Challenges in ARDS Definition, Management, and Identification of Effective Personalized Therapies
Abstract
1. Introduction
2. Evolution of the Definition of ARDS
3. Supportive Therapies
3.1. Tidal Volume
3.2. Positive End-Expiratory Pressure and Alveolar Recruitment
3.3. Driving Pressure and Plateau Pressure
3.4. Slower Is Better
3.5. Mechanical Power
3.6. Other Modes of Ventilation
3.7. Prone Positioning
3.8. Extracorporeal Membrane Oxygenation and Extracorporeal Carbon Dioxide Removal
3.9. Fluid Management
4. Pharmacologic Therapies for ARDS
4.1. Neuromuscular Blocking Agents
4.2. Corticosteroids
4.3. Aspirin
4.4. Interferons
4.5. Vitamins
4.6. Statins
4.7. N-Acetylcysteine
4.8. β-Agonists
4.9. Sivelestat
4.10. Vasodilators
4.11. Surfactants
4.12. Solnatide
4.13. Dilmapimod
4.14. Keratinocyte Growth Factor and Granulocyte-Macrophage Colony Stimulating Factor
4.15. Nebulized Heparin
4.16. Mesenchymal Stem Cells and Multipotent Progenitor Cells
5. Why Do Pharmacotherapies Fail in ARDS? The Importance of Personalized Medicine
6. Future Directions
7. Conclusions
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Conflicts of Interest
References
- Bellani, G.; Laffey, J.G.; Pham, T.; Fan, E.; Brochard, L.; Esteban, A.; Gattinoni, L.; van Haren, F.; Larsson, A.; McAuley, D.F.; et al. Epidemiology, Patterns of Care, and Mortality for Patients with Acute Respiratory Distress Syndrome in Intensive Care Units in 50 Countries. JAMA 2016, 315, 788. [Google Scholar] [CrossRef] [PubMed]
- Rubenfeld, G.D.; Caldwell, E.; Peabody, E.; Weaver, J.; Martin, D.P.; Neff, M.; Stern, E.J.; Hudson, L.D. Incidence and Outcomes of Acute Lung Injury. N. Engl. J. Med. 2005, 353, 1685–1693. [Google Scholar] [CrossRef] [PubMed]
- Bellani, G.; Pham, T.; Laffey, J.G. Missed or Delayed Diagnosis of ARDS: A Common and Serious Problem. Intensive Care Med. 2020, 46, 1180–1183. [Google Scholar] [CrossRef] [PubMed]
- Thille, A.W.; Peñuelas, O.; Lorente, J.A.; Fernández-Segoviano, P.; Rodriguez, J.-M.; Aramburu, J.-A.; Panizo, J.; Esteban, A.; Frutos-Vivar, F. Predictors of Diffuse Alveolar Damage in Patients with Acute Respiratory Distress Syndrome: A Retrospective Analysis of Clinical Autopsies. Crit. Care 2017, 21, 254. [Google Scholar] [CrossRef]
- Ashbaugh, D.G.; Boyd Bigelow, D.; Petty, T.L.; Levine, B.E. Acute Respiratory Distress in Adults. Lancet 1967, 290, 319–323. [Google Scholar] [CrossRef]
- Ranieri, V.; Rubenfeld, G.; Thompson, B.; Ferguson, N.; Caldwell, E.; Fan, E.; Camporota, L.; Slutsky, A. Acute Respiratory Distress Syndrome: The Berlin Definition. JAMA 2012, 307, 2526–2533. [Google Scholar] [CrossRef]
- Thille, A.W.; Esteban, A.; Fernández-Segoviano, P.; Rodriguez, J.-M.; Aramburu, J.-A.; Peñuelas, O.; Cortés-Puch, I.; Cardinal-Fernández, P.; Lorente, J.A.; Frutos-Vivar, F. Comparison of the Berlin Definition for Acute Respiratory Distress Syndrome with Autopsy. Am. J. Respir. Crit. Care Med. 2013, 187, 761–767. [Google Scholar] [CrossRef]
- García-de-Acilu, M.; Marin-Corral, J.; Vázquez, A.; Ruano, L.; Magret, M.; Ferrer, R.; Masclans, J.R.; Roca, O. Hypoxemic Patients With Bilateral Infiltrates Treated With High-Flow Nasal Cannula Present a Similar Pattern of Biomarkers of Inflammation and Injury to Acute Respiratory Distress Syndrome Patients*. Crit. Care Med. 2017, 45, 1845–1853. [Google Scholar] [CrossRef]
- Coudroy, R.; Frat, J.-P.; Boissier, F.; Contou, D.; Robert, R.; Thille, A.W. Early Identification of Acute Respiratory Distress Syndrome in the Absence of Positive Pressure Ventilation. Crit. Care Med. 2018, 46, 540–546. [Google Scholar] [CrossRef]
- Villar, J.; Fernández, R.L.; Ambrós, A.; Parra, L.; Blanco, J.; Domínguez-Berrot, A.M.; Gutiérrez, J.M.; Blanch, L.; Añón, J.M.; Martín, C.; et al. A Clinical Classification of the Acute Respiratory Distress Syndrome for Predicting Outcome and Guiding Medical Therapy*. Crit. Care Med. 2015, 43, 346–353. [Google Scholar] [CrossRef]
- Caironi, P.; Carlesso, E.; Cressoni, M.; Chiumello, D.; Moerer, O.; Chiurazzi, C.; Brioni, M.; Bottino, N.; Lazzerini, M.; Bugedo, G.; et al. Lung Recruitability Is Better Estimated According to the Berlin Definition of Acute Respiratory Distress Syndrome at Standard 5 Cm H2O Rather Than Higher Positive End-Expiratory Pressure. Crit. Care Med. 2015, 43, 781–790. [Google Scholar] [CrossRef]
- Riviello, E.D.; Kiviri, W.; Twagirumugabe, T.; Mueller, A.; Banner-Goodspeed, V.M.; Officer, L.; Novack, V.; Mutumwinka, M.; Talmor, D.S.; Fowler, R.A. Hospital Incidence and Outcomes of the Acute Respiratory Distress Syndrome Using the Kigali Modification of the Berlin Definition. Am. J. Respir. Crit. Care Med. 2016, 193, 52–59. [Google Scholar] [CrossRef]
- Kwizera, A.; Nakibuuka, J.; Nakiyingi, L.; Sendagire, C.; Tumukunde, J.; Katabira, C.; Ssenyonga, R.; Kiwanuka, N.; Kateete, D.P.; Joloba, M.; et al. Acute Hypoxaemic Respiratory Failure in a Low-Income Country: A Prospective Observational Study of Hospital Prevalence and Mortality. BMJ Open Respir. Res. 2020, 7, e000719. [Google Scholar] [CrossRef]
- Matthay, M.A.; Zemans, R.L.; Zimmerman, G.A.; Arabi, Y.M.; Beitler, J.R.; Mercat, A.; Herridge, M.; Randolph, A.G.; Calfee, C.S. Acute Respiratory Distress Syndrome. Nat. Rev. Dis. Primers 2019, 5, 18. [Google Scholar] [CrossRef]
- Silva, P.L.; Ball, L.; Rocco, P.R.M.; Pelosi, P. Power to Mechanical Power to Minimize Ventilator-Induced Lung Injury? Intensive Care Med. Exp. 2019, 7, 38. [Google Scholar] [CrossRef]
- Brower, R.; Matthay, M.; Morris, A.; Schoenfeld, D.; Thompson, B.; Wheeler, A. Ventilation with Lower Tidal Volumes as Compared with Traditional Tidal Volumes for Acute Lung Injury and the Acute Respiratory Distress Syndrome. N. Engl. J. Med. 2000, 342, 1301–1308. [Google Scholar] [CrossRef]
- Yamamoto, R.; Okazaki, S.R.; Fujita, Y.; Seki, N.; Kokei, Y.; Sekine, S.; Wada, S.; Norisue, Y.; Narita, C. Usefulness of Low Tidal Volume Ventilation Strategy for Patients with Acute Respiratory Distress Syndrome: A Systematic Review and Meta-Analysis. Sci. Rep. 2022, 12, 9331. [Google Scholar] [CrossRef]
- Walkey, A.J.; Goligher, E.C.; Del Sorbo, L.; Hodgson, C.L.; Adhikari, N.K.J.; Wunsch, H.; Meade, M.O.; Uleryk, E.; Hess, D.; Talmor, D.S.; et al. Low Tidal Volume versus Non-Volume-Limited Strategies for Patients with Acute Respiratory Distress Syndrome. A Systematic Review and Meta-Analysis. Ann. Am. Thorac. Soc. 2017, 14, S271–S279. [Google Scholar] [CrossRef]
- Parshuram, C.; Kavanagh, B. Meta-Analysis of Tidal Volumes in Ards. Am. J. Respir. Crit. Care Med. 2003, 167, 798–800. [Google Scholar] [CrossRef]
- Pisani, L.; Algera, A.G.; Neto, A.S.; Azevedo, L.; Pham, T.; Paulus, F.; de Abreu, M.G.; Pelosi, P.; Dondorp, A.M.; Bellani, G.; et al. Geoeconomic Variations in Epidemiology, Ventilation Management, and Outcomes in Invasively Ventilated Intensive Care Unit Patients without Acute Respiratory Distress Syndrome: A Pooled Analysis of Four Observational Studies. Lancet Glob. Health 2022, 10, e227–e235. [Google Scholar] [CrossRef]
- Needham, D.M.; Yang, T.; Dinglas, V.D.; Mendez-Tellez, P.A.; Shanholtz, C.; Sevransky, J.E.; Brower, R.G.; Pronovost, P.J.; Colantuoni, E. Timing of Low Tidal Volume Ventilation and Intensive Care Unit Mortality in Acute Respiratory Distress Syndrome. A Prospective Cohort Study. Am. J. Respir. Crit. Care Med. 2015, 191, 177–185. [Google Scholar] [CrossRef] [PubMed]
- Fuller, B.M.; Ferguson, I.T.; Mohr, N.M.; Drewry, A.M.; Palmer, C.; Wessman, B.T.; Ablordeppey, E.; Keeperman, J.; Stephens, R.J.; Briscoe, C.C.; et al. Lung-Protective Ventilation Initiated in the Emergency Department (LOV-ED): A Quasi-Experimental, Before-After Trial. Ann. Emerg. Med. 2017, 70, 406–418. [Google Scholar] [CrossRef] [PubMed]
- Griffiths, M.J.D.; McAuley, D.F.; Perkins, G.D.; Barrett, N.; Blackwood, B.; Boyle, A.; Chee, N.; Connolly, B.; Dark, P.; Finney, S.; et al. Guidelines on the Management of Acute Respiratory Distress Syndrome. BMJ Open Respir. Res. 2019, 6, e000420. [Google Scholar] [CrossRef] [PubMed]
- Villar, J.; Martín-Rodríguez, C.; Domínguez-Berrot, A.M.; Fernández, L.; Ferrando, C.; Soler, J.A.; Díaz-Lamas, A.M.; González-Higueras, E.; Nogales, L.; Ambrós, A.; et al. A Quantile Analysis of Plateau and Driving Pressures. Crit. Care Med. 2017, 45, 843–850. [Google Scholar] [CrossRef]
- Sahetya, S.K.; Goligher, E.C.; Brower, R.G. Fifty Years of Research in ARDS. Setting Positive End-Expiratory Pressure in Acute Respiratory Distress Syndrome. Am. J. Respir. Crit. Care Med. 2017, 195, 1429–1438. [Google Scholar] [CrossRef]
- Caironi, P.; Cressoni, M.; Chiumello, D.; Ranieri, M.; Quintel, M.; Russo, S.G.; Cornejo, R.; Bugedo, G.; Carlesso, E.; Russo, R.; et al. Lung Opening and Closing during Ventilation of Acute Respiratory Distress Syndrome. Am. J. Respir. Crit. Care Med. 2010, 181, 578–586. [Google Scholar] [CrossRef]
- Slutsky, A.S.; Ranieri, V.M. Ventilator-Induced Lung Injury. N. Engl. J. Med. 2013, 369, 2126–2136. [Google Scholar] [CrossRef]
- Fougères, E.; Teboul, J.-L.; Richard, C.; Osman, D.; Chemla, D.; Monnet, X. Hemodynamic Impact of a Positive End-Expiratory Pressure Setting in Acute Respiratory Distress Syndrome: Importance of the Volume Status. Crit. Care Med. 2010, 38, 802–807. [Google Scholar] [CrossRef]
- Mekontso Dessap, A.; Boissier, F.; Charron, C.; Bégot, E.; Repessé, X.; Legras, A.; Brun-Buisson, C.; Vignon, P.; Vieillard-Baron, A. Acute Cor Pulmonale during Protective Ventilation for Acute Respiratory Distress Syndrome: Prevalence, Predictors, and Clinical Impact. Intensive Care Med. 2016, 42, 862–870. [Google Scholar] [CrossRef]
- Cavalcanti, A.B.; Suzumura, É.A.; Laranjeira, L.N.; de Paisani, D.M.; Damiani, L.P.; Guimarães, H.P.; Romano, E.R.; de Regenga, M.M.; Taniguchi, L.N.T.; Teixeira, C.; et al. Effect of Lung Recruitment and Titrated Positive End-Expiratory Pressure (PEEP) vs Low PEEP on Mortality in Patients with Acute Respiratory Distress Syndrome. JAMA 2017, 318, 1335. [Google Scholar] [CrossRef]
- Brower, R.G.; Lanken, P.N.; MacIntyre, N.; Matthay, M.A.; Morris, A.; Ancukiewicz, M.; Schoenfeld, D.; Thompson, B.T. Higher versus Lower Positive End-Expiratory Pressures in Patients with the Acute Respiratory Distress Syndrome. N. Engl. J. Med. 2004, 351, 327–336. [Google Scholar] [CrossRef]
- Mercat, A.; Richard, J.-C.M.; Vielle, B.; Jaber, S.; Osman, D.; Diehl, J.-L.; Lefrant, J.-Y.; Prat, G.; Richecoeur, J.; Nieszkowska, A.; et al. Positive End-Expiratory Pressure Setting in Adults with Acute Lung Injury and Acute Respiratory Distress Syndrome. JAMA 2008, 299, 646. [Google Scholar] [CrossRef]
- Meade, M.O.; Cook, D.J.; Guyatt, G.H.; Slutsky, A.S.; Arabi, Y.M.; Cooper, D.J.; Davies, A.R.; Hand, L.E.; Zhou, Q.; Thabane, L.; et al. Ventilation Strategy Using Low Tidal Volumes, Recruitment Maneuvers, and High Positive End-Expiratory Pressure for Acute Lung Injury and Acute Respiratory Distress Syndrome. JAMA 2008, 299, 637. [Google Scholar] [CrossRef]
- Briel, M.; Meade, M.; Mercat, A.; Brower, R.G.; Talmor, D.; Walter, S.D.; Slutsky, A.S.; Pullenayegum, E.; Zhou, Q.; Cook, D.; et al. Higher vs Lower Positive End-Expiratory Pressure in Patients with Acute Lung Injury and Acute Respiratory Distress Syndrome. JAMA 2010, 303, 865. [Google Scholar] [CrossRef]
- Gattinoni, L.; Caironi, P.; Cressoni, M.; Chiumello, D.; Ranieri, V.M.; Quintel, M.; Russo, S.; Patroniti, N.; Cornejo, R.; Bugedo, G. Lung Recruitment in Patients with the Acute Respiratory Distress Syndrome. N. Engl. J. Med. 2006, 354, 1775–1786. [Google Scholar] [CrossRef]
- Cressoni, M.; Chiurazzi, C.; Gotti, M.; Amini, M.; Brioni, M.; Algieri, I.; Cammaroto, A.; Rovati, C.; Massari, D.; di Castiglione, C.B.; et al. Lung Inhomogeneities and Time Course of Ventilator-Induced Mechanical Injuries. Anesthesiology 2015, 123, 618–627. [Google Scholar] [CrossRef]
- Constantin, J.-M.; Jabaudon, M.; Lefrant, J.-Y.; Jaber, S.; Quenot, J.-P.; Langeron, O.; Ferrandière, M.; Grelon, F.; Seguin, P.; Ichai, C.; et al. Personalised Mechanical Ventilation Tailored to Lung Morphology versus Low Positive End-Expiratory Pressure for Patients with Acute Respiratory Distress Syndrome in France (the LIVE Study): A Multicentre, Single-Blind, Randomised Controlled Trial. Lancet Respir. Med. 2019, 7, 870–880. [Google Scholar] [CrossRef]
- Ball, L.; Serpa Neto, A.; Trifiletti, V.; Mandelli, M.; Firpo, I.; Robba, C.; Gama de Abreu, M.; Schultz, M.J.; Patroniti, N.; Rocco, P.R.M.; et al. Effects of Higher PEEP and Recruitment Manoeuvres on Mortality in Patients with ARDS: A Systematic Review, Meta-Analysis, Meta-Regression and Trial Sequential Analysis of Randomized Controlled Trials. Intensive Care Med. Exp. 2020, 8, 39. [Google Scholar] [CrossRef]
- Beitler, J.R.; Sarge, T.; Banner-Goodspeed, V.M.; Gong, M.N.; Cook, D.; Novack, V.; Loring, S.H.; Talmor, D. Effect of Titrating Positive End-Expiratory Pressure (PEEP) With an Esophageal Pressure–Guided Strategy vs an Empirical High PEEP-F io2 Strategy on Death and Days Free from Mechanical Ventilation Among Patients With Acute Respirator. JAMA 2019, 321, 846. [Google Scholar] [CrossRef]
- Pelosi, P.; Ball, L.; Barbas, C.S.V.; Bellomo, R.; Burns, K.E.A.; Einav, S.; Gattinoni, L.; Laffey, J.G.; Marini, J.J.; Myatra, S.N.; et al. Personalized Mechanical Ventilation in Acute Respiratory Distress Syndrome. Crit. Care 2021, 25, 250. [Google Scholar] [CrossRef]
- Pelosi, P.; Rocco, P.R.M.; Gama de Abreu, M. Close down the Lungs and Keep Them Resting to Minimize Ventilator-Induced Lung Injury. Crit. Care 2018, 22, 72. [Google Scholar] [CrossRef] [PubMed]
- Chen, L.; Jonkman, A.; Pereira, S.M.; Lu, C.; Brochard, L. Driving Pressure Monitoring during Acute Respiratory Failure in 2020. Curr. Opin. Crit. Care 2021, 27, 303–310. [Google Scholar] [CrossRef] [PubMed]
- Webb, H.; Tierney, D. Experimental Pulmonary Edema Due to Intermittent Positive Pressure Ventilation with High Inflation Pressures. Protection by Positive End-Expiratory Pressure. Am. Rev. Respir. Dis. 1974, 110, 556–565. [Google Scholar] [CrossRef] [PubMed]
- Chiumello, D.; Carlesso, E.; Brioni, M.; Cressoni, M. Airway Driving Pressure and Lung Stress in ARDS Patients. Crit. Care 2016, 20, 276. [Google Scholar] [CrossRef]
- Amato, M.B.P.; Meade, M.O.; Slutsky, A.S.; Brochard, L.; Costa, E.L.V.; Schoenfeld, D.A.; Stewart, T.E.; Briel, M.; Talmor, D.; Mercat, A.; et al. Driving Pressure and Survival in the Acute Respiratory Distress Syndrome. N. Engl. J. Med. 2015, 372, 747–755. [Google Scholar] [CrossRef]
- Tejerina, E.; Pelosi, P.; Muriel, A.; Peñuelas, O.; Sutherasan, Y.; Frutos-Vivar, F.; Nin, N.; Davies, A.R.; Rios, F.; Violi, D.A.; et al. Association between Ventilatory Settings and Development of Acute Respiratory Distress Syndrome in Mechanically Ventilated Patients Due to Brain Injury. J. Crit. Care 2017, 38, 341–345. [Google Scholar] [CrossRef]
- Pereira Romano, M.L.; Maia, I.S.; Laranjeira, L.N.; Damiani, L.P.; de Paisani, D.M.; de Borges, M.C.; Dantas, B.G.; Caser, E.B.; Victorino, J.A.; de Filho, W.O.; et al. Driving Pressure–Limited Strategy for Patients with Acute Respiratory Distress Syndrome. A Pilot Randomized Clinical Trial. Ann. Am. Thorac. Soc. 2020, 17, 596–604. [Google Scholar] [CrossRef]
- Laffey, J.G.; Bellani, G.; Pham, T.; Fan, E.; Madotto, F.; Bajwa, E.K.; Brochard, L.; Clarkson, K.; Esteban, A.; Gattinoni, L.; et al. Potentially Modifiable Factors Contributing to Outcome from Acute Respiratory Distress Syndrome: The LUNG SAFE Study. Intensive Care Med. 2016, 42, 1865–1876. [Google Scholar] [CrossRef]
- Aoyama, H.; Yamada, Y.; Fan, E. The Future of Driving Pressure: A Primary Goal for Mechanical Ventilation? J. Intensive Care 2018, 6, 64. [Google Scholar] [CrossRef]
- Maeda, Y.; Fujino, Y.; Uchiyama, A.; Matsuura, N.; Mashimo, T.; Nishimura, M. Effects of Peak Inspiratory Flow on Development of Ventilator-Induced Lung Injury in Rabbits. Anesthesiology 2004, 101, 722–728. [Google Scholar] [CrossRef]
- Costa, E.L.V.; Slutsky, A.S.; Brochard, L.J.; Brower, R.; Serpa-Neto, A.; Cavalcanti, A.B.; Mercat, A.; Meade, M.; Morais, C.C.A.; Goligher, E.; et al. Ventilatory Variables and Mechanical Power in Patients with Acute Respiratory Distress Syndrome. Am. J Respir. Crit. Care Med. 2021, 204, 303–311. [Google Scholar] [CrossRef]
- Felix, N.S.; Samary, C.S.; Cruz, F.F.; Rocha, N.N.; Fernandes, M.V.S.; Machado, J.A.; Bose-Madureira, R.L.; Capelozzi, V.L.; Pelosi, P.; Silva, P.L.; et al. Gradually Increasing Tidal Volume May Mitigate Experimental Lung Injury in Rats. Anesthesiology 2019, 130, 767–777. [Google Scholar] [CrossRef]
- Borsellino, B.; Schultz, M.J.; Gama de Abreu, M.; Robba, C.; Bilotta, F. Mechanical Ventilation in Neurocritical Care Patients: A Systematic Literature Review. Expert Rev. Respir. Med. 2016, 10, 1123–1132. [Google Scholar] [CrossRef]
- Nucci, G.; Suki, B.; Lutchen, K. Modeling Airflow-Related Shear Stress during Heterogeneous Constriction and Mechanical Ventilation. J. Appl. Physiol. 2003, 95, 348–356. [Google Scholar] [CrossRef]
- Wittenstein, J.; Huhle, R.; Scharffenberg, M.; Kiss, T.; Herold, J.; Vivona, L.; Bergamaschi, A.; Schultz, M.J.; Pelosi, P.; Gama de Abreu, M.; et al. Effects of Two Stepwise Lung Recruitment Strategies on Respiratory Function and Haemodynamics in Anaesthetised Pigs. Eur. J. Anaesthesiol. 2021, 38, 634–643. [Google Scholar] [CrossRef]
- Evans, L.; Rhodes, A.; Alhazzani, W.; Antonelli, M.; Coopersmith, C.M.; French, C.; Machado, F.R.; Mcintyre, L.; Ostermann, M.; Prescott, H.C.; et al. Surviving Sepsis Campaign: International Guidelines for Management of Sepsis and Septic Shock 2021. Crit. Care Med. 2021, 49, e1063–e1143. [Google Scholar] [CrossRef]
- Hodgson, C.L.; Cooper, D.J.; Arabi, Y.; King, V.; Bersten, A.; Bihari, S.; Brickell, K.; Davies, A.; Fahey, C.; Fraser, J.; et al. Maximal Recruitment Open Lung Ventilation in Acute Respiratory Distress Syndrome (PHARLAP). A Phase II, Multicenter Randomized Controlled Clinical Trial. Am. J. Respir. Crit. Care Med. 2019, 200, 1363–1372. [Google Scholar] [CrossRef]
- Katira, B.H.; Engelberts, D.; Otulakowski, G.; Giesinger, R.E.; Yoshida, T.; Post, M.; Kuebler, W.M.; Connelly, K.A.; Kavanagh, B.P. Abrupt Deflation after Sustained Inflation Causes Lung Injury. Am. J. Respir. Crit. Care Med. 2018, 198, 1165–1176. [Google Scholar] [CrossRef]
- Rocha, N.N.; Samary, C.S.; Antunes, M.A.; Oliveira, M.V.; Hemerly, M.R.; Santos, P.S.; Capelozzi, V.L.; Cruz, F.F.; Marini, J.J.; Silva, P.L.; et al. The Impact of Fluid Status and Decremental PEEP Strategy on Cardiac Function and Lung and Kidney Damage in Mild-Moderate Experimental Acute Respiratory Distress Syndrome. Respir. Res. 2021, 22, 214. [Google Scholar] [CrossRef]
- Xavier, P.H.; Fernandes Fonseca, A.C.; Gonçalves, L.A.; de Sousa, G.C.; Coelho da Silva, M.; de Magalhães Sacramento, R.F.; dos Santos Samary, C.; Medeiros, M.; Cruz, F.F.; Capelozzi, V.L.; et al. Lung Injury Is Induced by Abrupt Increase in Respiratory Rate but Prevented by Recruitment Maneuver in Mild Acute Respiratory Distress Syndrome in Rats. Anesthesiology 2022. Epub ahead of print. [Google Scholar] [CrossRef]
- Coppola, S.; Caccioppola, A.; Froio, S.; Formenti, P.; De Giorgis, V.; Galanti, V.; Consonni, D.; Chiumello, D. Effect of Mechanical Power on Intensive Care Mortality in ARDS Patients. Crit. Care 2020, 24, 246. [Google Scholar] [CrossRef] [PubMed]
- Serpa Neto, A.; Deliberato, R.O.; Johnson, A.E.W.; Bos, L.D.; Amorim, P.; Pereira, S.M.; Cazati, D.C.; Cordioli, R.L.; Correa, T.D.; Pollard, T.J.; et al. Mechanical Power of Ventilation Is Associated with Mortality in Critically Ill Patients: An Analysis of Patients in Two Observational Cohorts. Intensive Care Med. 2018, 44, 1914–1922. [Google Scholar] [CrossRef] [PubMed]
- Parhar, K.K.S.; Zjadewicz, K.; Soo, A.; Sutton, A.; Zjadewicz, M.; Doig, L.; Lam, C.; Ferland, A.; Niven, D.J.; Fiest, K.M.; et al. Epidemiology, Mechanical Power, and 3-Year Outcomes in Acute Respiratory Distress Syndrome Patients Using Standardized Screening. An Observational Cohort Study. Ann. Am. Thorac. Soc. 2019, 16, 1263–1272. [Google Scholar] [CrossRef] [PubMed]
- Cressoni, M.; Gotti, M.; Chiurazzi, C.; Massari, D.; Algieri, I.; Amini, M.; Cammaroto, A.; Brioni, M.; Montaruli, C.; Nikolla, K.; et al. Mechanical Power and Development of Ventilator-Induced Lung Injury. Anesthesiology 2016, 124, 1100–1108. [Google Scholar] [CrossRef]
- Chiu, L.-C.; Lin, S.-W.; Chuang, L.-P.; Li, H.-H.; Liu, P.-H.; Tsai, F.-C.; Chang, C.-H.; Hung, C.-Y.; Lee, C.-S.; Leu, S.-W.; et al. Mechanical Power during Extracorporeal Membrane Oxygenation and Hospital Mortality in Patients with Acute Respiratory Distress Syndrome. Crit. Care 2021, 25, 13. [Google Scholar] [CrossRef]
- Robba, C.; Badenes, R.; Battaglini, D.; Ball, L.; Brunetti, I.; Jakobsen, J.C.; Lilja, G.; Friberg, H.; Wendel-Garcia, P.D.; Young, P.J.; et al. Ventilatory Settings in the Initial 72 h and Their Association with Outcome in Out-of-Hospital Cardiac Arrest Patients: A Preplanned Secondary Analysis of the Targeted Hypothermia versus Targeted Normothermia after out-of-Hospital Cardiac Arrest (TTM2) Tr. Intensive Care Med. 2022, 48, 1024–1038. [Google Scholar] [CrossRef]
- Nieman, G.F.; Satalin, J.; Andrews, P.; Wilcox, K.; Aiash, H.; Baker, S.; Kollisch-Singule, M.; Madden, M.; Gatto, L.A.; Habashi, N.M. Preemptive Mechanical Ventilation Based on Dynamic Physiology in the Alveolar Microenvironment: Novel Considerations of Time-Dependent Properties of the Respiratory System. J. Trauma Acute Care Surg. 2018, 85, 1081–1091. [Google Scholar] [CrossRef]
- Chen, C.; Zhen, J.; Gong, S.; Yan, J.; Li, L. Efficacy of Airway Pressure Release Ventilation for Acute Respiratory Distress Syndrome: A Systematic Review with Meta-Analysis. Ann. Palliat. Med. 2021, 10, 10349–10359. [Google Scholar] [CrossRef]
- Zhong, X.; Wu, Q.; Yang, H.; Dong, W.; Wang, B.; Zhang, Z.; Liang, G. Airway Pressure Release Ventilation versus Low Tidal Volume Ventilation for Patients with Acute Respiratory Distress Syndrome/Acute Lung Injury: A Meta-Analysis of Randomized Clinical Trials. Ann. Transl. Med. 2020, 8, 1641. [Google Scholar] [CrossRef]
- Sun, X.; Liu, Y.; Li, N.; You, D.; Zhao, Y. The Safety and Efficacy of Airway Pressure Release Ventilation in Acute Respiratory Distress Syndrome Patients. Medicine 2020, 99, e18586. [Google Scholar] [CrossRef]
- Saddy, F.; Oliveira, G.P.; Garcia, C.S.N.B.; Nardelli, L.M.; Rzezinski, A.F.; Ornellas, D.S.; Morales, M.M.; Capelozzi, V.L.; Pelosi, P.; Rocco, P.R.M. Assisted Ventilation Modes Reduce the Expression of Lung Inflammatory and Fibrogenic Mediators in a Model of Mild Acute Lung Injury. Intensive Care Med. 2010, 36, 1417–1426. [Google Scholar] [CrossRef]
- Da Cruz, D.G.; de Magalhães, R.F.; Padilha, G.A.; da Silva, M.C.; Braga, C.L.; Silva, A.R.; Gonçalves de Albuquerque, C.F.; Capelozzi, V.L.; Samary, C.S.; Pelosi, P.; et al. Impact of Positive Biphasic Pressure during Low and High Inspiratory Efforts in Pseudomonas Aeruginosa-Induced Pneumonia. PLoS ONE 2021, 16, e0246891. [Google Scholar] [CrossRef]
- Thompson, A.F.; Moraes, L.; Rocha, N.N.; Fernandes, M.V.S.; Antunes, M.A.; Abreu, S.C.; Santos, C.L.; Capelozzi, V.L.; Samary, C.S.; de Abreu, M.G.; et al. Impact of Different Frequencies of Controlled Breath and Pressure-Support Levels during Biphasic Positive Airway Pressure Ventilation on the Lung and Diaphragm in Experimental Mild Acute Respiratory Distress Syndrome. PLoS ONE 2021, 16, e0256021. [Google Scholar] [CrossRef]
- Kollisch-Singule, M.; Andrews, P.; Satalin, J.; Gatto, L.A.; Nieman, G.F.; Habashi, N.M. The Time-Controlled Adaptive Ventilation Protocol: Mechanistic Approach to Reducing Ventilator-Induced Lung Injury. Eur. Respir. Rev. 2019, 28, 180126. [Google Scholar] [CrossRef]
- Silva, P.L.; Cruz, F.F.; dos Samary, C.S.; Moraes, L.; de Magalhães, R.F.; Fernandes, M.V.d.S.; Bose, R.; Pelegati, V.B.; Carvalho, H.F.; Capelozzi, V.L.; et al. Biological Response to Time-Controlled Adaptive Ventilation Depends on Acute Respiratory Distress Syndrome Etiology*. Crit. Care Med. 2018, 46, e609–e617. [Google Scholar] [CrossRef]
- Daoud, E.G.; Farag, H.L.; Chatburn, R.L. Airway Pressure Release Ventilation: What Do We Know? Respir. Care 2011, 57, 282–292. [Google Scholar] [CrossRef]
- Protti, A.; Cressoni, M.; Santini, A.; Langer, T.; Mietto, C.; Febres, D.; Chierichetti, M.; Coppola, S.; Conte, G.; Gatti, S.; et al. Lung Stress and Strain during Mechanical Ventilation. Am. J. Respir. Crit. Care Med. 2011, 183, 1354–1362. [Google Scholar] [CrossRef]
- Silva, P.L.; Ball, L.; Rocco, P.R.M.; Pelosi, P. Physiological and Pathophysiological Consequences of Mechanical Ventilation. Semin Respir. Crit. Care Med. 2022, 43, 321–334. [Google Scholar] [CrossRef]
- Battaglini, D.; Rocco, P.R.M.; Pelosi, P. New Insights in Mechanical Ventilation and Adjunctive Therapies in ARDS. Signa Vitae 2022, 1, 11. [Google Scholar] [CrossRef]
- Liu, S.; Yi, Y.; Wang, M.; Chen, Q.; Huang, Y.; Liu, L.; Xie, J.; Zhou, D.; Qiu, H. Higher Frequency Ventilation Attenuates Lung Injury during High-Frequency Oscillatory Ventilation in Sheep Models of Acute Respiratory Distress Syndrome. Anesthesiology 2013, 119, 398–411. [Google Scholar] [CrossRef]
- Downar, J.; Mehta, S. Bench-to-Bedside Review: High-Frequency Oscillatory Ventilation in Adults with Acute Respiratory Distress Syndrome. Crit. Care 2006, 10, 240. [Google Scholar] [CrossRef] [PubMed]
- Derdak, S.; Mehta, S.; Stewart, T.E.; Smith, T.; Rogers, M.; Buchman, T.G.; Carlin, B.; Lowson, S.; Granton, J. The Multicenter Oscillatory Ventila High-Frequency Oscillatory Ventilation for Acute Respiratory Distress Syndrome in Adults. Am. J. Respir. Crit. Care Med. 2002, 166, 801–808. [Google Scholar] [CrossRef] [PubMed]
- Meade, M.O.; Young, D.; Hanna, S.; Zhou, Q.; Bachman, T.E.; Bollen, C.; Slutsky, A.S.; Lamb, S.E.; Adhikari, N.K.J.; Mentzelopoulos, S.D.; et al. Severity of Hypoxemia and Effect of High-Frequency Oscillatory Ventilation in Acute Respiratory Distress Syndrome. Am. J. Respir. Crit. Care Med. 2017, 196, 727–733. [Google Scholar] [CrossRef] [PubMed]
- Sud, S.; Sud, M.; Friedrich, J.O.; Wunsch, H.; Meade, M.O.; Ferguson, N.D.; Adhikari, N.K. High-Frequency Ventilation versus Conventional Ventilation for Treatment of Acute Lung Injury and Acute Respiratory Distress Syndrome. In Cochrane Database of Systematic Reviews; John Wiley & Sons, Ltd.: Hoboken, NJ, USA, 2013; p. CD004085. [Google Scholar]
- Guérin, C.; Reignier, J.; Richard, J.-C.; Beuret, P.; Gacouin, A.; Boulain, T.; Mercier, E.; Badet, M.; Mercat, A.; Baudin, O.; et al. Prone Positioning in Severe Acute Respiratory Distress Syndrome. N. Engl. J. Med. 2013, 368, 2159–2168. [Google Scholar] [CrossRef]
- Zubieta-Calleja, G.R.; Zubieta-DeUrioste, N.; de Jesús Montelongo, F.; Sanchez, M.G.R.; Campoverdi, A.F.; Rocco, P.R.M.; Battaglini, D.; Ball, L.; Pelosi, P. Morphological and Functional Findings in COVID-19 Lung Disease as Compared to Pneumonia, ARDS, and High-Altitude Pulmonary Edema. Respir. Physiol. Neurobiol. 2023, 309, 104000. [Google Scholar] [CrossRef]
- Fan, E.; Del Sorbo, L.; Goligher, E.C.; Hodgson, C.L.; Munshi, L.; Walkey, A.J.; Adhikari, N.K.J.; Amato, M.B.P.; Branson, R.; Brower, R.G.; et al. An Official American Thoracic Society/European Society of Intensive Care Medicine/Society of Critical Care Medicine Clinical Practice Guideline: Mechanical Ventilation in Adult Patients with Acute Respiratory Distress Syndrome. Am. J. Respir. Crit. Care Med. 2017, 195, 1253–1263. [Google Scholar] [CrossRef]
- Guérin, C.; Beuret, P.; Constantin, J.M.; Bellani, G.; Garcia-Olivares, P.; Roca, O.; Meertens, J.H.; Maia, P.A.; Becher, T.; Peterson, J.; et al. A Prospective International Observational Prevalence Study on Prone Positioning of ARDS Patients: The APRONET (ARDS Prone Position Network) Study. Intensive Care Med. 2018, 44, 22–37. [Google Scholar] [CrossRef]
- Giani, M.; Martucci, G.; Madotto, F.; Belliato, M.; Fanelli, V.; Garofalo, E.; Forlini, C.; Lucchini, A.; Panarello, G.; Bottino, N.; et al. Prone Positioning during Venovenous Extracorporeal Membrane Oxygenation in Acute Respiratory Distress Syndrome. A Multicenter Cohort Study and Propensity-Matched Analysis. Ann. Am. Thorac. Soc. 2021, 18, 495–501. [Google Scholar] [CrossRef]
- Peek, G.J.; Clemens, F.; Elbourne, D.; Firmin, R.; Hardy, P.; Hibbert, C.; Killer, H.; Mugford, M.; Thalanany, M.; Tiruvoipati, R.; et al. CESAR: Conventional Ventilatory Support vs Extracorporeal Membrane Oxygenation for Severe Adult Respiratory Failure. BMC Health Serv. Res. 2006, 6, 163. [Google Scholar] [CrossRef]
- Urner, M.; Barnett, A.G.; Bassi, G.L.; Brodie, D.; Dalton, H.J.; Ferguson, N.D.; Heinsar, S.; Hodgson, C.L.; Peek, G.; Shekar, K.; et al. Venovenous Extracorporeal Membrane Oxygenation in Patients with Acute Covid-19 Associated Respiratory Failure: Comparative Effectiveness Study. BMJ 2022, 377, e068723. [Google Scholar] [CrossRef]
- Serpa Neto, A.; Schmidt, M.; Azevedo, L.C.P.; Bein, T.; Brochard, L.; Beutel, G.; Combes, A.; Costa, E.L.V.; Hodgson, C.; Lindskov, C.; et al. Associations between Ventilator Settings during Extracorporeal Membrane Oxygenation for Refractory Hypoxemia and Outcome in Patients with Acute Respiratory Distress Syndrome: A Pooled Individual Patient Data Analysis. Intensive Care Med. 2016, 42, 1672–1684. [Google Scholar] [CrossRef]
- May, A.G.; Sen, A.; Cove, M.E.; Kellum, J.A.; Federspiel, W.J. Extracorporeal CO2 Removal by Hemodialysis: In Vitro Model and Feasibility. Intensive Care Med. Exp. 2017, 5, 20. [Google Scholar] [CrossRef]
- Del Sorbo, L.; Cypel, M.; Fan, E. Extracorporeal Life Support for Adults with Severe Acute Respiratory Failure. Lancet Respir. Med. 2014, 2, 154–164. [Google Scholar] [CrossRef]
- Combes, A.; Auzinger, G.; Capellier, G.; du Cheyron, D.; Clement, I.; Consales, G.; Dabrowski, W.; De Bels, D.; de Molina Ortiz, F.J.G.; Gottschalk, A.; et al. ECCO2R Therapy in the ICU: Consensus of a European Round Table Meeting. Crit. Care 2020, 24, 490. [Google Scholar] [CrossRef]
- Bein, T.; Weber-Carstens, S.; Goldmann, A.; Müller, T.; Staudinger, T.; Brederlau, J.; Muellenbach, R.; Dembinski, R.; Graf, B.M.; Wewalka, M.; et al. Lower Tidal Volume Strategy (≈3 Ml/Kg) Combined with Extracorporeal CO2 Removal versus ‘Conventional’ Protective Ventilation (6 Ml/Kg) in Severe ARDS. Intensive Care Med. 2013, 39, 847–856. [Google Scholar] [CrossRef]
- Morris, A.H.; Wallace, C.J.; Menlove, R.L.; Clemmer, T.P.; Orme, J.F.; Weaver, L.K.; Dean, N.C.; Thomas, F.; East, T.D.; Pace, N.L.; et al. Randomized Clinical Trial of Pressure-Controlled Inverse Ratio Ventilation and Extracorporeal CO2 Removal for Adult Respiratory Distress Syndrome. Am. J. Respir. Crit. Care Med. 1994, 149, 295–305. [Google Scholar] [CrossRef]
- Fitzgerald, M.; Millar, J.; Blackwood, B.; Davies, A.; Brett, S.J.; McAuley, D.F.; McNamee, J.J. Extracorporeal Carbon Dioxide Removal for Patients with Acute Respiratory Failure Secondary to the Acute Respiratory Distress Syndrome: A Systematic Review. Crit. Care 2014, 18, 222. [Google Scholar] [CrossRef]
- Wiedemann, H.; Wheeler, A.; Bernard, G.; Thompson, B.; Hayden, D.; DeBoisblanc, B.; Connors Jr, A.; Hite, R.; Harabin, A. Comparison of Two Fluid-Management Strategies in Acute Lung Injury. N. Engl. J. Med. 2006, 354, 2564–2575. [Google Scholar] [CrossRef]
- Famous, K.R.; Delucchi, K.; Ware, L.B.; Kangelaris, K.N.; Liu, K.D.; Thompson, B.T.; Calfee, C.S. Acute Respiratory Distress Syndrome Subphenotypes Respond Differently to Randomized Fluid Management Strategy. Am. J. Respir. Crit. Care Med. 2017, 195, 331–338. [Google Scholar] [CrossRef]
- Battaglini, D.; Robba, C.; Pelosi, P.; Rocco, P.R.M. Treatment for Acute Respiratory Distress Syndrome in Adults: A Narrative Review of Phase 2 and 3 Trials. Expert Opin. Emerg. Drugs 2022, 27, 187–209. [Google Scholar] [CrossRef]
- Murray, M.J.; DeBlock, H.; Erstad, B.; Gray, A.; Jacobi, J.; Jordan, C.; McGee, W.; McManus, C.; Meade, M.; Nix, S.; et al. Clinical Practice Guidelines for Sustained Neuromuscular Blockade in the Adult Critically Ill Patient. Crit. Care Med. 2016, 44, 2079–2103. [Google Scholar] [CrossRef] [PubMed]
- Alhazzani, W.; Belley-Cote, E.; Møller, M.H.; Angus, D.C.; Papazian, L.; Arabi, Y.M.; Citerio, G.; Connolly, B.; Denehy, L.; Fox-Robichaud, A.; et al. Neuromuscular Blockade in Patients with ARDS: A Rapid Practice Guideline. Intensive Care Med. 2020, 46, 1977–1986. [Google Scholar] [CrossRef] [PubMed]
- Lin, P.; Zhao, Y.; Li, X.; Jiang, F.; Liang, Z. Decreased Mortality in Acute Respiratory Distress Syndrome Patients Treated with Corticosteroids: An Updated Meta-Analysis of Randomized Clinical Trials with Trial Sequential Analysis. Crit. Care 2021, 25, 122. [Google Scholar] [CrossRef] [PubMed]
- Meduri, G.U.; Golden, E.; Freire, A.X.; Taylor, E.; Zaman, M.; Carson, S.J.; Gibson, M.; Umberger, R. Methylprednisolone Infusion in Early Severe ARDS. Chest 2007, 131, 954–963. [Google Scholar] [CrossRef] [PubMed]
- Bernard, G.; Luce, J.; Sprung, C.; Rinaldo, J.; Tate, R.; Sibbald, W.; Kariman, K.; Higgins, S.; Bradley, R.; Metz, C. High-Dose Corticosteroids in Patients with the Adult Respiratory Distress Syndrome. N. Eng. J. Med. 1987, 317, 1565–1570. [Google Scholar] [CrossRef]
- Mezidi, M.; Guérin, C. Aspirin for Prevention of Acute Respiratory Distress Syndrome (ARDS): Let’s Not Throw the Baby with the Water! Ann. Transl. Med. 2016, 4, 376. [Google Scholar] [CrossRef]
- Kor, D.J.; Carter, R.E.; Park, P.K.; Festic, E.; Banner-Goodspeed, V.M.; Hinds, R.; Talmor, D.; Gajic, O.; Ware, L.B.; Gong, M.N. Effect of Aspirin on Development of ARDS in At-Risk Patients Presenting to the Emergency Department. JAMA 2016, 315, 2406. [Google Scholar] [CrossRef]
- Bellingan, G.; Maksimow, M.; Howell, D.C.; Stotz, M.; Beale, R.; Beatty, M.; Walsh, T.; Binning, A.; Davidson, A.; Kuper, M.; et al. The Effect of Intravenous Interferon-Beta-1a (FP-1201) on Lung CD73 Expression and on Acute Respiratory Distress Syndrome Mortality: An Open-Label Study. Lancet Respir. Med. 2014, 2, 98–107. [Google Scholar] [CrossRef]
- Parekh, D.; Dancer, R.C.A.; Scott, A.; D’Souza, V.K.; Howells, P.A.; Mahida, R.Y.; Tang, J.C.Y.; Cooper, M.S.; Fraser, W.D.; Tan, L.; et al. Vitamin D to Prevent Lung Injury Following Esophagectomy—A Randomized, Placebo-Controlled Trial*. Crit. Care Med. 2018, 46, e1128–e1135. [Google Scholar] [CrossRef]
- Fowler, A.A.; Truwit, J.D.; Hite, R.D.; Morris, P.E.; De Wilde, C.; Priday, A.; Fisher, B.; Thacker, L.R.; Natarajan, R.; Brophy, D.F.; et al. Effect of Vitamin C Infusion on Organ Failure and Biomarkers of Inflammation and Vascular Injury in Patients with Sepsis and Severe Acute Respiratory Failure. JAMA 2019, 322, 1261. [Google Scholar] [CrossRef]
- Craig, T.R.; Duffy, M.J.; Shyamsundar, M.; McDowell, C.; O’Kane, C.M.; Elborn, J.S.; McAuley, D.F. A Randomized Clinical Trial of Hydroxymethylglutaryl– Coenzyme A Reductase Inhibition for Acute Lung Injury (The HARP Study). Am. J. Respir. Crit. Care Med. 2011, 183, 620–626. [Google Scholar] [CrossRef]
- Truwit, J.; Bernard, G.; Steingrub, J.; Matthay, M.; Liu, K.; Albertson, T.; Brower, R.; Shanholtz, C.; Rock, P.; Douglas, I.; et al. Rosuvastatin for Sepsis-Associated Acute Respiratory Distress Syndrome. N. Engl. J. Med. 2014, 370, 2191–2200. [Google Scholar] [CrossRef]
- Calfee, C.S.; Delucchi, K.L.; Sinha, P.; Matthay, M.A.; Hackett, J.; Shankar-Hari, M.; McDowell, C.; Laffey, J.G.; O’Kane, C.M.; McAuley, D.F.; et al. Acute Respiratory Distress Syndrome Subphenotypes and Differential Response to Simvastatin: Secondary Analysis of a Randomised Controlled Trial. Lancet Respir. Med. 2018, 6, 691–698. [Google Scholar] [CrossRef]
- Zhang, X.; Zhu, Z.; Jiao, W.; Liu, W.; Liu, F.; Zhu, X. Ulinastatin Treatment for Acute Respiratory Distress Syndrome in China: A Meta-Analysis of Randomized Controlled Trials. BMC Pulm. Med. 2019, 19, 196. [Google Scholar] [CrossRef]
- Feng, Y. Efficacy of Statin Therapy in Patients with Acute Respiratory Distress Syndrome/Acute Lung Injury: A Systematic Review and Meta-Analysis. Eur. Rev. Med. Pharmacol. Sci. 2018, 22, 3190–3198. [Google Scholar] [CrossRef]
- Liu, J.; Chen, Y.; Gao, Y.; Walline, J.H.; Lu, X.; Yu, S.; Zhao, L.; Ge, Z.; Li, Y. N -Acetylcysteine as a Treatment for Amatoxin Poisoning: A Systematic Review. Clin. Toxicol. 2020, 58, 1015–1022. [Google Scholar] [CrossRef]
- Domenighetti, G.; Suter, P.M.; Schaller, M.-D.; Ritz, R.; Perret, C. Treatment with N-Acetylcysteine during Acute Respiratory Distress Syndrome: A Randomized, Double-Blind, Placebo-Controlled Clinical Study. J. Crit. Care 1997, 12, 177–182. [Google Scholar] [CrossRef]
- Taher, A.; Lashgari, M.; Sedighi, L.; Rahimi-bashar, F.; Poorolajal, J.; Mehrpooya, M. A Pilot Study on Intravenous N-Acetylcysteine Treatment in Patients with Mild-to-Moderate COVID19-Associated Acute Respiratory Distress Syndrome. Pharmacol. Rep. 2021, 73, 1650–1659. [Google Scholar] [CrossRef]
- Matthay, M.; Brower, R.; Carson, S.; Douglas, I.; Eisner, M.; Hite, D.; Holets, S.; Kallet, R.; Liu, K.; Maclntyre, N.; et al. Randomized, Placebo-Controlled Clinical Trial of an Aerosolized β 2 -Agonist for Treatment of Acute Lung Injury. Am. J. Respir. Crit. Care Med. 2011, 184, 561–568. [Google Scholar] [CrossRef]
- Perkins, G.D.; McAuley, D.F.; Thickett, D.R.; Gao, F. The β-Agonist Lung Injury Trial (BALTI). Am. J. Respir. Crit. Care Med. 2006, 173, 281–287. [Google Scholar] [CrossRef]
- Kadoi, Y.; Hinohara, H.; Kunimoto, F.; Saito, S.; Goto, F.; Kosaka, T.; Ieta, K. Pilot Study of the Effects of ONO-5046 in Patients with Acute Respiratory Distress Syndrome. Anesth. Analg. 2004, 99, 872–877. [Google Scholar] [CrossRef] [PubMed]
- Tamakuma, S.; Ogawa, M.; Aikawa, N.; Kubota, T.; Hirasawa, H.; Ishizaka, A.; Taenaka, N.; Hamada, C.; Matsuoka, S.; Abiru, T. Relationship between Neutrophil Elastase and Acute Lung Injury in Humans. Pulm. Pharmacol. Ther. 2004, 17, 271–279. [Google Scholar] [CrossRef] [PubMed]
- Zeiher, B.G.; Artigas, A.; Vincent, J.-L.; Dmitrienko, A.; Jackson, K.; Thompson, B.T.; Bernard, G. Neutrophil Elastase Inhibition in Acute Lung Injury: Results of the STRIVE Study. Crit. Care Med. 2004, 32, 1695–1702. [Google Scholar] [CrossRef] [PubMed]
- Michael, J.; Barton, R.; Saffle, J.; Mone, M.; Markewitz, B.; Hillier, K.; Elstad, M.; Campbell, E.; Troyer, B.; Whatley, R.; et al. Inhaled Nitric Oxide Versus Conventional Therapy. Am. J. Respir. Crit. Care Med. 1998, 157, 1372–1380. [Google Scholar] [CrossRef] [PubMed]
- Papazian, L.; Aubron, C.; Brochard, L.; Chiche, J.-D.; Combes, A.; Dreyfuss, D.; Forel, J.-M.; Guérin, C.; Jaber, S.; Mekontso-Dessap, A.; et al. Formal Guidelines: Management of Acute Respiratory Distress Syndrome. Ann. Intensive Care 2019, 9, 69. [Google Scholar] [CrossRef] [PubMed]
- Ford, H.J.; Anderson, W.H.; Wendlandt, B.; Bice, T.; Ceppe, A.; Lanier, J.; Carson, S.S. Randomized, Placebo-Controlled Trial of Inhaled Treprostinil for Patients at Risk for Acute Respiratory Distress Syndrome. Ann. Am. Thorac. Soc. 2021, 18, 641–647. [Google Scholar] [CrossRef]
- Willson, D.F.; Truwit, J.D.; Conaway, M.R.; Traul, C.S.; Egan, E.E. The Adult Calfactant in Acute Respiratory Distress Syndrome Trial. Chest 2015, 148, 356–364. [Google Scholar] [CrossRef]
- Meng, S.-S.; Chang, W.; Lu, Z.-H.; Xie, J.-F.; Qiu, H.-B.; Yang, Y.; Guo, F.-M. Effect of Surfactant Administration on Outcomes of Adult Patients in Acute Respiratory Distress Syndrome: A Meta-Analysis of Randomized Controlled Trials. BMC Pulm. Med. 2019, 19, 9. [Google Scholar] [CrossRef]
- Schmid, B.; Kredel, M.; Ullrich, R.; Krenn, K.; Lucas, R.; Markstaller, K.; Fischer, B.; Kranke, P.; Meybohm, P.; Zwißler, B.; et al. Safety and Preliminary Efficacy of Sequential Multiple Ascending Doses of Solnatide to Treat Pulmonary Permeability Edema in Patients with Moderate-to-Severe ARDS—A Randomized, Placebo-Controlled, Double-Blind Trial. Trials 2021, 22, 643. [Google Scholar] [CrossRef]
- Christie, J.D.; Vaslef, S.; Chang, P.K.; May, A.K.; Gunn, S.R.; Yang, S.; Hardes, K.; Kahl, L.; Powley, W.M.; Lipson, D.A.; et al. A Randomized Dose-Escalation Study of the Safety and Anti-Inflammatory Activity of the P38 Mitogen-Activated Protein Kinase Inhibitor Dilmapimod in Severe Trauma Subjects at Risk for Acute Respiratory Distress Syndrome. Crit. Care Med. 2015, 43, 1859–1869. [Google Scholar] [CrossRef]
- Yang, S.; Dumitrescu, T.P. Population Pharmacokinetics and Pharmacodynamics Modelling of Dilmapimod in Severe Trauma Subjects at Risk for Acute Respiratory Distress Syndrome. Drugs R D 2017, 17, 145–158. [Google Scholar] [CrossRef]
- Shyamsundar, M.; McAuley, D.F.; Ingram, R.J.; Gibson, D.S.; O’Kane, D.; McKeown, S.T.; Edwards, A.; Taggart, C.; Elborn, J.S.; Calfee, C.S.; et al. Keratinocyte Growth Factor Promotes Epithelial Survival and Resolution in a Human Model of Lung Injury. Am. J. Respir. Crit. Care Med. 2014, 189, 1520–1529. [Google Scholar] [CrossRef]
- McAuley, D.F.; Cross, L.M.; Hamid, U.; Gardner, E.; Elborn, J.S.; Cullen, K.M.; Dushianthan, A.; Grocott, M.P.; Matthay, M.A.; O’Kane, C.M. Keratinocyte Growth Factor for the Treatment of the Acute Respiratory Distress Syndrome (KARE): A Randomised, Double-Blind, Placebo-Controlled Phase 2 Trial. Lancet Respir. Med. 2017, 5, 484–491. [Google Scholar] [CrossRef]
- Paine, R.; Standiford, T.J.; Dechert, R.E.; Moss, M.; Martin, G.S.; Rosenberg, A.L.; Thannickal, V.J.; Burnham, E.L.; Brown, M.B.; Hyzy, R.C. A Randomized Trial of Recombinant Human Granulocyte-Macrophage Colony Stimulating Factor for Patients with Acute Lung Injury. Crit. Care Med. 2012, 40, 90–97. [Google Scholar] [CrossRef]
- Zheng, G.; Huang, L.; Tong, H.; Shu, Q.; Hu, Y.; Ge, M.; Deng, K.; Zhang, L.; Zou, B.; Cheng, B.; et al. Treatment of Acute Respiratory Distress Syndrome with Allogeneic Adipose-Derived Mesenchymal Stem Cells: A Randomized, Placebo-Controlled Pilot Study. Respir. Res. 2014, 15, 39. [Google Scholar] [CrossRef]
- Wick, K.D.; Leligdowicz, A.; Zhuo, H.; Ware, L.B.; Matthay, M.A. Mesenchymal Stromal Cells Reduce Evidence of Lung Injury in Patients with ARDS. JCI Insight 2021, 6, e1488983. [Google Scholar] [CrossRef]
- Bellingan, G.; Jacono, F.; Bannard-Smith, J.; Brealey, D.; Meyer, N.; Thickett, D.; Young, D.; Bentley, A.; McVerry, B.J.; Wunderink, R.G.; et al. Safety and Efficacy of Multipotent Adult Progenitor Cells in Acute Respiratory Distress Syndrome (MUST-ARDS): A Multicentre, Randomised, Double-Blind, Placebo-Controlled Phase 1/2 Trial. Intensive Care Med. 2022, 48, 36–44. [Google Scholar] [CrossRef]
- Moss, M.; Huang, D.; Brower, R.; Ferguson, N.; Ginde, A.; Gong, M.; Grissom, C.; Gundel, S.; Hayden, D.; Hite, R.; et al. Early Neuromuscular Blockade in the Acute Respiratory Distress Syndrome. N. Engl. J. Med. 2019, 380, 1997–2008. [Google Scholar] [CrossRef]
- Ho, A.T.N.; Patolia, S.; Guervilly, C. Neuromuscular Blockade in Acute Respiratory Distress Syndrome: A Systematic Review and Meta-Analysis of Randomized Controlled Trials. J. Intensive Care 2020, 8, 12. [Google Scholar] [CrossRef]
- Tarazan, N.; Alshehri, M.; Sharif, S.; Al Duhailib, Z.; Møller, M.H.; Belley-Cote, E.; Alshahrani, M.; Centofanti, J.; McIntyre, L.; Baw, B.; et al. Neuromuscular Blocking Agents in Acute Respiratory Distress Syndrome: Updated Systematic Review and Meta-Analysis of Randomized Trials. Intensive Care Med. Exp. 2020, 8, 61. [Google Scholar] [CrossRef]
- Villar, J.; Ferrando, C.; Martínez, D.; Ambrós, A.; Muñoz, T.; Soler, J.A.; Aguilar, G.; Alba, F.; González-Higueras, E.; Conesa, L.A.; et al. Dexamethasone Treatment for the Acute Respiratory Distress Syndrome: A Multicentre, Randomised Controlled Trial. Lancet Respir. Med. 2020, 8, 267–276. [Google Scholar] [CrossRef] [PubMed]
- Tung, Y.-T.; Wei, C.-H.; Yen, C.-C.; Lee, P.-Y.; Ware, L.B.; Huang, H.-E.; Chen, W.; Chen, C.-M. Aspirin Attenuates Hyperoxia-Induced Acute Respiratory Distress Syndrome (ARDS) by Suppressing Pulmonary Inflammation via the NF-ΚB Signaling Pathway. Front. Pharmacol. 2022, 12, 3938. [Google Scholar] [CrossRef] [PubMed]
- Ranieri, V.M.; Pettilä, V.; Karvonen, M.K.; Jalkanen, J.; Nightingale, P.; Brealey, D.; Mancebo, J.; Ferrer, R.; Mercat, A.; Patroniti, N.; et al. Effect of Intravenous Interferon β-1a on Death and Days Free from Mechanical Ventilation Among Patients With Moderate to Severe Acute Respiratory Distress Syndrome. JAMA 2020, 323, 725. [Google Scholar] [CrossRef] [PubMed]
- Ginde, A.; Brower, R.; Caterino, J.; Finck, L.; Banner-Goodspeed, V.; Grissom, C.; Hayden, D.; Hough, C.; Hyzy, R.; Khan, A.; et al. Early High-Dose Vitamin D 3 for Critically Ill, Vitamin D–Deficient Patients. N. Engl. J. Med. 2019, 381, 2529–2540. [Google Scholar] [CrossRef]
- McAuley, D.F.; Laffey, J.G.; O’Kane, C.M.; Perkins, G.D.; Mullan, B.; Trinder, T.J.; Johnston, P.; Hopkins, P.A.; Johnston, A.J.; McDowell, C.; et al. Simvastatin in the Acute Respiratory Distress Syndrome. N. Engl. J. Med. 2014, 371, 1695–1703. [Google Scholar] [CrossRef]
- Boyle, A.J.; Ferris, P.; Bradbury, I.; Conlon, J.; Shankar-Hari, M.; Rogers, A.J.; O’Kane, C.M.; McAuley, D.F. Baseline Plasma IL-18 May Predict Simvastatin Treatment Response in Patients with ARDS: A Secondary Analysis of the HARP-2 Randomised Clinical Trial. Crit. Care 2022, 26, 164. [Google Scholar] [CrossRef]
- Dinglas, V.D.; Hopkins, R.O.; Wozniak, A.W.; Hough, C.L.; Morris, P.E.; Jackson, J.C.; Mendez-Tellez, P.A.; Bienvenu, O.J.; Ely, E.W.; Colantuoni, E.; et al. One-Year Outcomes of Rosuvastatin versus Placebo in Sepsis-Associated Acute Respiratory Distress Syndrome: Prospective Follow-up of SAILS Randomised Trial. Thorax 2016, 71, 401–410. [Google Scholar] [CrossRef]
- Ji, M.; Chen, T.; Wang, B.; Chen, M.; Ding, Q.; Chen, L.; Fang, Y.; Yu, X.; Chen, Y.; Wang, X.; et al. Effects of Ulinastatin Combined with Mechanical Ventilation on Oxygen Metabolism, Inflammation and Stress Response and Antioxidant Capacity of ARDS. Exp. Ther. Med. 2018, 15, 4665–4670. [Google Scholar] [CrossRef]
- Battaglini, D.; Cruz, F.; Robba, C.; Pelosi, P.; Rocco, P.R.M. Failed Clinical Trials on COVID-19 Acute Respiratory Distress Syndrome in Hospitalized Patients: Common Oversights and Streamlining the Development of Clinically Effective Therapeutics. Expert Opin. Investig. Drugs 2022, 31, 995–1015. [Google Scholar] [CrossRef]
- Zhang, Y.; Ding, S.; Li, C.; Wang, Y.; Chen, Z.; Wang, Z. Effects of N-Acetylcysteine Treatment in Acute Respiratory Distress Syndrome: A Meta-Analysis. Exp. Ther. Med. 2017, 14, 2863–2868. [Google Scholar] [CrossRef]
- Suter, P.M.; Domenighetti, G.; Schaller, M.-D.; Laverrière, M.-C.; Ritz, R.; Perret, C. N-Acetylcysteine Enhances Recovery from Acute Lung Injury in Man. Chest 1994, 105, 190–194. [Google Scholar] [CrossRef]
- Moradi, M.; Mojtahedzadeh, M.; Mandegari, A.; Soltan-Sharifi, M.S.; Najafi, A.; Khajavi, M.R.; Hajibabayee, M.; Ghahremani, M.H. The Role of Glutathione-S-Transferase Polymorphisms on Clinical Outcome of ALI/ARDS Patient Treated with N-Acetylcysteine. Respir. Med. 2009, 103, 434–441. [Google Scholar] [CrossRef]
- Gates, S.; Perkins, G.; Lamb, S.; Kelly, C.; Thickett, D.; Young, J.; McAuley, D.; Snaith, C.; McCabe, C.; Hulme, C.; et al. Beta-Agonist Lung Injury TrIal-2 (BALTI-2): A Multicentre, Randomised, Double-Blind, Placebo-Controlled Trial and Economic Evaluation of Intravenous Infusion of Salbutamol versus Placebo in Patients with Acute Respiratory Distress Syndrome. Health Technol. Assess 2013, 17, 1–87. [Google Scholar] [CrossRef]
- Pu, S.; Wang, D.; Liu, D.; Zhao, Y.; Qi, D.; He, J.; Zhou, G. Effect of Sivelestat Sodium in Patients with Acute Lung Injury or Acute Respiratory Distress Syndrome: A Meta-Analysis of Randomized Controlled Trials. BMC Pulm. Med. 2017, 17, 148. [Google Scholar] [CrossRef]
- Walmrath, D.; Schneider, T.; Schermuly, R.; Olschewski, H.; Grimminger, F.; Seeger, W. Direct Comparison of Inhaled Nitric Oxide and Aerosolized Prostacyclin in Acute Respiratory Distress Syndrome. Am. J. Respir. Crit. Care Med. 1996, 153, 991–996. [Google Scholar] [CrossRef]
- Frossard, J.L.; Saluja, A.K.; Mach, N.; Lee, H.S.; Bhagat, L.; Hadenque, A.; Rubbia-Brandt, L.; Dranoff, G.; Steer, M.L. In Vivo Evidence for the Role of GM-CSF as a Mediator in Acute Pancreatitis-Associated Lung Injury. Am. J. Physiol.-Lung Cell. Mol. Physiol. 2002, 283, L541–L548. [Google Scholar] [CrossRef]
- Dixon, B.; Smith, R.J.; Campbell, D.J.; Moran, J.L.; Doig, G.S.; Rechnitzer, T.; MacIsaac, C.M.; Simpson, N.; van Haren, F.M.P.; Ghosh, A.N.; et al. Nebulised Heparin for Patients with or at Risk of Acute Respiratory Distress Syndrome: A Multicentre, Randomised, Double-Blind, Placebo-Controlled Phase 3 Trial. Lancet Respir. Med. 2021, 9, 360–372. [Google Scholar] [CrossRef]
- Sinha, P.; Bos, L.D. Pathophysiology of the Acute Respiratory Distress Syndrome. Crit. Care Clin. 2021, 37, 795–815. [Google Scholar] [CrossRef]
- Liu, X.; Jiang, Y.; Jia, X.; Ma, X.; Han, C.; Guo, N.; Peng, Y.; Liu, H.; Ju, Y.; Luo, X.; et al. Identification of Distinct Clinical Phenotypes of Acute Respiratory Distress Syndrome with Differential Responses to Treatment. Crit. Care 2021, 25, 320. [Google Scholar] [CrossRef]
- Sinha, P.; Delucchi, K.L.; Thompson, B.T.; McAuley, D.F.; Matthay, M.A.; Calfee, C.S. Latent Class Analysis of ARDS Subphenotypes: A Secondary Analysis of the Statins for Acutely Injured Lungs from Sepsis (SAILS) Study. Intensive Care Med. 2018, 44, 1859–1869. [Google Scholar] [CrossRef]
- Spagnolo, F.; Ghiorzo, P.; Orgiano, L.; Pastorino, L.; Picasso, V.; Tornari, E.; Ottaviano, V.; Queirolo, P. BRAF-Mutant Melanoma: Treatment Approaches, Resistance Mechanisms, and Diagnostic Strategies. Onco Targets Ther. 2015, 8, 157. [Google Scholar] [CrossRef] [PubMed]
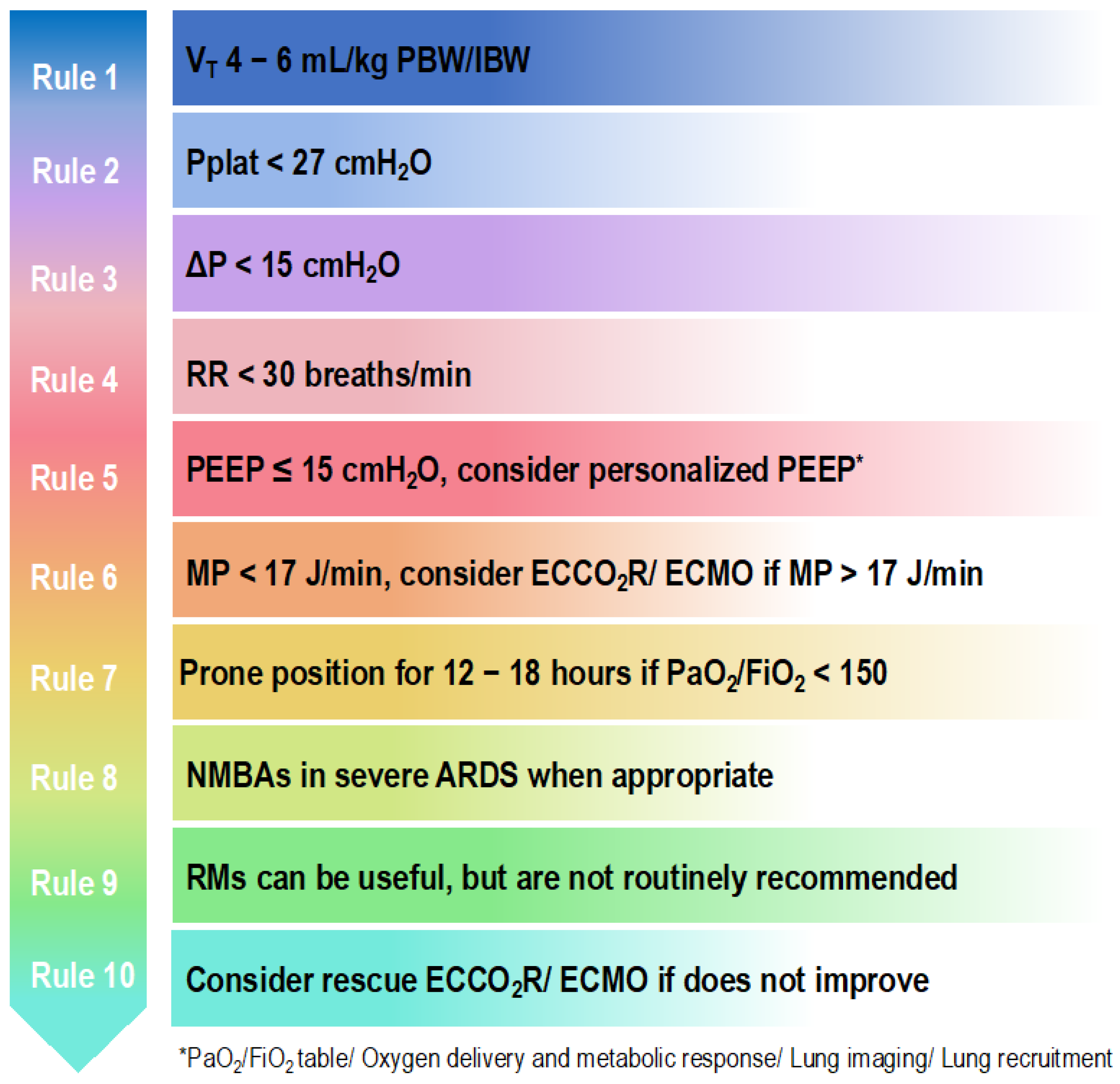
- Battaglini, D.; Sottano, M.; Ball, L.; Robba, C.; Rocco, P.R.M.; Pelosi, P. Ten Golden Rules for Individualized Mechanical Ventilation in Acute Respiratory Distress Syndrome. J. Intensive Med. 2021, 1, 42–51. [Google Scholar] [CrossRef]
- Battaglini, D.; Al-Husinat, L.; Normando, A.G.; Leme, A.P.; Franchini, K.; Morales, M.; Pelosi, P.; Rocco, P.R. Personalized Medicine Using Omics Approaches in Acute Respiratory Distress Syndrome to Identify Biological Phenotypes. Respir. Res. 2022, 23, 318. [Google Scholar] [CrossRef] [PubMed]

| Drug. | Rationale for Using in ARDS | Current Status |
|---|---|---|
| NMBAs | NMBAs paralyze skeletal muscles by blocking the transmission of nerve impulses at the myoneural junction [102,103]. | Considered in cases of early and severe ARDS with deep sedation, invasive mechanical ventilation, and the need for prone positioning within 48 h. There is no evidence to support NMBAs routine and early use [102,103]. |
| Corticosteroids | Anti-inflammatory protein expression is regulated in the nucleus by the activated glucocorticoid receptor–glucocorticoid complex, thus reducing inflammation [104]. | Not approved as a medical treatment guideline with no clear benefits in outcome. According to current research [104,105,106], there could be a significant patient benefit and the risk of adverse events is thought to be low. However, clinical trials, the majority of which were carried out before the advent of lung protective ventilation strategies, provided controversial results. Corticosteroids may be beneficial for certain steroid responsive illnesses that resemble ARDS. |
| Aspirin | Aspirin acts on platelet aggregation via inhibition of platelet thromboxane A2-synthesis. In ARDS, aspirin reduces pulmonary neutrophil infiltration as well as alveolar inflammation and injury [107]. | Not approved. No clear benefits in outcome [107,108]. |
| Interferons | Interferons are anti-inflammatory cytokines In ARDS, they facilitate clearance of bacteria, neutrophil apoptosis and efferocytosis, and promote lung repair [109]. | Not approved. No clear benefits in outcome [109]. |
| Vitamins | Vitamin D has an immunomodulator effect on innate and adaptive immunity [110], whereas vitamin C attenuates the expression of pro-inflammatory cytokines and inhibits nuclear factor kB [111]. | Not approved. No clear benefits in outcome [110,111]. |
| Statins | Statins act via inhibition of hydroxymethylglutaryl-coenzyme A reductase and also have many other pleiotropic effects, such as anti-inflammatory and anti-proliferative effects on lung inflammation [112]. | Not approved. No clear benefits in outcome [113] Statins may probably have different effects according to patient’s sub-phenotype [114,115,116]. |
| N-acetylcysteine | N-acetylcysteine acts as an antioxidant [117]. | Not approved. No clear benefits in outcome [118,119]. |
| β-Agonists | β-Agonists reduce bronchospasm, airway resistance, and inflammation as well as improve alveolar fluid clearance and stimulate alveolar epithelial and endothelial repair, thus benefiting pulmonary mechanics [120,121]. | Not approved. No clear benefits in outcome [120,121]. |
| Sivelestat | Sivelestat is an inhibitor of human neutrophil elastase. In ARDS, it improves oxygenation and reduces inflammation [122,123]. | Not approved. No clear benefits in outcome [124]. |
| Vasodilators | Nitric oxide activates soluble guanylyl cyclase (sGC) to produce cyclic guanosine monophosphate (cGMP). It improves oxygenation by increasing perfusion to well-ventilated lung regions as well as presents anti-inflammatory effects [125,126]. Prostaglandins have vasodilatory properties [127]. | Not approved. No clear benefits in outcome [125,126,127]. |
| Surfactants | Surfactants act by reducing alveolar surface tension, thus preventing alveolar collapse and limiting pulmonary edema. Surfactants also have anti-inflammatory and antimicrobial properties [128]. | Not approved. No clear benefits in outcome [128,129]. |
| Solnatide | Solnatide is a synthetic peptide mimicking the lectin-like domain of tumor necrosis factor. In ARDS, it reduces extravascular lung water (edema) and activates epithelial sodium channels, increases occludin expression, thus improving lung function [130]. | Not approved. No clear benefits in outcome [130]. |
| Dilmapimod | Dilmapimod is a p38 mitogen activated protein kinase. It reduces the levels of proinflammatory cytokines and chemokines as well as cell infiltration to inflammation sites [131]. | Not approved. No clear benefits in outcome [132]. |
| KGF and GM-CSF | KGF is a mitogen for specific different types of epithelial cells. In ARDS, KFG inhibits apoptosis and has mitogenic effects. GM-CSF stimulates maturation of alveolar epithelial cells [133,134]. | Not approved. No clear benefits in outcome [133,134,135]. |
| Nebulized heparin | In ARDS, nebulized heparin improves oxygenation and reduces lung edema [155]. | Not approved. No clear benefits in outcome [155]. |
| MSCs | MSCs modulate the immune response and reduce lung injury [136]. | Not approved. No clear benefits in outcome [136,137,138]. |
Disclaimer/Publisher’s Note: The statements, opinions and data contained in all publications are solely those of the individual author(s) and contributor(s) and not of MDPI and/or the editor(s). MDPI and/or the editor(s) disclaim responsibility for any injury to people or property resulting from any ideas, methods, instructions or products referred to in the content. |
© 2023 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Battaglini, D.; Fazzini, B.; Silva, P.L.; Cruz, F.F.; Ball, L.; Robba, C.; Rocco, P.R.M.; Pelosi, P. Challenges in ARDS Definition, Management, and Identification of Effective Personalized Therapies. J. Clin. Med. 2023, 12, 1381. https://doi.org/10.3390/jcm12041381
Battaglini D, Fazzini B, Silva PL, Cruz FF, Ball L, Robba C, Rocco PRM, Pelosi P. Challenges in ARDS Definition, Management, and Identification of Effective Personalized Therapies. Journal of Clinical Medicine. 2023; 12(4):1381. https://doi.org/10.3390/jcm12041381
Chicago/Turabian StyleBattaglini, Denise, Brigitta Fazzini, Pedro Leme Silva, Fernanda Ferreira Cruz, Lorenzo Ball, Chiara Robba, Patricia R. M. Rocco, and Paolo Pelosi. 2023. "Challenges in ARDS Definition, Management, and Identification of Effective Personalized Therapies" Journal of Clinical Medicine 12, no. 4: 1381. https://doi.org/10.3390/jcm12041381
APA StyleBattaglini, D., Fazzini, B., Silva, P. L., Cruz, F. F., Ball, L., Robba, C., Rocco, P. R. M., & Pelosi, P. (2023). Challenges in ARDS Definition, Management, and Identification of Effective Personalized Therapies. Journal of Clinical Medicine, 12(4), 1381. https://doi.org/10.3390/jcm12041381








