Dental and Maxillofacial Emergency Algorithms in Swiss Emergency Departments
Abstract
1. Introduction
2. Materials and Methods
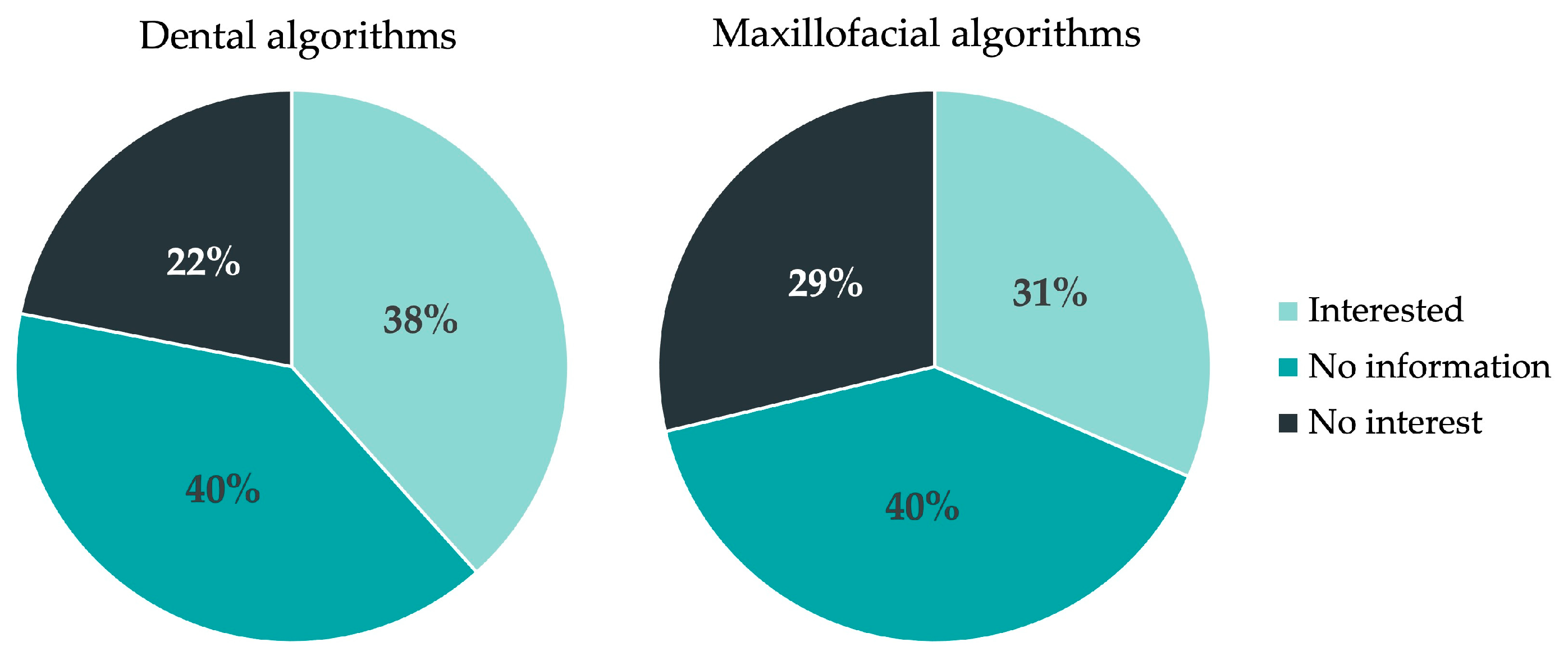
3. Results
4. Discussion
5. Conclusions
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Conflicts of Interest
References
- Koordinationsgruppe für die Statistik der Unfallversicherung UVG (KSUV). Unfallstatistik UVG 2021. Available online: https://www.unfallstatistik.ch/d/publik/publikationen_d.htm (accessed on 30 November 2022).
- Wu, J.; Min, A.; Wang, W.; Su, T. Trends in the incidence, prevalence and years lived with disability of facial fracture at global, regional and national levels from 1990 to 2017. PeerJ 2021, 9, e10693. [Google Scholar] [CrossRef] [PubMed]
- Wusiman, P.; Maimaitituerxun, B.; Saimaiti, A.; Moming, A. Epidemiology and Pattern of Oral and Maxillofacial Trauma. J. Craniofacial Surg. 2020, 31, e517–e520. [Google Scholar] [CrossRef] [PubMed]
- Bertossi, D.; Barone, A.; Iurlaro, A.; Marconcini, S.; De Santis, D.; Finotti, M.; Procacci, P. Odontogenic Orofacial Infections. J. Craniofacial Surg. 2017, 28, 197–202. [Google Scholar] [CrossRef] [PubMed]
- Weise, H.; Naros, A.; Weise, C.; Reinert, S.; Hoefert, S. Severe odontogenic infections with septic progress—A constant and increasing challenge: A retrospective analysis. BMC Oral Health 2019, 19, 1–6. [Google Scholar] [CrossRef] [PubMed]
- Ogle, O.E. Odontogenic Infections. Dent. Clin. 2017, 61, 235–252. [Google Scholar] [CrossRef] [PubMed]
- Igoumenakis, D.; Gkinis, G.; Kostakis, G.; Mezitis, M.; Rallis, G. Severe Odontogenic Infections: Causes of Spread and Their Management. Surg. Infect. 2014, 15, 64–68. [Google Scholar] [CrossRef]
- Rastenienė, R.; Puriene, A.; Aleksejūnienė, J.; Peciuliene, V.; Zaleckas, L. Odontogenic Maxillofacial Infections: A Ten-Year Retrospective Analysis. Surg. Infect. 2015, 16, 305–312. [Google Scholar] [CrossRef]
- Petti, S.; Glendor, U.; Andersson, L. World traumatic dental injury prevalence and incidence, a meta-analysis-One billion living people have had traumatic dental injuries. Dent. Traumatol. 2018, 34, 71–86. [Google Scholar] [CrossRef]
- Lam, R. Epidemiology and outcomes of traumatic dental injuries: A review of the literature. Aust. Dent. J. 2016, 61 (Suppl. S1), 4–20. [Google Scholar] [CrossRef]
- Patel, K.K.; Driscoll, P. Dental knowledge of accident and emergency senior house officers. Emerg. Med. J. 2002, 19, 539–541. [Google Scholar] [CrossRef]
- Tewari, N.; Jonna, I.; Mathur, V.P.; Goel, S.; Ritwik, P.; Rahul, M.; Haldar, P.; Bansal, K.; Pandey, R.M. Global status of knowledge for the prevention and emergency management of traumatic dental injuries among non-dental healthcare professionals: A systematic review and meta-analysis. Injury 2021, 52, 2025–2037. [Google Scholar] [CrossRef]
- Kuspinar, A.; Hirdes, J.P.; Berg, K.; McArthur, C.; Morris, J.N. Development and validation of an algorithm to assess risk of first-time falling among home care clients. BMC Geriatr. 2019, 19, 264. [Google Scholar] [CrossRef] [PubMed]
- Schwalbe, N.; Wahl, B. Artificial intelligence and the future of global health. Lancet 2020, 395, 1579–1586. [Google Scholar] [CrossRef] [PubMed]
- Arbeitsgemeinschaft der Wissenschaftlichen Medizinischen Fachgesellschaften (AWMF)—Ständige Kommission “Leitlinien”. AWMF-Regelwerk “Leitlinien”. Available online: https://www.awmf.org/regelwerk/ (accessed on 14 January 2023).
- MedStandards. Available online: https://medstandards.com/ (accessed on 30 November 2022).
- Looney, G.L.; Roy, A.; Anderson, G.V.; Scharf, R.F. Research algorithms for emergency medicine. Ann. Emerg. Med. 1980, 9, 12–17. [Google Scholar] [CrossRef] [PubMed]
- Furgler, P. Schaufelberger, Mireille Algo-SURF© 2011. Available online: https://www.lesestoff.ch/de/detail/ISBN-9783905699142/Furger-Philippe/Algo-SURF%C2%A9-2011 (accessed on 10 December 2022).
- Harrison, M.; Mohammed, A.; Harrison, M.; Mohammed, A. (Eds.) Algorithms for Emergency Medicine; Oxford University Press: Oxford, UK; New York, NY, USA, 2023; ISBN 978-0-19-882913-3. [Google Scholar]
- Emergency Medicine Kenya Foundation. Emergency Care Algorithms. Available online: https://www.emergencymedicinekenya.org/algorithms/ (accessed on 10 December 2022).
- Bundesamt für Gesundheit (BAG). Kennzahlen Der Schweizer Spitäler 2022. Available online: https://spitalstatistik.bagapps.ch/data/download/kzp20_publication.pdf?v=1647414823 (accessed on 3 December 2022).
- Bundesamt für Statistik (BFS). Statistik Der Stationären Betriebe Des Gesundheitswesens—Krankenhaustypologie. Available online: https://www.bfs.admin.ch/bfs/de/home/statistiken/gesundheit/erhebungen/ks.assetdetail.23546402.html (accessed on 16 January 2023).
- StrawPoll. Available online: https://strawpoll.com/de/create/ (accessed on 4 December 2022).
- Berg, B.-I.; Juergens, P.; Soerensen, Y.; Savic, M.; Zeilhofer, H.-F.; Schwenzer-Zimmerer, K. Traumatology of the facial skeleton in octogenarian patients: A retrospective analysis of 96 cases. J. Cranio Maxillofac. Surg. 2014, 42, 870–873. [Google Scholar] [CrossRef]
- Lieger, O.; Zix, J.; Kruse, A.; Iizuka, T. Dental Injuries in Association with Facial Fractures. J. Oral Maxillofac. Surg. 2009, 67, 1680–1684. [Google Scholar] [CrossRef] [PubMed]
- Erol, B.; Tanrikulu, R.; Görgün, B. Maxillofacial Fractures. Analysis of demographic distribution and treatment in 2901patients (25-year experience). J. Cranio Maxillofac. Surg. 2004, 32, 308–313. [Google Scholar] [CrossRef]
- de Barros, T.E.P.; Campolongo, G.D.; Zanluqui, T.; Duarte, D. Facial trauma in the largest city in latin america, são paulo, 15 years after the enactment of the compulsory seat belt law. Clinics 2010, 65, 1043–1047. [Google Scholar] [CrossRef]
- Alvi, A.; Doherty, T.; Lewen, G. Facial Fractures and Concomitant Injuries in Trauma Patients. Laryngoscope 2003, 113, 102–106. [Google Scholar] [CrossRef]
- Cabalag, M.S.; Wasiak, J.; Andrew, N.E.; Tang, J.; Kirby, J.C.; Morgan, D.J. Epidemiology and management of maxillofacial fractures in an Australian trauma centre. J. Plast. Reconstr. Aesthetic Surg. 2014, 67, 183–189. [Google Scholar] [CrossRef]
- Lee, K.H.; Snape, L.; Steenberg, L.J.; Worthington, J. Comparison between interpersonal violence and motor vehicle accidents in the aetiology of maxillofacial fractures. ANZ J. Surg. 2007, 77, 695–698. [Google Scholar] [CrossRef] [PubMed]
- Bamjee, Y.; Lownie, J.; Cleaton-Jones, P.; Lownie, M. Maxillofacial injuries in a group of South Africans under 18 years of age. Br. J. Oral Maxillofac. Surg. 1996, 34, 298–302. [Google Scholar] [CrossRef]
- Pohl, Y.; Tekin, U.; Boll, M.; Filippi, A.; Kirschner, H. Investigations on a cell culture medium for storage and transportation of avulsed teeth. Aust. Endod. J. 1999, 25, 70–75. [Google Scholar] [CrossRef]
- Krastl, G.; Filippi, A.; Weiger, R. Initial management of dental trauma: Musts, shoulds, and cans. Quintessence Int. 2020, 51, 763–774. [Google Scholar] [CrossRef] [PubMed]
- Filippi, A. Verhalten Am Unfallort Nach Zahntrauma. Quintessenz 2009, 60, 541–545. [Google Scholar]
- Zeissler-Lajtman, A.; Connert, T.; Kühl, S.; Filippi, A. Cling film as storage medium for avulsed teeth. An in vitro pilot study. Swiss Dent. J. 2017, 127, 954–959. [Google Scholar]
- Kahler, B.; Hu, J.-Y.; Marriot-Smith, C.S.; Heithersay, G.S. Splinting of teeth following trauma: A review and a new splinting recommendation. Aust. Dent. J. 2016, 61 (Suppl. S1), 59–73. [Google Scholar] [CrossRef]
- National Council on Radiation. Measurements. Scientific Committee 46-3 on ALARA for Occupationally-Exposed Individuals in Clinical Radiology. Scientific Committee 46 on Operational Radiation Safety Implementation of the Principle of as Low as Reasonably Achievable (ALARA) for Medical and Dental Personnel: Recommendations of the National Council on Radiation Protection and Measurements; National Council on Radiation: Bethesda, MD, USA, 1990; ISBN 0-929600-15-0. [Google Scholar]
- Costa-Tort, J.; Flaviano, V.S.-D.; González-Navarro, B.; Jané-Salas, E.; Estrugo-Devesa, A.; López-López, J. Update on the management of anticoagulated and antiaggregated patients in dental practice: Literature review. J. Clin. Exp. Dent. 2021, 13, e948–e956. [Google Scholar] [CrossRef]
- Hickey, M.; McIntyre, L.; Taljaard, M.; Abdulaziz, K.; Yadav, K.; Hickey, C.; Perry, J.J. Effect of prenotification on the response rate of a postal survey of emergency physicians: A randomised, controlled, assessor-blind trial. BMJ Open 2021, 11, e052843. [Google Scholar] [CrossRef]
- VanGeest, J.B.; Johnson, T.; Welch, V.L. Methodologies for Improving Response Rates in Surveys of Physicians: A Systematic Review. Evaluation Health Prof. 2007, 30, 303–321. [Google Scholar] [CrossRef]
- Reinisch, J.F.; Yu, D.C.; Li, W.-Y. Getting a Valid Survey Response from 662 Plastic Surgeons in the 21st Century. Ann. Plast. Surg. 2016, 76, 3–5. [Google Scholar] [CrossRef]
- Feveile, H.; Olsen, O.; Hogh, A. A randomized trial of mailed questionnaires versus telephone interviews: Response patterns in a survey. BMC Med. Res. Methodol. 2007, 7, 27. [Google Scholar] [CrossRef] [PubMed]
- Shih, T.-H.; Fan, X. Comparing Response Rates from Web and Mail Surveys: A Meta-Analysis. Field Methods 2008, 20, 249–271. [Google Scholar] [CrossRef]
- Gaucher, N.; Trottier, E.D.; Côté, A.-J.; Ali, H.; Lavoie, B.; Bourque, C.-J.; Ali, S.; Pediatric Emergency Research Canada. A survey of Canadian emergency physicians’ experiences and perspectives during the COVID-19 pandemic. Can. J. Emerg. Med. 2021, 23, 466–474. [Google Scholar] [CrossRef] [PubMed]
- Stuck, A.; Crowley, C.; Casale, M.; Castillo, E. 223 National Survey of Emergency Physicians Concerning Home-Based Care Options as Alternatives to Emergency Department-Based Hospital Admissions. Ann. Emerg. Med. 2016, 68, S87. [Google Scholar] [CrossRef]
- Chary, A.N.; Lesser, A.; Inouye, S.K.; Carpenter, C.R.; Stuck, A.R.; Kennedy, M. A Survey of Delirium Self-Reported Knowledge and Practices among Emergency Physicians in the United States. J. Geriatr. Emerg. Med. 2021, 2, 5. [Google Scholar] [CrossRef]
- Plantz, S.H.; Kreplick, L.W.; Panacek, E.A.; Mehta, T.; Adler, J.; McNamara, R.M. A national survey of board-certified emergency physicians: Quality of care and practice structure issues. Am. J. Emerg. Med. 1998, 16, 1–4. [Google Scholar] [CrossRef] [PubMed]
- Perry, J.J.; Losier, J.H.; Stiell, I.G.; Sharma, M.; Abdulaziz, K. National survey of emergency physicians for transient ischemic attack (TIA) risk stratification consensus and appropriate treatment for a given level of risk. Can. J. Emerg. Med. 2015, 18, 10–18. [Google Scholar] [CrossRef]
- Fehlbaum, B.; Waiblinger, E.; Turner, C.D. A comparison of attitudes towards animals between the German- and French-speaking part of Switzerland. Schweiz. Arch. Für Tierheilkd. 2010, 152, 285–293. [Google Scholar] [CrossRef]
- Fischer, S.; Bosshard, G.; Faisst, K.; Tschopp, A.; Fischer, J.; Bär, W.; Gutzwiller, F. Swiss doctors’ attitudes towards end-of-life decisions and their determinants: A comparison of three language regions. Swiss Med. Wkly. 2006, 136, 370–376. [Google Scholar] [CrossRef] [PubMed]
- Glaus, A.; Fäh, B.; Hornung, R.; Senn, H.; Stiefel, F. Breast cancer prevention behaviour: A perspective of women from three language regions of Switzerland. Pflege 2004, 17, 385–394. [Google Scholar] [CrossRef] [PubMed]
- AO CMF. AO Surgery Reference. Available online: https://surgeryreference.aofoundation.org/cmf/trauma (accessed on 21 February 2023).
- Spital Emmental. Rettungsdienstliche Algorithmen. Available online: https://www.spital-emmental.ch/upload/docs/extranetdokumente/RD-Algorithmen%20RSE%202013.pdf (accessed on 17 January 2023).
- Centre Hospitalier Universitaire Vaudois (CHUV). Guidelines Trauma. Available online: https://www.chuv.ch/fr/chirurgie-viscerale/chv-home/professionnels-de-la-sante/filiere-trauma/guidelines-trauma-chuv (accessed on 14 January 2023).
- Chattha, A.; Lee, J.C.; Johnson, P.K.; Patel, A. An Algorithmic Approach to the Management of Ballistic Facial Trauma in the Civilian Population. J. Craniofacial Surg. 2018, 29, 2010–2016. [Google Scholar] [CrossRef] [PubMed]
- Ellis, E. An Algorithm for the Treatment of Noncondylar Mandibular Fractures. J. Oral Maxillofac. Surg. 2013, 72, 939–949. [Google Scholar] [CrossRef] [PubMed]
- Peterson, E.C.B.; Nguyen, D.C.; Baughman, E.J.M.; Skolnick, G.B.B.; Chi, J.J.M.; Patel, K.B.M. Algorithm for Management of Mandibular Condylar Base Fractures. Plast. Reconstr. Surg. Glob. Open 2020, 8, e3145. [Google Scholar] [CrossRef] [PubMed]
- Xu, X.; Zhu, F.; Wang, F.; Liao, Q.; Zhang, W.; Xu, B.; Shu, J. A New Treatment-Oriented Classification and Treatment Algorithm for Comminuted Mandibular Fractures. Available online: https://www.researchsquare.com/article/rs-275587/v1 (accessed on 18 January 2023).
- Zadik, Y. Algorithm of first-aid management of dental trauma for medics and corpsmen. Dent. Traumatol. 2008, 24, 698–701. [Google Scholar] [CrossRef]
- Baxter, M.; Crouch, R.; Bowyer, E. Adult Major Trauma Guidelines—University Hospital Southampton NHS Foundation Trust. Available online: https://www.uhs.nhs.uk/Media/SUHTExtranet/WessexTraumaNetwork/UHS-adult-major-trauma-guidelines.pdf (accessed on 18 January 2023).
- The Recommended Guidelines of the American Association of Endodontists for The Treatment of Traumatic Dental Injuries. Available online: https://www.aae.org/specialty/wp-content/uploads/sites/2/2019/02/19_TraumaGuidelines.pdf (accessed on 18 January 2023).
- Northern Region Trauma Network. Management of Severe Haemorrhage from Midface Trauma. Available online: https://www.northerntrauma.co.nz/adult_trauma/management-of-severe-haemorrhage-from-midface-trauma/ (accessed on 18 January 2023).
- Brighton and Sussex University Hospitals. Paediatric Clinical Practice Guideline. Available online: https://www.bsuh.nhs.uk/library/wp-content/uploads/sites/8/2020/09/Paediatric-Guidelines-Jaw-fractures-and-dislocations.pdf (accessed on 18 January 2023).
- Facial Fracture Management Handbook—Mandible Fractures|Iowa Head and Neck Protocols. Available online: https://medicine.uiowa.edu/iowaprotocols/facial-fracture-management-handbook-mandible-fractures (accessed on 18 January 2023).
- Initial Evaluation and Management of Facial Trauma in Adult © 2023 UpToDate. Available online: https://www.uptodate.com/contents/initial-evaluation-and-management-of-facial-trauma-in-adults (accessed on 18 January 2023).
- Vanderbilt University Medical Center. VUMC Facial Trauma Practice Management Guidelines. Available online: https://www.vumc.org/trauma-and-scc/sites/default/files/public_files/Protocols/Facial%20Trauma%20PMG.pdf (accessed on 18 January 2023).
- The Royal Children’s Hospital Melbourne. The Paediatric Trauma Manual—Maxillofacial Injury. Available online: https://www.rch.org.au/trauma-service/manual/maxillofacial-injury/ (accessed on 18 January 2023).



| Questions and Corresponding Answer Possibilities | |
|---|---|
| Are electronic algorithms/protocols, such as “medStandards”, available in your ED? | |
| No Yes | Is there any demand for algorithms? |
| Do you have algorithms/protocols regarding maxillofacial surgery in your clinic? | |
| Yes No | Own protocols ready for distribution? Is there a demand for maxillofacial algorithms? |
| Do you have dental algorithms/protocols in your clinic? | |
| Yes No | Could you send them to us? Would there be a demand for such algorithms? |
| Do you have own algorithms/protocols, or a commercially available product? | |
| Own/in-house algorithms/protocols Commercially available algorithms/protocols | Which brand? |
| How often do you use such algorithms/protocols in general? | |
| Daily Several times a week Monthly Less than monthly | |
Disclaimer/Publisher’s Note: The statements, opinions and data contained in all publications are solely those of the individual author(s) and contributor(s) and not of MDPI and/or the editor(s). MDPI and/or the editor(s) disclaim responsibility for any injury to people or property resulting from any ideas, methods, instructions or products referred to in the content. |
© 2023 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Sommacal, A.; Bingisser, R.; Filippi, A.; Bethke, M.; Thieringer, F.M.; Jaquiéry, C.; Berg, B.-I. Dental and Maxillofacial Emergency Algorithms in Swiss Emergency Departments. J. Clin. Med. 2023, 12, 2952. https://doi.org/10.3390/jcm12082952
Sommacal A, Bingisser R, Filippi A, Bethke M, Thieringer FM, Jaquiéry C, Berg B-I. Dental and Maxillofacial Emergency Algorithms in Swiss Emergency Departments. Journal of Clinical Medicine. 2023; 12(8):2952. https://doi.org/10.3390/jcm12082952
Chicago/Turabian StyleSommacal, Adelita, Roland Bingisser, Andreas Filippi, Mascha Bethke, Florian M. Thieringer, Claude Jaquiéry, and Britt-Isabelle Berg. 2023. "Dental and Maxillofacial Emergency Algorithms in Swiss Emergency Departments" Journal of Clinical Medicine 12, no. 8: 2952. https://doi.org/10.3390/jcm12082952
APA StyleSommacal, A., Bingisser, R., Filippi, A., Bethke, M., Thieringer, F. M., Jaquiéry, C., & Berg, B.-I. (2023). Dental and Maxillofacial Emergency Algorithms in Swiss Emergency Departments. Journal of Clinical Medicine, 12(8), 2952. https://doi.org/10.3390/jcm12082952









