Cardiovascular and Neurological Complications of COVID-19: A Narrative Review
Abstract
:1. Introduction
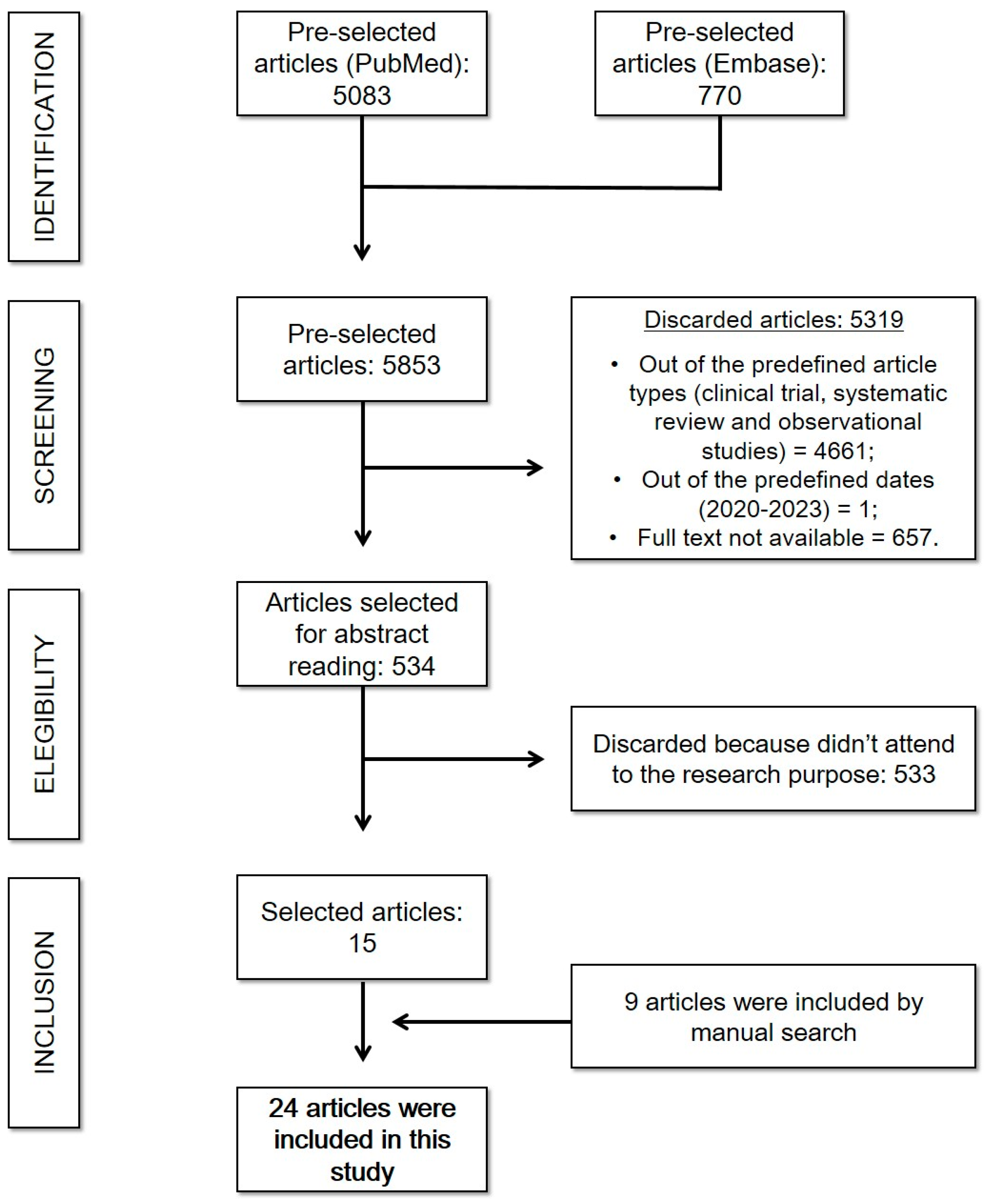
2. Methods
3. Results
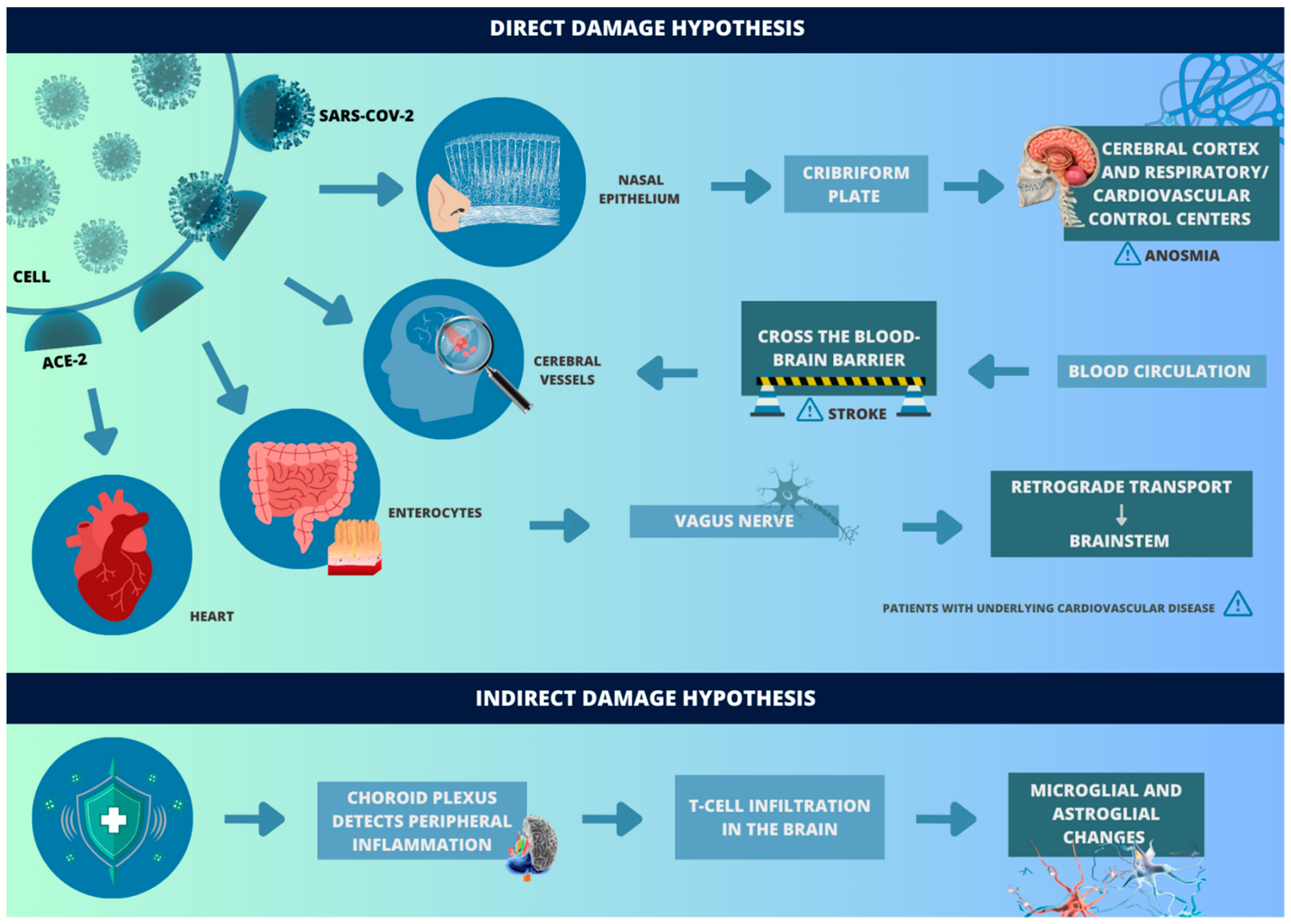
3.1. Pathophysiology and Clinical Features
3.2. Acute Complications
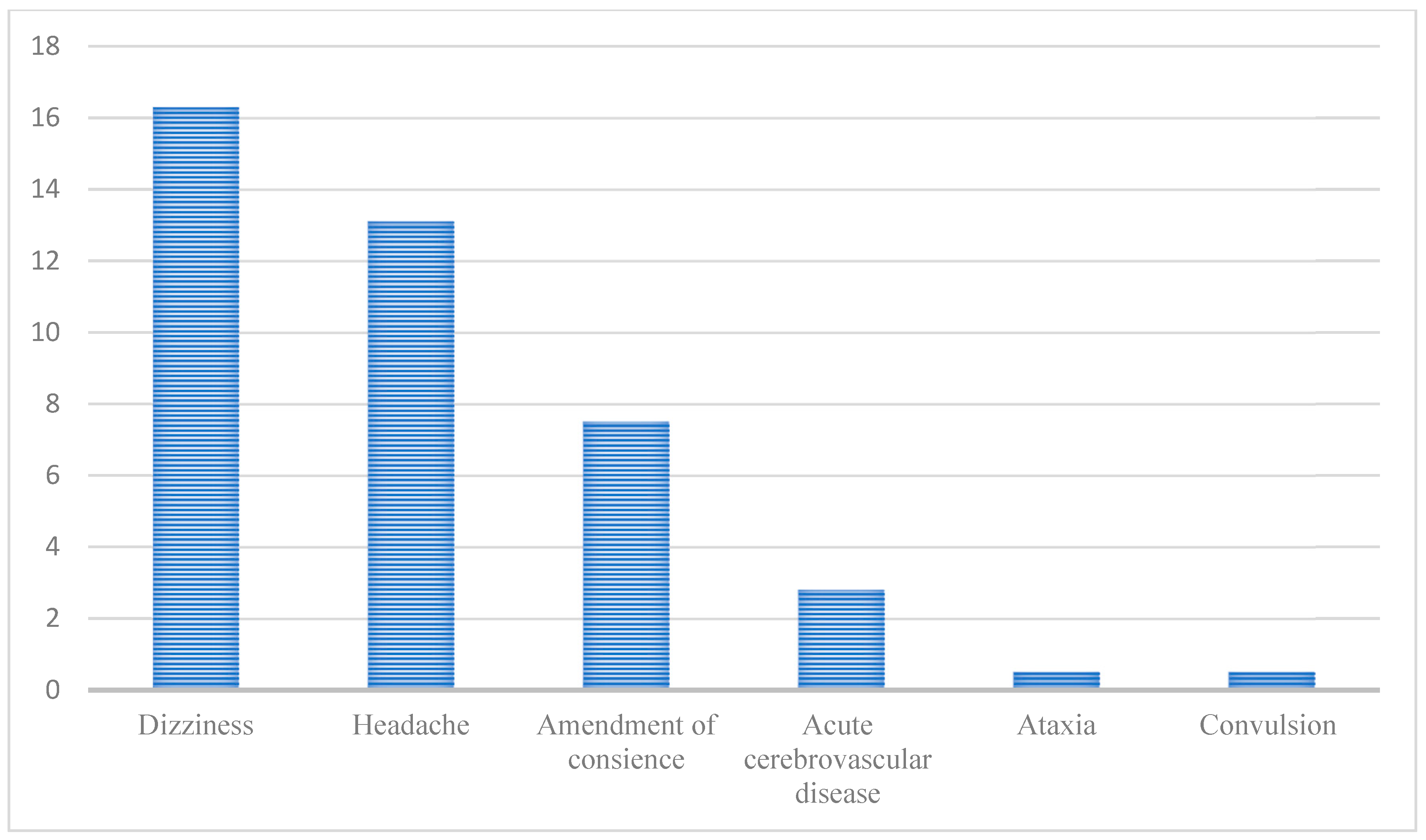
3.2.1. Acute Complications Related to Neurological System
Anosmia and Ageusia
Acute Cerebrovascular Disease
3.2.2. Acute Complications Related to Cardiovascular System
Myocardial Injury and Myocarditis
Stress Cardiomyopathy
Arrhythmias
Heart Failure
3.3. Long-Term Complications
3.3.1. Neurologic Long-Term Complications
3.3.2. Cardiovascular Long-Term Complications
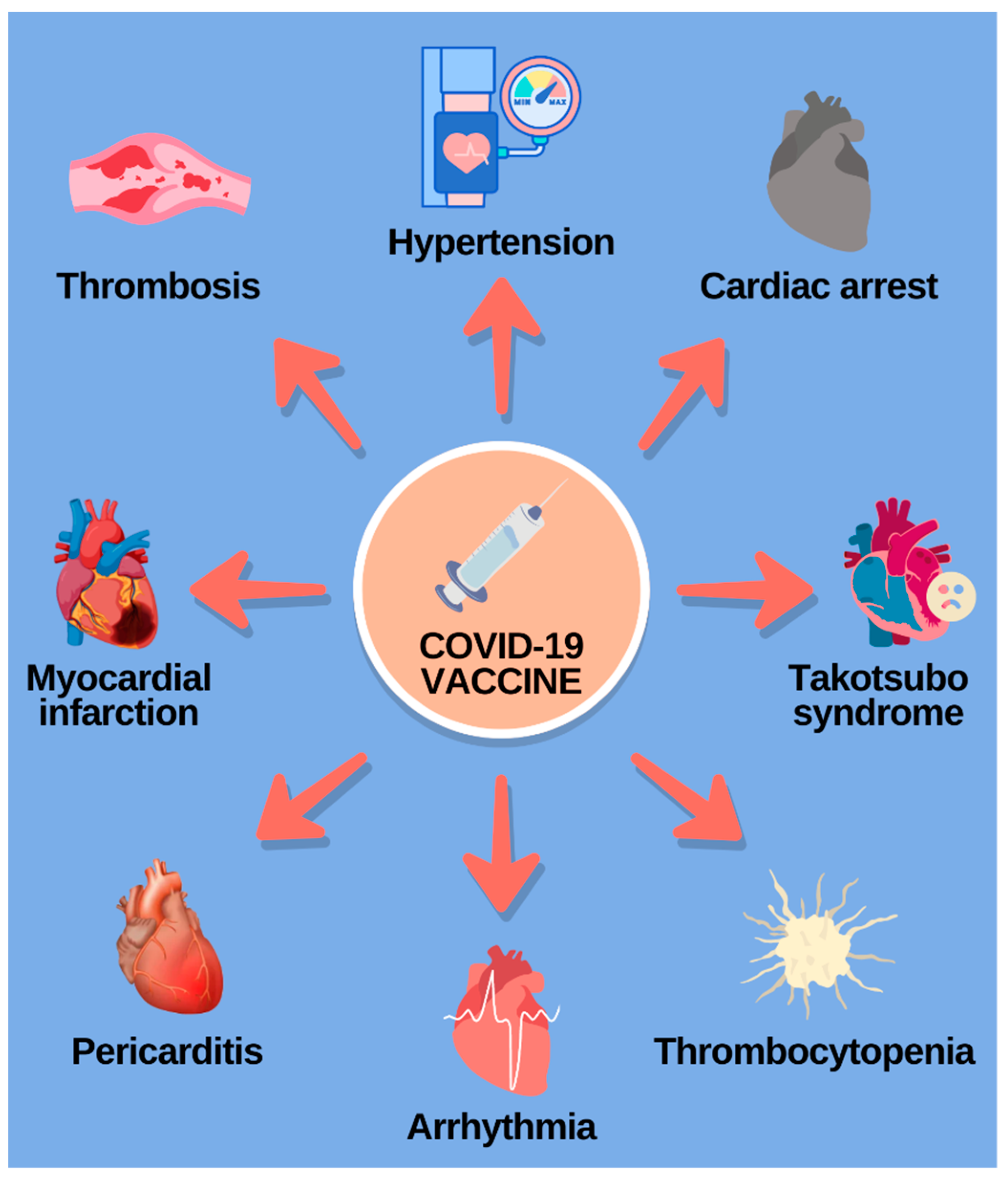
3.4. Post-Vaccine Complications
3.4.1. Cardiovascular Post-Vaccine Complications
3.4.2. Neurologic Post-Vaccine Complications
4. Conclusions
Funding
Conflicts of Interest
References
- Hui, D.S.; Azhar, E.I.; Madani, T.A.; Ntoumi, F.; Kock, R.; Dar, O.; Ippolito, G.; Mchugh, T.D.; Memish, Z.A.; Drosten, C.; et al. The continuing 2019-nCoV epidemic threat of novel coronaviruses to global health—The latest 2019 novel coronavirus outbreak in Wuhan, China. Psychiatry Res. 2020, 14, 264–266. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Deng, S.-Q.; Peng, H.-J. Characteristics of and Public Health Responses to the Coronavirus Disease 2019 Outbreak in China. J. Clin. Med. 2020, 9, 575. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Hu, B.; Guo, H.; Zhou, P.; Shi, Z.L. Characteristics of SARS-CoV-2 and COVID-19. Nat. Rev. Microbiol. 2021, 19, 141–154. [Google Scholar] [CrossRef]
- Wu, Z.; McGoogan, J.M. Characteristics of and Important Lessons from the Coronavirus Disease 2019 (COVID-19) Outbreak in China: Summary of a Report of 72314 Cases from the Chinese Center for Disease Control and Prevention. JAMA J. Am. Med. Assoc. 2020, 323, 1239–1242. [Google Scholar] [CrossRef]
- Pelosi, P.; Tonelli, R.; Torregiani, C.; Baratella, E.; Confalonieri, M.; Battaglini, D.; Marchioni, A.; Confalonieri, P.; Clini, E.; Salton, F.; et al. Different Methods to Improve the Monitoring of Noninvasive Respiratory Support of Patients with Severe Pneumonia/ARDS Due to COVID-19: An Update. J. Clin. Med. 2022, 11, 1704. [Google Scholar] [CrossRef] [PubMed]
- Guan, W.J.; Ni, Z.Y.; Hu, Y.; Liang, W.H.; Qu, C.Q.; He, J.X.; Liu, L.; Shan, H.; Lei, C.L.; Hui, D.S.C.; et al. Clinical Characteristics of Coronavirus Disease 2019 in China. New Engl. J. Med. 2020, 382, 1708–1720. [Google Scholar] [CrossRef]
- Chen, N.; Zhou, M.; Dong, X.; Qu, J.; Gong, F.; Han, Y.; Qiu, Y.; Wang, J.; Liu, Y.; Wei, Y.; et al. Epidemiological and clinical characteristics of 99 cases of 2019 novel coronavirus pneumonia in Wuhan, China: A descriptive study. Lancet 2020, 395, 507–513. [Google Scholar] [CrossRef] [Green Version]
- Zambelli, G. Clinical cases. Psicoter. E Sci. Um. 2021, 8960, 511–513. [Google Scholar]
- Fritsche, L.G.; Jin, W.; Admon, A.J.; Mukherjee, B. Characterizing and Predicting Post-Acute Sequelae of SARS CoV-2 1 Infection (PASC) in a Large Academic Medical Center in the US 2 3. Available online: https://www.medrxiv.org/content/10.1101/2022.10.21.22281356v3 (accessed on 30 January 2023).
- Martínez, H.R.; Figueroa-Sánchez, J.A.; Castilleja-Leal, F.; Martínez-Reséndez, M.F.; Ferrigno, A. The underrated nervous system involvement by COVID-19. Rev. Mex. Neurocienc. 2020, 21, 158–162. [Google Scholar] [CrossRef]
- Song, J.; Li, Y.; Huang, X.; Chen, Z.; Li, Y.; Liu, C.; Chen, Z.; Duan, X. Systematic analysis of ACE2 and TMPRSS2 expression in salivary glands reveals underlying transmission mechanism caused by SARS-CoV-2. J. Med. Virol. 2020, 92, 2556–2566. [Google Scholar] [CrossRef]
- Hamming, I.; Timens, W.; Bulthuis, M.L.C.; Lely, A.T.; Navis, G.J.; van Goor, H. Tissue distribution of ACE2 protein, the functional receptor for SARS coronavirus. A first step in understanding SARS pathogenesis. J. Pathol. 2004, 203, 631–637. [Google Scholar] [CrossRef] [PubMed]
- Meinhardt, J.; Radke, J.; Dittmayer, C.; Franz, J.; Thomas, C.; Mothes, R.; Laue, M.; Schneider, J.; Brünink, S.; Greuel, S.; et al. Olfactory transmucosal SARS-CoV-2 invasion as a port of central nervous system entry in individuals with COVID-19. Nat. Neurosci. 2021, 24, 168–175. [Google Scholar] [CrossRef] [PubMed]
- Achar, A.; Ghosh, C. COVID-19-Associated Neurological Disorders: The Potential Route of CNS Invasion and Blood-Brain Relevance. Cells 2020, 9, 2360. [Google Scholar] [CrossRef] [PubMed]
- Awogbindin, I.O.; Ben-Azu, B.; Olusola, B.A.; Akinluyi, E.T.; Adeniyi, P.A.; Di Paolo, T.; Tremblay, M.È. Microglial Implications in SARS-CoV-2 Infection and COVID-19: Lessons From Viral RNA Neurotropism and Possible Relevance to Parkinson’s Disease. Front. Cell Neurosci. 2021, 15, 670298. [Google Scholar] [CrossRef]
- YYang, A.C.; Kern, F.; Losada, P.M.; Agam, M.R.; Maat, C.A.; Schmartz, G.P.; Fehlmann, T.; Stein, J.A.; Schaum, N.; Lee, D.P.; et al. Dysregulation of brain and choroid plexus cell types in severe COVID-19. Nature 2021, 595, 565–571. [Google Scholar] [CrossRef]
- Bourgonje, A.R.; Abdulle, A.E.; Timens, W.; Hillebrands, J.L.; Navis, G.J.; Gordijn, S.J.; Bolling, M.C.; Dijkstra, G.; Voors, A.A.; Osterhaus, A.D.; et al. Angiotensin-converting enzyme 2 (ACE2), SARS-CoV-2 and the pathophysiology of coronavirus disease 2019 (COVID-19). J. Pathol. 2020, 251, 228–248. [Google Scholar] [CrossRef] [PubMed]
- Chang, W.T.; Toh, H.S.; Liao, C.T.; Yu, W.L. Cardiac Involvement of COVID-19: A Comprehensive Review Wei-Ting. Am. J. Med. Sci. 2021, 21, 14–22. [Google Scholar] [CrossRef]
- Dahm, T.; Rudolph, H.; Schwerk, C.; Schroten, H.; Tenenbaum, T. Neuroinvasion and Inflammation in Viral Central Nervous System Infections. Mediat. Inflamm. 2016, 2016, 8562805. [Google Scholar] [CrossRef] [Green Version]
- Robinson, C.P.; Busl, K.M. Neurologic Manifestations of Severe Respiratory Viral Contagions. Crit. Care Explor. 2020, 2, e0107. [Google Scholar] [CrossRef]
- Boldrini, M.; Canoll, P.D.; Klein, R.S. How COVID-19 Affects the Brain. JAMA Psychiatry. Am. Med. Assoc. 2021, 78, 682–683. [Google Scholar] [CrossRef]
- Carod-Artal, F.; García-Moncó, J. Epidemiology, pathophysiology, and classification of the neurological symptoms of post-COVID-19 syndrome. Neurol. Perspect. 2021, 1, S5–S15. [Google Scholar] [CrossRef] [PubMed]
- Akbarialiabad, H.; Hossein, M.; Ashkan, T.; Nasrollah, A. Long COVID, a comprehensive systematic scoping review. Infection 2021, 49, 1163–1186. [Google Scholar] [CrossRef] [PubMed]
- Pleasure, S.J.; Green, A.J.; Josephson, S.A. The Spectrum of Neurologic Disease in the Severe Acute Respiratory Syndrome Coronavirus 2 Pandemic Infection: Neurologists Move to the Frontlines. JAMA Neurol. 2020, 77, 679–680. [Google Scholar] [CrossRef] [PubMed]
- Beyrouti, R.; Adams, E.M.; Benjamin, L.; Cohen, H.; Farmer, S.F.; Goh, Y.Y.; Humphries, F.; Jäger, H.R.; Losseff, A.N.; Perry, R.J.; et al. Characteristics of ischaemic stroke associated with COVID-19. J. Neurol. Neurosurg. Psychiatry 2020, 91, 889–891. [Google Scholar] [CrossRef] [PubMed]
- Stiller, K. Physiotherapy in intensive care: An updated systematic review. Chest 2013, 144, 825–847. [Google Scholar] [CrossRef]
- Correia, A.O.; Feitosa, P.W.G.; Moreira, J.L.D.S.; Nogueira, S.R.; Fonseca, R.B.; Nobre, M.E.P. Neurological manifestations of COVID-19 and other coronaviruses: A systematic review. Neurol. Psychiatry Brain Res. 2020, 37, 27–32. [Google Scholar] [CrossRef]
- Madani Neishaboori, A.; Moshrefiaraghi, D.; Mohamed Ali, K.; Toloui, A.; Yousefifard, M.; Hosseini, M. Central Nervous System Complications in COVID-19 Patients; a Systematic Review and Meta-Analysis based on Current Evidence. Arch. Acad. Emerg. Medicine. 2020, 8, e62. Available online: http://journals.sbmu.ac.ir/aaem (accessed on 3 February 2023).
- Teixeira-Vaz, A.; Rocha, J.A.; Reis DA e Oliveira, M.; Moreira, T.S.; Silva, A.I.; Monteiro-Soares, M.; Paiva, J.A. COVID-19 crítico e disfunção neurológica–Uma análise comparativa direta entre o SARS-CoV-2 e outros agentes infecciosos. Rev. Bras. Ter. Intensiva. 2022, 34, 342–350. [Google Scholar] [CrossRef]
- Vargas-Gandica, J.; Winter, D.; Schnippe, R.; Rodriguez-Morales, A.G.; Mondragon, J.; Antezana, J.P.E.; Trelles-Thorne, M.D.P.; Bonilla-Aldana, D.K.; Rodriguez-Morales, A.J.; Paniz-Mondolfi, A. Ageusia and anosmia, a common sign of COVID-19? A case series from four countries. J. NeuroVirol. 2020, 26, 785–789. [Google Scholar] [CrossRef]
- Lee, J.-M.; Lee, S.J. Olfactory and Gustatory Dysfunction in a COVID-19 Patient with Ankylosing Spondylitis Treated with Etanercept: Case Report. J. Korean Med. Sci. 2020, 35, e201. [Google Scholar] [CrossRef]
- AghAghagoli, G.; Marin, B.G.; Katchur, N.; Chaves-Sell, F.; Asaad, W.F.; Murphy, S.A. Neurological Involvement in COVID-19 and Potential Mechanisms: A Review. Neurocritical Care 2020, 34, 1062–1071. [Google Scholar] [CrossRef]
- Boscutti, A.; Delvecchio, G.; Pigoni, A.; Cereda, G.; Ciappolino, V.; Bellani, M.; Fusar-Poli, P.; Brambilla, P. Olfactory and gustatory dysfunctions in SARS-CoV-2 infection: A systematic review. Brain Behav. Immun. Health 2021, 15, 100268. [Google Scholar] [CrossRef] [PubMed]
- Maury, A.; Lyoubi, A.; Peiffer-Smadja, N.; de Broucker, T.; Meppiel, E. Neurological manifestations associated with SARS-CoV-2 and other coronaviruses: A narrative review for clinicians. Rev. Neurol. 2021, 177, 51–64. [Google Scholar] [CrossRef] [PubMed]
- Fotuhi, M.; Mian, A.; Meysami, S.; Raji, C.A. Neurobiology of COVID-19. J. Alzheimer’s Dis. 2020, 76, 3–19. [Google Scholar] [CrossRef]
- Munhoz, R.P.; Pedroso, J.L.; Nascimento, F.A.; Almeida, S.M.; Barsottini, O.G.P.; Cardoso, F.E.C.; Teive, H.A.G. Neurological complications in patients with SARS-CoV-2 infection: A systematic review. Arq. Neuropsiquiatr. 2020, 78, 290–300. [Google Scholar] [CrossRef]
- Neto, J.C.; Feitosa, E.M.S.; Cunha, B.S.; Nascimento, M.N.R.; Félix, N.D.D.C. Stroke in COVID-19 patients: A scoping review. Texto Context. Enferm. 2021, 30. [Google Scholar]
- Varatharaj, A.; Thomas, N.; Ellul, A.M.; Davies, N.W.; Pollak, A.T.; Tenorio, E.L.; Sultan, M.; Easton, A.; Breen, G.; Zandi, M.; et al. Neurological and neuropsychiatric complications of COVID-19 in 153 patients: A UK-wide surveillance study. Lancet Psychiatry 2020, 7, 875–882. [Google Scholar] [CrossRef]
- Hess, D.C.; Eldahshan, W.; Rutkowski, E. COVID-19-Related Stroke. Transl. Stroke Res. 2020, 11, 322–325. [Google Scholar] [CrossRef]
- Wang, A.; Mandigo, G.K.; Yim, P.D.; Meyers, P.M.; LaVine, S.D. Stroke and mechanical thrombectomy in patients with COVID-19: Technical observations and patient characteristics. J. NeuroInterv. Surg. 2020, 12, 648–653. [Google Scholar] [CrossRef]
- Kunal, S.; Sharma, S.M.; Sharma, S.K.; Gautam, D.; Bhatia, H.; Mahla, H.; Sharma, S.; Bhandari, S. Cardiovascular complications and its impact on outcomes in COVID-19. Indian Hear. J. 2020, 72, 593–598. [Google Scholar] [CrossRef]
- Castiello, T.; Georgiopoulos, G.; Finocchiaro, G.; Claudia, M.; Gianatti, A.; Delialis, D.; Aimo, A.; Prasad, S. COVID-19 and myocarditis: A systematic review and overview of current challenges. Hear. Fail. Rev. 2021, 27, 251–261. [Google Scholar] [CrossRef] [PubMed]
- Jaiswal, V.; Sarfraz, Z.; Sarfraz, A.; Mukherjee, D.; Batra, N.; Hitawala, G.; Yaqoob, S.; Patel, A.; Agarwala, P.; Ruchika Sarfraz, M.; et al. COVID-19 Infection and Myocarditis: A State-of-the-Art Systematic Review. J. Prim. Care Community Health 2021, 12, 21501327211056800. [Google Scholar] [CrossRef] [PubMed]
- Guo, T.; Fan, Y.; Chen, M.; Wu, X.; Zhang, L.; He, T.; Wang, H.; Wan, J.; Wang, X.; Lu, Z. Cardiovascular Implications of Fatal Outcomes of Patients With Coronavirus Disease 2019 (COVID-19). JAMA Cardiol. 2020, 5, 811–818. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Sandoval, Y.; Januzzi, J.; Jaffe, A. Cardiac Troponin for Assessment of Myocardial Injury in COVID-19. J. Am. Coll. Cardiol. 2020, 8, 147–154. [Google Scholar] [CrossRef] [PubMed]
- Singh, S.; Desai, R.; Gandhi, Z.; Fong, H.K.; Doreswamy, S.; Desai, V.; Chockalingam, A.; Mehta, P.K.; Sachdeva, R.; Kumar, G. Takotsubo Syndrome in Patients with COVID-19: A Systematic Review of Published Cases. SN Compr. Clin. Med. 2020, 2, 2102–2108. [Google Scholar] [CrossRef]
- Techasatian, W.; Nishimura, Y.; Nagamine, T.; Ha, G.; Huang, R.; Shah, P.; Yeo, J.; Kanitsoraphan, C. Characteristics of Takotsubo cardiomyopathy in patients with COVID-19: Systematic scoping review. Am. Hear. J. Plus Cardiol. Res. Pr. 2022, 13, 100092. [Google Scholar] [CrossRef]
- McCullough, S.A.; Goyal, P.; Krishnan, U.; Choi, J.J.; Safford, M.M.; Okin, P.M. Electrocardiographic Findings in Coronavirus Disease-19: Insights on Mortality and Underlying Myocardial Processes. J. Cardiac Fail. 2020, 26, 626–632. [Google Scholar] [CrossRef]
- Pellicori, P.; Doolub, G.; Wong, C.M.; Lee, K.S.; Mangion, K.; Ahmad, M.; Berry, C.; Squire, I.; Lambiase, P.D.; Lyon, A.; et al. COVID-19 and its cardiovascular effects: A systematic review of prevalence studies. Cochrane Database Syst. Rev. 2021, 3, CD013879. [Google Scholar]
- Rey, J.R.; Caro-Codón, J.; Rosillo, S.O.; Iniesta, Á.M.; Castrejón-Castrejón, S.; Marco-Clement, I.; Martín-Polo, L.; Merino-Argos, C.; Rodríguez-Sotelo, L.; García-Veas, J.M.; et al. Heart failure in COVID-19 patients: Prevalence, incidence and prognostic implications. Eur. J. Heart Fail 2020, 22, 2205–2215. [Google Scholar] [CrossRef]
- Garrigues, E.; Janvier, P.; Kherabi, Y.; Le Bot, A.; Hamon, A.; Gouze, H.; Doucet, L.; Berkani, S.; Oliosi, E.; Mallart, E.; et al. Post-discharge persistent symptoms and health-related quality of life after hospitalization for COVID-19. J. Infect. 2020, 81, e4–e6. [Google Scholar] [CrossRef]
- Gadani, S.P.; Cronk, J.C.; Norris, G.T.; Kipnis, J. IL-4 in the Brain: A Cytokine To Remember. J. Immunol. 2012, 189, 4213–4219. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Sun, B.; Tang, N.; Peluso, M.J.; Iyer, N.S.; Torres, L.; Donatelli, J.L.; Munter, S.E.; Nixon, C.C.; Rutishauser, R.L.; Rodriguez-Barraquer, I.; et al. Characterization and Biomarker Analyses of Post-COVID-19 Complications and Neurological Manifestations. Cells 2021, 10, 386. [Google Scholar] [CrossRef] [PubMed]
- Espíndola, O.M.; Gomes, Y.C.P.; Brandão, C.O.; Torres, R.C.; Siqueira, M.; Soares, C.N.; Lima, M.A.S.D.; Leite, A.C.C.B.; Venturotti, C.O.; Carvalho, A.J.C.; et al. Inflammatory Cytokine Patterns Associated with Neurological Diseases in Coronavirus Disease 2019. Ann. Neurol. 2021, 89, 1041–1045. [Google Scholar] [CrossRef] [PubMed]
- Pilotto, A.; Cristillo, V.; Piccinelli, S.C.; Zoppi, N.; Bonzi, G.; Sattin, D.; Schiavolin, S.; Raggi, A.; Canale, A.; Gipponi, S.; et al. Long-term neurological manifestations of COVID-19: Prevalence and predictive factors. Neurol. Sci. 2021, 42, 4903–4907. [Google Scholar] [CrossRef]
- Metlay, J.P.; Fine, M.J.; Schulz, R.; Marrie, T.J.; Coley, C.M.; Kapoor, W.N.; Singer, D.E. Measuring symptomatic and functional recovery in patients with community-acquired pneumonia. J. Gen. Intern. Med. 1997, 12, 423–430. [Google Scholar] [CrossRef] [Green Version]
- Sarfraz, Z.; Sarfraz, A.; Barrios, A.; Garimella, R.; Dominari, A.; Kc, M.; Pandav, K.; Pantoja, J.C.; Retnakumar, V.; Cherrez-Ojeda, I. Cardio-Pulmonary Sequelae in Recovered COVID-19 Patients: Considerations for Primary Care. J. Prim. Care Community Health 2021, 12, 21501327211023726. [Google Scholar] [CrossRef]
- Elseidy, S.A.; Awad, A.K.; Vorla, M.; Fatima, A.; Elbadawy, M.A.; Mandal, D.; Mohamad, T. Cardiovascular complications in the Post-Acute COVID-19 syndrome (PACS). IJC Hear. Vasc. 2022, 40, 101012. [Google Scholar] [CrossRef]
- Puntmann, V.O.; Carerj, M.L.; Wieters, I.; Fahim, M.; Arendt, C.; Hoffmann, J.; Shchendrygina, A.; Escher, F.; Vasa-Nicotera, M.; Zeiher, A.M.; et al. Outcomes of Cardiovascular Magnetic Resonance Imaging in Patients Recently Recovered From Coronavirus Disease 2019 (COVID-19). JAMA Cardiol. 2020, 5, 1265. [Google Scholar] [CrossRef]
- Liu, R.; Pan, J.; Zhang, C.; Sun, X. Cardiovascular Complications of COVID-19 Vaccines. Front. Cardiovasc. Med. 2022, 9, 1–7. [Google Scholar] [CrossRef]
- Li, Y.E.; Wang, S.; Reiter, R.J.; Ren, J. International Journal of Infectious Diseases Clinical cardiovascular emergencies and the cellular basis of COVID-19 vaccination: From dream to reality? Int. J. Infect. Dis. 2022, 124, 1–10. [Google Scholar] [CrossRef]
- De Amaral, M.E.A.; Ávila, L.R.; de Amaral, B.M.F.; Nasser, A.K.S.; Silva JPM e Taveira, J.H.A. Síndrome de Guillain-Barré associada à COVID-19: Uma revisão sistemática. Res. Soc. Dev. 2021, 10, e198101522585. [Google Scholar] [CrossRef]
- Rao, S.J.; Khurana, S.; Murthy, G.; Dawson, E.T.; Jazebi, N.; Haas, C.J. A case of Guillain–Barre syndrome following Pfizer COVID-19 vaccine. J. Community Hosp. Intern. Med. Perspect. 2021, 11, 597–600. [Google Scholar] [CrossRef] [PubMed]

| Neurological Complications | |
|---|---|
| Early Complications | Late Complications |
| Anosmia/ageusia | Memory problems |
| Acute cerebrovascular disease | Learning problems |
| Delirium | Hallucinations |
| Seizures | Alteration of neuroplasticity |
| Encephalopathy | Increased risk of stroke |
| Cardiovascular Complications | |
|---|---|
| Early Complications | Late Complications |
| Myocardial injury and Myocarditis | Myocardial inflammation |
| Stress cardiomyopathy | Regional scar |
| Arrhythmias | Pericardial enhancement |
| Heart failure | |
| Manifestation | Total Cases N | Janssen N (%) | Moderna N (%) | Pfizer N (%) | Unknown N (%) |
|---|---|---|---|---|---|
| Acute cardiac event | 68 | 4 (5.8%) | 22 (32.3%) | 42 (61.7%) | - |
| Arrhythmia | 16,046 | 475 (2.9%) | 2606 (16.2%) | 12,881 (80.2%) | 84 (0.5%) |
| Cardiac failure | 3325 | 88 (2.6%) | 650 (19.5%) | 2562 (77.0%) | 25 (0.7%) |
| Cardiac valve disease | 137 | 10 (7.2%) | 26 (18.9%) | 100 (72.9%) | 1 (0.7%) |
| Cardiomegaly | 1315 | 61 (4.6%) | 437 (33.2%) | 808 (61.4%) | 9 (0.6%) |
| Endocarditis | 234 | 14 (5.9%) | 50 (21.3%) | 170 (72.6%) | - |
| Myocarditis | 16,902 | 255 (1.5%) | 3929 (23.2%) | 12,641 (74.7%) | 77 (0.4%) |
| Pericarditis | 11,241 | 204 (1.8%) | 2108 (18.7%) | 8866 (78.8%) | 63 (0.5%) |
Disclaimer/Publisher’s Note: The statements, opinions and data contained in all publications are solely those of the individual author(s) and contributor(s) and not of MDPI and/or the editor(s). MDPI and/or the editor(s) disclaim responsibility for any injury to people or property resulting from any ideas, methods, instructions or products referred to in the content. |
© 2023 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Sousa Rêgo, L.O.; Alves Braga, L.L.; Vilas-Boas, G.S.; Oliveira Cardoso, M.S.; Duraes, A.R. Cardiovascular and Neurological Complications of COVID-19: A Narrative Review. J. Clin. Med. 2023, 12, 2819. https://doi.org/10.3390/jcm12082819
Sousa Rêgo LO, Alves Braga LL, Vilas-Boas GS, Oliveira Cardoso MS, Duraes AR. Cardiovascular and Neurological Complications of COVID-19: A Narrative Review. Journal of Clinical Medicine. 2023; 12(8):2819. https://doi.org/10.3390/jcm12082819
Chicago/Turabian StyleSousa Rêgo, Luma Ornelas, Lara Landulfo Alves Braga, Gustavo Sampaio Vilas-Boas, Maiana Santos Oliveira Cardoso, and Andre Rodrigues Duraes. 2023. "Cardiovascular and Neurological Complications of COVID-19: A Narrative Review" Journal of Clinical Medicine 12, no. 8: 2819. https://doi.org/10.3390/jcm12082819
APA StyleSousa Rêgo, L. O., Alves Braga, L. L., Vilas-Boas, G. S., Oliveira Cardoso, M. S., & Duraes, A. R. (2023). Cardiovascular and Neurological Complications of COVID-19: A Narrative Review. Journal of Clinical Medicine, 12(8), 2819. https://doi.org/10.3390/jcm12082819









