Healthcare Resources Utilization throughout the Last Year of Life after Acute Myocardial Infarction
Abstract
:1. Introduction
2. Materials and Methods
2.1. Study Population
2.2. Study Design
2.3. Study Groups
2.4. Statistical Analysis
3. Results
3.1. Study Population and Groups
3.2. HRU and Costs
3.3. Multivariable Analysis
3.4. Predictive Ability of the Models
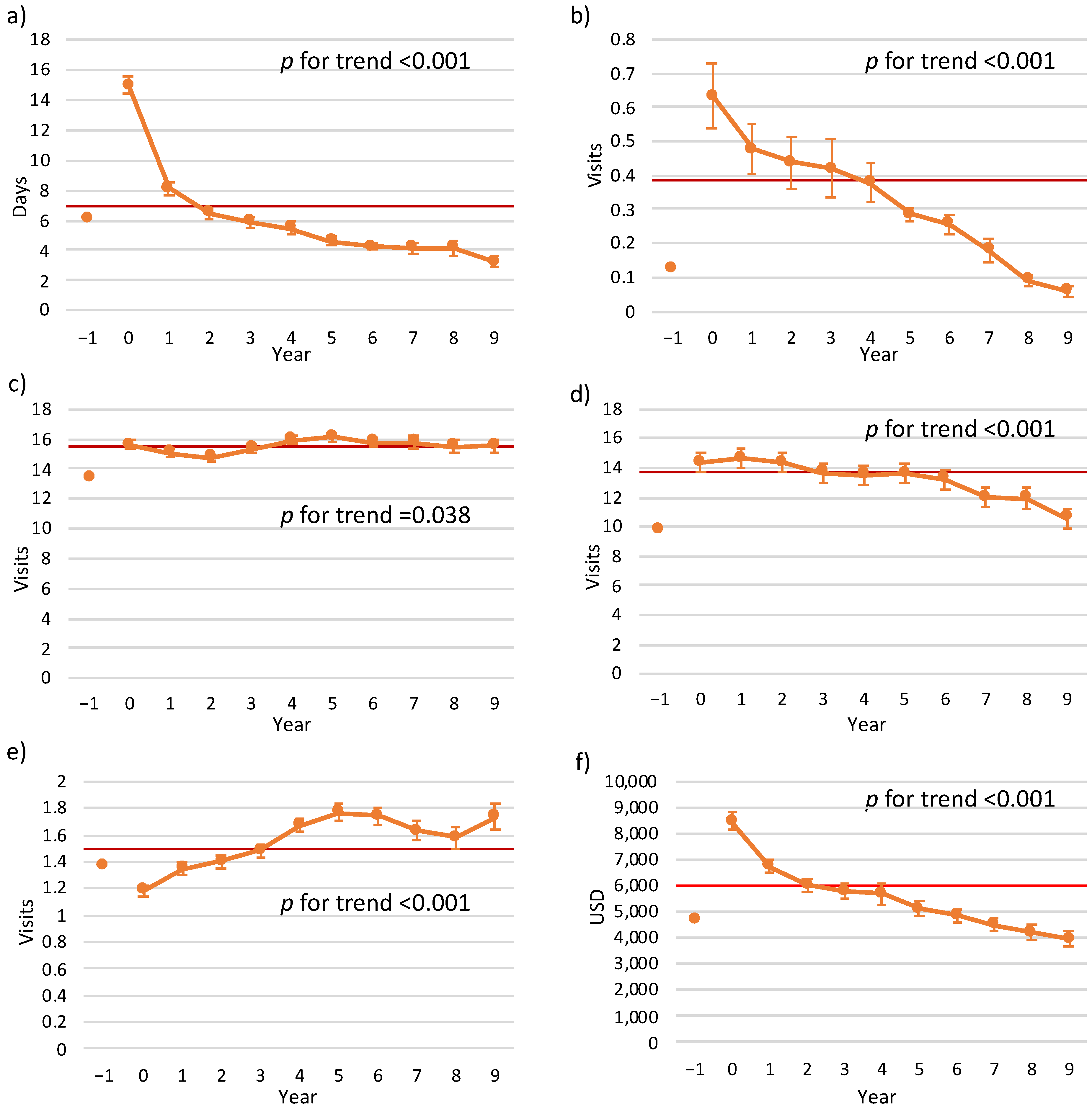
3.5. Trends in HRU Prior to Mortality Years
4. Discussion
Limitations
5. Conclusions
Supplementary Materials
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Acknowledgments
Conflicts of Interest
References
- Peterson, E.D.; Shah, B.R.; Parsons, L.; Pollack, C.V., Jr.; French, W.J.; Canto, J.G.; Gibson, C.M.; Rogers, W.J. Trends in quality of care for patients with acute myocardial infarction in the National Registry of Myocardial Infarction from 1990 to 2006. Am. Heart J. 2008, 156, 1045–1055. [Google Scholar] [CrossRef]
- Braunwald, E.; Antman, E.M.; Beasley, J.W.; Califf, R.M.; Cheitlin, M.D.; Hochman, J.; Jones, R.H.; Kereiakes, D.; Kupersmith, J.; Levin, T.N.; et al. ACC/AHA 2002 guideline update for the management of patients with unstable angina and non-ST-segment elevation myocardial infarction—Summary article: A report of the American College of Cardiology/American Heart Association task force on practice guidelines (Committee on the Management of Patients with Unstable Angina). J. Am. Coll. Cardiol. 2002, 40, 1366–1374. [Google Scholar]
- Kushner, F.G.; Hand, M.; Smith, S.C., Jr.; King, S.B., 3rd; Anderson, J.L.; Antman, E.M.; Bailey, S.R.; Bates, E.R.; Blankenship, J.C.; Casey, D.E., Jr.; et al. 2009 focused updates: ACC/AHA guidelines for the management of patients with ST-elevation myocardial infarction (updating the 2004 guideline and 2007 focused update) and ACC/AHA/SCAI guidelines on percutaneous coronary intervention (updating the 2005 guideline and 2007 focused update) a report of the American College of Cardiology Foundation/American Heart Association Task Force on Practice Guidelines. J. Am. Coll. Cardiol. 2009, 54, 2205–2241. [Google Scholar]
- Plakht, Y.; Gilutz, H.; Shiyovich, A. Temporal trends in acute myocardial infarction: What about survival of hospital survivors? Disparities between STEMI & NSTEMI remain. Soroka acute myocardial infarction II (SAMI-II) project. Int. J. Cardiol. 2016, 203, 1073–1081. [Google Scholar]
- Plakht, Y.; Gilutz, H.; Shiyovich, A. Excess long-term mortality among hospital survivors of acute myocardial infarction. Soroka Acute Myocardial Infarction (SAMI) project. Public Health 2017, 143, 25–36. [Google Scholar] [CrossRef]
- Yang, E.; Stokes, M.; Johansson, S.; Mellström, C.; Magnuson, E.; Cohen, D.J.; Hunt, P. Clinical and economic outcomes among elderly myocardial infarction survivors in the United States. Cardiovasc. Ther. 2016, 34, 450–459. [Google Scholar] [CrossRef]
- Janzon, M.; Henriksson, M.; Hasvold, P.; Hjelm, H.; Thuresson, M.; Jernberg, T. Long-term resource use patterns and healthcare costs after myocardial infarction in a clinical practice setting: Results from a contemporary nationwide registry study. Eur. Heart J. Qual. Care Clin. Outcome 2016, 2, 291–298. [Google Scholar] [CrossRef] [Green Version]
- Rosella, L.C.; Kornas, K.; Bornbaum, C.; Huang, A.; Watson, T.; Shuldiner, J.; Wodchis, W.P. Population-Based Estimates of Health Care Utilization and Expenditures by Adults During the Last 2 Years of Life in Canada's Single-Payer Health System. JAMA Netw. Open 2020, 3, e201917. [Google Scholar] [CrossRef] [Green Version]
- Greenle, M.M.; Hirschman, K.B.; Coburn, K.; Marcantonio, S.; Hanlon, A.L.; Naylor, M.; Mauer, E.; Ulrich, C. End-of-life Health-Care Utilization Patterns Among Chronically Ill Older Adults. Am. J. Hosp. Palliat. Care 2019, 36, 507–512. [Google Scholar] [CrossRef]
- Greenle, M.M.; Hirschman, K.B.; Coburn, K.; Marcantonio, S.; Hanlon, A.L.; Naylor, M.; Mauer, E.; Ulrich, C. Hospital resource utilization and presence of advance directives at the end of life for adults with congenital heart disease. Congenit. Heart Dis. 2018, 13, 721–727. [Google Scholar]
- Dunlay, S.M.; Redfield, M.M.; Jiang, R.; Weston, S.A.; Roger, V.L. Care in the last year of life for community patients with heart failure. Circ. Heart Fail. 2015, 8, 489–496. [Google Scholar] [CrossRef] [Green Version]
- Hogan, C.; Lunney, J.; Gabel, J.; Lynn, J. Medicare beneficiaries’ costs of care in the last year of life. Health. Aff. 2001, 20, 188–195. [Google Scholar] [CrossRef] [Green Version]
- Plakht, Y.; Greenberg, D.; Gilutz, H.; Arbelle, J.E.; Shiyovich, A. Mortality and healthcare resource utilization following acute myocardial infarction according to adherence to recommended medical therapy guidelines. Health Policy 2020, 124, 1200–1208. [Google Scholar] [CrossRef]
- State of Israel. Ministry of Health. Available online: https://www.health.gov.il/English/Pages/HomePage.aspx (accessed on 18 November 2021).
- Goldsbury, D.E.; O’Connell, D.L.; Girgis, A.; Wilkinson, A.; Phillips, J.L.; Davidson, P.M.; Ingham, J.M. Acute hospital-based services used by adults during the last year of life in New South Wales, Australia: A population-based retrospective cohort study. BMC Health Serv. Res. 2015, 15, 537. [Google Scholar] [CrossRef] [Green Version]
- Madelaire, C.; Gustafsson, F.; Kristensen, S.L.; D’Souza, M.; Stevenson, L.W.; Kober, L.; Torp-Pedersen, C.; Gislason, G.; Schou, M. Burden and Causes of Hospital Admissions in Heart Failure During the Last Year of Life. JACC Heart Fail. 2019, 7, 561–570. [Google Scholar] [CrossRef]
- Hollingworth, W.; Biswas, M.; Maishman, R.L.; Dayer, M.J.; McDonagh, T.; Purdy, S.; Reeves, B.C.; Rogers, C.A.; Williams, R.; Pufulete, M. The healthcare costs of heart failure during the last five years of life: A retrospective cohort study. Int. J. Cardiol. 2016, 224, 132–138. [Google Scholar] [CrossRef] [Green Version]
- Chróinín, D.N.; Goldsbury, D.E.; Beveridge, A.; Davidson, P.M.; Girgis, A.; Ingham, N.; Phillips, J.L.; Wilkinson, A.M.; Ingham, J.M.; O’Connell, D.L. Health-services utilisation amongst older persons during the last year of life: A population-based study. BMC Geriatr. 2018, 18, 317. [Google Scholar] [CrossRef] [Green Version]
- Hill, A.D.; Stukel, T.A.; Fu, L.; Scales, D.C.; Laupacis, A.; Rubenfeld, G.D.; Wunsch, H.; Downar, J.; Rockwood, K.; Heyland, D.K.; et al. Trends in site of death and health care utilization at the end of life: A population-based cohort study. CMAJ Open 2019, 7, E306–E315. [Google Scholar] [CrossRef] [Green Version]
- Ganz, F.D.; Roeh, K.; Eid, M.; Hasin, T.; Harush, C.; Gotsman, I. The need for palliative and support care services for heart failure patients in the community. Eur. J. Cardiovasc. Nurs. 2021, 20, 138–146. [Google Scholar] [CrossRef]
- Hamood, H.; Hamood, R.; Green, M.S.; Almog, R. Determinants of adherence to evidence-based therapy after acute myocardial infarction. Eur. J. Prev. Cardiol. 2016, 23, 975–985. [Google Scholar] [CrossRef]
- Rodriguez, F.; Cannon, C.P.; Steg, P.G.; Kumbhani, D.J.; Goto, S.; Smith, S.C.; Eagle, K.A.; Ohman, E.M.; Umez-Eronini, A.A.; Hoffman, E.; et al. Predictors of long-term adherence to evidence-based cardiovascular disease medications in outpatients with stable atherothrombotic disease: Findings from the REACH Registry. Clin. Cardiol. 2013, 36, 721–727. [Google Scholar] [CrossRef] [Green Version]
- Osterberg, L.; Blaschke, T. Adherence to medication. N. Engl. J. Med. 2005, 353, 487–497. [Google Scholar] [CrossRef] [Green Version]
- Du, L.; Cheng, Z.; Zhang, Y.; Li, Y.; Mei, D. The impact of medication adherence on clinical outcomes of coronary artery disease: A meta-analysis. Eur. J. Prev. Cardiol. 2017, 24, 962–970. [Google Scholar] [CrossRef]
- Cordero, A.; Rodriguez Padial, L.; Batalla, A.; López Barreiro, L.; Torres Calvo, F.; Castellano, J.M.; Ruiz, E.; Bertomeu-Martínez, V. Optimal pharmacological treatment and adherence to medication in secondary prevention of cardiovascular events in Spain: Results from the CAPS study. Cardiovasc. Ther. 2017, 35, e12240. [Google Scholar] [CrossRef]
- Bansilal, S.; Castellano, J.M.; Garrido, E.; Wei, H.G.; Freeman, A.; Spettell, C.; Garcia-Alonso, F.; Lizano, I.; Arnold, R.J.; Rajda, J.; et al. Assessing the Impact of Medication Adherence on Long-Term Cardiovascular Outcomes. J. Am. Coll. Cardiol. 2016, 68, 789–801. [Google Scholar] [CrossRef]
- Tamir, O.; Peleg, R.; Dreiher, J.; Abu-Hammad, T.; Abu Rabia, Y.; Abu Rashid, M.; Eisenberg, A.; Sibersky, D.; Kazanovich, A.; Khalil, E.; et al. Cardiovascular risk factors in the Bedouin population: Management and compliance. Isr. Med. Assoc. J. 2007, 9, 652–655. [Google Scholar]
- Agrawal, Y.; Panaich, S.; Aggarwal, S.; Saltiel, F.; Kalavakunta, J.K.; Gupta, V. Demographic parameters related to 30-day readmission of patients with acute myocardial infarction: Analysis of 2,371,867 hospitalizations. Int. J. Cardiol. 2016, 214, 408–409. [Google Scholar] [CrossRef]
- Plakht, Y.; Gilutz, H.; Arbelle, J.E.; Greenberg, D.; Shiyovich, A. Sex and Ethnic Disparities in Health-Related Outcomes Following Acute Myocardial Infarction in Israel. Isr. Med. Assoc. J. 2020, 22, 303–309. [Google Scholar]
| Parameter | Study Group | Total | p | |
|---|---|---|---|---|
| Years of Survival | Years of Death | |||
| n (Person-Years) | 41,244 | 2855 | 44,099 | |
| Demographics | ||||
| Age (years), Mean (SD) | 63.24 (13.09) | 73.98 (11.13) | 63.94 (13.23) | <0.001 |
| Sex (males) | 29,716 (72.0) | 1654 (57.9) | 31,370 (71.1) | <0.001 |
| Nationality (minorities) | 9580 (23.2) | 503 (17.6) | 10,083 (22.9) | <0.001 |
| Cardiac diseases | ||||
| Supraventricular arrhythmias | 5186 (12.6) | 718 (25.1) | 5904 (13.4) | <0.001 |
| CHF | 4833 (11.7) | 754 (26.4) | 5587 (12.7) | <0.001 |
| CIHD | 34,024 (82.5) | 1989 (69.7) | 36,013 (81.7) | <0.001 |
| Cardiovascular risk factors | ||||
| Renal diseases | 12,262 (29.7) | 1518 (53.2) | 13,780 (31.2) | <0.001 |
| Diabetes mellitus | 14,382 (34.9) | 1370 (48.0) | 15,752 (35.7) | <0.001 |
| Dyslipidemia | 29,349 (71.2) | 1666 (58.4) | 31,015 (70.3) | <0.001 |
| Hypertension | 21,423 (51.9) | 1604 (56.2) | 23,027 (52.2) | <0.001 |
| Obesity | 9977 (24.2) | 546 (19.1) | 10,523 (23.9) | <0.001 |
| Smoking | 18,152 (44.0) | 735 (25.7) | 18,887 (42.8) | <0.001 |
| PVD | 4220 (10.2) | 535 (18.7) | 4755 (10.8) | <0.001 |
| Other disorders | ||||
| COPD | 2249 (5.5) | 347 (12.2) | 2596 (5.9) | <0.001 |
| Neurological disorders | 4925 (11.9) | 707 (24.8) | 5632 (12.8) | <0.001 |
| Malignancy | 1013 (2.5) | 144 (5.0) | 1157 (2.6) | <0.001 |
| Anemia | 20,058 (48.6) | 1922 (67.3) | 21,980 (49.8) | <0.001 |
| Schizophrenia/Psychosis | 544 (1.3) | 75 (2.6) | 619 (1.4) | <0.001 |
| GI bleeding | 743 (1.8) | 86 (3.0) | 829 (1.9) | <0.001 |
| Alcohol/drug addiction | 809 (2.0) | 63 (2.2) | 872 (2.0) | 0.363 |
| HRU one year prior to AMI, Mean (SD) | ||||
| LOS (Days) | 3.54 (8.49) | 6.55 (13.24) | 3.74 (8.91) | <0.001 |
| Number of ED visits a | 0.097 (0.44) | 0.122 (0.641) | 0.099 (0.451) | 0.038 |
| Number of primary clinic visits | 10.63 (10.18) | 13.69 (12.02) | 10.83 (10.33) | <0.001 |
| Number of ambulatory visits | 6.79 (13.89) | 10.03 (21.19) | 7.00 (14.50) | <0.001 |
| Number of consultant visits | 1.06 (1.94) | 1.33 (2.10) | 1.08 (1.95) | <0.001 |
| Total cost (USD) | 3174.46 (6045.33) | 4825.91 (9156.25) | 3281.37 (6306.42) | <0.001 |
| Characteristics of the hospitalization | ||||
| Encounter year, 2002–2006 | 21,516 (52.2) | 1710 (59.9) | 23,226 (52.7) | <0.001 |
| 2007–2012 | 19,728 (47.8) | 1145 (40.1) | 20,873 (47.3) | |
| Type of AMI, STEMI | 22,001 (53.3) | 1130 (39.6) | 23,131 (52.5) | <0.001 |
| Type of treatment, Noninvasive | 7861 (19.1) | 1368 (47.9) | 9229 (20.9) | <0.001 |
| PCI | 27,066 (65.6) | 1233 (43.2) | 28,299 (64.2) | |
| CABG | 6313 (15.3) | 254 (8.9) | 6567 (14.9) | |
| Results of echocardiography b | ||||
| Echo performance | 35,404 (85.8) | 1981 (69.4) | 37,385 (84.8) | <0.001 |
| Severe LV dysfunction | 2770 (7.8) | 322 (16.3) | 3092 (8.3) | <0.001 |
| LV hypertrophy | 1327 (3.7) | 146 (7.4) | 1473 (3.9) | <0.001 |
| Mitral regurgitation | 1596 (4.5) | 197 (9.9) | 1793 (4.8) | <0.001 |
| Pulmonary hypertension | 1893 (5.3) | 271 (13.7) | 2164 (5.8) | <0.001 |
| Results of angiography c | ||||
| Angiography performance | 32,221 (78.1) | 1449 (50.8) | 33,670 (76.4) | <0.001 |
| Measure of CAD, No or non-significant | 1587 (4.9) | 92 (6.3) | 1679 (5.0) | <0.001 |
| One vessel | 8453 (26.2) | 249 (17.2) | 8702 (25.8) | |
| Two vessels | 9154 (28.4) | 342 (23.6) | 9496 (28.2) | |
| Three vessels/LM | 13,027 (40.4) | 766 (52.9) | 13,793 (41.0) | |
| Characteristics of the follow-up | ||||
| Compliance to the medical treatment during the first year d | 9825 (23.8) | 429 (15.0) | 10,254 (23.3) | <0.001 |
| Length of follow-up (years), Mean (SD) | 4.59 (2.65) | 4.60 (2.45) | 4.59 (2.64) | 0.908 |
| 1–5 | 5636 (13.7) | 180 (6.3) | 5816 (13.2) | <0.001 |
| 5–10 | 35,608 (86.3) | 2675 (93.7) | 38,283 (86.8) | |
| Parameter | Percentiles | Values | Study Group | Total | p | |
|---|---|---|---|---|---|---|
| Years of Survival | Years of Death | |||||
| n (Person-Years) | 41,244 | 2855 | 44,099 | |||
| LOS (Days) | ||||||
| Mean (SD) | 3.15 (12.23) | 17.59 (27.269) | 4.08 (14.16) | <0.001 | ||
| 10–50 | 0 | 28,611 (69.4) | 705 (24.7) | 29,316 (66.5) | <0.001 | |
| 60 | 1–2 | 3486 (8.5) | 165 (5.8) | 3651 (8.3) | ||
| 70 | 2–5 | 3339 (8.1) | 287 (10.1) | 3626 (8.2) | ||
| 80 | 5–13 | 3098 (7.5) | 542 (19.0) | 3640 (8.3) | ||
| 90 | ≥14 | 2710 (6.6) | 1156 (40.5) | 3866 (8.8) | ||
| Number of ED visits a | ||||||
| Mean (SD) | 0.32 (2.24) | 0.57 (3.81) | 0.332 (2.37) | <0.001 | ||
| 0–80 | 0–1 | 38,444 (93.2) | 2270 (79.5) | 40,714 (92.3) | <0.001 | |
| 90 | ≥2 | 2800 (6.8) | 585 (20.5) | 3385 (7.7) | ||
| Number of primary clinic visits | ||||||
| Mean (SD) | 12.96 (11.30) | 13.26 (13.41) | 12.98 (11.45) | 0.237 | ||
| 10–30 | 0–6 | 11,883 (28.8) | 1041 (36.5) | 12,924 (29.3) | <0.001 | |
| 40–70 | 6–17 | 17,181 (41.7) | 939 (32.9) | 18,120 (41.1) | ||
| 80–90 | ≥18 | 12,180 (29.5) | 875 (30.7) | 13,055 (29.6) | ||
| Number of ambulatory visits | ||||||
| Mean (SD) | 10.29 (21.24) | 11.90 (28.90) | 10.39 (21.82) | 0.003 | ||
| 10–40 | 0–3 | 17,964 (43.6) | 1566 (54.9) | 19,530 (44.3) | <0.001 | |
| 50 | 3–5 | 3708 (9.0) | 241 (8.4) | 3949 (9.0) | ||
| 60–90 | ≥6 | 19,572 (47.5) | 1048 (36.7) | 20,620 (46.8) | ||
| Number of consultant visits | ||||||
| Mean (SD) | 1.48 (2.25) | 0.90 (1.95) | 1.45 (2.23) | <0.001 | ||
| 10–50 | 0–1 | 19,599 (47.5) | 1847 (64.7) | 21,446 (48.6) | <0.001 | |
| 60–90 | ≥2 | 21,645 (52.5) | 1008 (35.3) | 22,653 (51.4) | ||
| Total cost (USD) | ||||||
| Mean (SD) | 3757.16 (9194.36) | 8428.67 (15,178.26) | 4059.60 (9761.90) | <0.001 | ||
| 10–60 | <3491 | 29,470 (71.5) | 1401 (49.1) | 30,871 (70.0) | <0.001 | |
| 70 | 3491–4765 | 4101 (9.9) | 308 (10.8) | 4409 (10.0) | ||
| 80 | 4765–7300 | 3995 (9.7) | 415 (14.5) | 4410 (10.0) | ||
| 90 | ≥7300 | 3678 (8.9) | 731 (25.6) | 4409 (10.0) | ||
| Model a | Parameter | Percentiles | Values | OR | (95% CI) | p |
|---|---|---|---|---|---|---|
| a. | LOS (Days) | 10–50 | 0 | 1 (ref.) | ||
| 60 | 1–2 | 1.921 | (1.615; 2.284) | <0.001 | ||
| 70 | 2–5 | 3.488 | (3.025; 4.022) | <0.001 | ||
| 80 | 5–13 | 7.100 | (6.305; 7.996) | <0.001 | ||
| 90 | ≥14 | 17.311 | (15.638; 19.164) | <0.001 | ||
| a. | Number of ED visits b | 10–80 | 0–1 | 1 (ref.) | ||
| 90 | ≥2 | 3.538 | (3.204; 3.908) | <0.001 | ||
| a. | Number of primary clinic visits | 10–30 | 0–6 | 1 (ref.) | ||
| 40–70 | 6–17 | 0.624 | (0.570; 0.683) | <0.001 | ||
| 80–90 | ≥18 | 0.820 | (0.748; 0.899) | <0.001 | ||
| a. | Number of ambulatory visits | 10–40 | 0–3 | 1 (ref.) | ||
| 50 | 3–5 | 0.746 | (0.648; 0.858) | <0.001 | ||
| 60–90 | ≥6 | 0.614 | (0.568; 0.665) | <0.001 | ||
| a. | Number of consultant visits | 10–50 | 0–1 | 1 (ref.) | ||
| 60–90 | ≥2 | 0.494 | (0.457; 0.534) | <0.001 | ||
| b. | LOS (Days) | 10–50 | 0 | 1 (ref.) | ||
| 60 | 1–2 | 2.857 | (2.386; 3.421) | <0.001 | ||
| 70 | 2–5 | 5.138 | (4.418; 5.975) | <0.001 | ||
| 80 | 5–13 | 10.414 | (9.124; 11.885) | <0.001 | ||
| 90 | ≥14 | 25.160 | (22.279; 28.413) | <0.001 | ||
| Number of ED visits b | 10–80 | 0–1 | 1 (ref.) | |||
| 90 | ≥2 | 2.526 | (2.242; 2.844) | <0.001 | ||
| Number of primary clinic visits | 10–30 | 0–6 | 1 (ref.) | |||
| 40–70 | 6–17 | 0.527 | (0.474; 0.587) | <0.001 | ||
| 80–90 | ≥18 | 0.385 | (0.339; 0.437) | <0.001 | ||
| Number of ambulatory visits | 10–40 | 0–3 | 1 (ref.) | |||
| 50 | 3–5 | 0.682 | (0.586; 0.795) | <0.001 | ||
| 60–90 | ≥6 | 0.585 | (0.532; 0.643) | <0.001 | ||
| Number of consultant visits | 10–50 | 0–1 | 1 (ref.) | |||
| 60–90 | ≥2 | 0.591 | (0.537; 0.650) | <0.001 | ||
| c. | LOS (Days) | 10–50 | 0 | 1 (ref.) | ||
| 60 | 1–2 | 2.445 | (2.032; 2.942) | <0.001 | ||
| 70 | 2–5 | 3.537 | (3.029; 4.130) | <0.001 | ||
| 80 | 5–13 | 6.619 | (5.768; 7.595) | <0.001 | ||
| 90 | ≥14 | 16.257 | (14.281; 18.507) | <0.001 | ||
| Number of ED visits b | 10–80 | 0–1 | 1 (ref.) | |||
| 90 | ≥2 | 2.675 | (2.346; 3.051) | <0.001 | ||
| Number of primary clinic visits | 10–30 | 0–6 | 1 (ref.) | <0.001 | ||
| 40–70 | 6–17 | 0.565 | (0.505; 0.632) | <0.001 | ||
| 80–90 | ≥18 | 0.411 | (0.357; 0.474) | <0.001 | ||
| Number of ambulatory visits | 10–40 | 0–3 | 1 (ref.) | |||
| 50 | 3–5 | 0.679 | (0.578; 0.798) | <0.001 | ||
| 60–90 | ≥6 | 0.587 | (0.526; 0.656) | <0.001 | ||
| Number of consultant visits | 10–50 | 0–1 | 1 (ref.) | |||
| 60–90 | ≥2 | 0.642 | (0.579; 0.712) | <0.001 | ||
| d. | Total cost (USD) | 10–60 | <3491 | 1 (ref.) | ||
| 70 | 3491–4765 | 1.580 | (1.391; 1.794) | <0.001 | ||
| 80 | 4765–7300 | 2.185 | (1.947; 2.452) | <0.001 | ||
| 90 | ≥7300 | 4.181 | (3.809; 4.589) | <0.001 | ||
| e. | Total cost (USD) | 10–60 | <3491 | 1 (ref.) | ||
| 70 | 3491–4765 | 1.376 | (1.204; 1.573) | <0.001 | ||
| 80 | 4765–7300 | 1.919 | (1.697; 2.170) | <0.001 | ||
| 90 | ≥7300 | 3.430 | (3.055; 3.851) | <0.001 |
Disclaimer/Publisher’s Note: The statements, opinions and data contained in all publications are solely those of the individual author(s) and contributor(s) and not of MDPI and/or the editor(s). MDPI and/or the editor(s) disclaim responsibility for any injury to people or property resulting from any ideas, methods, instructions or products referred to in the content. |
© 2023 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Plakht, Y.; Gilutz, H.; Arbelle, J.E.; Greenberg, D.; Shiyovich, A. Healthcare Resources Utilization throughout the Last Year of Life after Acute Myocardial Infarction. J. Clin. Med. 2023, 12, 2773. https://doi.org/10.3390/jcm12082773
Plakht Y, Gilutz H, Arbelle JE, Greenberg D, Shiyovich A. Healthcare Resources Utilization throughout the Last Year of Life after Acute Myocardial Infarction. Journal of Clinical Medicine. 2023; 12(8):2773. https://doi.org/10.3390/jcm12082773
Chicago/Turabian StylePlakht, Ygal, Harel Gilutz, Jonathan Eli Arbelle, Dan Greenberg, and Arthur Shiyovich. 2023. "Healthcare Resources Utilization throughout the Last Year of Life after Acute Myocardial Infarction" Journal of Clinical Medicine 12, no. 8: 2773. https://doi.org/10.3390/jcm12082773





