The Impact of Emergency Department Arrival Time on Door-to-Balloon Time in Patients with ST-Segment Elevation Myocardial Infarction Receiving Primary Percutaneous Coronary Intervention
Abstract
1. Introduction
2. Materials and Methods
2.1. Study Design, Settings, and Data Collection
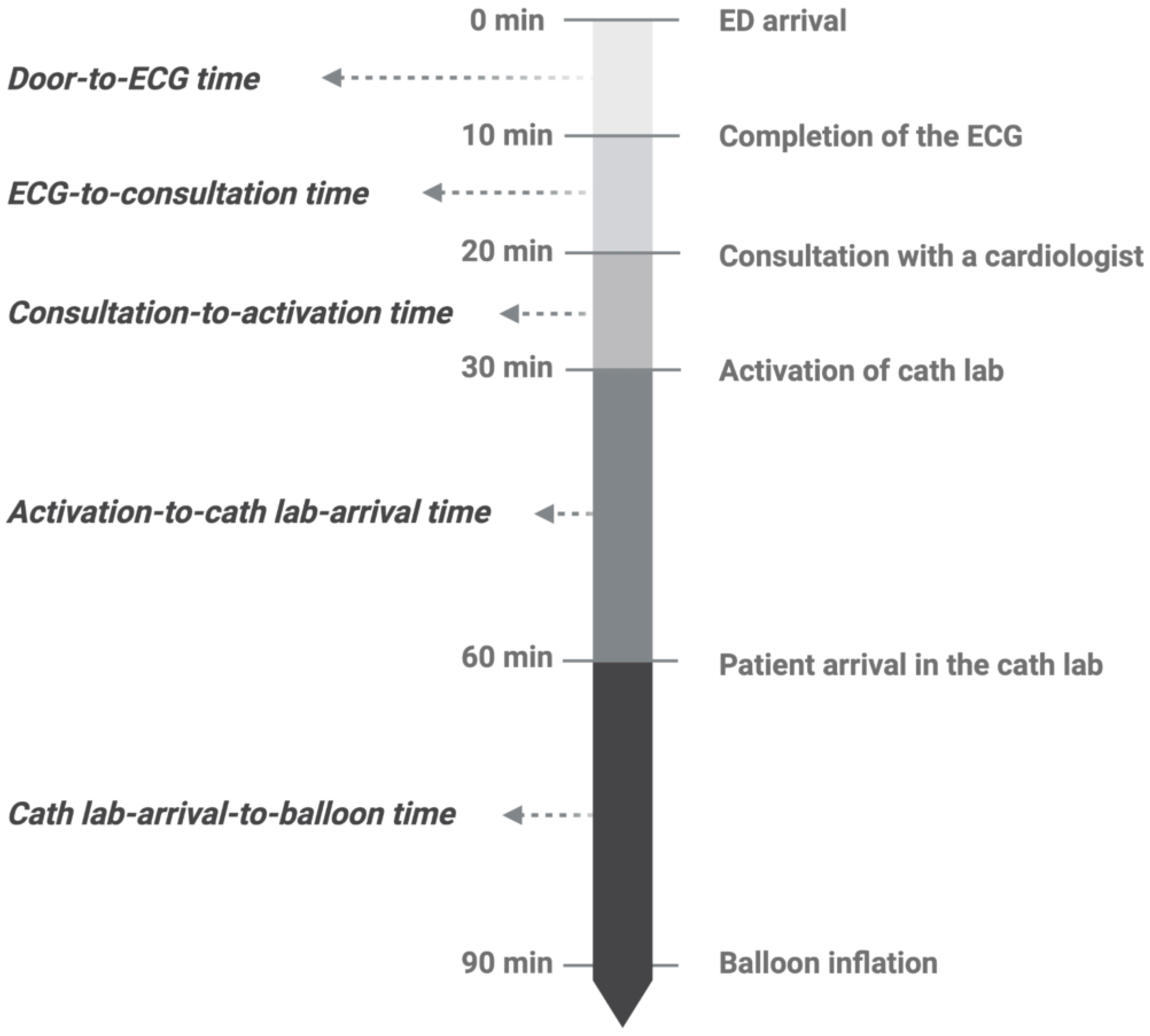
2.2. Patient Assignment and Outcome Measurement
2.3. Statistical Analysis
3. Results
3.1. Study Population
3.2. Baseline Characteristics
3.3. DTB Time and Time Segments of DTB Time
3.4. Temporal Differences and the Measured Outcomes
4. Discussion
5. Conclusions
Supplementary Materials
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Acknowledgments
Conflicts of Interest
References
- O’Gara, P.T.; Kushner, F.G.; Ascheim, D.D.; Casey, D.E.; Chung, M.K.; de Lemos, J.A.; Ettinger, S.M.; Fang, J.C.; Fesmire, F.M.; Franklin, B.A.; et al. 2013 ACCF/AHA guideline for the management of ST-elevation myocardial infarction. Circulation 2013, 127, e362–e425. [Google Scholar] [CrossRef]
- Ibanez, B.; James, S.; Agewall, S.; Antunes, M.J.; Bucciarelli-Ducci, C.; Bueno, H.; Caforio, A.L.P.; Crea, F.; Goudevenos, J.A.; Halvorsen, S.; et al. 2017 ESC guidelines for the management of acute myocardial infarction in patients presenting with ST-segment elevation: The task force for the management of acute myocardial infarction in patients presenting with ST-segment elevation of the European Society of Cardiology (ESC). Eur. Heart J. 2018, 39, 119–177. [Google Scholar] [CrossRef] [PubMed]
- Li, L.; Wu, M.Y.; Zhang, F.; Li, S.F.; Cui, Y.X.; Hu, D.; Chen, H. Perspective of delay in door-to-balloon time among Asian population. J. Geriatr. Cardiol. 2018, 15, 732–737. [Google Scholar] [CrossRef] [PubMed]
- Foo, C.Y.; Bonsu, K.O.; Nallamothu, B.K.; Reid, C.M.; Dhippayom, T.; Reidpath, D.D.; Chaiyakunapruk, N. Coronary intervention door-to-balloon time and outcomes in ST-elevation myocardial infarction: A meta-analysis. Heart 2018, 104, 1362–1369. [Google Scholar] [CrossRef] [PubMed]
- Tsukui, T.; Sakakura, K.; Taniguchi, Y.; Yamamoto, K.; Wada, H.; Momomura, S.I.; Fujita, H. Determinants of short and long door-to-balloon time in current primary percutaneous coronary interventions. Heart Vessel. 2018, 33, 498–506. [Google Scholar] [CrossRef]
- Erol, M.K.; Kayıkçıoğlu, M.; Kılıçkap, M.; Güler, A.; Öztürk, Ö.; Tuncay, B.; İnci, S.; Balaban, İ.; Tatar, F.; Çırakoğlu, Ö.F.; et al. Time delays in each step from symptom onset to treatment in acute myocardial infarction: Results from a nation-wide TURKMI registry. Anatol. J. Cardiol. 2021, 25, 294–303. [Google Scholar] [CrossRef] [PubMed]
- Atzema, C.L.; Austin, P.C.; Tu, J.V.; Schull, M.J. Emergency department triage of acute myocardial infarction patients and the effect on outcomes. Ann. Emerg. Med. 2009, 53, 736–745. [Google Scholar] [CrossRef]
- Noguchi, M.; Ako, J.; Morimoto, T.; Homma, Y.; Shiga, T.; Obunai, K.; Watanabe, H. Modifiable factors associated with prolonged door to balloon time in patients with ST-segment elevation myocardial infarction undergoing primary percutaneous coronary intervention. Heart Vessel. 2018, 33, 1139–1148. [Google Scholar] [CrossRef] [PubMed]
- Krishnan, S.V.; Ravi, M.; Abraham, S.V.; Palatty, B.U.; Balakrishnan, J.M. Door to balloon time in patients presenting with acute ST elevation myocardial infarction and time factors influencing it; an observational study from a tertiary care teaching hospital in India. Indian Heart J. 2021, 73, 359–361. [Google Scholar] [CrossRef] [PubMed]
- Sim, W.J.; Ang, A.S.; Tan, M.C.; Xiang, W.W.; Foo, D.; Loh, K.K.; Jafary, F.H.; Watson, T.J.; Ong, P.J.L.; Ho, H.H. Causes of delay in door-to-balloon time in south-east Asian patients undergoing primary percutaneous coronary intervention. PLoS ONE 2017, 12, e0185186. [Google Scholar] [CrossRef]
- Sadeghi, H.M.; Grines, C.L.; Chandra, H.R.; Mehran, R.; Fahy, M.; Cox, D.A.; Garcia, E.; Tcheng, J.E.; Griffin, J.J.; Stuckey, T.D.; et al. Magnitude and impact of treatment delays on weeknights and weekends in patients undergoing primary angioplasty for acute myocardial infarction (the Cadillac trial). Am. J. Cardiol. 2004, 94, 637–640. [Google Scholar] [CrossRef]
- Jayawardana, S.; Salas-Vega, S.; Cornehl, F.; Krumholz, H.M.; Mossialos, E. The Relationship between off-hours admissions for primary percutaneous coronary intervention, door-to-balloon time and mortality for patients with ST-elevation myocardial infarction in England: A registry-based prospective national cohort study. BMJ Qual. Saf. 2020, 29, 541–549. [Google Scholar] [CrossRef]
- Enezate, T.H.; Omran, J.; Al-Dadah, A.S.; Alpert, M.; Mahmud, E.; Patel, M.; Aronow, H.D.; Bhatt, D.L. Comparison of outcomes of ST-elevation myocardial infarction treated by percutaneous coronary intervention during off-hours versus on-hours. Am. J. Cardiol. 2017, 120, 1742–1754. [Google Scholar] [CrossRef] [PubMed]
- Sorita, A.; Ahmed, A.; Starr, S.R.; Thompson, K.M.; Reed, D.A.; Prokop, L.; Shah, N.D.; Murad, M.H.; Ting, H.H. Off-hour presentation and outcomes in patients with acute myocardial infarction: Systematic review and meta-analysis. BMJ 2014, 348, f7393. [Google Scholar] [CrossRef] [PubMed]
- Geng, J.; Ye, X.; Liu, C.; Xie, J.; Chen, J.; Xu, B.; Wang, B. Outcomes of off- and on-hours admission in ST-segment elevation myocardial infarction patients undergoing primary percutaneous coronary intervention: A retrospective observational cohort study. Medicine 2016, 95, e4093. [Google Scholar] [CrossRef] [PubMed]
- Fabbian, F.; Bhatia, S.; De Giorgi, A.; Maietti, E.; Bhatia, S.; Shanbhag, A.; Deshmukh, A. Circadian periodicity of ischemic heart disease: A systematic review of the literature. Heart Fail. Clin. 2017, 13, 673–680. [Google Scholar] [CrossRef]
- Lin, C.Y.; Lee, Y.C. Effectiveness of hospital emergency department regionalization and categorization policy on appropriate patient emergency care use: A nationwide observational study in Taiwan. BMC Health Serv. Res. 2021, 21, 21. [Google Scholar] [CrossRef]
- Joint Commission of Taiwan. Accreditation and Certification—Accreditation, Inspection, Certification—Hospital Accreditation and Certification. Available online: https://www.jct.org.tw/cp-1339-8352-44faf-2.html (accessed on 20 December 2022).
- Su, H.Y.; Tsai, J.L.; Hsu, Y.C.; Lee, K.H.; Chang, C.S.; Sun, C.K.; Wang, Y.H.; Chi, S.C.; Hsu, C.W. A modified cardiac triage strategy reduces door to ECG time in patients with ST elevation myocardial infarction. Sci. Rep. 2021, 11, 6358. [Google Scholar] [CrossRef]
- Yates, R.B.; Hiestand, B.C. Effects of age, race, and sex on door-to-electrocardiogram time in emergency department non-ST elevation acute coronary syndrome patients. J. Emerg. Med. 2011, 40, 123–127. [Google Scholar] [CrossRef] [PubMed]
- Nakahashi, T.; Sakata, K.; Masuda, J.; Kumagai, N.; Higuma, T.; Ogimoto, A.; Tanigawa, T.; Hanada, H.; Nakamura, M.; Takamura, M.; et al. Comparison of door-to-balloon time and 30-day mortality according to symptom presentation in patients with acute myocardial infarction. Circ. Rep. 2021, 3, 194–200. [Google Scholar] [CrossRef]
- Dreyer, R.P.; Beltrame, J.F.; Tavella, R.; Air, T.; Hoffmann, B.; Pati, P.K.; Di Fiore, D.; Arstall, M.; Zeitz, C. Evaluation of gender differences in door-to-balloon time in ST-elevation myocardial infarction. Heart Lung Circ. 2013, 22, 861–869. [Google Scholar] [CrossRef]
- Chew, N.W.S.; Sia, C.H.; Wee, H.L.; Benedict, L.J.-D.; Rastogi, S.; Kojodjojo, P.; Chor, W.P.D.; Leong, B.S.; Koh, B.C.; Tam, H.; et al. Impact of the COVID-19 pandemic on door-to-balloon time for primary percutaneous coronary intervention—Results from the Singapore western STEMI network. Circ. J. 2021, 85, 139–149. [Google Scholar] [CrossRef]
- Mously, H.; Shah, N.; Zuzek, Z.; Alshaghdali, I.; Karim, A.; Jaswaney, R.; Filby, S.J.; Simon, D.I.; Shishehbor, M.H.; Forouzandeh, F. Door-to-balloon time for ST-elevation MI in the coronavirus disease 2019 Era. US Cardiol. Rev. 2021, 15, e13. [Google Scholar] [CrossRef]
- De Luca, G.; Algowhary, M.; Uguz, B.; Oliveira, D.C.; Ganyukov, V.; Zimbakov, Z.; Cercek, M.; Jensen, L.O.; Loh, P.H.; Calmac, L.; et al. COVID-19 pandemic, mechanical reperfusion and 30-day mortality in ST elevation myocardial infarction. Heart 2022, 108, 458–466. [Google Scholar] [CrossRef] [PubMed]
- Kobayashi, S.; Sakakura, K.; Jinnouchi, H.; Taniguchi, Y.; Tsukui, T.; Watanabe, Y.; Yamamoto, K.; Seguchi, M.; Wada, H.; Fujita, H. Comparison of door-to-balloon time and in-hospital outcomes in patients with ST-elevation myocardial infarction between before versus after COVID-19 pandemic. Cardiovasc. Interv. Ther. 2022, 37, 641–650. [Google Scholar] [CrossRef]
- Ryu, S.; Kim, D.; Jung, L.Y.; Kim, B.; Lee, C.S. Decreased door-to-balloon time in patients with ST-segment elevation myocardial infarction during the early COVID-19 pandemic in South Korea: An observational study. Medicine 2022, 101, e29596. [Google Scholar] [CrossRef] [PubMed]
- Tungsubutra, W.; Ngoenjan, D. Door-to-balloon time and factors associated with delayed door-to-balloon time in ST-segment elevation myocardial infarction at Thailand’s largest tertiary referral centre. J. Eval. Clin. Pract. 2019, 25, 434–440. [Google Scholar] [CrossRef] [PubMed]
- Bradley, E.H.; Herrin, J.; Wang, Y.; Barton, B.A.; Webster, T.R.; Mattera, J.A.; Roumanis, S.A.; Curtis, J.P.; Nallamothu, B.K.; Magid, D.J.; et al. Strategies for reducing the door-to-balloon time in acute myocardial infarction. N. Engl. J. Med. 2006, 355, 2308–2320. [Google Scholar] [CrossRef]
- Mahmud, E.; Dauerman, H.L.; Welt, F.G.P.; Messenger, J.C.; Rao, S.V.; Grines, C.; Mattu, A.; Kirtane, A.J.; Jauhar, R.; Meraj, P.; et al. Management of acute myocardial infarction during the COVID-19 pandemic: A position statement from the Society for Cardiovascular Angiography and Interventions (SCAI), the American College of Cardiology (ACC), and the American College of Emergency Physicians (ACEP). J. Am. Coll. Cardiol. 2020, 76, 1375–1384. [Google Scholar] [CrossRef] [PubMed]
- Chew, N.W.S.; Ow, Z.G.W.; Teo, V.X.Y.; Heng, R.R.Y.; Ng, C.H.; Lee, C.H.; Low, A.F.; Chan, M.Y.; Yeo, T.C.; Tan, H.C.; et al. The global effect of the COVID-19 pandemic on STEMI care: A systematic review and meta-analysis. Can. J. Cardiol. 2021, 37, 1450–1459. [Google Scholar] [CrossRef] [PubMed]


| Time of ED Visit | ||||||||||
|---|---|---|---|---|---|---|---|---|---|---|
| Daytime 08:01–16:00 (n = 327) | Evening 16:01–24:00 (n = 268) | Nighttime 00:01–08:00 (n = 137) | p-Value | |||||||
| Demographics | ||||||||||
| Age (year) | 63.8 | (12.7) | 60.2* | (13.1) | 61.0 | (13.6) | 0.003 | |||
| Body weight (kg) | 67.7 | (60.0–76.2) | (n = 325) | 68.2 | (60.0–77.0) | (n = 265) | 70.2 | (59.9–80.0) | (n = 134) | 0.284 |
| BMI | 25.1 | (3.5) | (n = 325) | 25.5 | (4.2) | (n = 265) | 25.7 | (4.3) | (n = 134) | 0.284 |
| Triage vital signs | ||||||||||
| BT (°C) | 36.0 | (35.5–36.4) | (n = 326) | 36.0 | (35.5–36.5) | 35.9 *,# | (35.2–36.2) | 0.013 | ||
| HR (bpm) | 72.0 | (60.0–87.0) | 76.0 | (65.0–89.0) | (n = 265) | 75.0 | (61.0–89.0) | 0.074 | ||
| SBP (mmHg) | 133.0 | (32.4) | (n = 326) | 136.8 | (32.7) | (n = 264) | 132.3 | (33.3) | 0.282 | |
| DBP (mmHg) | 84.3 | (20.3) | (n = 326) | 86.8 | (21.7) | (n = 264) | 84.6 | (19.4) | 0.336 | |
| SpO2 (%) | 97.0 | (95.0–98.0) | (n = 177) | 97.0 | (96.0–99.0) | (n = 125) | 97.0 | (95.0–98.0) | (n = 79) | 0.885 |
| Laboratory test results | ||||||||||
| WBC count (×1000/uL) | 10.4 | (8.3–13.0) | 10.5 | (8.7–12.2) | 10.4 | (8.4–13.2) | 0.989 | |||
| Troponin-I level (ng/mL) | 0.2 | (0.0–3.8) | (n = 325) | 0.1 | (0.0–2.2) | 0.2 | (0.0–2.9) | 0.533 | ||
| EF for cardiac echo (%) | 57.0 | (48.0–65.0) | (n = 313) | 56.0 | (47.1–65.0) | (n = 261) | 57.4 | (46.9–63.3) | (n = 135) | 0.824 |
| Duration of hospitalization (days) | 5.0 | (4.0–6.0) | 5.0 | (4.0–6.0) | 4.0 | (3.0–6.0) | 0.256 | |||
| Time interval (min) | ||||||||||
| Door-to-ECG time | 4.0 | (3.0–6.0) | 5.0 | (3.0–6.0) | 5.0 | (3.0–6.0) | 0.872 | |||
| ECG-to-consultation time | 5.0 | (2.0–9.0) | 5.0 | (3.0–8.0) | 5.0 | (3.0–12.0) | 0.161 | |||
| Consultation-to-activation time | 4.0 | (2.0–7.0) | 4.0 | (2.0–6.0) | 5.0 *,# | (3.0–9.0) | <0.001 | |||
| Activation-to-cath lab-arrival time | 17.0 | (13.0–25.0) | 27.0 * | (19.8–33.0) | 28.0 * | (22.0–35.0) | <0.001 | |||
| Cath lab-arrival-to-balloon time | 21.0 | (15.0–29.0) | 23.0 | (17.0–28.3) | 23.0 | (18.0–28.0) | 0.063 | |||
| Door-to-balloon time | 57.0 | (47.0–72.0) | 67.0 * | (57.0–76.3) | 72.0 *,# | (63.0–84.0) | <0.001 | |||
| Time of ED Visit | |||||||
|---|---|---|---|---|---|---|---|
| Daytime 08:01–16:00 (n = 327) | Evening 16:01–24:00 (n = 268) | Nighttime 00:01–08:00 (n = 137) | p-Value | ||||
| n | (%) | n | (%) | n | (%) | ||
| Age group | 0.010 | ||||||
| <65 years | 170 | (51.99) | 174 | (64.93) | 87 | (63.50) | |
| 65–75 years | 92 | (28.13) | 52 | (19.40) | 24 | (17.52) | |
| ≥75 years | 65 | (19.88) | 42 | (15.67) | 26 | (18.98) | |
| Female sex | 56 | (17.13) | 45 | (16.79) | 18 | (13.14) | 0.544 |
| Season | 0.256 | ||||||
| Spring | 77 | (23.55) | 61 | (22.76) | 40 | (29.20) | |
| Summer | 76 | (23.24) | 68 | (25.37) | 24 | (17.52) | |
| Fall | 86 | (26.30) | 63 | (23.51) | 43 | (31.39) | |
| Winter | 88 | (26.91) | 76 | (28.36) | 30 | (21.90) | |
| ED visit time | 0.876 | ||||||
| Weekday | 228 | (69.72) | 192 | (71.64) | 97 | (70.80) | |
| Weekend | 99 | (30.28) | 76 | (28.36) | 40 | (29.20) | |
| During COVID-19 pandemic (2020–2021) | 76 | (23.24) | 51 | (19.03) | 24 | (17.52) | 0.274 |
| Ambulance-transported patient | 88 | (26.91) | 67 | (25.00) | 33 | (24.09) | 0.776 |
| Triage level | 0.094 | ||||||
| 1 | 28 | (8.56) | 28 | (10.45) | 23 | (16.79) | |
| 2 | 268 | (81.96) | 221 | (82.46) | 102 | (74.45) | |
| 3 | 31 | (9.48) | 19 | (7.09) | 12 | (8.76) | |
| Medical history | |||||||
| DM | 131 | (40.06) | 102 | (38.06) | 55 | (40.15) | 0.864 |
| HTN | 213 | (65.14) | 171 | (63.81) | 87 | (63.50) | 0.920 |
| Hyperlipidemia | 197 | (60.24) | 168 | (62.69) | 77 | (56.20) | 0.450 |
| CVA | 27 | (8.26) | 22 | (8.21) | 6 | (4.38) | 0.304 |
| CKD | 31 | (9.48) | 14 | (5.22) | 12 | (8.76) | 0.140 |
| ESRD | 9 | (2.75) | 8 | (2.99) | 1 | (0.73) | 0.344 |
| CAD | 51 | (15.60) | 31 | (11.57) | 19 | (13.87) | 0.366 |
| COPD | 13 | (3.98) | 6 | (2.24) | 3 | (2.19) | 0.385 |
| PAOD | 4 | (1.22) | 2 | (0.75) | 3 | (2.21) | 0.454 |
| Smoking | 192 | (58.72) | 167 | (62.31) | 80 | (58.39) | 0.616 |
| ECG report | |||||||
| Anterior STEMI | 151 | (46.18) | 124 | (46.27) | 61 | (44.53) | 0.938 |
| Inferior STEMI | 160 | (48.93) | 138 | (51.69) | 67 | (49.26) | 0.786 |
| Lateral STEMI | 14 | (4.28) | 11 | (4.12) | 0 | (0.00) | 0.051 |
| Posterior STEMI | 3 | (0.92) | 7 | (2.62) | 2 | (1.47) | 0.263 |
| LBBB | 1 | (0.31) | 1 | (0.37) | 2 | (1.46) | 0.273 |
| AV block | 28 | (8.56) | 18 | (6.72) | 14 | (10.22) | 0.453 |
| Findings of coronary angiography | |||||||
| 1-vessel disease | 88 | (27.00) | 83 | (30.97) | 49 | (35.77) | 0.527 |
| 2-vessel disease | 123 | (37.73) | 98 | (36.57) | 41 | (29.93) | |
| 3-vessel disease | 114 | (34.97) | 86 | (32.09) | 47 | (34.31) | |
| LM occlusion | 12 | (3.67) | 16 | (5.97) | 7 | (5.11) | 0.416 |
| LAD occlusion (≥50%) | 262 | (80.12) | 215 | 80.22) | 109 | (79.56) | 0.987 |
| LCX occlusion (≥50%) | 170 | (51.99) | 125 | (46.64) | 68 | (49.64) | 0.431 |
| RCA occlusion (≥50%) | 226 | (69.11) | 187 | (69.78) | 88 | (64.23) | 0.494 |
| Time interval | |||||||
| Door-to-ECG > 10 min | 24 | (7.34) | 17 | (6.34) | 12 | (8.76) | 0.672 |
| ECG-to-consultation > 10 min | 59 | (18.04) | 53 | (19.78) | 37 | (27.01) | 0.087 |
| Consultation-to-activation > 10 min | 37 | (11.31) | 25 | (9.33) | 21 | (15.33) | 0.197 |
| Activation-to-cath lab-arrival > 30 min | 43 | (13.15) | 81 | (30.22) | 57 | (41.61) | <0.001 |
| Cath lab-arrival-to-balloon time > 30 min | 72 | (22.02) | 58 | (21.64) | 28 | (20.44) | 0.931 |
| Door-to-balloon time > 90 min | 22 | (6.73) | 27 | (10.07) | 22 | (16.06) | 0.008 |
| Parameters | OR | 95% CI | p-Value | aOR | 95% CI | p-Value |
|---|---|---|---|---|---|---|
| Age (per year) | 1.02 | (1.00–1.04) | 0.019 | – | ||
| Female sex | 2.41 | (1.39–4.19) | 0.002 | 2.44 | (1.37–4.32) | 0.002 |
| Weekend | 0.94 | (0.54–1.61) | 0.815 | – | ||
| During COVID-19 pandemic | 0.60 | (0.30–1.21) | 0.155 | – | ||
| Triage level | ||||||
| 1 | Reference | Reference | ||||
| 2 | 0.58 | (0.28–1.21) | 0.146 | 0.67 | (0.32–1.40) | 0.283 |
| 3 | 2.20 | (0.91–5.32) | 0.079 | 2.42 | (0.97–6.00) | 0.058 |
| Lateral wall STEMI | 0.80 | (0.19–3.47) | 0.767 | – | ||
| ED visit time | ||||||
| 08:01–16:00 | Reference | Reference | ||||
| 16:01–24:00 | 1.55 | (0.86–2.80) | 0.142 | 1.66 | (0.91–3.03) | 0.097 |
| 00:01–08:00 | 2.65 | (1.41–4.97) | 0.002 | 2.87 | (1.50–5.51) | 0.002 |
| Door-to-ECG > 10 min | ECG-to-Consultation > 10 min | Consultation-to-Activation > 10 min | Activation-to-Cath Lab-Arrival > 30 min | Cath Lab-Arrival-to-Balloon Time > 30 min | |||||||||||
|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|
| Parameters | aOR | 95% CI | p-Value | aOR | 95% CI | p-Value | aOR | 95% CI | p-Value | aOR | 95% CI | p-Value | aOR | 95% CI | p-Value |
| Age (per year) | 1.03 | (1.00–1.06) | 0.030 | – | – | – | – | ||||||||
| Female sex | 3.23 | (1.63–6.39) | <0.001 | – | – | – | – | ||||||||
| Weekend | – | – | – | 2.11 | (1.44–3.11) | <0.001 | – | ||||||||
| During COVID-19 pandemic | – | – | 2.06 | (1.25–3.41) | 0.005 | 4.66 | (3.06–7.10) | <0.001 | 0.52 | (0.32–0.86) | 0.011 | ||||
| Triage level | |||||||||||||||
| 1 | Reference | Reference | |||||||||||||
| 2 | 0.44 | (0.19–1.00) | 0.049 | 1.14 | (0.76–1.73) | 0.530 | – | – | – | ||||||
| 3 | 3.05 | (1.17–7.95) | 0.023 | 1.69 | (1.05–2.72) | 0.031 | – | – | – | ||||||
| Lateral wall STEMI | – | – | – | – | – | ||||||||||
| ED visit time | |||||||||||||||
| 08:01–16:00 | Reference | Reference | Reference | Reference | Reference | ||||||||||
| 16:01–24:00 | 1.02 | (0.51–2.03) | 0.956 | 0.85 | (0.48–1.50) | 0.567 | 0.84 | (0.49–1.43) | 0.516 | 3.53 | (2.26–5.54) | <0.001 | 0.94 | (0.63–1.39) | 0.751 |
| 00:01–08:00 | 1.38 | (0.63–3.01) | 0.425 | 1.60 | (0.75–3.41) | 0.229 | 1.51 | (0.84–2.70) | 0.168 | 6.25 | (3.75–10.40) | <0.001 | 0.89 | (0.54–1.46) | 0.638 |
Disclaimer/Publisher’s Note: The statements, opinions and data contained in all publications are solely those of the individual author(s) and contributor(s) and not of MDPI and/or the editor(s). MDPI and/or the editor(s) disclaim responsibility for any injury to people or property resulting from any ideas, methods, instructions or products referred to in the content. |
© 2023 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Hsiao, Y.-T.; Hung, J.-F.; Zhang, S.-Q.; Yeh, Y.-N.; Tsai, M.-J. The Impact of Emergency Department Arrival Time on Door-to-Balloon Time in Patients with ST-Segment Elevation Myocardial Infarction Receiving Primary Percutaneous Coronary Intervention. J. Clin. Med. 2023, 12, 2392. https://doi.org/10.3390/jcm12062392
Hsiao Y-T, Hung J-F, Zhang S-Q, Yeh Y-N, Tsai M-J. The Impact of Emergency Department Arrival Time on Door-to-Balloon Time in Patients with ST-Segment Elevation Myocardial Infarction Receiving Primary Percutaneous Coronary Intervention. Journal of Clinical Medicine. 2023; 12(6):2392. https://doi.org/10.3390/jcm12062392
Chicago/Turabian StyleHsiao, Yu-Ting, Jui-Fu Hung, Shi-Quan Zhang, Ya-Ni Yeh, and Ming-Jen Tsai. 2023. "The Impact of Emergency Department Arrival Time on Door-to-Balloon Time in Patients with ST-Segment Elevation Myocardial Infarction Receiving Primary Percutaneous Coronary Intervention" Journal of Clinical Medicine 12, no. 6: 2392. https://doi.org/10.3390/jcm12062392
APA StyleHsiao, Y.-T., Hung, J.-F., Zhang, S.-Q., Yeh, Y.-N., & Tsai, M.-J. (2023). The Impact of Emergency Department Arrival Time on Door-to-Balloon Time in Patients with ST-Segment Elevation Myocardial Infarction Receiving Primary Percutaneous Coronary Intervention. Journal of Clinical Medicine, 12(6), 2392. https://doi.org/10.3390/jcm12062392






