Outcomes of Endodontic-Treated Teeth Obturated with Bioceramic Sealers in Combination with Warm Gutta-Percha Obturation Techniques: A Prospective Clinical Study
Abstract
:1. Introduction
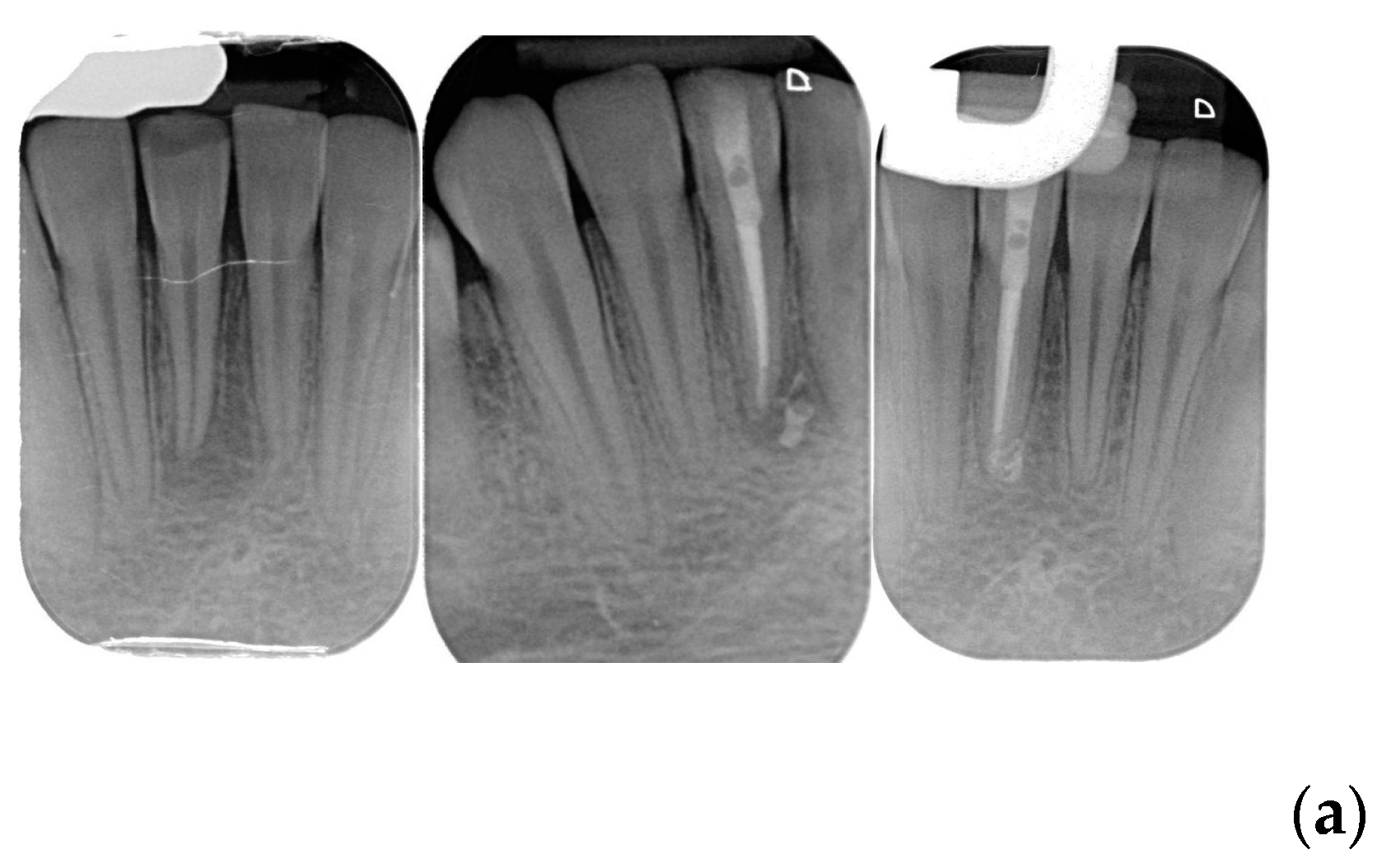
2. Materials and Methods
- Healed: teeth in good function, without symptoms and without radiographic periapical lesion;
- Not healed: nonfunctional teeth with symptoms with or without radiographic periapical lesion or teeth without symptoms with unchanged, new, or enlarged radiographic periapical lesion;
- Healing: teeth that are without symptoms and good function, with a decreased size of radiographic periapical lesion.
2.1. Outcome Evaluation
2.2. Statistical Analysis
3. Results
4. Discussion
5. Conclusions
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Conflicts of Interest
References
- Jeong, J.W.; DeGraft-Johnson, A.; Dorn, S.O.; Di Fiore, P.M. Dentinal Tubule penetration of a calcium silicate–based root canal sealer with different obturation. J. Endod. 2017, 43, 633–637. [Google Scholar] [CrossRef]
- Akesl, H.; Makowka, S.; Bosaid, F.; Sarkar, D.; Azim, A.A. Effect of heat application on the physical properties and chemical structure of calcium silicate-based sealers. Clin. Oral Investig. 2021, 25, 2717–2725. [Google Scholar] [CrossRef] [PubMed]
- Donnermeyer, D.; Ibing, M.; Burklein, S.; Weber, I.; Reitze, M.P.; Schafer, E. Physico-chemical investigation of endodontic sealers exposed to simulated intracanal heat application: Hydraulic calcium silicate-based sealers. Materials 2021, 14, 728. [Google Scholar] [CrossRef]
- Abdellatif, D.; Amato, A.; Calapaj, M.; Pisano, M.; Iandolo, A. A novel modified obturation technique using biosealers: An ex vivo study. J. Conserv. Dent. 2023, 24, 369–373. [Google Scholar]
- Pontoriero, D.I.K.; Ferrari Cagidiaco, E.; Cardinali, F.; Fornara, R.; Amato, M.; Grandini, S.; Ferrari, M. Sealing ability of two bioceramic sealers used in combination with three obturation techniques. J. Osseointegr. 2022, 14, 143–148. [Google Scholar]
- Viola, N.V.; Tanomaru Filho, M.; Cerri, P.S. Mta versus portland cement: Review of literature. RSBO Rev. Sul-Bras. De Odontol. 2011, 8, 446–452. [Google Scholar]
- Prati, C.; Gandolfi, M.G. Calcium silicate bioactive cements: Biological perspectives and clinical applications. Dent. Mater. 2015, 31, 351–370. [Google Scholar] [CrossRef]
- Utneja, S.; Nawal, R.R.; Talwar, S.; Verma, M. Current perspectives of bio-ceramic technology in endodontics: Calcium enriched mixture cement—Review of its composition, properties and applications. Restor. Dent. Endod. 2015, 40, 1–13. [Google Scholar] [CrossRef]
- Jitaru, S.; Hodisan, I.; Timis Lucian, A.; Bud, M. The use of bioceramics in endodontics—Literature review. Clujul. Med. 2016, 89, 470–473. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Arora, V.; Nikhil, V.; Sharma, N.; Arora, P. Bioactive dentin replacement. J. Dent. Med. Sci. 2013, 12, 51–57. [Google Scholar] [CrossRef]
- Malhotra, N.; Agarwal, A.; Mala, K. Mineral trioxide aggregate: A review of physical properties. Compend. Contin. Educ. Dent. 2013, 34, e25–e32. [Google Scholar]
- Parirokh, M.; Torabinejad, M. Mineral trioxide aggregate: A comprehensive literature review—Part I: Chemical, physical, and antibacterial properties. J. Endod. 2010, 36, 16–27. [Google Scholar] [CrossRef] [PubMed]
- Torabinejad, M.; Parirokh, M. Mineral trioxide aggregate: A comprehensive literature review—Part II: Leakage and biocompatibility investigations. J. Endod. 2010, 36, 190–202. [Google Scholar] [CrossRef] [PubMed]
- Parirokh, M.; Torabinejad, M. Mineral trioxide aggregate: A comprehensive literature review—Part III: Clinical applications, drawbacks, and mechanism of action. J. Endod. 2010, 36, 400–413. [Google Scholar] [CrossRef] [PubMed]
- Torabinejad, M.; Parirokh, M.; Dummer, P.M.H. Mineral trioxide aggregate and other bioactive endodontic cements: An updated overview—Part II: Other clinical applications and complications. Int. Endod. J. 2018, 51, 284–317. [Google Scholar] [CrossRef]
- Pontoriero, D.I.K.; Madaro, G.; Vanagolli, V.; Benedicenti, S.; Verniani, G.; Ferrari Cagidiaco, E.; Grandini, S.; Ferrari, M. Sealing ability of a bioceramic sealer used in combination with cold and warm obturation techniques. J. Osseointegr. 2021, 13, 248–255. [Google Scholar]
- Gade, V.J.; Belsare, L.D.; Patil, S.; Bhede, R.; Gade, J.R. Evaluation of push-out bond strength of endosequence BC sealer with lateral condensation and thermoplasticized technique: An in vitro study. J. Conserv. Dent. 2015, 18, 124–127. [Google Scholar]
- Celikten, B.; Uzuntas, C.I.; Orhan, A. Micro-CT assessment of the sealing ability of three root canal filling techniques. J. Oral Sci. 2015, 57, 361–366. [Google Scholar] [CrossRef] [Green Version]
- Camilleri, J. Sealers and warm gutta-percha obturation techniques. J. Endod. 2015, 41, 72–78. [Google Scholar] [CrossRef]
- DeLong, C.; He, J.; Woodmansey, K.F. The effect of obturation technique on the push-out bond strength of calcium silicate sealers. J. Endod. 2015, 41, 385–388. [Google Scholar] [CrossRef]
- Torabinejad, M.; Bahjri, K. Essential elements of evidence-based endodontics: Steps involved in concluding clinical research. J. Endod. 2005, 31, 563–569. [Google Scholar] [CrossRef]
- Berghenholtz, G.; Kvist, T. Evidence-base endodontics. Endod. Top. 2014, 31, 3–18. [Google Scholar] [CrossRef]
- Atmeh, A.R.; Hadis, M.; Camilleri, J. Real-time chemical analysis of root filling materials with heating: Guidelines for safe temperature levels. Int. Endod. J. 2020, 53, 698–708. [Google Scholar] [CrossRef]
- Yamauchi, S.; Watanabe, S.; Okiji, T. Effects of heating on the physical properties of premixed calcium silicate-based root canal sealers. J. Oral Sci. 2020, 63, 65–69. [Google Scholar] [CrossRef]
- Ng, Y.L.; Mann, V.; Rahbaran, S.; Lewsey, J.; Gulabivala, K. Outcome of primary root canal treatment: Systematic review of the literature—Part 2. Influence of clinical factors Int. Endod. J. 2008, 41, 6–31. [Google Scholar]
- Zhang, X.; Pei, X.; Pei, X.; Wan, Q.; Chen, J.; Wang, J. Success and Complication Rates of Root-Filled Teeth Restored with Zirconia Posts: A Critical Review. Int. J. Prosthodont. 2019, 32, 411–419. [Google Scholar] [CrossRef]
- Pontoriero, D.K.I.; Grandini, S.; Spagnuolo, G.; Discepoli, N.; Benedicenti, S.; Maccagnola, V.; Mosca, A.; Ferrari Cagidiaco, E.; Ferrari, M. Clinical outcomes of endodontic treatments and restorations with and without posts up to 18 years. J. Clin. Med. 2021, 10, 908. [Google Scholar] [CrossRef]
- European Society of Endodontology. Quality guidelines for endodontic treatment: Consensus report of the European Society of Endodontology. Int. Endodon. J. 2006, 39, 921–930. [Google Scholar] [CrossRef]
- Kim, J.H.; Cho, S.Y.; Choi, Y.; Kim, D.H.; Shin, S.J.; Jung, I.Y. Clinical efficacy of sealer-based obturation using calcium silicate sealers: A randomized clinical trial. J. Endod. 2022, 48, 144–151. [Google Scholar] [CrossRef]
- Orstavik, D.; Kerekes, K.; Eriksen, H.M. The periapical index: A scoring systems for radiographic assessment of apical periodontitis. Endod. Dent. Traumatol. 1986, 2, 20–34. [Google Scholar] [CrossRef]
- Orstavik, D. Time-course and risk analyses of the development and healing of chronic apical periodontitis in man. Int. Endod. J. 1996, 29, 150–155. [Google Scholar] [CrossRef] [PubMed]
- Chybowski, E.A.; Glickman, G.N.; Patel, Y. Clinical outcome of non-surgical root canal treatment using a single-cone technique with Endosequence bioceramic sealer: A retrospective analysis. J. Endod. 2018, 44, 941–945. [Google Scholar] [CrossRef]
- Manfredini, D.; Tognini, F.; Biondi, K.; Bosco, M. Sample size calculation on temporomandibolar disorders. Minerva Stomatatol. 2003, 52, 309–319. [Google Scholar]
- Graunaite, I.; Skucaite, N.; Lodiene, G.; Agentiene, I.; Machiulskiene, V.J. Effect of Resin-based and Bioceramic Root Canal Sealers on Postoperative Pain: A Split-mouth Randomized Controlled Trial. J. Endod. 2018, 44, 689–693. [Google Scholar] [CrossRef]
- Shim, K.; Jang, Y.E.; Kim, Y. Comparison of the effects of bioceramic and conventional resin-based sealers on postoperative pain after nonsurgical riit canal treatment: A randomized controlled clinical study. Materials 2021, 14, 2661. [Google Scholar] [CrossRef]
- Yu, Y.H.; Kushnir, L.; Kohli, M.; Karabucak, B. Comparing the incidence of postoperative pain after root canal filling warm vertical obturation with resin-based sealerand sealer-based obturation with calcium silicate-based sealer: A prospective clinical trial. Clin. Oral Investig. 2021, 25, 5033–5042. [Google Scholar] [CrossRef]
- Cosar, M.; Demirci, G.K.; Caliskan, M.K. The effect of two different root canal sealers on treatment outcome and post-obturation pain in single-visit root canal treatment: A prospective randomized clinical trial. Int. Endod. J. 2022, 17, 13870. [Google Scholar] [CrossRef]
- Chopra, V.; Davis, G.; Baysan, A. Clinical and radiographic outcome of non-surgical endodontic treatment using calcium silicate-based versus resin-based sealers—A systematic review and meta-analysis of clinical studies. J. Funct. Biomater. 2022, 13, 38. [Google Scholar] [CrossRef]
- Song, M.; Park, M.G.; Kwak, S.W.; Kim, R.H.; Ha, J.H.; Kim, H.C. Pilot evaluation of sealer-based root canal obturation using epoxy-resin-based and calcium-silicate-based sealers: A randomized clinical trial. Materials 2022, 15, 5146. [Google Scholar] [CrossRef]
- Drumond, J.P.S.C.; Maeda, W.; Nascimento, W.M.; Campos, D.; Prado, M.C.; Jesus Soares, A.; Frozoni, M.J. Comparison of Postobturation Pain Experience after Apical Extrusion of Calcium Silicate–and Resin–Based Root Canal Sealers. J. Endod. 2021, 47, 1278–1284. [Google Scholar] [CrossRef]
- Bardini, G.; Casula, L.; Ambu, E.; Musu, D.; Mercadè, M.; Cotti, E. A 12-month follow-up of primary and secondary root canal treatment in teeth obturated with a hydraulic sealer. Clin. Oral Investig. 2021, 15, 2757–2764. [Google Scholar] [CrossRef]
- Ng, Y.L.; Mann, V.; Gulabivala, K. A prospective study of the factors affecting outcomes of nonsurgical root canal treatment: Part 1—Periapical health. Int. Endod. J. 2011, 44, 583–609. [Google Scholar] [CrossRef]
- De Bem, I.A.; de Oliveira, R.A.; Weissheimer, T. Effect of ultrasonic activation of endodontic sealers on intratubular penetration and bond strength to root dentin. J. Endod. 2020, 46, 1302–1308. [Google Scholar] [CrossRef]
- Egemen, A.; Belli, S. The effect of primary root canal treatment on dentinal tubule penetration of calcium silicate-based sealers during endodontic retreatment. J. Endod. 2022, 48, 1169–1177. [Google Scholar] [CrossRef] [PubMed]
- Lee, B.N.; Hong, J.U.; Kim, S.M. Anti-inflammatory and osteogenic effects of calcium silicate-based root canal sealers. J. Endod. 2019, 45, 73–78. [Google Scholar] [CrossRef] [PubMed]
- Friedman, S.; Mor, C. The success of endodontic therapy healing and functionality. J. Calif. Dent. Assoc. 2004, 32, 493–503. [Google Scholar] [CrossRef]
- Bender, I.B.; Seltzer, S.; Soltanoff, W. Endodontic success of a reappraisal of criteria. I. Oral Surg. Oral Med. Oral Pathol. 1966, 22, 780–789. [Google Scholar] [CrossRef] [PubMed]
- Boucher, Y.; Matossian, L.; Rilliard, F.; Machtou, P. Radiographic evaluation of the prevalence and technical quality of root canal treatment in a French subpopulation. Int. Endod. J. 2002, 35, 229–238. [Google Scholar] [CrossRef]
- Estrela, C.; Holland, R.; Rodrigues, C.; Alencar, A.H.G.; Sousa-Neto, M.D.; Pecora, J.D. Characterization of Successful Root Canal Treatment. Braz. Dent. J. 2014, 25, 3–11. [Google Scholar] [CrossRef] [Green Version]
- Ferrari, M.; Ferrari Cagidiaco, E.; Goracci, C.; Sorrentino, R.; Zarone, F.; Grandini, S.; Joda, T. Posterior partial crowns out of lithium disilicate (LS2) with or without posts: A randomized controlled prospective clinical trial with a 3-year follow up. J. Dent. 2019, 83, 12–19. [Google Scholar] [CrossRef]

| Sex (n = 168) | Male 85 (50.6%) | Female 83 (49.4%) | ||
| Age | >50 63 (37.5%) | <50 105 (62.5%) | ||
| Type of Treatment (n = 210) | Initial RCT 98 (46.7%) | ReTx 112 (53.3%) | ||
| Tooth Type (n = 210) | Maxillary Anterior 15 | Maxillary Posterior 110 | Mandibular Anterior 12 | Mandibular Posterior 73 |
| PARL Presence | Present 125 (59.5%) | Absent 85 (40.5%) | ||
| Lesion Size (n = 125) | >5 mm 46 (36.8%) | <5 mm 79 (63.2%) | ||
| Bioceramic Sealers (n = 210) | CeraSeal 115 (54.5%) | BioRoot 35 (16.7%) | AH Plus Bio 40 (19%) | Bio-C SEALER ION 20 (9.5%) |
| Factors/Demography | Healed | Healing | Not Healed | Success | p Value | |
|---|---|---|---|---|---|---|
| Total (n = 210) | 154 (73.3%) | 54 | 2 | 208 | ||
| −25.70% | −0.95% | −99% | ||||
| Age (years) | 0.31 | |||||
| (n = 168) | ||||||
| >50 years | ||||||
| (n = 82) (39%) | 57 (69.5%) | 24 (29.3%) | 1 (1.2%) | 81 (98.8%) | ||
| <50 years | ||||||
| (n = 128) (61%) | 97 (75.8%) | 30 (23.4%) | 1 (0.8%) | 127 (99.2%) | ||
| Treatment type | Not applicable | |||||
| (n = 210) | ||||||
| Initial | ||||||
| (n = 98) (46.7%) | 98 (100%) | 98 (100%) | ||||
| ReTx | ||||||
| (n = 112) (53.3%) | 56 (50%) | 54 (48.2%) | 2 (1.8%) | 110 (98.2%) | ||
| Lesion | Not applicable | |||||
| (n = 210) | ||||||
| Present | ||||||
| (n = 125) (59.5%) | 69 (55.2%) | 54 (43.2%) | 2 (1.6%) | 123 (98.4%) | ||
| Absent | ||||||
| (n = 85) (40.5%) | 85 (100%) | 85 (100%) | ||||
| Lesion Size | <0.01 | |||||
| (n = 125) | ||||||
| >5 mm | ||||||
| (n = 46) (36.8%) | 25 (54.3%) | 19 (41.3%) | 2 (4.4%) | 44 (95.6%) | ||
| <5 mm | ||||||
| (n = 79) (63.2%) | 68 (86%) | 11 (13.9%) | 79 (100%) | |||
| Sealer Extrusion | <0.01 | |||||
| (n = 210) | ||||||
| Present | ||||||
| 85 (40.5%) | 40 (47%) | 43 (50.6%) | 2 (2.4%) | 83 (97.6%) | ||
| Absent | ||||||
| 125 (59.5%) | 114 (91.2%) | 11 (8.8%) | 125 (100%) | |||
| Bioceramic Sealers | <0.01 | |||||
| (n = 210) | ||||||
| CeraSeal | ||||||
| (n = 115) (54.8%) | 96 (83.5%) | 18 (15.6%) | 1 (0.9%) | 114 (99.1%) | ||
| BioRoot | ||||||
| (n = 35) (16.7%) | 17 (48.6%) | 18 (51.4%) | 35 (100%) | |||
| AH Plus Bio | ||||||
| (n = 40) (19%) | 28 (70%) | 11 (27.5%) | 1 (2.5%) | 39 (97.5%) | ||
| BIO-C SEALER ION | ||||||
| (n = 20) (9.5%) | 13 (65%) | 7 (35%) | 20 (100%) |
Disclaimer/Publisher’s Note: The statements, opinions and data contained in all publications are solely those of the individual author(s) and contributor(s) and not of MDPI and/or the editor(s). MDPI and/or the editor(s) disclaim responsibility for any injury to people or property resulting from any ideas, methods, instructions or products referred to in the content. |
© 2023 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Pontoriero, D.I.K.; Ferrari Cagidiaco, E.; Maccagnola, V.; Manfredini, D.; Ferrari, M. Outcomes of Endodontic-Treated Teeth Obturated with Bioceramic Sealers in Combination with Warm Gutta-Percha Obturation Techniques: A Prospective Clinical Study. J. Clin. Med. 2023, 12, 2867. https://doi.org/10.3390/jcm12082867
Pontoriero DIK, Ferrari Cagidiaco E, Maccagnola V, Manfredini D, Ferrari M. Outcomes of Endodontic-Treated Teeth Obturated with Bioceramic Sealers in Combination with Warm Gutta-Percha Obturation Techniques: A Prospective Clinical Study. Journal of Clinical Medicine. 2023; 12(8):2867. https://doi.org/10.3390/jcm12082867
Chicago/Turabian StylePontoriero, Denise Irene Karin, Edoardo Ferrari Cagidiaco, Valerio Maccagnola, Daniele Manfredini, and Marco Ferrari. 2023. "Outcomes of Endodontic-Treated Teeth Obturated with Bioceramic Sealers in Combination with Warm Gutta-Percha Obturation Techniques: A Prospective Clinical Study" Journal of Clinical Medicine 12, no. 8: 2867. https://doi.org/10.3390/jcm12082867
APA StylePontoriero, D. I. K., Ferrari Cagidiaco, E., Maccagnola, V., Manfredini, D., & Ferrari, M. (2023). Outcomes of Endodontic-Treated Teeth Obturated with Bioceramic Sealers in Combination with Warm Gutta-Percha Obturation Techniques: A Prospective Clinical Study. Journal of Clinical Medicine, 12(8), 2867. https://doi.org/10.3390/jcm12082867







