The Efficacy of Microfracture Combined with Extracorporeal Shock Wave Therapy for Treating Osteochondral Lesion of the Talus and the Quality of Regenerated Cartilage: A Retrospective Cohort Study and MRI Assessment
Abstract
:1. Introduction
2. Methods
2.1. Subjects
2.2. General Characteristics
2.3. Arthroscopic MF Operation
2.4. PRP Injection
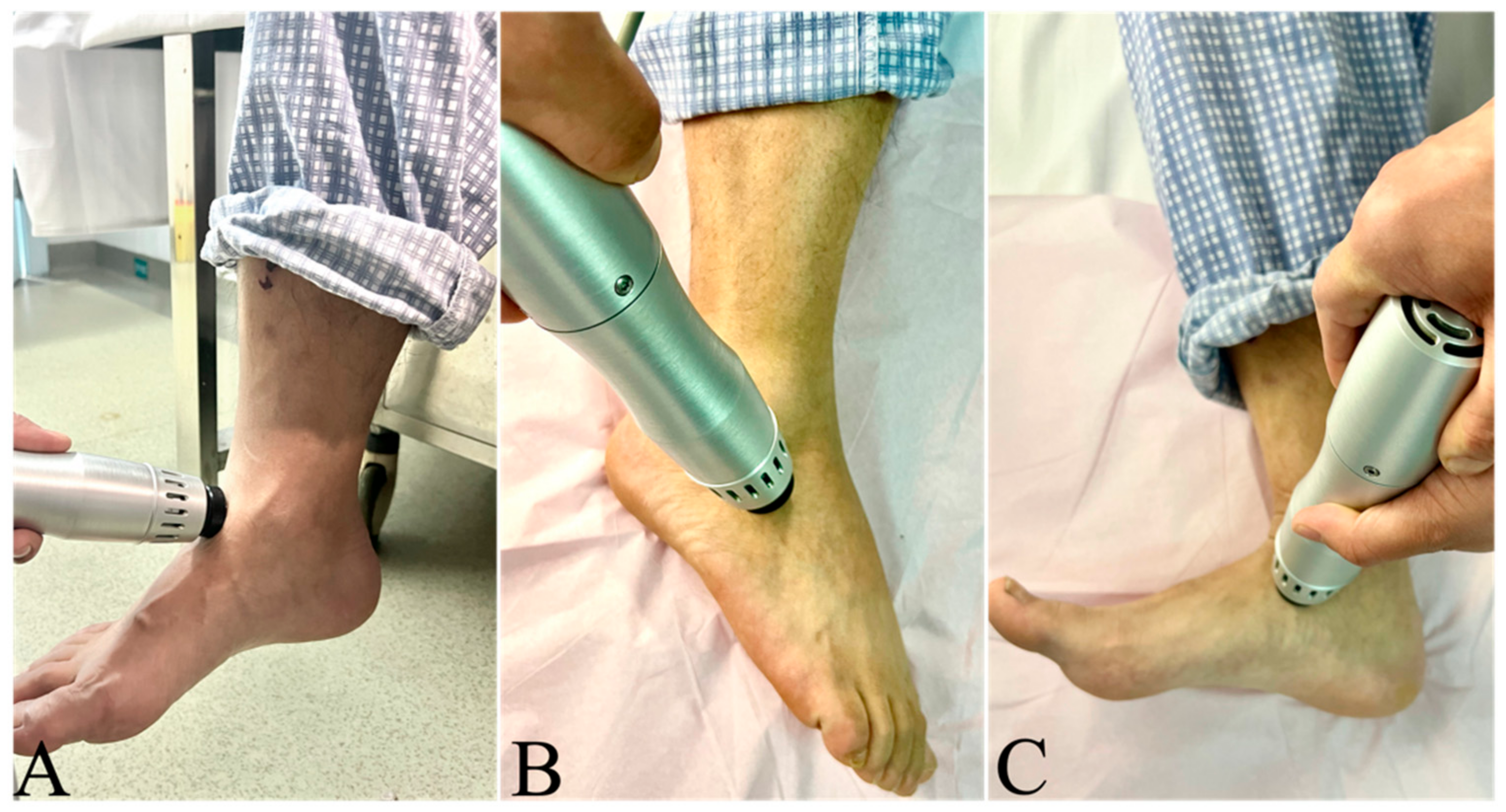
2.5. ESWT
2.6. Subjective Assessments
2.7. Successful Rate of the Treatments
2.8. MRI T2 Mapping for the Outcomes of Cartilage Repair
2.9. Statistical Analysis
3. Results
3.1. Comparisons of the Efficacy
3.2. MRI T2 Mapping for the Cartilage Repair
3.3. Multiple Linear-Regression Analysis
4. Discussion
5. Conclusions
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Conflicts of Interest
References
- van Dijk, C.N.; Reilingh, M.L.; Zengerink, M.; van Bergen, C.J. Osteochondral defects in the ankle: Why painful? Knee Surg Sport. Traumatol. Arthrosc. 2010, 18, 570–580. [Google Scholar] [CrossRef] [PubMed]
- Polat, G.; Erşen, A.; Erdil, M.E.; Kızılkurt, T.; Kılıçoğlu, Ö.; Aşık, M. Long-term results of microfracture in the treatment of talus osteochondral lesions. Knee Surg. Sport. Traumatol. Arthrosc. 2016, 24, 1299–1303. [Google Scholar] [CrossRef] [PubMed]
- Hepple, S.; Winson, I.G.; Glew, D. Osteochondral lesions of the talus: A revised classification. Foot Ankle Int. 1999, 20, 789–793. [Google Scholar] [CrossRef] [PubMed]
- Zhang, C.; Huang, H.; Yang, L.; Duan, X. Extracorporeal Shock Wave Therapy for Pain Relief After Arthroscopic Treatment of Osteochondral Lesions of Talus. J. Foot Ankle Surg. 2020, 59, 190–194. [Google Scholar] [CrossRef] [PubMed]
- Yausep, O.E.; Madhi, I.; Trigkilidas, D. Platelet rich plasma for treatment of osteochondral lesions of the talus: A systematic review of clinical trials. J. Orthop. 2020, 18, 218–225. [Google Scholar] [CrossRef]
- Becher, C.; Driessen, A.; Hess, T.; Longo, U.G.; Maffulli, N.; Thermann, H. Microfracture for chondral defects of the talus: Maintenance of early results at midterm follow-up. Knee Surg Sport. Traumatol. Arthrosc. 2010, 18, 656–663. [Google Scholar] [CrossRef]
- Boffa, A.; Previtali, D.; Altamura, S.A.; Zaffagnini, S.; Candrian, C.; Filardo, G. Platelet-Rich Plasma Augmentation to Microfracture Provides a Limited Benefit for the Treatment of Cartilage Lesions: A Meta-analysis. Orthop. J. Sport. Med. 2020, 8, 2325967120910504. [Google Scholar] [CrossRef]
- Xu, Y.; Wu, K.; Liu, Y.; Geng, H.; Zhang, H.; Liu, S.; Qu, H.; Xing, G. The effect of extracorporeal shock wave therapy on the treatment of moderate to severe knee osteoarthritis and cartilage lesion. Medicine 2019, 98, e15523. [Google Scholar] [CrossRef]
- Kang, S.; Gao, F.; Han, J.; Mao, T.; Li, Z. Extracorporeal shock wave treatment can normalize painful bone marrow edema in knee osteoarthritis: A comparative historical cohort study. Medicine 2018, 97, e9796. [Google Scholar] [CrossRef]
- Shi, L.; Yang, X.; Wang, P.; Ma, X.; Li, D.; Wu, X.; Gao, F.; Sun, W. Quantitative Magnetic Resonance Imaging of Femoral Head Articular Cartilage Change in Patients with Hip Osteonecrosis Treated with Extracorporeal Shock Wave Therapy. Int. J. Clin. Pract. 2022, 2022, 8609868. [Google Scholar] [CrossRef]
- Ma, H.Z.; Zeng, B.F.; Li, X.L. Upregulation of VEGF in subchondral bone of necrotic femoral heads in rabbits with use of extracorporeal shock waves. Calcif. Tissue Int. 2007, 81, 124–131. [Google Scholar] [CrossRef]
- Looze, C.A.; Capo, J.; Ryan, M.K.; Begly, J.P.; Chapman, C.; Swanson, D.; Singh, B.C.; Strauss, E. Evaluation and Management of Osteochondral Lesions of the Talus. Cartilage 2017, 8, 19–30. [Google Scholar] [CrossRef]
- Choi, W.J.; Park, K.K.; Kim, B.S.; Lee, J.W. Osteochondral Lesion of the Talus: Is There a Critical Defect Size for Poor Outcome? Am. J. Sport. Med. 2009, 37, 1974–1980. [Google Scholar] [CrossRef]
- Lee, K.B.; Bai, L.B.; Chung, J.Y.; Seon, J.K. Arthroscopic microfracture for osteochondral lesions of the talus. Knee Surg Sport. Traumatol. Arthrosc. 2010, 18, 247–253. [Google Scholar] [CrossRef]
- Chuckpaiwong, B.; Berkson, E.M.; Theodore, G.H. Microfracture for Osteochondral Lesions of the Ankle: Outcome Analysis and Outcome Predictors of 105 Cases. Arthroscopy 2008, 24, 106–112. [Google Scholar] [CrossRef]
- Ding, Y.; Liu, B.; Qiao, H.; Yin, L.; He, W.; Si, F.; Wang, D. Can knee flexion contracture affect cervical alignment and neck tension? A prospective self-controlled pilot study. Spine J. Off. J. North Am. Spine Soc. 2020, 20, 251–260. [Google Scholar] [CrossRef]
- Steadman, J.R.; Rodkey, W.G.; Rodrigo, J.J. Microfracture: Surgical technique and rehabilitation to treat chondral defects. Clin. Orthop. Relat. Res. 2001, 391, S362–S369. [Google Scholar] [CrossRef]
- Guney, A.; Yurdakul, E.; Karaman, I.; Bilal, O.; Kafadar, I.H.; Oner, M. Medium-term outcomes of mosaicplasty versus arthroscopic microfracture with or without platelet-rich plasma in the treatment of osteochondral lesions of the talus. Knee Surg. Sport. Traumatol. Arthrosc. Off. J. ESSKA 2016, 24, 1293–1298. [Google Scholar] [CrossRef]
- Varenika, V.; Harter, J.; Chu, E.; Steinbach, L. The posterolateral approach for fluoroscopy-guided tibiotalar joint injection. Skelet. Radiol. 2017, 46, 1–3. [Google Scholar] [CrossRef]
- Gao, F.; Chen, N.; Sun, W.; Wang, B.; Shi, Z.; Cheng, L.; Li, Z.; Guo, W. Combined Therapy with Shock Wave and Retrograde Bone Marrow-Derived Cell Transplantation for Osteochondral Lesions of the Talus. Sci. Rep. 2017, 7, 2106. [Google Scholar] [CrossRef]
- Kitaoka, H.B.; Alexander, I.J.; Adelaar, R.S.; Nunley, J.A.; Myerson, M.S.; Sanders, M.; Lutter, L.D. Clinical Rating Systems for the Ankle-Hindfoot, Midfoot, Hallux, and Lesser Toes. Foot Ankle Int. 1997, 18, 187–188. [Google Scholar] [CrossRef] [PubMed]
- Nieminen, M.T.; Rieppo, J.; Silvennoinen, J.; Helminen, H.J.; Jurvelin, J.S. Quantitative MR microscopy of enzymatically degraded articular cartilage. Magn. Reson. Med. 2000, 43, 676–681. [Google Scholar] [CrossRef]
- Gianakos, A.L.; Yasui, Y.; Hannon, C.P.; Kennedy, J.G. Current management of talar osteochondral lesions. World J. Orthop. 2017, 8, 12–20. [Google Scholar] [CrossRef] [PubMed]
- Shimozono, Y.; Yasui, Y.; Ross, A.W.; Kennedy, J.G. Osteochondral lesions of the talus in the athlete: Up to date review. Curr. Rev. Musculoskelet. Med. 2017, 10, 131–140. [Google Scholar] [CrossRef] [PubMed]
- Eslamian, F.; Shakouri, S.K.; Jahanjoo, F.; Hajialiloo, M.; Notghi, F. Extra Corporeal Shock Wave Therapy Versus Local Corticosteroid Injection in the Treatment of Chronic Plantar Fasciitis, a Single Blinded Randomized Clinical Trial. Pain Med. 2016, 17, 1722–1731. [Google Scholar] [CrossRef]
- Assirelli, E.; Filardo, G.; Mariani, E.; Kon, E.; Roffi, A.; Vaccaro, F.; Marcacci, M.; Facchini, A.; Pulsatelli, L. Effect of two different preparations of platelet-rich plasma on synoviocytes. Knee Surg. Sport. Traumatol. Arthrosc. Off. J. ESSKA 2015, 23, 2690–2703. [Google Scholar] [CrossRef]
- Nurden, A.T. Platelets, inflammation and tissue regeneration. Thromb. Haemost. 2011, 105, S13–S33. [Google Scholar] [CrossRef]
- Bendinelli, P.; Matteucci, E.; Dogliotti, G.; Corsi, M.M.; Banfi, G.; Maroni, P.; Desiderio, M.A. Molecular basis of anti-inflammatory action of platelet-rich plasma on human chondrocytes: Mechanisms of NF-κB inhibition via HGF. J. Cell. Physiol. 2010, 225, 757–766. [Google Scholar] [CrossRef]
- Khatab, S.; van Buul, G.M.; Kops, N.; Bastiaansen-Jenniskens, Y.M.; Bos, P.K.; Verhaar, J.A.; van Osch, G.J. Intra-articular Injections of Platelet-Rich Plasma Releasate Reduce Pain and Synovial Inflammation in a Mouse Model of Osteoarthritis. Am. J. Sport. Med. 2018, 46, 977–986. [Google Scholar] [CrossRef]
- Badekas, T.; Takvorian, M.; Souras, N. Treatment principles for osteochondral lesions in foot and ankle. Int. Orthop. 2013, 37, 1697–1706. [Google Scholar] [CrossRef]
- Li, S.; Wang, K.; Sun, H.; Luo, X.; Wang, P.; Fang, S.; Chen, H.; Sun, X. Clinical effects of extracorporeal shock-wave therapy and ultrasound-guided local corticosteroid injections for plantar fasciitis in adults: A meta-analysis of randomized controlled trials. Medicine 2018, 97, e13687. [Google Scholar] [CrossRef]
- Maier, C.F.; Tan, S.G.; Hariharan, H.; Potter, H.G. T2 quantitation of articular cartilage at 1.5 T. J. Magn. Reson. Imaging JMRI 2003, 17, 358–364. [Google Scholar] [CrossRef]
- Blumenkrantz, G.; Majumdar, S. Quantitative magnetic resonance imaging of articular. Eur. Cells Mater. 2007, 13, 76–86. [Google Scholar] [CrossRef]
- Wang, C.-J.; Huang, K.-E.; Sun, Y.-C.; Yang, Y.-J.; Ko, J.-Y.; Weng, L.-H.; Wang, F.-S. VEGF Modulates Angiogenesis and Osteogenesis in Shockwave-Promoted Fracture Healing in Rabbits. J. Surg. Res. 2011, 171, 114–119. [Google Scholar] [CrossRef]

| Characteristics | MF + PRP (n = 33) | MF + ESWT (n = 43) | p Value |
|---|---|---|---|
| Age (year) | 33.9 ± 6.8 | 34.4 ± 7.5 | t = −0.337 p = 0.737 |
| Sex (n) | male 26 female 7 | male 32 female 11 | χ2 = 0.197 p =0.657 |
| BMI | 25.99 ± 2.74 | 24.86 ± 2.89 | t = 1.742 p = 0.086 |
| Disease history (month) | 4.2 ± 3.2 | 5.0 ± 5.0 | t = −0.778 p = 0.439 |
| ICRS grade (n) | grade 3 15 grade 4 18 | grade 3 24 grade 4 19 | χ2 = 0.802 p = 0.370 |
| OLT area (mm2) | 135.61 ± 5.62 | 136.54 ± 5.51 | t = −0.721 p = 0.473 |
| Follow up (month) | 28.9 ± 5.7 | 27.4 ± 3.0 | t = 1.447 p = 0.155 |
| Complications (n) | no 29 synovitis 1 ankle pain 3 | no 31 synovitis 2 ankle pain 3 edema 7 | χ2 = 2.799 p = 0.094 |
| Efficacy Parameter | MF + PRP (n = 33) | MF + ESWT (n = 43) | p Value |
|---|---|---|---|
| Baseline daily activity VAS | 4.1 ± 0.2 | 4.0 ± 0.6 | t = 0.790 p = 0.433 |
| Daily activity VAS | 1.2 ± 0.4 | 1.3 ± 0.4 | t = −0.439 p = 0.662 |
| Baseline exercise VAS | 6.4 ± 0.8 | 6.5 ± 0.6 | t = −0.391 p = 0.697 |
| Exercise VAS | 2.4 ± 0.6 | 2.8 ± 0.4 | t = −2.634 p = 0.011 * |
| Baseline AOFAS | 65.8 ± 8.0 | 63.7 ± 14.8 | t = 0.731 p = 0.467 |
| AOFAS | 94.0 ± 5.3 | 96.7 ± 4.2 | t = −2.371 p = 0.021 * |
| Successful rate (n) | Success 14 Unsuccess 19 | Success 26 Unsuccess 17 | χ2 = 2.438 p = 0.184 |
| T2 Mapping Value | MF + PRP (n = 33) | MF + ESWT (n = 43) | p Value |
|---|---|---|---|
| Baseline | 39.73 ± 3.26 | 39.81 ± 3.67 | t = −0.107 p = 0.915 |
| Follow up | 23.29 ± 4.43 | 16.53 ± 2.90 | t = 8.025 p < 0.001 ** |
| Parameters | B | SEM | p-Value | VIF |
|---|---|---|---|---|
| Treatment | −6.951 | 0.547 | 0.000 ** | 1.052 |
| Age | 0.393 | 0.037 | 0.000 ** | 1.530 |
| Sex | 0.424 | 0.756 | 0.577 | 1.155 |
| BMI | 0.114 | 0.098 | 0.252 | 1.142 |
| Disease history | 0.060 | 0.065 | 0.359 | 1.132 |
| ICRS grade | 0.391 | 0.553 | 0.481 | 1.538 |
| OLT area | 0.085 | 0.059 | 0.152 | 1.052 |
Disclaimer/Publisher’s Note: The statements, opinions and data contained in all publications are solely those of the individual author(s) and contributor(s) and not of MDPI and/or the editor(s). MDPI and/or the editor(s) disclaim responsibility for any injury to people or property resulting from any ideas, methods, instructions or products referred to in the content. |
© 2023 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Li, J.; Ma, Q.; Hou, J.; Liu, Y.; Lu, P.; Liu, P.; Zhang, Z.; Xing, G. The Efficacy of Microfracture Combined with Extracorporeal Shock Wave Therapy for Treating Osteochondral Lesion of the Talus and the Quality of Regenerated Cartilage: A Retrospective Cohort Study and MRI Assessment. J. Clin. Med. 2023, 12, 2966. https://doi.org/10.3390/jcm12082966
Li J, Ma Q, Hou J, Liu Y, Lu P, Liu P, Zhang Z, Xing G. The Efficacy of Microfracture Combined with Extracorporeal Shock Wave Therapy for Treating Osteochondral Lesion of the Talus and the Quality of Regenerated Cartilage: A Retrospective Cohort Study and MRI Assessment. Journal of Clinical Medicine. 2023; 12(8):2966. https://doi.org/10.3390/jcm12082966
Chicago/Turabian StyleLi, Jian, Qiaozhi Ma, Jianlei Hou, Yufen Liu, Pengfei Lu, Pengwei Liu, Zhongwen Zhang, and Gengyan Xing. 2023. "The Efficacy of Microfracture Combined with Extracorporeal Shock Wave Therapy for Treating Osteochondral Lesion of the Talus and the Quality of Regenerated Cartilage: A Retrospective Cohort Study and MRI Assessment" Journal of Clinical Medicine 12, no. 8: 2966. https://doi.org/10.3390/jcm12082966




