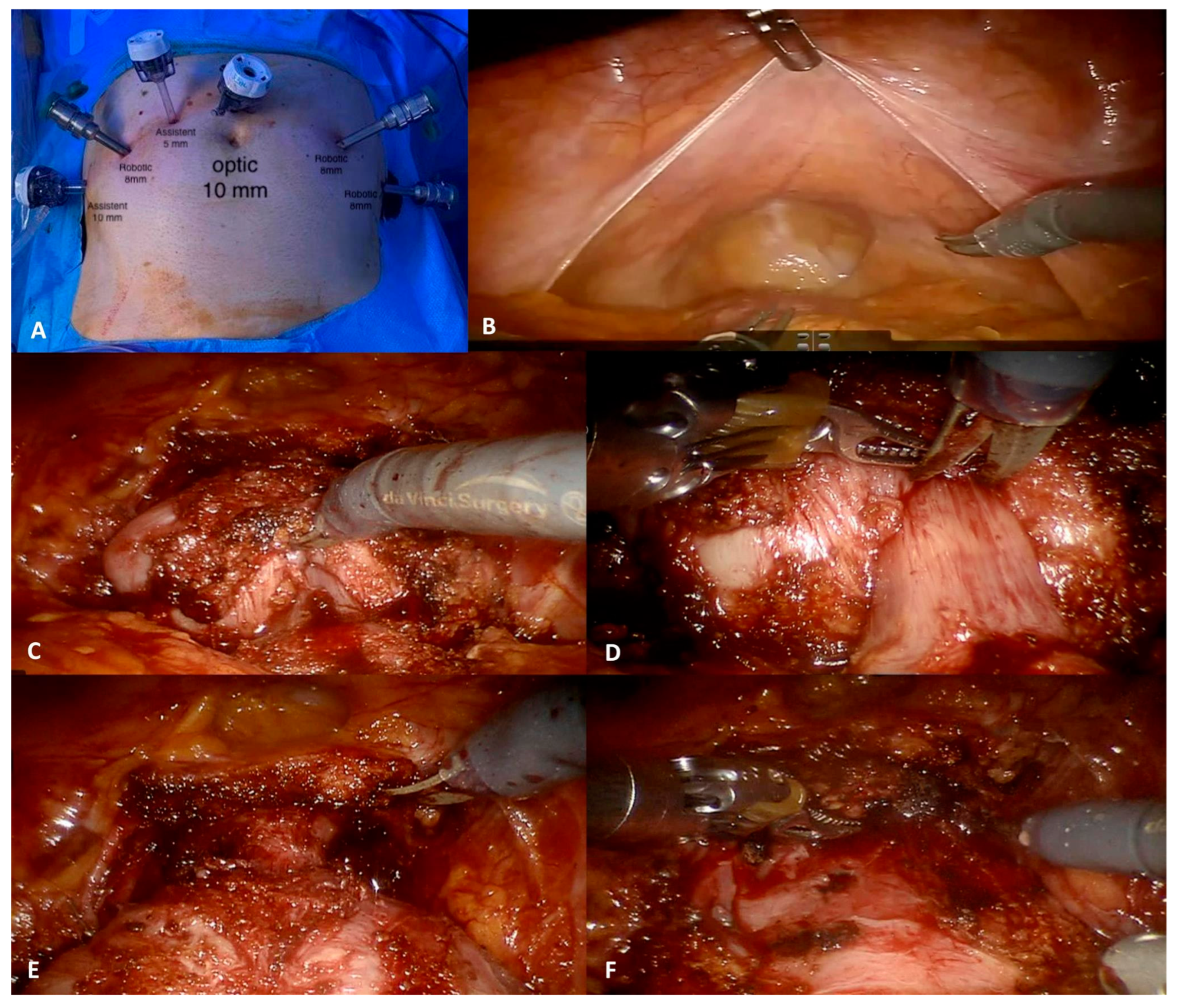
2.1. Surgical Technique: Nuances for Urinary Continence Recovery
2.2. Dataset and Perioperative Protocol
2.3. Outcome Measure
2.4. Statistical Analysis
3. Results
4. Discussion
5. Conclusions
Supplementary Materials
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Conflicts of Interest
References
- Bill-Axelson, A.; Holmberg, L.; Ruutu, M.; Häggman, M.; Andersson, S.-O.; Bratell, S.; Spångberg, A.; Busch, C.; Nordling, S.; Garmo, H.; et al. Radical Prostatectomy versus Watchful Waiting in Early Prostate Cancer. N. Engl. J. Med. 2005, 352, 1977–1984. [Google Scholar] [CrossRef] [PubMed]
- Novara, G.; Ficarra, V.; Mocellin, S.; Ahlering, T.E.; Carroll, P.R.; Graefen, M.; Guazzoni, G.; Menon, M.; Patel, V.R.; Shariat, S.F.; et al. Systematic Review and Meta-analysis of Studies Reporting Oncologic Outcome After Robot-assisted Radical Prostatectomy. Eur. Urol. 2012, 62, 382–404. [Google Scholar] [CrossRef] [PubMed]
- Ficarra, V.; Novara, G.; Rosen, R.C.; Artibani, W.; Carroll, P.R.; Costello, A.; Menon, M.; Montorsi, F.; Patel, V.R.; Stolzenburg, J.-U.; et al. Systematic Review and Meta-analysis of Studies Reporting Urinary Continence Recovery After Robot-assisted Radical Prostatectomy. Eur. Urol. 2012, 62, 405–417. [Google Scholar] [CrossRef] [PubMed]
- Bianchi, L.; Gandaglia, G.; Fossati, N.; Larcher, A.; Pultrone, C.; Turri, F.; Selli, C.; De Groote, R.; De Naeyer, G.; Borghesi, M.; et al. Oncologic outcomes in prostate cancer patients treated with robot-assisted radical prostatectomy: Results from a single institution series with more than 10 years follow up. Minerva Urol. Nefrol. 2019, 71, 38–46. [Google Scholar] [CrossRef]
- Walsh, P.C. Anatomic radical prostatectomy: Evolution of the surgical technique. J. Urol. 1998, 160 (6 Pt 2), 2418–2424. [Google Scholar] [CrossRef]
- Patel, V.R.; Palmer, K.J.; Coughlin, G.; Samavedi, S. Robot-Assisted Laparoscopic Radical Prostatectomy: Perioperative Outcomes of 1500 Cases. J. Endourol. 2008, 22, 2299–2306. [Google Scholar] [CrossRef]
- Hung, S.-C.; Ou, Y.-C.; Cheng, C.-L.; Hung, S.-W.; Ho, H.-C.; Chiu, K.-Y.; Wang, S.-S.; Chen, C.-S.; Li, J.-R.; Yang, C.-K. Standardized procedure of robotic assisted laparoscopic radical prostatectomy from case 1 to case 1200. Urol. Sci. 2016, 27, 199–207. [Google Scholar] [CrossRef]
- Sanda, M.G.; Dunn, R.L.; Michalski, J.; Sandler, H.M.; Northouse, L.; Hembroff, L.; Lin, X.; Greenfield, T.K.; Litwin, M.S.; Saigal, C.S.; et al. Quality of Life and Satisfaction with Outcome among Prostate-Cancer Survivors. N. Engl. J. Med. 2008, 358, 1250–1261. [Google Scholar] [CrossRef]
- Marchioni, M.; Primiceri, G.; Castellan, P.; Schips, L.; Mantica, G.; Chapple, C.; Papalia, R.; Porpiglia, F.; Scarpa, R.M.; Esperto, F. Conservative management of urinary incontinence following robot-assisted radical prostatectomy. Minerva Urol. Nephrol. 2020, 72, 555–562. [Google Scholar] [CrossRef]
- Holze, S.; Mende, M.; Healy, K.V.; Koehler, N.; Gansera, L.; Truss, M.C.; Rebmann, U.; Degener, S.; Stolzenburg, J.-U. Comparison of various continence definitions in a large group of patients undergoing radical prostatectomy: A multicentre, prospective study. BMC Urol. 2019, 19, 70. [Google Scholar] [CrossRef]
- Marzi, V.L.; Morselli, S.; Fusco, F.; Baldesi, R.; Campi, R.; Liaci, A.; Gemma, L.; Morelli, G.; Serni, S. Advance Xp® Male Sling can be an Effective and Safe Treatment for Post-Prostatectomy Stress Urinary Incontinence Also in Patients with Prior History of External Beam Radiation Therapy: A Multicentric Experience. Surg. Innov. 2021, 28, 723–730. [Google Scholar] [CrossRef] [PubMed]
- Ahlering, T.E.; Gordon, A.; Morales, B.; Skarecky, D.W. Preserving Continence During Robotic Prostatectomy. Curr. Urol. Rep. 2013, 14, 52–58. [Google Scholar] [CrossRef] [PubMed]
- Chung, J.W.; Kim, S.W.; Kang, H.W.; Ha, Y.S.; Choi, S.H.; Lee, J.N.; Kim, B.S.; Kim, H.T.; Kim, T.H.; Yoon, G.S.; et al. Efficacy of modified radical prostatectomy technique for recovery of urinary incontinence in high-grade prostate cancer. Minerva Urol. Nefrol. 2020, 72, 605–614. [Google Scholar] [CrossRef]
- Vis, A.N.; van der Poel, H.G.; Ruiter, A.E.; Hu, J.C.; Tewari, A.K.; Rocco, B.; Patel, V.R.; Razdan, S.; Nieuwenhuijzen, J.A. Posterior, Anterior, and Periurethral Surgical Reconstruction of Urinary Continence Mechanisms in Robot-assisted Radical Prostatectomy: A Description and Video Compilation of Commonly Performed Surgical Techniques. Eur. Urol. 2019, 76, 814–822. [Google Scholar] [CrossRef] [PubMed]
- Friedlander, D.; Alemozaffar, M.; Hevelone, N.; Lipsitz, S.R.; Hu, J.C. Stepwise Description and Outcomes of Bladder Neck Sparing During Robot-Assisted Laparoscopic Radical Prostatectomy. J. Urol. 2012, 188, 1754–1760. [Google Scholar] [CrossRef] [PubMed]
- Student, V.; Vidlar, A.; Grepl, M.; Hartmann, I.; Buresova, E. Advanced Reconstruction of Vesicourethral Support (ARVUS) during Robot-assisted Radical Prostatectomy: One-year Functional Outcomes in a Two-group Randomised Controlled Trial. Eur. Urol. 2017, 71, 822–830. [Google Scholar] [CrossRef]
- Patel, V.R.; Coelho, R.F.; Palmer, K.J.; Rocco, B. Periurethral Suspension Stitch During Robot-Assisted Laparoscopic Radical Prostatectomy: Description of the Technique and Continence Outcomes. Eur. Urol. 2009, 56, 472–478. [Google Scholar] [CrossRef]
- Porpiglia, F.; Bertolo, R.; Manfredi, M.; De Luca, S.; Checcucci, E.; Morra, I.; Passera, R.; Fiori, C. Total Anatomical Reconstruction During Robot-assisted Radical Prostatectomy: Implications on Early Recovery of Urinary Continence. Eur. Urol. 2016, 69, 485–495. [Google Scholar] [CrossRef]
- Hamada, A.; Razdan, S.; Etafy, M.H.; Fagin, R.; Razdan, S. Early Return of Continence in Patients Undergoing Robot-Assisted Laparoscopic Prostatectomy Using Modified Maximal Urethral Length Preservation Technique. J. Endourol. 2014, 28, 930–938. [Google Scholar] [CrossRef]
- Schlomm, T.; Heinzer, H.; Steuber, T.; Salomon, G.; Engel, O.; Michl, U.; Haese, A.; Graefen, M.; Huland, H. Full Functional-Length Urethral Sphincter Preservation During Radical Prostatectomy. Eur. Urol. 2011, 60, 320–329. [Google Scholar] [CrossRef]
- Mungovan, S.F.; Sandhu, J.S.; Akin, O.; Smart, N.A.; Graham, P.L.; Patel, M.I. Preoperative Membranous Urethral Length Measurement and Continence Recovery Following Radical Prostatectomy: A Systematic Review and Meta-analysis. Eur. Urol. 2017, 71, 368–378. [Google Scholar] [CrossRef] [PubMed]
- Mattei, A.; Naspro, R.; Annino, F.; Burke, D.; Guida, R.; Gaston, R. Tension and Energy-Free Robotic-Assisted Laparoscopic Radical Prostatectomy with Interfascial Dissection of the Neurovascular Bundles. Eur. Urol. 2007, 52, 687–695. [Google Scholar] [CrossRef] [PubMed]
- Kowalczyk, K.J.; Huang, A.C.; Hevelone, N.D.; Lipsitz, S.R.; Yu, H.-Y.; Ulmer, W.D.; Kaplan, J.R.; Patel, S.; Nguyen, P.L.; Hu, J.C. Stepwise Approach for Nerve Sparing Without Countertraction During Robot-Assisted Radical Prostatectomy: Technique and Outcomes. Eur. Urol. 2011, 60, 536–547. [Google Scholar] [CrossRef] [PubMed]
- Hurtes, X.; Rouprêt, M.; Vaessen, C.; Pereira, H.; D’Arcier, B.F.; Cormier, L.; Bruyère, F. Anterior suspension combined with posterior reconstruction during robot-assisted laparoscopic prostatectomy improves early return of urinary continence: A prospective randomized multicentre trial. BJU Int. 2012, 110, 875–883. [Google Scholar] [CrossRef]
- Gautam, G.; Rocco, B.; Patel, V.R.; Zorn, K.C. Posterior Rhabdosphincter Reconstruction During Robot-assisted Radical Prostatectomy: Critical Analysis of Techniques and Outcomes. Urology 2010, 76, 734–741. [Google Scholar] [CrossRef]
- Joshi, N.; de Blok, W.; van Muilekom, E.; van der Poel, H. Impact of Posterior Musculofascial Reconstruction on Early Continence After Robot-Assisted Laparoscopic Radical Prostatectomy: Results of a Prospective Parallel Group Trial. Eur. Urol. 2010, 58, 84–89. [Google Scholar] [CrossRef]
- Coelho, R.F.; Chauhan, S.; Orvieto, M.A.; Sivaraman, A.; Palmer, K.J.; Coughlin, G.; Patel, V.R. Influence of Modified Posterior Reconstruction of the Rhabdosphincter on Early Recovery of Continence and Anastomotic Leakage Rates after Robot-Assisted Radical Prostatectomy. Eur. Urol. 2011, 59, 72–80, Erratum in: Eur. Urol. 2018. [Google Scholar] [CrossRef]
- Rocco, B.; Gregori, A.; Stener, S.; Santoro, L.; Bozzola, A.; Galli, S.; Knez, R.; Scieri, F.; Scaburri, A.; Gaboardi, F. Posterior Reconstruction of the Rhabdosphincter Allows a Rapid Recovery of Continence after Transperitoneal Videolaparoscopic Radical Prostatectomy. Eur. Urol. 2007, 51, 996–1003. [Google Scholar] [CrossRef]
- Grasso, A.A.; Mistretta, F.A.; Sandri, M.; Cozzi, G.; de Lorenzis, E.; Rosso, M.; Albo, G.; Palmisano, F.; Mottrie, A.; Haese, A.; et al. Posterior musculofascial reconstruction after radical prostatectomy: An updated systematic review and a meta-analysis. BJU Int. 2016, 118, 20–34. [Google Scholar] [CrossRef]
- Checcucci, E.; Pecoraro, A.; Manfredi, M.; Amparore, D.; Aimar, R.; Piramide, F.; Granato, S.; Volpi, G.; Autorino, R.; Fiori, C.; et al. The importance of anatomical reconstruction for continence recovery after robot assisted radical prostatectomy: A systematic review and pooled analysis from referral centers. Minerva Urol. Nephrol. 2021, 73, 165–177. [Google Scholar] [CrossRef]
- Schifano, N.; Capogrosso, P.; Tutolo, M.; Dehò, F.; Montorsi, F.; Salonia, A. How to Prevent and Manage Post-Prostatectomy Incontinence: A Review. World J. Men’s Health 2021, 39, 581. [Google Scholar] [CrossRef] [PubMed]
- Pasticier, G.; Rietbergen, J.B.; Guillonneau, B.; Fromont, G.; Menon, M.; Vallancien, G. Robotically Assisted Laparoscopic Radical Prostatectomy: Feasibility Study in Men. Eur. Urol. 2001, 40, 70–74. [Google Scholar] [CrossRef] [PubMed]
- Hernandez, D.J.; Nielsen, M.E.; Han, M.; Partin, A.W. Contemporary Evaluation of the D’Amico Risk Classification of Prostate Cancer. Urology 2007, 70, 931–935. [Google Scholar] [CrossRef] [PubMed]
- Mazzone, E.; Gandaglia, G.; Ploussard, G.; Marra, G.; Valerio, M.; Campi, R.; Mari, A.; Minervini, A.; Serni, S.; Moschini, M.; et al. Risk Stratification of Patients Candidate to Radical Prostatectomy Based on Clinical and Multiparametric Magnetic Resonance Imaging Parameters: Development and External Validation of Novel Risk Groups. Eur. Urol. 2022, 81, 193–203. [Google Scholar] [CrossRef] [PubMed]
- Milsom, I.; Irwin, D.E. A Cross-Sectional, Population-Based, Multinational Study of the Prevalence of Overactive Bladder and Lower Urinary Tract Symptoms: Results from the EPIC Study. Eur. Urol. Suppl. 2007, 6, 4–9. [Google Scholar] [CrossRef]
- Abrams, P.; Constable, L.D.; Cooper, D.; MacLennan, G.; Drake, M.J.; Harding, C.; Mundy, A.; McCormack, K.; McDonald, A.; Norrie, J.; et al. Outcomes of a Noninferiority Randomised Controlled Trial of Surgery for Men with Urodynamic Stress Incontinence After Prostate Surgery (MASTER). Eur. Urol. 2021, 79, 812–823. [Google Scholar] [CrossRef]
- Dindo, D.; Demartines, N.; Clavien, P.-A. Classification of Surgical Complications: A new proposal with evaluation in a cohort of 6336 patients and results of a survey. Ann. Surg. 2004, 240, 205–213. [Google Scholar] [CrossRef]
- Zorn, K.C.; Tholomier, C.; Bienz, M.; Hueber, P.-A.; Trinh, Q.D.; El-Hakim, A.; Alhathal, N.; Lebeau, T.; Benayoun, S.; Valdivieso, R.; et al. Oncological and functional outcomes of 722 robot-assisted radical prostatectomy (RARP) cases: The largest Canadian 5-year experience. Can. Urol. Assoc. J. 2014, 8, 195–201, Erratum in Can. Urol. Assoc. J. 2015, 9, E760. [Google Scholar] [CrossRef]
- Cindolo, L.; Antonelli, A.; Sandri, M.; Annino, F.; Celia, A.; De Concilio, B.; Giommoni, V.; Nucciotti, R.; Sessa, F.; Porreca, A.; et al. The role of vascular clamping during robot-assisted partial nephrectomy for localized renal cancer: Rationale and design of the CLOCK randomized phase III study. Minerva Urol. Nefrol. 2019, 71, 96–100. [Google Scholar] [CrossRef]
- Ploussard, G. Robotic surgery in urology: Facts and reality. What are the real advantages of robotic approaches for prostate cancer patients? Curr. Opin. Urol. 2018, 28, 153–158. [Google Scholar] [CrossRef]
- Tewari, A.; Srivasatava, A.; Menon, M. MEMBERS OF THE VIP TEAM A prospective comparison of radical retropubic and robot-assisted prostatectomy: Experience in one institution. BJU Int. 2003, 92, 205–210. [Google Scholar] [CrossRef] [PubMed]
- Ficarra, V.; Novara, G.; Fracalanza, S.; D’Elia, C.; Secco, S.; Iafrate, M.; Cavalleri, S.; Artibani, W. A prospective, non-randomized trial comparing robot-assisted laparoscopic and retropubic radical prostatectomy in one European institution. BJU Int. 2009, 104, 534–539. [Google Scholar] [CrossRef] [PubMed]
- Rocco, B.; Matei, D.-V.; Melegari, S.; Ospina, J.C.; Mazzoleni, F.; Errico, G.; Mastropasqua, M.; Santoro, L.; Detti, S.; DE Cobelli, O. Robotic vs open prostatectomy in a laparoscopically naive centre: A matched-pair analysis. BJU Int. 2009, 104, 991–995. [Google Scholar] [CrossRef] [PubMed]
- Walz, J.; Epstein, J.I.; Ganzer, R.; Graefen, M.; Guazzoni, G.; Kaouk, J.; Menon, M.; Mottrie, A.; Myers, R.P.; Patel, V.; et al. A Critical Analysis of the Current Knowledge of Surgical Anatomy of the Prostate Related to Optimisation of Cancer Control and Preservation of Continence and Erection in Candidates for Radical Prostatectomy: An Update. Eur. Urol. 2016, 70, 301–311. [Google Scholar] [CrossRef]
- Sammon, J.; Kim, T.-K.; Trinh, Q.-D.; Bhandari, A.; Kaul, S.; Sukumar, S.; Rogers, C.G.; Peabody, J.O. Anastomosis During Robot-assisted Radical Prostatectomy: Randomized Controlled Trial Comparing Barbed and Standard Monofilament Suture. Urology 2011, 78, 572–579. [Google Scholar] [CrossRef]
- Vora, A.A.; Dajani, D.; Lynch, J.H.; Kowalczyk, K.J. Anatomic and technical considerations for optimizing recovery of urinary function during robotic-assisted radical prostatectomy. Curr. Opin. Urol. 2013, 23, 78–87. [Google Scholar] [CrossRef]
- Mottrie, A.; Gallina, A.; De Wil, P.; Thüer, D.; Novara, G.; Ficarra, V. Balancing continence function and oncological outcomes during robot-assisted radical prostatectomy (RARP). BJU Int. 2011, 108 Pt 2, 999–1006. [Google Scholar] [CrossRef]
- You, Y.C.; Kim, T.H.; Sung, G.T. Effect of Bladder Neck Preservation and Posterior Urethral Reconstruction during Robot-Assisted Laparoscopic Radical Prostatectomy for Urinary Continence. Korean J. Urol. 2012, 53, 29–33. [Google Scholar] [CrossRef]
- Freire, M.P.; Weinberg, A.C.; Lei, Y.; Soukup, J.R.; Lipsitz, S.R.; Prasad, S.M.; Korkes, F.; Lin, T.; Hu, J.C. Anatomic Bladder Neck Preservation During Robotic-Assisted Laparoscopic Radical Prostatectomy: Description of Technique and Outcomes. Eur. Urol. 2009, 56, 972–980. [Google Scholar] [CrossRef]
- Rocco, F.; Carmignani, L.; Acquati, P.; Gadda, F.; Dell’Orto, P.; Rocco, B.; Casellato, S.; Gazzano, G.; Consonni, D. Early Continence Recovery after Open Radical Prostatectomy with Restoration of the Posterior Aspect of the Rhabdosphincter. Eur. Urol. 2007, 52, 376–383. [Google Scholar] [CrossRef]
- Tewari, A.; Jhaveri, J.; Rao, S.; Yadav, R.; Bartsch, G.; Te, A.; Ioffe, E.; Pineda, M.; Mudaliar, S.; Nguyen, L.; et al. Total reconstruction of the vesico-urethral junction. BJU Int. 2008, 101, 871–877. [Google Scholar] [CrossRef] [PubMed]
- Patel, V.R.; Thaly, R.; Shah, K. Robotic radical prostatectomy: Outcomes of 500 cases. BJU Int. 2007, 99, 1109–1112. [Google Scholar] [CrossRef] [PubMed]
- Sutherland, D.E.; Linder, B.; Guzman, A.M.; Hong, M.; Frazier, H.A.; Engel, J.D.; Bianco, F.J. Posterior Rhabdosphincter Reconstruction During Robotic Assisted Radical Prostatectomy: Results From a Phase II Randomized Clinical Trial. J. Urol. 2011, 185, 1262–1267. [Google Scholar] [CrossRef]
- Ogawa, S.; Hoshi, S.; Koguchi, T.; Hata, J.; Sato, Y.; Akaihata, H.; Kataoka, M.; Haga, N.; Kojima, Y. Three-Layer Two-Step Posterior Reconstruction Using Peritoneum During Robot-Assisted Radical Prostatectomy to Improve Recovery of Urinary Continence: A Prospective Comparative Study. J. Endourol. 2017, 31, 1251–1257. [Google Scholar] [CrossRef] [PubMed]
- Menon, M.; Muhletaler, F.; Campos-Sánchez, M.; Peabody, J.O. Assessment of Early Continence After Reconstruction of the Periprostatic Tissues in Patients Undergoing Computer Assisted (Robotic) Prostatectomy: Results of a 2 Group Parallel Randomized Controlled Trial. J. Urol. 2008, 180, 1018–1023. [Google Scholar] [CrossRef] [PubMed]
- Sammon, J.D.; Muhletaler, F.; Peabody, J.O.; Diaz-Insua, M.; Satyanaryana, R.; Menon, M. Long-term Functional Urinary Outcomes Comparing Single- vs Double-layer Urethrovesical Anastomosis: Two-year Follow-up of a Two-group Parallel Randomized Controlled Trial. Urology 2010, 76, 1102–1107. [Google Scholar] [CrossRef] [PubMed]
- Koliakos, N.; Mottrie, A.; Buffi, N.; De Naeyer, G.; Willemsen, P.; Fonteyne, E. Posterior and anterior fixation of the urethra during robotic prostatectomy improves early continence rates. Scand. J. Urol. Nephrol. 2010, 44, 5–10. [Google Scholar] [CrossRef]
| Variables | n = 925 |
|---|---|
| Patient’s characteristics | |
| Age at diagnosis, yrs, median (IQR) | 68 (63–72) |
| BMI at surgery, kg/m2, median (IQR) | 26 (24.0–28.0) |
| Charlson Comorbidity Index (CCI) | 1 (0–2) |
| Cardiovascular disease n (%) | 244 (26.4) |
| Diabetes mellitus, n (%) | 80 (8.6) |
| Anticoagulant/antiaggregant, n (%) | 226 (24.4) |
| Family history of prostate cancer, n (%) | 80 (8.6) |
| Preoperative urinary incontinence (UI) *, n (%) | 145 (15.7) |
| Preoperative ED, n (%) | 145(15.7) |
| Positive DRE, n (%) | 473 (51.1) |
| PSA value at diagnosis, ng/mL, median (IQR) | 6.8 (4.7–9.7) |
| Preoperative MRI, n (%) | 518 (56) |
| Prostate volume, cc, median ° (IQR) | 45 (34.0–54.0) |
| Characteristics at biopsy | |
| Type of biopsy, n (%) | |
| Systematic biopsy | 520 (56.2) |
| Cognitive biopsy | 51 (5.5) |
| MRI-targeted biopsy | 349 (37.7) |
| Incidental prostate cancer following TURP. | 5 (0.5) |
| Highest ISUP Grade Group at random ç biopsy cores, n (%) | |
| Patients with no positive random biopsy cores | 114 (12.3) |
| Grade Group 1 | 187 (20.2) |
| Grade Group 2 | 284 (30.7) |
| Grade Group 3 | 183 (19.8) |
| Grade Group 4 | 102 (11) |
| Grade Group 5 | 55 (5.9) |
| Extra-capsular invasion at biopsy, n (%) | 16 (1.7) |
| Seminal vesicle invasion at biopsy, n (%) | 8 (0.9) |
| Perineural invasion at biopsy (PNI), n (%) | 237 (25.6) |
| Characteristics at imaging | |
| Preoperative staging | 751 (81.1) |
| Extra-capsular extension at imaging, n (%) | 50 (6.5) |
| Seminal vesicle invasion at imaging, n (%) | 23 (3.0) |
| cT, n (%) | |
| T1 | 424 (45.8) |
| T2 | 467 (50.5) |
| T3–4 | 34 (3.7) |
| cN+, n (%) | 64 (6.9) |
| Localized disease § | 839 (90.7) |
| EAU class risk stratification, n (%) | |
| Low-risk disease | 117 (12.6) |
| Intermediate-risk disease | 438 (47.3) |
| High-risk disease | 289 (31.2) |
| Locally advanced disease | 81 (8.7) |
| Variables | n = 925 |
|---|---|
| Surgical features | |
| Nerve-sparing RALP, n (%) | 572 (61.8) |
| Monolateral nerve-sparing RALP n (%) | 353 (38.2) |
| Bilateral nerve-sparing RALP n (%) | 237 (25.6) |
| Pelvic lymph node dissection during (LND) RALP, n (%) | 487 (52.6) |
| Patient with locally advanced disease undergoing nerve-sparing RALP, n (%) | 24 (2.6) |
| Patients with high-risk or locally advanced EAU disease underging pelvic lymph node dissection, n (%) | 299 (32.3) |
| Histopathologic features | |
| Definitive histology findings, n (%) | |
| Acinar adenocarcinoma | 876 (94.7) |
| Intraductal carcinoma | 5 (0.5) |
| Mixed | 14 (1.5) |
| Others (sarcomatoid, squamous and adenosquamous) | 30 (3.2) |
| Clinically significant positive surgical margin (PSM), more than 2 mm, n (%) | 72 (7.8) |
| Highest ISUP grade group post-RP histopathologic assessment, n (%) ° | |
| Grade Group 1 | 81 (8.9) |
| Grade Group 2 | 400 (43.8) |
| Grade Group 3 | 182 (19.9) |
| Grade Group 4 | 154 (16.8) |
| Grade Group 5 | 97 (10.6) |
| Gleason Score (GS) at definitive post-RP histopathologic assessment, n (%) | |
| GS 6 (3 + 3) | 81 (8.9) |
| GS 7 (3 + 4 and 4 + 3) | 619 (67.7) |
| GS 8 (4 + 4 and 5 + 3 and 3 + 5) | 129 (14.1) |
| GS 9 (4 + 5 and 5 + 4) | 85 (9.3) |
| Perineural invasion (IPN) at at definitive post-RP histopathologic assessment, n (%) | 428 (46.3) |
| pT, n (%) | |
| T2 | 349 (37.8) |
| T3 | 574(62.0) |
| T4 | 2 (0.2) |
| pN, n (%) | |
| Nx | 438 (47.4) |
| N0 | 381 (41.2) |
| N1 | 106 (11.5) |
| pM, n (%) °° | |
| Mx | 882 (95.4) |
| M0 | 40 (4.3) |
| M1 (extraregional LND) | 3 (0.3) |
| Variables | n = 925 |
|---|---|
| Follow-up | |
| Duration of f-up, months, median (IQR) | 17 (11-27) |
| Biochemical recurrence (BCR)at last follow-up | 63 (6.8) |
| -Of patients with BCR: | |
| -adjuvant radiotherapy (in 10 cases concomitant ormonotherapy) | 27 (42) |
| -salvage radiotherapy | 8 (12) |
| -systemic ormonotherapy | 9 (14) |
| Early (30 day) continence rate, n (%) * | |
| Fully continent, no pad/die | 766 (82.8) |
| 1 or more pads/dies | 159 (17.2) |
| Patients with moderate/severe incontinence within 30 days | |
| 2 pads/dies | 125 (78.6) |
| 3 pads/dies | 26 (16.4) |
| >3 pads/dies | 8 (5) |
| Continence at last follow-up days, n (%) | |
| Fully continent, no pad/die | 885 (95.5) |
| 1 or more pads/dies | 40 (5.5) |
| Patients with moderate/severe incontinence after 30 days | |
| 2 pads/dies | 25 (62.5) |
| 3 pads/dies | 14 (35) |
| >3 pads/dies | 1 (2.5) |
| Clavien–Dindo (CD) > 2 (within 30 days), n (%) | |
| CD IIIa (10 cases requiring percutaneous drainage for symptomatic lymphocele and 5 requiring endoscopic catheter positioning for mdc spread) | 15 (1.6) |
| CD IIIb (1 case clot retention requiring endoscopic evacuation and 1 case requiring re-intervention for uretrovesical anastomosis) | 2 (0.2) |
| CD IV (1 case of post-operative cerebrovascular ischemia requiring neurovascular thrombolysis) | 1 (0.1) |
| Claviend Dindo (CD) > 2 after 30 days), n (%) | |
| CD IIIa (13 cases requiring percutaneous drainage for symptomatic lymphocele, 5 percutaneous drainages for abdominal abscessus) | 18 (1.9) |
| CD IIIb (13 endoscopic urethrotomy for endoscopic stricture, 4 paraumbilical haernia requiring surgical repair, 1 re-operation for bladder repair, 1 case requiring re-intervention for uretrovesical anastomosis and 1 case requiring endoscopic surgery for clip removal) | 20 (2.1) |
| CD IV (1 case of acute abdomen for bowel strangulation) | 1 (0.1) |
| Multivariate Logistic Regressions for all Patients (n = 925) | ||||
|---|---|---|---|---|
| Variables | OR | p | 95% Confidence Interval | |
| Inferior | Superior | |||
| Cardiovascular disease (absent vs. present at diagnosis) | 0.463 | <0.01 | 0.321 | 0.667 |
| Pelvic lymph node dissection during RALP | 1.337 | 0.187 | 0.868 | 2.058 |
| Nerve-sparing (vs. radical) RALP | 1.522 | 0.045 | 1.007 | 2.300 |
| EAU low-risk disease referent | - | - | - | - |
| EAU intermediate-risk disease | 0.967 | 0.941 | 0.401 | 2.330 |
| EAU high-risk disease | 1.183 | 0.632 | 0.596 | 2.347 |
| EAU locally advanced disease | 1.189 | 0.618 | 0.602 | 2.347 |
Disclaimer/Publisher’s Note: The statements, opinions and data contained in all publications are solely those of the individual author(s) and contributor(s) and not of MDPI and/or the editor(s). MDPI and/or the editor(s) disclaim responsibility for any injury to people or property resulting from any ideas, methods, instructions or products referred to in the content. |
© 2023 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Sessa, F.; Nicoletti, R.; Pecoraro, A.; Polverino, P.; Rivetti, A.; Conte, F.L.; Lo Re, M.; Belmonte, M.; Alberti, A.; Dibilio, E.; et al. Urinary Continence Recovery after Robotic Radical Prostatectomy without Anterior or Posterior Reconstruction: Experience from a Tertiary Referral Center. J. Clin. Med. 2023, 12, 1358. https://doi.org/10.3390/jcm12041358
Sessa F, Nicoletti R, Pecoraro A, Polverino P, Rivetti A, Conte FL, Lo Re M, Belmonte M, Alberti A, Dibilio E, et al. Urinary Continence Recovery after Robotic Radical Prostatectomy without Anterior or Posterior Reconstruction: Experience from a Tertiary Referral Center. Journal of Clinical Medicine. 2023; 12(4):1358. https://doi.org/10.3390/jcm12041358
Chicago/Turabian StyleSessa, Francesco, Rossella Nicoletti, Alessio Pecoraro, Paolo Polverino, Anna Rivetti, Francesco Lupo Conte, Mattia Lo Re, Mario Belmonte, Andrea Alberti, Edoardo Dibilio, and et al. 2023. "Urinary Continence Recovery after Robotic Radical Prostatectomy without Anterior or Posterior Reconstruction: Experience from a Tertiary Referral Center" Journal of Clinical Medicine 12, no. 4: 1358. https://doi.org/10.3390/jcm12041358
APA StyleSessa, F., Nicoletti, R., Pecoraro, A., Polverino, P., Rivetti, A., Conte, F. L., Lo Re, M., Belmonte, M., Alberti, A., Dibilio, E., Gallo, M. L., Manera, A., Gacci, M., Sebastianelli, A., Vignolini, G., Serni, S., Campi, R., & Li Marzi, V. (2023). Urinary Continence Recovery after Robotic Radical Prostatectomy without Anterior or Posterior Reconstruction: Experience from a Tertiary Referral Center. Journal of Clinical Medicine, 12(4), 1358. https://doi.org/10.3390/jcm12041358








