Strategies for Safe Implantation and Effective Performance of Single-Chamber and Dual-Chamber Leadless Pacemakers
Abstract
:1. Introduction
2. Leadless Ventricular Pacemakers
2.1. Brief History and Current State of Two Leadless Systems
2.2. Evaluation of Clinical Performance and Recommendation of Strategies
2.2.1. Cardiac Perforation and Pericardial Effusion
2.2.2. Dislodgment
2.2.3. Vascular Complications
2.2.4. Infection
2.2.5. Tricuspid Valve Regurgitation
2.3. Gaps in Experience
3. Leadless AV Synchronization
3.1. Brief Introduction of the Algorithm of the Micra AV
3.2. Evaluation of the AV Synchrony and Recommendation of Strategies
- A.
- Patients’ factors:
- (a)
- Patient characteristics: High AV synchrony was associated with a lower BMI, a lower proportion of congestive heart failure, a history of cardiac surgery, and pulmonary hypertension [71]. It is a hypothesis the A4 amplitude was negatively related to a history of coronary artery bypass grafting due to the ischemia-inducing reduced atrial contractions [76];
- (b)
- Electrocardiogram (ECG): Some cases of low AV synchrony could be related to sinus rates < 50/min [15], and an analysis in a real-world setting of outpatients indicated that the median AV synchrony was 91% when the patients had sinus rates of 50–80/min, and that it decreased to 33% when the patients had sinus rates of >80/min [72]. Therefore, a sinus rate of 50–80/min contributes to high AV synchrony. Several kinds of arrhythmia, such as a sinus rate variability of >5 bpm at rest [76], AF/atrial flutter [71], and a high premature atrial/ventricular complex [15], are associated with lower AV synchrony. The A4 amplitude was positively correlated with p-wave amplitude in lead aVR [76];
- (c)
- Echocardiography: A higher A wave in the echocardiography reflects a stronger atrial contraction and a greater possibility of being discerned by the Mica AV. In a past study, the authors demonstrated that an E/A ratio of <0.94 indicated a high AV synchrony [76], in comparison with an E/A ratio of >1.5, which is considered a contraindication to Micra AV implantation. A small-sample study indicated that an A wave velocity > 73 cm/s could predict appropriate atrial sensing [77];
- (d)
- Maneuver and posture: The AV synchrony ranged from 89.2% during resting to 69.8% during standing, and to 74.7% during fast walking [16]. The higher sinus rate and volatile direction of the acceleration during activity could influence the sensing of atrial mechanical contraction, as reflected by the lower ambulatory AV synchrony of 74.7% a real-world setting [68], compared with that of 80.0% in a clinical trial for patients with AV blocks [15]. Hence, the Micra AV is more suitable for patients with sedentary lifestyles.
- B.
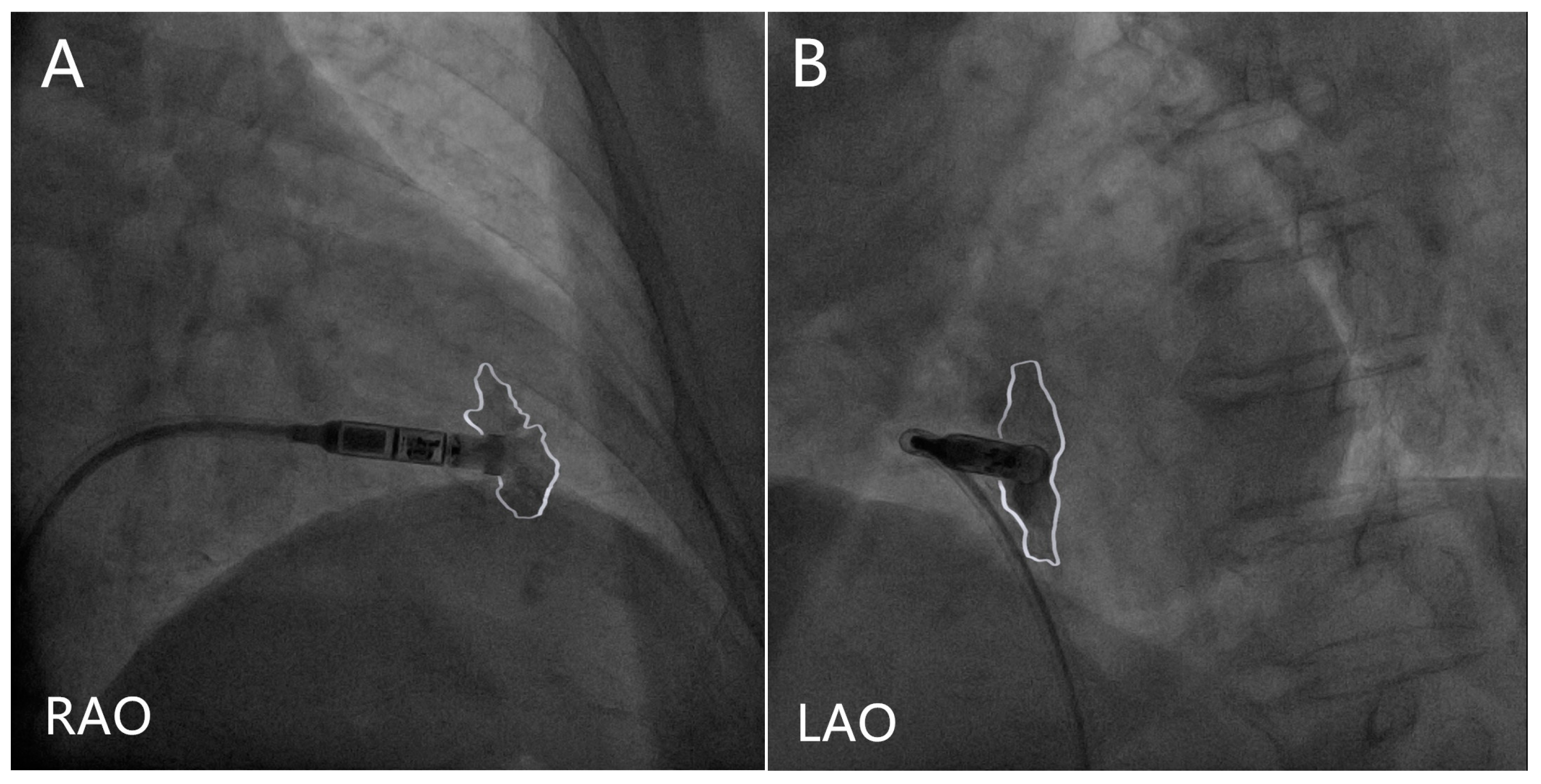
- Procedure technique: The Micra AV implant location has not been reported to have a significant influence on the AV synchrony [16] or A4 amplitude [76]. In terms of the implant location selection, physicians should take the electrical parameters of the RV and relevant complications into consideration; however, the AV synchrony cannot be evaluated or mediated during the procedure, which is another drawback of the Mica AV hardware design.
- C.
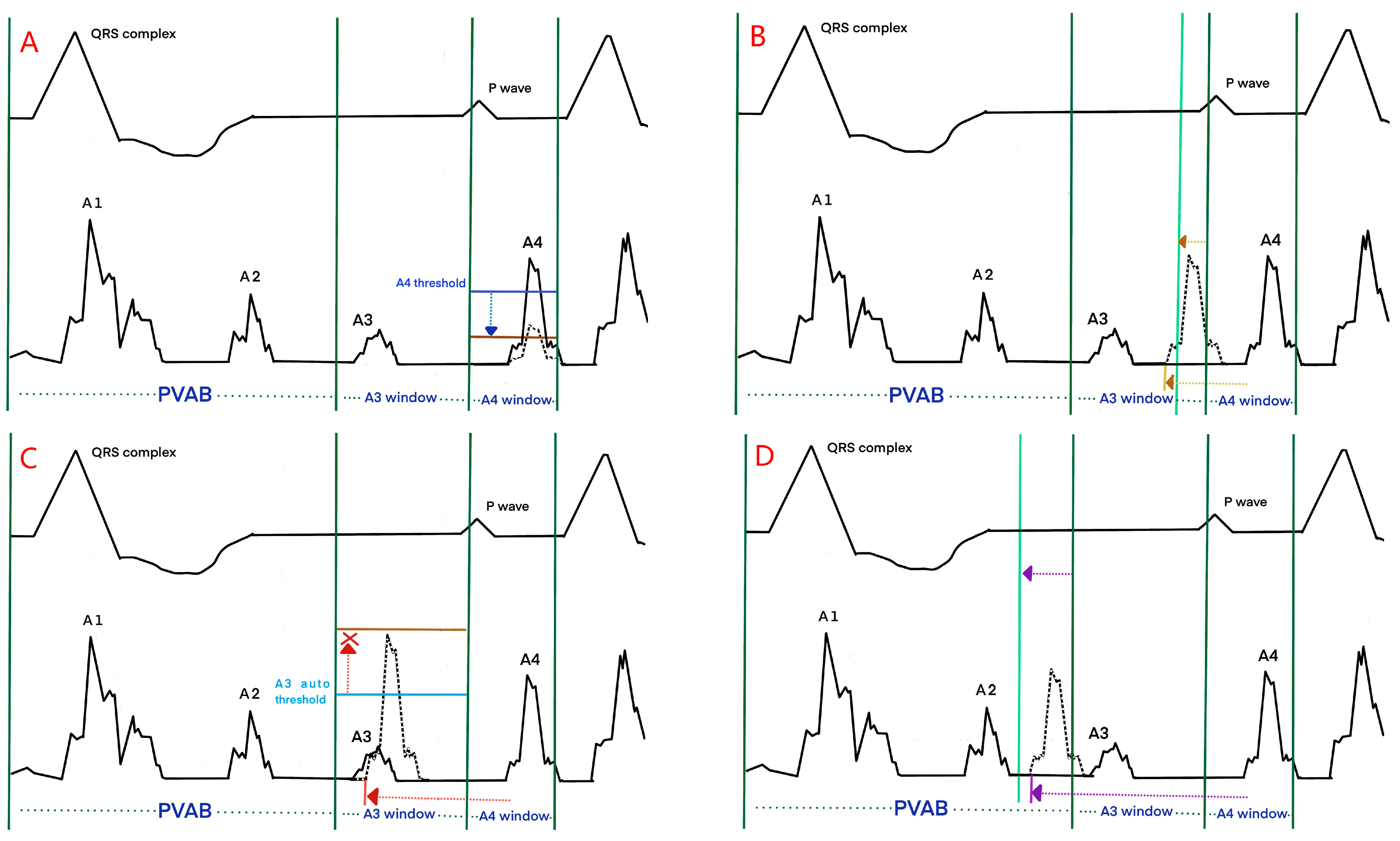
- Device programming: The nominal values of the Micra AV were optimized for patients during resting. Regular postimplant device reprogramming is necessary and should be individually optimized. The manual atrial mechanical (MAM) test is to line up A1–A4 signals with the corresponding surface ECG signals (Figure 2). Firstly, the MAM test with “auto” atrial mechanical features turned-off runs in the VDI mode to allow a clear distinction of the A1–A4 signals, and subsequently, MAM test runs in the VDD mode to make adjustment based on the track of atrial activity. The systematic and stepwise approaches including MAM test and adjustments of the A4 threshold, A3 window, and A3 threshold are to accurately discern A4 [78,79].
- a.
- The A4 threshold: In situations of low A4 amplitudes, a lower A4 threshold facilitates a reduction in the under-sensed A4 and improves the AV synchrony [72,73]; Meanwhile, in the case of low A4 amplitudes, the device’s built-in 3-axis accelerometer atrial-sensing vectors can be changed from a selection of one or two vectors to a recruitment of all three vectors to improve AV synchrony at the cost of negative impact on battery longevity [78,79]. When the A4 threshold is too low, the over-sensed A4 could impair the AV synchrony, which was observed in a study in which a higher A4 threshold was found to be related to a higher AV synchrony [74] (Figure 3A);
- b.
- The A3 window end: In situations of sinus tachycardia, the A4 signal falls in the A3 window, which reduces the AV synchrony. A shorter A3 window end interval for detecting the A4 signal and improving the AV synchrony has been confirmed in multiple studies [72,73,74]. A rate-dependent A3 window may be promising for tracking atrial contractions at higher heart rates. However, some researchers have suggested setting the A3 window below 700 ms and deactivating the automatic adjustment to improve the AV synchrony [74] (Figure 3B);
- c.
- The A3 threshold: In situations of sinus tachycardia, the A4 signal begins with the encroachment into the A3 window; however, as the heart rate is further elevated, the A4 signal could merge with the A3 signal and the A3 auto threshold function could result in the under-sensing of A4. Turning the A3 auto threshold function off and fixing the A3 threshold contribute to AV synchrony, and this is especially suitable for elevated sinus rates of 80–110/min [71]. A lower A3 threshold could improve the AV synchrony [74,76] (Figure 3C);
- d.
- The PVAB: In situations of Wenckebach behavior, the progressive shortening of the RP interval means that the P wave falls in the PVAB period, which results in the intermittent loss of A4 [76]. Shortening the PVAB to minimize the p-wave blanking is recommended. Wenckebach behavior occurs in patients with intrinsic conduction for whom the AV synchrony is high; therefore, the benefit of shortening PVAB is limited (Figure 3D);
- e.
- AV conduction mode switch: The algorithm of the Micra AV assumes intact intrinsic conduction in cases of ventricular rates of >40/min by default, and it switches to VVI-40 and VVIR pacing [16] if this function is activated. However, in situations of 2:1 AV blocks with sinus rates of ≥80/min, or complete AV blocks with ventricular escape beats of ≥40/min, such a function decreases the AV synchrony, and the recommendation is to switch it off [73,80];
- f.
- Rate smoothing feature: This feature was delivered at a rate smoothing interval (typically 100 ms) longer than the median R-R interval if A4 was not detected and improved the AV synchrony by 9% [15]. In situations of high sinus rate variability or high/low sinus rates, the efficacy of such a feature is somewhat compromised. Some studies suggested programming the rate smoothing interval longer than 100ms in patients with high sinus rate variabilities and low sinus rates [68], and programming the interval to 50 ms in patients with sinus rates of >90/min [16];
- g.
4. Selection Strategy for LPMs vs. TPMs
4.1. Selection Strategy for VVI-LPMs vs. DDD-TPMs
4.2. Selection Strategy for VDD-LPMs vs. DDD-TPMs
4.3. Conduction System Pacing
5. Leadless Atrial Pacemakers
6. Dual-Chamber Leadless and Battery-Less Pacemakers
6.1. The Conception of True Dual-Chamber Leadless and Battery-Less Pacemakers
6.2. Communication Technology for the Realization of Dual-Chamber Leadless Pacemakers
6.2.1. Radio-Frequency (RF) Communication
6.2.2. Conductive Intracardiac Communication (CIC)
6.3. Energy Programs for the Realization of Dual-Chamber Battery-Less Pacemakers
6.3.1. Acoustic Energy
6.3.2. RF Energy
6.3.3. Kinetic Energy
7. Conclusions
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Conflicts of Interest
References
- Raatikainen, M.J.P.; Arnar, D.O.; Zeppenfeld, K.; Merino, J.L.; Levya, F.; Hindriks, G.; Kuck, K.H. Statistics on the use of cardiac electronic devices and electrophysiological procedures in the European Society of Cardiology countries: 2014 report from the European Heart Rhythm Association. Europace 2015, 17, i1–i75. [Google Scholar] [PubMed] [Green Version]
- Pakarinen, S.; Oikarinen, L.; Toivonen, L. Short-term implantation-related complications of cardiac rhythm management device therapy: A retrospective single-centre 1-year survey. Europace 2010, 12, 103–108. [Google Scholar] [PubMed]
- Udo, E.O.; Zuithoff, N.P.; van Hemel, N.M.; de Cock, C.C.; Hendriks, T.; Doevendans, P.A.; Moons, K.G. Incidence and predictors of short- and long-term complications in pacemaker therapy: The FOLLOWPACE study. Heart Rhythm 2012, 9, 728–735. [Google Scholar] [CrossRef] [PubMed]
- Kirkfeldt, R.E.; Johansen, J.B.; Nohr, E.A.; Jorgensen, O.D.; Nielsen, J.C. Complications after cardiac implantable electronic device implantations: An analysis of a complete, nationwide cohort in Denmark. Eur. Heart J. 2014, 35, 1186–1194. [Google Scholar] [PubMed] [Green Version]
- Cho, M.S.; Kim, J.; Lee, J.B.; Nam, G.B.; Choi, K.J.; Kim, Y.H. Incidence and predictors of moderate to severe tricuspid regurgitation after dual-chamber pacemaker implantation. Pacing Clin. Electrophysiol. 2019, 42, 85–92. [Google Scholar]
- Malagù, M.; Vitali, F.; Brieda, A.; Cimaglia, P.; De Raffele, M.; Tazzari, E.; Musolino, C.; Balla, C.; Serenelli, M.; Cultrera, R.; et al. Antibiotic prophylaxis based on individual infective risk stratification in cardiac implantable electronic device: The practice study. Europace 2022, 24, 413–420. [Google Scholar]
- Cantillon, D.J.; Exner, D.V.; Badie, N.; Davis, K.; Gu, N.Y.; Nabutovsky, Y.; Doshi, R. Complications and health care costs associated with transvenous cardiac pacemakers in a nationwide assessment. JACC Clin. Electrophysiol. 2017, 3, 1296–1305. [Google Scholar]
- Cantillon, D.J.; Dukkipati, S.R.; Ip, J.H.; Exner, D.V.; Niazi, I.K.; Banker, R.S.; Rashtian, M.; Plunkitt, K.; Tomassoni, G.F.; Nabutovsky, Y.; et al. Comparative study of acute and mid-term complications with leadless and transvenous cardiac pacemakers. Heart Rhythm 2018, 15, 1023–1030. [Google Scholar]
- El-Chami, M.F.; Bockstedt, L.; Longacre, C.; Higuera, L.; Stromberg, K.; Crossley, G.; Kowal, R.C.; Piccini, J.P. Leadless vs. transvenous single-chamber ventricular pacing in the Micra CED study: 2-year follow-up. Eur. Heart J. 2022, 43, 1207–1215. [Google Scholar]
- Sperzel, J.; Defaye, P.; Delnoy, P.P.; Garcia Guerrero, J.J.; Knops, R.E.; Tondo, C.; Deharo, J.C.; Wong, T.; Neuzil, P. Primary safety results from the LEADLESS Observational Study. Europace 2018, 20, 1491–1497. [Google Scholar]
- Lakkireddy, D.; Knops, R.; Atwater, B.; Neuzil, P.; Ip, J.; Gonzalez, E.; Friedman, P.; Defaye, P.; Exner, D.; Aonuma, K.; et al. A worldwide experience of the management of battery failures and chronic device retrieval of the nanostim leadless pacemaker. Hear Rhythm 2017, 14, 1756–1763. [Google Scholar]
- Reddy, V.Y.; Exner, D.V.; Doshi, R.; Tomassoni, G.; Bunch, T.J.; Estes, N.A.M.; Neužil, P.; Paulin, F.L.; Garcia Guerrero, J.J.; Cantillon, D.J.; et al. Primary results on safety and efficacy from the LEADLESS II-phase 2 worldwide clinical trial. JACC Clin. Electrophysiol. 2022, 8, 115–117. [Google Scholar] [CrossRef] [PubMed]
- Piccini, J.P.; Stromberg, K.; Jackson, K.P.; Kowal, R.C.; Duray, G.Z.; El-Chami, M.F.; Crossley, G.H.; Hummel, J.D.; Narasimhan, C.; Omar, R.; et al. Patient selection, pacing indications, and subsequent outcomes with de novo leadless single-chamber VVI pacing. Europace 2019, 21, 1686–1693. [Google Scholar]
- Steinwender, C.; Lercher, P.; Schukro, C.; Blessberger, H.; Prenner, G.; Andreas, M.; Kraus, J.; Ammer, M.; Stühlinger, M. State of the art: Leadless ventricular pacing:a national expert consensus of the Austrian Society of Cardiology. J. Interv. Card. Electrophysiol. 2020, 57, 27–37. [Google Scholar] [PubMed] [Green Version]
- Chinitz, L.; Ritter, P.; Khelae, S.K.; Iacopino, S.; Garweg, C.; Grazia-Bongiorni, M.; Neuzil, P.; Johansen, J.B.; Mont, L.; Gonzalez, E.; et al. Accelerometer-based atrioventricular synchronous pacing with a ventricular leadless pacemaker: Results from the Micra atrioventricular feasibility studies. Heart Rhythm 2018, 15, 1363–1371. [Google Scholar] [PubMed]
- Steinwender, C.; Khelae, S.K.; Garweg, C.; Chan, J.Y.S.; Ritter, P.; Johansen, J.B.; Sagi, V.; Epstein, L.M.; Piccini, J.P.; Pascual, M.; et al. Atrioventricular synchronous pacing using a leadless ventricular pacemaker: Results from the MARVEL 2 study. JACC Clin. Electrophysiol. 2020, 6, 94–106. [Google Scholar]
- Glikson, M.; Nielsen, J.C.; Kronborg, M.B.; Michowitz, Y.; Auricchio, A.; Barbash, I.M.; Barrabés, J.A.; Boriani, G.; Braunschweig, F.; Brignole, M.; et al. 2021 ESC Guidelines on cardiac pacing and cardiac resynchronization therapy. Eur. Heart J. 2021, 42, 3427–3520. [Google Scholar]
- Tonegawa-Kuji, R.; Kanaoka, K.; Mori, M.; Nakai, M.; Iwanaga, Y. Mortality and 30-day readmission rates after inpatient leadless pacemaker implantation: Insights from a nationwide readmissions database. Can. J. Cardiol. 2022, 38, 1697–1705. [Google Scholar]
- Gulletta, S.; Schiavone, M.; Gasperetti, A.; Breitenstein, A.; Palmisano, P.; Mitacchione, G.; Chierchia, G.B.; Montemerlo, E.; Statuto, G.; Russo, G.; et al. Peri-procedural and mid-term follow-up age-related differences in leadless pacemaker implantation: Insights from a multicenter European registry. Int. J. Cardiol. 2023, 371, 197–203. [Google Scholar]
- Reynolds, D.; Duray, G.Z.; Omar, R.; Soejima, K.; Neuzil, P.; Zhang, S.; Narasimhan, C.; Steinwender, C.; Brugada, J.; Lloyd, M.; et al. A leadless intracardiac transcatheter pacing system. N. Engl. J. Med. 2016, 374, 533–541. [Google Scholar]
- El-Chami, M.F.; Al-Samadi, F.; Clementy, N.; Garweg, C.; Martinez-Sande, J.L.; Piccini, J.P.; Iacopino, S.; Lloyd, M.; Viñolas Prat, X.; Jacobsen, M.D.; et al. Updated performance of the Micra transcatheter pacemaker in the real-world setting: A comparison to the investigational study and a transvenous historical control. Heart Rhythm 2018, 15, 1800–1807. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Darlington, D.; Brown, P.; Carvalho, V.; Bourne, H.; Mayer, J.; Jones, N.; Walker, V.; Siddiqui, S.; Patwala, A.; Kwok, C.S. Efficacy and safety of leadless pacemaker: A systematic review, pooled analysis and meta-analysis. Indian Pacing Electrophysiol. 2022, 22, 77–86. [Google Scholar]
- Bertelli, M.; Toniolo, S.; Ziacchi, M.; Gasperetti, A.; Schiavone, M.; Arosio, R.; Capobianco, C.; Mitacchione, G.; Statuto, G.; Angeletti, A.; et al. Is less always more? A prospective two-centre study addressing clinical outcomes in leadless versus transvenous single-chamber pacemaker recipients. J. Clin. Med. 2022, 11, 6071. [Google Scholar] [PubMed]
- Tjong, F.V.Y.; Knops, R.E.; Udo, E.O.; Brouwer, T.F.; Dukkipati, S.R.; Koruth, J.S.; Petru, J.; Sediva, L.; van Hemel, N.M.; Neuzil, P.; et al. Leadless pacemaker versus transvenous single-chamber pacemaker therapy: A propensity matched analysis. Heart Rhythm 2018, 15, 1387–1393. [Google Scholar] [CrossRef] [PubMed]
- Vincent, L.; Grant, J.; Peñalver, J.; Ebner, B.; Maning, J.; Olorunfemi, O.; Goldberger, J.J.; Mitrani, R.D. Early trends in leadless pacemaker implantation: Evaluating nationwide in-hospital outcomes. Heart Rhythm 2022, 19, 1334–1342. [Google Scholar]
- Piccini, J.P.; El-Chami, M.; Wherry, K.; Crossley, G.H.; Kowal, R.C.; Stromberg, K.; Longacre, C.; Hinnenthal, J.; Bockstedt, L. Contemporaneous comparison of outcomes among patients implanted with a leadless vs. transvenous single chamber ventricular pacemaker. JAMA Cardiol. 2021, 6, 1187–1195. [Google Scholar]
- Piccini, J.P.; Cunnane, R.; Steffel, J.; El-Chami, M.F.; Reynolds, D.; Roberts, P.R.; Soejima, K.; Steinwender, C.; Garweg, C.; Chinitz, L.; et al. Development and validation of a risk score for predicting pericardial effusion in patients undergoing leadless pacemaker implantation: Experience with the Micra transcatheter pacemaker. Europace 2022, 24, 1119–1126. [Google Scholar]
- Hauser, R.G.; Gornick, C.C.; Abdelhadi, R.H.; Tang, C.Y.; Casey, S.A.; Sengupta, J.D. Major adverse clinical events associated with implantation of a leadless intracardiac pacemaker. Heart Rhythm 2021, 18, 1132–1139. [Google Scholar] [CrossRef]
- Okabe, T.; Afzal, M.R.; Houmsse, M.; Makary, M.S.; Elliot, E.D.; Daoud, E.G.; Augostini, R.S.; Hummel, J.D. Tine-based leadless pacemaker: Strategies for safe implantation in unconventional clinical scenarios. JACC Clin. Electrophysiol. 2020, 6, 1318–1331. [Google Scholar]
- Garweg, C.; Vandenberk, B.; Foulon, S.; Haemers, P.; Ector, J.; Willems, R. Leadless pacing with Micra TPS: A comparison between right ventricular outflow tract, mid-septal, and apical implant sites. J. Cardiovasc. Electrophysiol. 2019, 30, 2002–2011. [Google Scholar] [CrossRef]
- Chen, X.; Huang, W. Strategies to overcome complicated situations in leadless pacemaker implantation. Pacing Clin. Electrophysiol. 2021, 44, 1959–1962. [Google Scholar] [CrossRef]
- Bhardwaj, R.; Kewcharoen, J.; Contractor, T.; Nayak, S.; Ai, S.; Kim, U.; Mandapati, R.; Garg, J. Echocardiogram-guided leadless pacemaker implantation. JACC Clin. Electrophysiol. 2022, 8, 1581–1582. [Google Scholar] [CrossRef] [PubMed]
- Lloyd, M.S.; El-Chami, M.F.; Nilsson, K.R., Jr.; Cantillon, D.J. Transcatheter/leadless pacing. Heart Rhythm 2018, 15, 624–628. [Google Scholar] [CrossRef] [PubMed]
- Mitacchione, G.; Arabia, G.; Schiavone, M.; Cerini, M.; Gasperetti, A.; Salghetti, F.; Bontempi, L.; Viecca, M.; Curnis, A.; Forleo, G.B. Intraoperative sensing increase predicts long-term pacing threshold in leadless pacemakers. J. Interv. Card. Electrophysiol. 2022, 63, 679–686. [Google Scholar] [CrossRef]
- Mitacchione, G.; Schiavone, M.; Gasperetti, A.; Arabia, G.; Breitenstein, A.; Cerini, M.; Palmisano, P.; Montemerlo, E.; Ziacchi, M.; Gulletta, S.; et al. Outcomes of Leadless Pacemaker implantation following transvenous lead extraction in high-volume referral centers: Real-world data from a large international registry. Heart Rhythm 2022, 20, 395–404. [Google Scholar] [CrossRef] [PubMed]
- Laczay, B.; Aguilera, J.; Cantillon, D.J. Leadless cardiac ventricular pacing using helix fixation: Step-by-step guide to implantation. J. Cardiovasc. Electrophysiol. 2023, 34, 748–759. [Google Scholar] [CrossRef] [PubMed]
- Hauser, R.G.; Gornick, C.C.; Abdelhadi, R.H.; Tang, C.Y.; Kapphahn-Bergs, M.; Casey, S.A.; Okeson, B.K.; Steele, E.A.; Sengupta, J.D. Leadless pacemaker perforations: Clinical consequences and related device and user problems. J. Cardiovasc. Electrophysiol. 2022, 33, 154–159. [Google Scholar] [CrossRef]
- Wang, Y.; Hou, W.; Zhou, C.; Yin, Y.; Lu, S.; Liu, G.; Duan, C.; Cao, M.; Li, M.; Toft, E.S.; et al. Meta-analysis of the incidence of lead dislodgement with conventional and leadless pacemaker systems. Pacing Clin. Electrophysiol. 2018, 41, 1365–1371. [Google Scholar] [CrossRef]
- Terricabras, M.; Khaykin, Y. Successful leadless pacemaker retrieval from the left pulmonary artery: A case report. Heart Rhythm Case Rep. 2020, 6, 798–799. [Google Scholar] [CrossRef]
- Sugiura, K.; Baba, Y.; Hirota, T.; Kubo, T.; Kitaoka, H. A drifting dislodged leadless pacemaker in the bilateral pulmonary arteries. JACC Case Rep. 2022, 4, 844–846. [Google Scholar] [CrossRef]
- Fichtner, S.; Estner, H.L.; Näbauer, M.; Hausleiter, J. Percutaneous extraction of a leadless Micra pacemaker after dislocation: A case report. Eur. Heart J. Case Rep. 2019, 3, ytz113. [Google Scholar] [CrossRef] [Green Version]
- Karim, S.; Abdelmessih, M.; Marieb, M.; Reiner, E.; Grubman, E. Extraction of a Micra transcatheter pacing system: First-in-human experience. Heart Rhythm Case Rep. 2015, 2, 60–62. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Sterliński, M.; Demkow, M.; Plaskota, K.; Oręziak, A. Percutaneous extraction of a leadless Micra pacemaker from the pulmonary artery in a patient with complex congenital heart disease and complete heart block. EuroIntervention 2018, 14, 236–237. [Google Scholar] [CrossRef] [PubMed]
- Hasegawa-Tamba, S.; Ikeda, Y.; Tsutsui, K.; Kato, R.; Muramatsu, T.; Matsumoto, K. Two-directional snare technique to rescue detaching leadless pacemaker. Heart Rhythm Case Rep. 2020, 6, 711–714. [Google Scholar] [CrossRef]
- Roberts, P.R.; Clementy, N.; Al Samadi, F.; Garweg, C.; Martinez-Sande, J.L.; Iacopino, S.; Johansen, J.B.; Vinolas Prat, X.; Kowal, R.C.; Klug, D.; et al. A leadless pacemaker in the real-world setting: The Micra Transcatheter Pacing System Post-Approval Registry. Heart Rhythm 2017, 14, 1375–1379. [Google Scholar] [CrossRef] [Green Version]
- Sterliński, M.; Demkow, M.; Oręziak, A.; Szumowski, Ł. What is retrieved must dislocate first: Few consideration how to avoid leadless pacemaker escape. Pacing Clin. Electrophysiol. 2021, 44, 1137–1138. [Google Scholar] [CrossRef] [PubMed]
- Afzal, M.R.; Daoud, E.G.; Cunnane, R.; Mulpuru, S.K.; Koay, A.; Hussain, A.; Omar, R.; Wei, K.K.; Amin, A.; Kidwell, G.; et al. Techniques for successful early retrieval of the Micra transcatheter pacing system: A worldwide experience. Heart Rhythm 2018, 15, 841–846. [Google Scholar] [CrossRef]
- Romeo, E.; D’Alto, M.; Cappelli, M.; Nigro, G.; Correra, A.; Colonna, D.; Sarubbi, B.; Golino, P. Retrieval of a leadless transcatheter pacemaker from the right pulmonary artery: A case report. Pacing Clin. Electrophysiol. 2021, 44, 952–954. [Google Scholar] [CrossRef]
- Sundaram, S.; Choe, W. The one that got away: A leadless pacemaker embolizes to the lungs. Heart Rhythm 2016, 13, 2316. [Google Scholar] [CrossRef]
- El-Chami, M.F.; Garweg, C.; Iacopino, S.; Al-Samadi, F.; Martinez-Sande, J.L.; Tondo, C.; Johansen, J.B.; Prat, X.V.; Piccini, J.P.; Cha, Y.M.; et al. Leadless pacemaker implant, anticoagulation status, and outcomes: Results from the Micra Transcatheter Pacing System Post-Approval Registry. Heart Rhythm 2022, 19, 228–234. [Google Scholar] [CrossRef]
- Kiani, S.; Black, G.B.; Rao, B.; Thakkar, N.; Massad, C.; Patel, A.V.; Merchant, F.M.; Hoskins, M.H.; De Lurgio, D.B.; Patel, A.M.; et al. Outcomes of Micra leadless pacemaker implantation with uninterrupted anticoagulation. J. Cardiovasc. Electrophysiol. 2019, 30, 1313–1318. [Google Scholar] [CrossRef]
- San Antonio, R.; Chipa-Ccasani, F.; Apolo, J.; Linhart, M.; Trotta, O.; Pujol-López, M.; Niebla, M.; Alarcón, F.; Trucco, E.; Arbelo, E.; et al. Management of anticoagulation in patients undergoing leadless pacemaker implantation. Heart Rhythm. 2019, 16, 1849–1854. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Palmisano, P.; Iacopino, S.; De Vivo, S.; D’Agostino, C.; Tomasi, L.; Startari, U.; Ziacchi, M.; Pisanò, E.C.L.; Santobuono, V.E.; Caccavo, V.P.; et al. Leadless transcatheter pacemaker: Indications, implantation technique and peri-procedural patient management in the Italian clinical practice. Int. J. Cardiol. 2022, 365, 49–56. [Google Scholar] [CrossRef] [PubMed]
- Malagù, M.; D’Aniello, E.; Vitali, F.; Balla, C.; Gasbarro, V.; Bertini, M. Leadless pacemaker implantation in superobese patient. Rev. Cardiovasc. Med. 2022, 23, 125. [Google Scholar] [CrossRef]
- Kelm, M.; Perings, S.M.; Jax, T.; Lauer, T.; Schoebel, F.C.; Heintzen, M.P.; Perings, C.; Strauer, B.E. Incidence and clinical outcome of iatrogenic femoral arteriovenous fistulas: Implications for risk stratification and treatment. J. Am. Coll. Cardiol. 2002, 40, 291–297. [Google Scholar] [CrossRef] [Green Version]
- Zilinyi, R.S.; Sethi, S.S.; Parikh, M.A.; Parikh, S.A. Iatrogenic arteriovenous fistula following femoral access precipitating high-output heart failure. JACC Case Rep. 2021, 3, 421–424. [Google Scholar] [CrossRef]
- Madia, C. Management trends for postcatheterization femoral artery pseudoaneurysms. JAAPA 2019, 32, 15–18. [Google Scholar] [CrossRef]
- Chang, D.; Gabriels, J.K.; Soo Kim, B.; Ismail, H.; Willner, J.; Beldner, S.J.; John, R.M.; Epstein, L.M. Concomitant leadless pacemaker implantation and lead extraction during an active infection. J. Cardiovasc. Electrophysiol. 2020, 31, 860–867. [Google Scholar] [CrossRef] [PubMed]
- Beurskens, N.E.G.; Tjong, F.V.Y.; Dasselaar, K.J.; Kuijt, W.J.; Wilde, A.A.M.; Knops, R.E. Leadless pacemaker implantation after explantation of infected conventional pacemaker systems: A viable solution? Heart Rhythm 2019, 16, 66–71. [Google Scholar] [CrossRef]
- Breeman, K.T.N.; Beurskens, N.E.G.; Driessen, A.H.G.; Wilde, A.A.M.; Tjong, F.V.Y.; Knops, R.E. Timing and mid-term outcomes of using leadless pacemakers as replacement for infected cardiac implantable electronic devices. J. Interv. Card. Electrophysiol. 2022. [Google Scholar] [CrossRef]
- Bicong, L.; Allen, J.C.; Arps, K.; Al-Khatib, S.M.; Bahnson, T.D.; Daubert, J.P.; Frazier-Mills, C.; Hegland, D.D.; Jackson, K.P.; Jackson, L.R.; et al. Leadless pacemaker implantation after lead extraction for cardiac implanted electronic device infection. J. Cardiovasc. Electrophysiol. 2022, 33, 464–470. [Google Scholar] [CrossRef] [PubMed]
- Al-Mohaissen, M.A.; Chan, K.L. Prevalence and mechanism of tricuspid regurgitation following implantation of endocardial leads for pacemaker or cardioverter-defibrillator. J. Am. Soc. Echocardiogr. 2012, 25, 245–252. [Google Scholar] [CrossRef] [PubMed]
- Sasaki, K.; Togashi, D.; Nakajima, I.; Suchi, T.; Nakayama, Y.; Harada, T.; Akashi, Y.J. Clinical outcomes of non-atrial fibrillation bradyarrhythmias treated with a ventricular demand leadless pacemaker compared with an atrioventricular synchronous transvenous pacemaker-a propensity score-matched analysis. Circ. J. 2022, 86, 1283–1291. [Google Scholar] [CrossRef] [PubMed]
- Vaidya, V.R.; Dai, M.; Asirvatham, S.J.; Rea, R.F.; Thome, T.M.; Srivathsan, K.; Mulpuru, S.K.; Kusumoto, F.; Venkatachalam, K.L.; Ryan, J.D.; et al. Real-world experience with leadless cardiac pacing. Pacing Clin. Electrophysiol. 2019, 42, 366–373. [Google Scholar] [CrossRef]
- Ohta, Y.; Goda, A.; Daimon, A.; Manabe, E.; Masai, K.; Kishima, H.; Mine, T.; Asakura, M.; Ishihara, M. The differences between conventional lead, thin lead, and leadless pacemakers regarding effects on tricuspid regurgitation in the early phase. J. Med. Ultrason. 2023, 50, 51–56. [Google Scholar] [CrossRef]
- Beurskens, N.E.G.; Tjong, F.V.Y.; de Bruin-Bon, R.H.A.; Dasselaar, K.J.; Kuijt, W.J.; Wilde, A.A.M.; Knops, R.E. Impact of leadless pacemaker therapy on cardiac and atrioventricular valve function through 12 months of follow-up. Circ. Arrhythm. Electrophysiol. 2019, 12, e007124. [Google Scholar] [CrossRef]
- Breeman, K.T.N.; Oosterwerff, E.F.J.; Dijkshoorn, L.A.; Salavati, A.; Beurskens, N.E.G.; Wilde, A.A.M.; Delnoy, P.H.M.; Tjong, F.V.Y.; Knops, R.E. Real-world long-term battery longevity of Micra leadless pacemakers. J. Interv. Card. Electrophysiol. 2022. [Google Scholar] [CrossRef]
- Garweg, C.; Piccini, J.P.; Epstein, L.M.; Frazier-Mills, C.; Chinitz, L.A.; Steinwender, C.; Stromberg, K.; Sheldon, T.; Fagan, D.H.; El-Chami, M.F. Correlation between AV synchrony and device collected AM-VP sequence counter in atrioventricular synchronous leadless pacemakers: A real-world assessment. J. Cardiovasc. Electrophysiol. 2023, 34, 197–206. [Google Scholar] [CrossRef]
- Grubman, E.; Ritter, P.; Ellis, C.R.; Giocondo, M.; Augostini, R.; Neuzil, P.; Ravindran, B.; Patel, A.M.; Omdahl, P.; Pieper, K.; et al. To retrieve, or not to retrieve: System revisions with the Micra transcatheter pacemaker. Heart Rhythm 2017, 14, 1801–1806. [Google Scholar] [CrossRef] [Green Version]
- Omdahl, P.; Eggen, M.D.; Bonner, M.D.; Iaizzo, P.A.; Wika, K. Right ventricular anatomy can accommodate multiple Micra transcatheter pacemakers. Pacing Clin. Electrophysiol. 2016, 39, 393–397. [Google Scholar] [CrossRef] [Green Version]
- Kowlgi, G.N.; Tseng, A.S.; Tempel, N.D.; Henrich, M.J.; Venkatachalam, K.L.; Scott, L.; Shen, W.K.; Deshmukh, A.J.; Madhavan, M.; Lee, H.C.; et al. A real-world experience of atrioventricular synchronous pacing with leadless ventricular pacemakers. J. Cardiovasc. Electrophysiol. 2022, 33, 982–993. [Google Scholar] [CrossRef]
- Neugebauer, F.; Noti, F.; van Gool, S.; Roten, L.; Baldinger, S.H.; Seiler, J.; Madaffari, A.; Servatius, H.; Ryser, A.; Tanner, H.; et al. Leadless atrioventricular synchronous pacing in an outpatient setting: Early lessons learned on factors affecting atrioventricular synchrony. Heart Rhythm 2022, 19, 748–756. [Google Scholar] [CrossRef]
- El-Chami, M.F.; Bhatia, N.K.; Merchant, F.M. Atrio-ventricular synchronous pacing with a single chamber leadless pacemaker: Programming and trouble shooting for common clinical scenarios. J. Cardiovasc. Electrophysiol. 2021, 32, 533–539. [Google Scholar] [CrossRef] [PubMed]
- Briongos-Figuero, S.; Estévez-Paniagua, Á.; Sánchez Hernández, A.; Jiménez, S.; Gómez-Mariscal, E.; Abad Motos, A.; Muñoz-Aguilera, R. Optimizing atrial sensing parameters in leadless pacemakers: Atrioventricular synchrony achievement in the real world. Heart Rhythm 2022, 19, 2011–2018. [Google Scholar] [CrossRef]
- Chinitz, L.A.; El-Chami, M.F.; Sagi, V.; Garcia, H.; Hackett, F.K.; Leal, M.; Whalen, P.; Henrikson, C.A.; Greenspon, A.J.; Sheldon, T.; et al. Ambulatory atrioventricular synchronous pacing over time using a leadless ventricular pacemaker: Primary results from the AccelAV study. Heart Rhythm 2023, 20, 46–54. [Google Scholar] [CrossRef] [PubMed]
- Garweg, C.; Khelae, S.K.; Steinwender, C.; Chan, J.Y.S.; Ritter, P.; Johansen, J.B.; Sagi, V.; Epstein, L.M.; Piccini, J.P.; Pascual, M.; et al. Predictors of atrial mechanical sensing and atrioventricular synchrony with a leadless ventricular pacemaker: Results from the MARVEL 2 Study. Heart Rhythm 2020, 17, 2037–2045. [Google Scholar] [CrossRef]
- Pujol-López, M.; Garcia-Ribas, C.; Doltra, A.; Guasch, E.; Vazquez-Calvo, S.; Niebla, M.; Domingo, R.; Roca-Luque, I.; Tolosana, J.M.; Mont, L. Pulsed doppler A-wave as an aid in patient selection for atrioventricular synchrony through a leadless ventricular pacemaker. J. Interv. Card. Electrophysiol. 2023, 66, 261–263. [Google Scholar] [CrossRef] [PubMed]
- Mitacchione, G.; Schiavone, M.; Gasperetti, A.; Viecca, M.; Curnis, A.; Forleo, G.B. Atrioventricular synchronous leadless pacemaker: State of art and broadened indications. Rev. Cardiovasc. Med. 2021, 22, 395–401. [Google Scholar] [CrossRef] [PubMed]
- Mitacchione, G.; Schiavone, M.; Gasperetti, A.; Ruggiero, D.; Denora, M.; Viecca, M.; Forleo, G.B. Micra-AV leadless pacemaker and atrioventricular (dys)synchrony: A stepwise process. Pacing Clin. Electrophysiol. 2021, 44, 1738–1742. [Google Scholar] [CrossRef] [PubMed]
- Garweg, C.; Khelae, S.K.; Chan, J.Y.S.; Chinitz, L.; Ritter, P.; Johansen, J.B.; Sagi, V.; Epstein, L.M.; Piccini, J.P.; Pascual, M.; et al. Behavior of AV synchrony pacing mode in a leadless pacemaker during variable AV conduction and arrhythmias. J. Cardiovasc. Electrophysiol. 2021, 32, 1947–1957. [Google Scholar] [CrossRef]
- Duray, G.Z.; Ritter, P.; El-Chami, M.; Narasimhan, C.; Omar, R.; Tolosana, J.M.; Zhang, S.; Soejima, K.; Steinwender, C.; Rapallini, L.; et al. Long-term performance of a transcatheter pacing system: 12-Month results from the Micra Transcatheter Pacing Study. Heart Rhythm 2017, 14, 702–709. [Google Scholar] [CrossRef] [Green Version]
- Russo, V.; D’Andrea, A.; De Vivo, S.; Rago, A.; Manzo, G.; Bocchetti, A.; Papa, A.A.; Giordano, V.; Ammendola, E.; Sarubbi, B.; et al. Single-chamber leadless cardiac pacemaker in patients without atrial fibrillation: Findings from Campania leadless registry. Front. Cardiovasc. Med. 2022, 8, 781335. [Google Scholar] [CrossRef] [PubMed]
- Buckingham, T.A.; Janosik, D.L.; Pearson, A.C. Pacemaker hemodynamics: Clinical implications. Prog. Cardiovasc. Dis. 1992, 34, 347–366. [Google Scholar] [CrossRef]
- Benditt, D.G.; Milstein, S.; Buetikofer, J.; Gornick, C.C.; Mianulli, M.; Fetter, J. Sensor-triggered, rate-variable cardiac pacing. Current technologies and clinical implications. Ann. Intern. Med. 1987, 107, 714–724. [Google Scholar] [CrossRef]
- Ng, A.C.; Allman, C.; Vidaic, J.; Tie, H.; Hopkins, A.P.; Leung, D.Y. Long-term impact of right ventricular septal versus apical pacing on left ventricular synchrony and function in patients with second-or third-degree heart block. Am. J. Cardiol. 2009, 103, 1096–1101. [Google Scholar] [CrossRef]
- Arnold, A.D.; Whinnett, Z.I.; Vijayaraman, P. His-Purkinje conduction system pacing: State of the art in 2020. Arrhythm. Electrophysiol. Rev. 2020, 9, 136–145. [Google Scholar] [PubMed]
- Vatterott, P.J.; Eggen, M.D.; Hilpisch, K.E.; Drake, R.A.; Grubac, V.; Anderson, T.A.; Colin, B.P.; Seifert, K.R.; Mesich, M.L.; Ramon, L.C. Implant, performance, and retrieval of an atrial leadless pacemaker in sheep. Heart Rhythm 2021, 18, 288–296. [Google Scholar] [CrossRef]
- Rashtian, M.; Banker, R.S.; Neuzil, P.; Breeman, K.; Nee, P.; Badie, N.; Victorine, K.; Ligon, D.; Rippy, M.K.; Eldadah, Z.; et al. Preclinical safety and electrical performance of novel atrial leadless pacemaker with dual-helix fixation. Heart Rhythm 2022, 19, 776–781. [Google Scholar] [CrossRef] [PubMed]
- NCT05252702; Aveir Dual-Chamber Leadless i2i IDE Study. Abbott Medical Devices: Abbott Park, IL, USA, 2022.
- Bose, P.; Khaleghi, A.; Albatat, M.; Bergsland, J.; Balasingham, I. RF channel modeling for implant-to-implant communication and implant to subcutaneous implant communication for future leadless cardiac pacemakers. IEEE Trans. Biomed. Eng. 2018, 65, 2798–2807. [Google Scholar] [CrossRef] [Green Version]
- Bereuter, L.; Kuenzle, T.; Niederhauser, T.; Kucera, M.; Obrist, D.; Reichlin, T.; Tanner, H.; Haeberlin, A. Fundamental characterization of conductive intracardiac communication for leadless multisite pacemaker systems. IEEE Trans. Biomed. Circuits Syst. 2019, 13, 237–247. [Google Scholar] [CrossRef]
- Bereuter, L.; Gysin, M.; Kueffer, T.; Kucera, M.; Niederhauser, T.; Fuhrer, J.; Heinisch, P.; Zurbuchen, A.; Obrist, D.; Tanner, H.; et al. Leadless Dual-chamber pacing a novel communication method for wireless pacemaker synchronization. JACC Basic Transl. Sci. 2018, 3, 813–823. [Google Scholar] [CrossRef] [PubMed]
- Cantillon, D.J.; Gambhir, A.; Banker, R.; Rashtian, M.; Doshi, R.; Badie, N.; Booth, D.; Yang, W.; Nee, P.; Fishler, M.; et al. Wireless communication between paired leadless pacemakers for dual-chamber synchrony. Circ. Arrhythm. Electrophysiol. 2022, 15, e010909. [Google Scholar] [CrossRef] [PubMed]
- Okabe, T.; Hummel, J.D.; Bank, A.J.; Niazi, I.K.; McGrew, F.A.; Kindsvater, S.; Oza, S.R.; Scherschel, J.A.; Walsh, M.N.; Singh, J.P. Leadless left ventricular stimulation with WiSE-CRT System-Initial experience and results from phase I of SOLVE-CRT Study (nonrandomized, roll-in phase). Heart Rhythm 2022, 19, 22–29. [Google Scholar] [CrossRef] [PubMed]
- Reddy, V.Y.; Miller, M.A.; Neuzil, P.; Søgaard, P.; Butter, C.; Seifert, M.; Delnoy, P.P.; van Erven, L.; Schalji, M.; Boersma, L.V.A.; et al. Cardiac resynchronization therapy with wireless left ventricular endocardial pacing The SELECT-LV Study. J. Am. Coll. Cardiol. 2017, 69, 2119–2129. [Google Scholar] [CrossRef]
- Neuzil, P.; Reddy, V.Y. Leadless cardiac pacemakers: Pacing paradigm change. Curr. Cardiol. Rep. 2015, 17, 68. [Google Scholar] [CrossRef]
- Benditt, D.G.; Goldstein, M.; Belalcazar, A. The leadless ultrasonic pacemaker: A sound idea? Heart Rhythm 2009, 6, 749–751. [Google Scholar] [CrossRef]
- Anwar, U.; Ajijola, O.A.; Shivkumar, K.; Markovic, D. Towards a leadless wirelessly controlled intravenous cardiac pacemaker. IEEE Trans. Biomed. Eng. 2022, 69, 3074–3086. [Google Scholar] [CrossRef]
- Choi, Y.S.; Yin, R.T.; Pfenniger, A.; Koo, J.; Avila, R.; Benjamin Lee, K.; Chen, S.W.; Lee, G.; Li, G.; Qiao, Y.; et al. Fully implantable and bioresorbable cardiac pacemakers without leads or batteries. Nat Biotechnol. 2021, 39, 1228–1238. [Google Scholar] [CrossRef]
- Franzina, N.; Zurbuchen, A.; Zumbrunnen, A.; Niederhauser, T.; Reichlin, T.; Burger, J.; Haeberlin, A. A miniaturized endocardial electromagnetic energy harvester for leadless cardiac pacemakers. PLoS ONE 2020, 15, e0239667. [Google Scholar] [CrossRef]
- Zurbuchen, A.; Haeberlin, A.; Bereuter, L.; Wagner, J.; Pfenniger, A.; Omari, S.; Schaerer, J.; Jutzi, F.; Huber, C.; Fuhrer, J.; et al. The Swiss approach for a heartbeat-driven lead- and batteryless pacemaker. Heart Rhythm 2017, 14, 294–299. [Google Scholar] [CrossRef] [Green Version]
- Tholl, M.V.; Haeberlin, A.; Meier, B.; Shaheen, S.; Bereuter, L.; Becsek, B.; Tanner, H.; Niederhauser, T.; Zurbuchen, A. An intracardiac flow based electromagnetic energy harvesting mechanism for cardiac pacing. IEEE Trans. Biomed. Eng. 2019, 66, 530–538. [Google Scholar] [CrossRef] [PubMed]
- Ryu, H.; Park, H.M.; Kim, M.K.; Kim, B.; Myoung, H.S.; Kim, T.Y.; Yoon, H.J.; Kwak, S.S.; Kim, J.; Hwang, T.H.; et al. Self-rechargeable cardiac pacemaker system with triboelectric nanogenerators. Nat. Commun. 2021, 12, 4374. [Google Scholar] [CrossRef] [PubMed]

| Heart Sound | Echocardiography | Electrocardiogram | ||
|---|---|---|---|---|
| A1 | Mitral/tricuspid valve closure | S1 | At the end of QRS complex | |
| A2 | Aortic/pulmonic valve closure | S2 | At the end of T wave | |
| A3 | Early passive ventricular filling | S3 | E wave | Before the onset of the P wave |
| A4 | Atrial contraction | S4 | A wave | After the inscription of the P wave |
Disclaimer/Publisher’s Note: The statements, opinions and data contained in all publications are solely those of the individual author(s) and contributor(s) and not of MDPI and/or the editor(s). MDPI and/or the editor(s) disclaim responsibility for any injury to people or property resulting from any ideas, methods, instructions or products referred to in the content. |
© 2023 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Tong, F.; Sun, Z. Strategies for Safe Implantation and Effective Performance of Single-Chamber and Dual-Chamber Leadless Pacemakers. J. Clin. Med. 2023, 12, 2454. https://doi.org/10.3390/jcm12072454
Tong F, Sun Z. Strategies for Safe Implantation and Effective Performance of Single-Chamber and Dual-Chamber Leadless Pacemakers. Journal of Clinical Medicine. 2023; 12(7):2454. https://doi.org/10.3390/jcm12072454
Chicago/Turabian StyleTong, Fei, and Zhijun Sun. 2023. "Strategies for Safe Implantation and Effective Performance of Single-Chamber and Dual-Chamber Leadless Pacemakers" Journal of Clinical Medicine 12, no. 7: 2454. https://doi.org/10.3390/jcm12072454
APA StyleTong, F., & Sun, Z. (2023). Strategies for Safe Implantation and Effective Performance of Single-Chamber and Dual-Chamber Leadless Pacemakers. Journal of Clinical Medicine, 12(7), 2454. https://doi.org/10.3390/jcm12072454







