Sex-Related Differences in Outpatient Healthcare of Acute Coronary Syndrome: Evidence from an Italian Real-World Investigation
Abstract
:1. Introduction
2. Materials and Methods
2.1. Setting
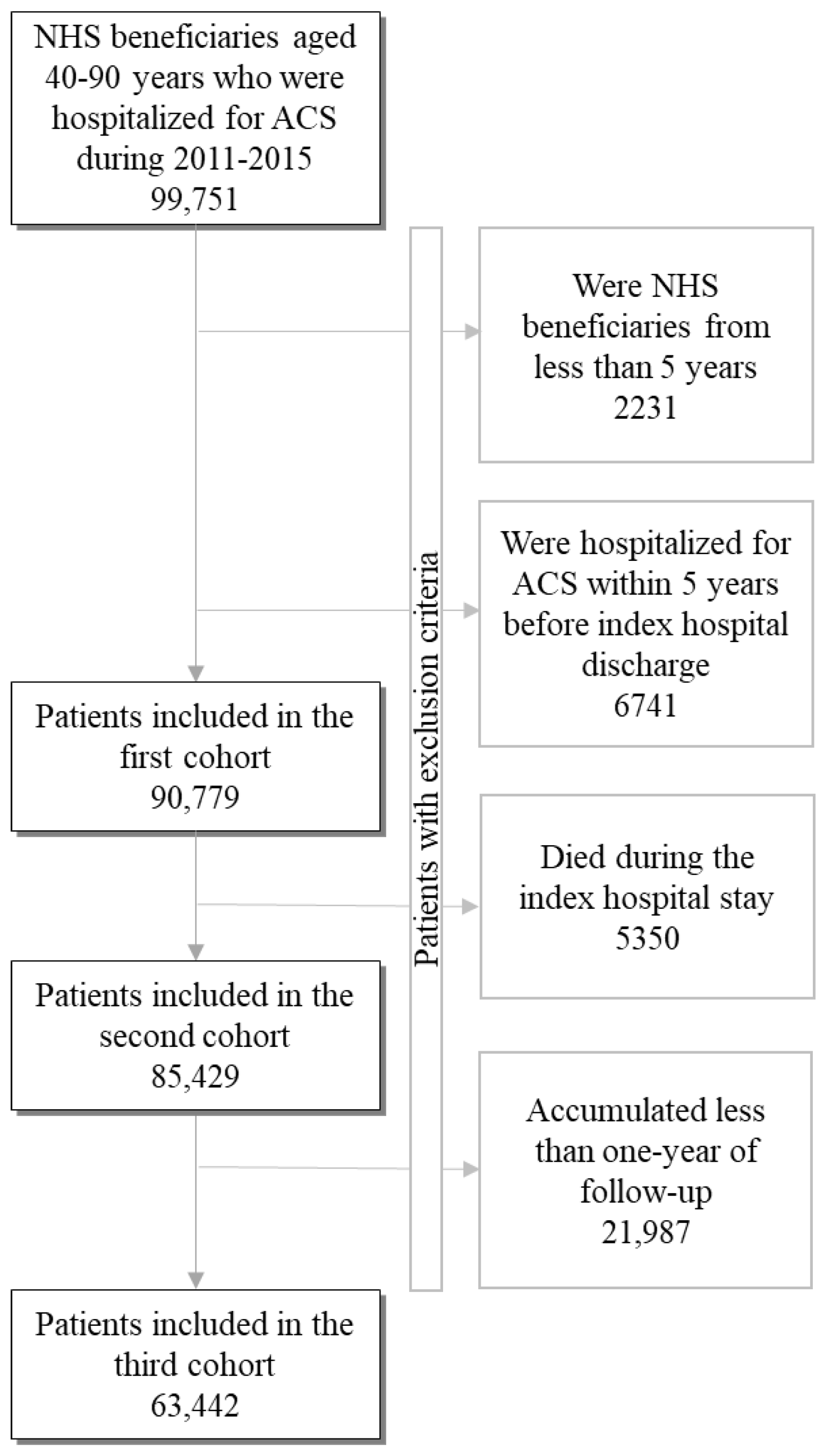
2.2. Cohort Selection
2.3. Cohort Baseline Characteristics
2.4. Clinical Outcomes
2.5. Adherence to Recommendations
2.6. Data Analysis
3. Results
3.1. Patients
3.2. Clinical Outcomes
3.3. Out-Of-Hospital Healthcare
3.4. Sex, Out-Of-Hospital Healthcare and Clinical Outcomes
4. Discussion
5. Conclusions
Supplementary Materials
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Conflicts of Interest
References
- Ferrario, M.M.; Fornari, C.; Bolognesi, L.; Gussoni, M.T.; Benedetti, M.; Sega, R.; Borchini, R.; Cesana, G. Recent time trends of myocardial infarction rates in northern Italy. Results from the MONICA and CAMUNI registries in Brianza: 1993–1994 versus 1997–1998. Ital. Heart J. 2003, 4 (Suppl. 8), 651–657. [Google Scholar]
- Barchielli, A.; Balzi, D.; Pasqua, A.; Buiatti, E. Incidence of acute myocardial infarction in Tuscany, 1997–2002: Data from the Acute Myocardial Infarction Registry of Tuscany (Tosc-AMI). Epidemiol. Prev. 2006, 30, 161–168. [Google Scholar] [PubMed]
- Amsterdam, E.A.; Wenger, N.K.; Brindis, R.G.; Casey, D.E.; Ganiats, T.G.; Holmes, D.R.; Jaffe, A.S.; Jneid, H.; Kelly, R.F.; Kontos, M.C.; et al. AHA/ACC guideline for the management of patients with non-ST-elevation acute coronary syndromes: Executive summary: A report of the American College of Cardiology/American Heart Association Task Force on Practice Guidelines. Circulation 2014, 130, 2354–2394. [Google Scholar] [CrossRef] [PubMed]
- Ibanez, B.; James, S.; Agewall, S.; Antunes, M.; Bucciarelli-Ducci, C.; Bueno, H.; Caforio, A.; Crea, F.; Goudevenos, J.; Halvorsen, S.; et al. ESC Guidelines for the management of acute myocardial infarction in patients presenting with ST-segment elevation: The Task Force for the management of acute myocardial infarction in patients presenting with ST-segment elevation of the European Society of Cardiology (ESC). Eur. Heart J. 2017, 39, 119–177. [Google Scholar]
- Piironen, M.; Ukkola, O.; Huikuri, H.; Havulinna, A.S.; Koukkunen, H.; Mustonen, J.; Ketonen, M.; Lehto, S.; Airaksinen, J.; Kesaeniemi, Y.A.; et al. Trends in long-term prognosis after acute coronary syndrome. Eur. J. Prev. Cardiol. 2017, 24, 274–280. [Google Scholar] [CrossRef]
- Bansilal, S.; Castellano, J.M.; Garrido, E.; Wei, H.G.; Freeman, A.; Spettell, C.; Garcia-Alonso, F.; Lizano, I.; Arnold, R.J.; Rajda, J.; et al. Assessing the impact of medication adherence on long-term cardiovascular outcomes. J. Am. Coll. Cardiol. 2016, 68, 789–801. [Google Scholar] [CrossRef]
- Choudhry, N.K.; Glynn, R.J.; Avorn, J.; Lee, J.L.; Brennan, T.A.; Reisman, L.; Toscano, M.; Levin, R.; Matlin, O.S.; Antman, E.M.; et al. Untangling the relationship between medication adherence and post-myocardial infarction outcomes: Medication adherence and clinical outcomes. Am. Heart J. 2014, 167, 51–58.e5. [Google Scholar] [CrossRef]
- Worrall-Carter, L.; McEvedy, S.; Wilson, A.; Rahman, M.A. Gender Differences in Presentation, Coronary Intervention, and Outcomes of 28,985 Acute Coronary Syndrome Patients in Victoria, Australia. Women’s Health Issues 2016, 26, 14–20. [Google Scholar] [CrossRef]
- Lee, C.Y.; Liu, K.T.; Lu, H.T.; Ali, R.M.; Fong, A.Y.Y.; Ahmad, W.A.W. Sex and gender differences in presentation, treatment and outcomes in acute coronary syndrome, a 10 year study from a multi-ethnic Asian population: The Malaysian National Cardiovascular Disease Database-Acute Coronary Syndrome (NCVD-ACS) registry. PLoS ONE 2021, 16, e0246474. [Google Scholar] [CrossRef]
- Haaf, M.E.T.; Bax, M.; Berg, J.M.T.; Brouwer, J.; Hof, A.W.V.; van der Schaaf, R.J.; Stella, P.R.; Gin, R.M.T.J.; Tonino, P.A.; de Vries, A.G.; et al. Sex differences in characteristics and outcome in acute coronary syndrome patients in the Netherlands. Neth. Heart J. 2019, 27, 263–271. [Google Scholar] [CrossRef]
- Hao, Y.; Liu, J.; Liu, J.; Yang, N.; Smith, S.C.S., Jr.; Huo, Y.; Fonarow, G.C.; Ge, J.; Taubert, K.A.; Morgan, L.; et al. Sex Differences in In-Hospital Management and Outcomes of Patients With Acute Coronary Syndrome. Circulation 2019, 139, 1776–1785. [Google Scholar] [CrossRef] [PubMed]
- Malacrida, R.; Genoni, M.; Maggioni, A.P.; Spataro, V.; Parish, S.; Palmer, A.; Collins, R.; Moccetti, T. A comparison of the early outcome of acute myocardial infarction in women and men. The Third International Study of Infarct Survival Collaborative Group. N. Engl. J. Med. 1998, 388, 8–14. [Google Scholar] [CrossRef] [PubMed]
- Lin, C.F.; Shen, L.J.; Hsiao, F.Y.; Gau, C.S.; Wu, F.L.L. Sex differences in the treatment and outcome of patients with acute coronary syndrome after percutaneous coronary intervention: A population-based study. J. Women’s Health 2014, 23, 238–245. [Google Scholar] [CrossRef] [PubMed]
- Alabas, O.A.; Gale, C.P.; Hall, M.; Rutherford, M.J.; Szummer, K.; Lawesson, S.S.; Alfredsson, J.; Lindahl, B.; Jernberg, T. Sex Differences in Treatments, Relative Survival, and Excess Mortality Following Acute Myocardial Infarction: National Cohort Study Using the SWEDEHEART Registry. J. Am. Heart Assoc. 2017, 6, e007123. [Google Scholar] [CrossRef]
- Hyun, K.; Negrone, A.; Redfern, J.; Atkins, E.; Chow, C.; Kilian, J.; Rajaratnam, R.; Brieger, D. Gender Difference in Secondary Prevention of Cardiovascular Disease and Outcomes Following the Survival of Acute Coronary Syndrome. Heart Lung Circ. 2021, 30, 121–127. [Google Scholar] [CrossRef]
- Trifirò, G.; Gini, R.; Barone-Adesi, F.; Beghi, E.; Cantarutti, A.; Capuano, A.; Carnovale, C.; Clavenna, A.; Dellagiovanna, M.; Ferrajolo, C.; et al. The Role of European Healthcare Databases for Post-Marketing Drug Effectiveness, Safety and Value Evaluation: Where Does Italy Stand? Drug Saf. 2019, 42, 347–363. [Google Scholar] [CrossRef]
- Rea, F.; Ronco, R.; Pedretti, R.F.; Merlino, L.; Corrao, G. Better adherence with out-of-hospital healthcare improved long-term prognosis of acute coronary syndromes: Evidence from an Italian real-world investigation. Int. J. Cardiol. 2020, 318, 14–20. [Google Scholar] [CrossRef]
- Rea, F.; Cantarutti, A.; Merlino, L.; Ungar, A.; Corrao, G.; Mancia, G. Antihypertensive Treatment in Elderly Frail Patients: Evidence From a Large Italian Database. Hypertension 2020, 76, 442–449. [Google Scholar] [CrossRef]
- Corrao, G.; Rea, F.; Di Martino, M.; De Palma, R.; Scondotto, S.; Fusco, D.; Lallo, A.; Belotti, L.M.B.; Ferrante, M.; Addario, S.P.; et al. Developing and validating a novel multisource comorbidity score from administrative data: A large population-based cohort study from Italy. BMJ Open. 2017, 7, e019503. [Google Scholar] [CrossRef]
- Goldberger, J.J.; Bonow, R.O.; Cuffe, M.; Dyer, A.; Rosenberg, Y.; O’Rourke, R.; Shah, P.K.; Smith, S.C.S., Jr.; PACE-MI Investigators. beta-blocker use following myocardial infarction: Low prevalence of evidence-based dosing. Am. Heart J. 2010, 160, 435–442. [Google Scholar] [CrossRef]
- Andrade, S.E.; Kahler, K.H.; Frech, F.; Chan, K.A. Methods for evaluation of medication adherence and persistence using automated databases. Pharmacoepidemiol. Drug Saf. 2006, 15, 565–574. [Google Scholar] [CrossRef] [PubMed]
- Austin, P. Balance diagnostics for comparing the distribution of baseline covariates between treatment groups in propensity-score matched samples. Stat Med. 2009, 28, 3083–3107. [Google Scholar] [CrossRef] [PubMed]
- Austin, P. A comparison of 12 algorithms for matching on the propensity score. Stat. Med. 2014, 33, 1057–1069. [Google Scholar] [CrossRef]
- Fine, J.; Gray, R.J. A Proportional hazards model for the subdistribution of a competing risk. J. Am. Stat. Ass. 1999, 94, 496–509. [Google Scholar] [CrossRef]
- Buckley, J.P.; Doherty, B.T.; Keil, A.P.; Engel, S.M. Statistical Approaches for Estimating Sex-Specific Effects in Endocrine Disruptors Research. Environ. Health Perspect. 2017, 125, 067013. [Google Scholar] [CrossRef]
- Higgins, J.; Thompson, S.; Deeks, J.; Altman, D. Measuring inconsistency in meta-analyses. BMJ 2003, 327, 557–560. [Google Scholar] [CrossRef]
- Kawamoto, K.; Davis, M.; Duvernoy, C. Acute Coronary Syndromes: Differences in Men and Women. Curr. Atheroscler. Rep. 2016, 18, 73. [Google Scholar] [CrossRef]
- Programma Nazionale Esiti, Report 2021; Ministero della Salute, 2021. Available online: https://pne.agenas.it/main/doc/Report_PNE_2021.pdf (accessed on 17 April 2023).
- Mallidi, J.; Lata, K. Role of Gender in Dual Antiplatelet Therapy After Acute Coronary Syndrome. Curr. Atheroscler. Rep. 2019, 21, 34. [Google Scholar] [CrossRef]
- Moriel, M.; Tzivoni, D.; Behar, S.; Zahger, D.; Hod, H.; Hasdai, D.; Sandach, A.; Gottlieb, S. Contemporary treatment and adherence to guidelines in women and men with acute coronary syndromes. Int. J. Cardiol. 2008, 131, 97–104. [Google Scholar] [CrossRef]
- Ji, H.; Fang, L.; Yuan, L.; Zhang, Q. Effects of Exercise-Based Cardiac Rehabilitation in Patients with Acute Coronary Syndrome: A Meta-Analysis. Med. Sci. Monit. 2019, 25, 5015–5027. [Google Scholar] [CrossRef]
- Sunamura, M.; ter Hoeve, N.; Berg-Emons, R.J.G.V.D.; Boersma, E.; van Domburg, R.T.; Geleijnse, M.L. Cardiac rehabilitation in patients with acute coronary syndrome with primary percutaneous coronary intervention is associated with improved 10-year survival. Eur. Heart J. Qual. Care Clin. Outcomes 2018, 4, 168–172. [Google Scholar] [CrossRef] [PubMed]
- Rodrigues, P.; Santos, M.; Sousa, M.J.; Brochado, B.; Anjo, D.; Barreira, A.; Preza-Fernandes, J.; Palma, P.; Viamonte, S.; Torres, S. Cardiac Rehabilitation after an Acute Coronary Syndrome: The Impact in Elderly Patients. Cardiology 2015, 131, 177–185. [Google Scholar] [CrossRef] [PubMed]
- Collet, J.-P.; Thiele, H.; Barbato, E.; Barthélémy, O.; Bauersachs, J.; Bhatt, D.; Dendale, P.; Dorobantu, M.; Edvardsen, T.; Folliguet, T.; et al. 2020 ESC Guidelines for the management of acute coronary syndromes in patients presenting without persistent ST-segment elevation: The Task Force for the management of acute coronary syndromes in patients presenting without persistent ST-segment elevation. Eur. Heart J. 2021, 42, 1289–1367. [Google Scholar] [CrossRef] [PubMed]
- Gamble, M.; McAllister, F.A.; Johnson, J.A.; Eurich, D.T. Quantifying the impact of drug exposure misclassification due to restrictive drug coverage in administrative databases: A simulation cohort study. Value Health 2012, 15, 191–197. [Google Scholar] [CrossRef] [PubMed]
- Pauly, N.J.; Talbert, J.C.; Brown, J. Low-cost generic program use by Medicare beneficiaries: Implications for medication exposure misclassification in administrative claims data. J. Manag. Care. Spec. Pharm. 2016, 22, 741–751. [Google Scholar] [CrossRef]

| Whole Population (N = 90,779) | Women (N = 31,671) | Men (N = 59,108) | SD | p-Value * | |
|---|---|---|---|---|---|
| Age (years) | 0.66 | <0.001 | |||
| 40–60 | 21,443 (23.6%) | 3924 (12.4%) | 17,519 (29.6%) | ||
| 61–70 | 20,798 (22.9%) | 5368 (17.0%) | 15,430 (26.1%) | ||
| 71–80 | 26,573 (29.3%) | 10,063 (31.8%) | 16,510 (27.9%) | ||
| 81–90 | 21,965 (24.2%) | 12,316 (38.9%) | 9649 (16.3%) | ||
| ACS diagnosis | 0.12 | <0.001 | |||
| STEMI | 41,450 (45.7%) | 13,366 (42.2%) | 28,084 (47.5%) | ||
| NSTEMI | 30,812 (33.9%) | 11,531 (36.4%) | 19,281 (32.6%) | ||
| Unstable angina | 18,517 (20.4%) | 6774 (21.4%) | 11,743 (19.9%) | ||
| Clinical profile † | 0.31 | <0.001 | |||
| Good | 22,808 (25.1%) | 5503 (17.4%) | 17,305 (29.3%) | ||
| Intermediate | 28,062 (30.9%) | 9666 (30.5%) | 18,396 (31.1%) | ||
| Poor | 29,323 (32.3%) | 12,337 (39.0%) | 16,986 (28.7%) | ||
| Very poor | 10,586 (11.7%) | 4105 (13.2%) | 6421 (10.9%) | ||
| Comorbidities ‡ | |||||
| Hypertension | 66,561 (73.3%) | 25,997 (82.1%) | 40,564 (68.6%) | 0.32 | <0.001 |
| Dyslipidaemia | 34,649 (38.2%) | 12,227 (38.6%) | 22,422 (37.9%) | 0.01 | 0.047 |
| Cerebrovascular disease | 7148 (7.9%) | 2987 (9.4%) | 4161 (7.0%) | 0.09 | <0.001 |
| Diabetes | 21,373 (23.5%) | 7856 (24.8%) | 13,517 (22.9%) | 0.05 | <0.001 |
| Chronic renal failure | 1042 (1.2%) | 334 (1.1%) | 708 (1.2%) | 0.01 | 0.054 |
| COPD | 28,421 (31.3%) | 11,104 (35.1%) | 17,317 (29.3%) | 0.12 | <0.001 |
| Depression | 17,305 (19.1%) | 9215 (29.1%) | 8090 (13.7%) | 0.38 | <0.001 |
| OR (95% CI) | |
|---|---|
| Sex: Women vs. Men | 1.02 (0.96–1.08) |
| Age (years) | |
| 40–60 | 1.00 [Reference] |
| 61–70 | 1.67 (1.44–1.92) |
| 71–80 | 2.89 (2.53–3.30) |
| 81–90 | 6.30 (5.23–7.19) |
| ACS diagnosis | |
| Unstable angina | 1.00 [Reference] |
| NSTEMI | 1.40 (1.28–1.53) |
| STEMI | 2.16 (1.98–2.35) |
| Comorbidities ‡ | |
| Hypertension | 2.06 (1.85–2.30) |
| Dyslipidaemia | 0.73 (0.69–0.78) |
| Cerebrovascular disease | 1.28 (1.17–1.39) |
| Diabetes | 1.15 (1.08–1.23) |
| Chronic renal failure | 1.01 (0.81–1.25) |
| COPD | 0.91 (0.86–0.97) |
| Depression | 1.28 (1.20–1.36) |
| Clinical profile † | |
| Good | 1.00 [Reference] |
| Intermediate | 1.09 (0.97–1.21) |
| Poor | 1.54 (1.38–1.72) |
| Very poor | 2.57 (2.26–2.92) |
| Original Cohort (N = 63,442) | Matched Cohort (N = 28,708) | |||||||
|---|---|---|---|---|---|---|---|---|
| Women (N = 20,450) | Men (N = 42,992) | SD | p-Value * | Women (N = 14,354) | Men (N = 14,354) | SD | p-Value * | |
| Drug therapies | ||||||||
| Prescription | ||||||||
| Renin–angiotensin system blockers | 15,285 (74.7%) | 33,716 (78.4%) | 0.09 | <0.001 | 10,726 (74.7%) | 11,346 (79.0%) | 0.10 | <0.001 |
| Beta-blockers | 16,372 (80.1%) | 35,820 (83.3%) | 0.08 | <0.001 | 11,665 (81.3%) | 11,696 (81.5%) | 0.01 | <0.001 |
| Statins | 15,988 (78.2%) | 38,621 (89.8%) | 0.32 | <0.001 | 11,471 (79.9%) | 12,578 (87.6%) | 0.21 | <0.001 |
| Dual antiplatelet treatment | 12,290 (60.1%) | 31,995 (74.4%) | 0.31 | <0.001 | 8772 (61.1%) | 10,257 (71.5%) | 0.22 | <0.001 |
| Three out of four | 14,596 (71.4%) | 35,810 (83.3%) | 0.29 | <0.001 | 10,442 (72.8%) | 11,600 (80.8%) | 0.19 | <0.001 |
| Adherence § | ||||||||
| Renin–angiotensin system blockers | 8772 (57.4%) | 20,251 (60.1%) | 0.05 | <0.001 | 6165 (57.5%) | 6829 (60.2%) | 0.06 | <0.001 |
| Beta-blockers | 8988 (54.9%) | 21,005 (58.6%) | 0.08 | <0.001 | 6500 (55.7%) | 6620 (56.6%) | 0.02 | <0.001 |
| Statins | 10,428 (65.2%) | 29,711 (76.9%) | 0.26 | <0.001 | 7651 (66.7%) | 9290 (73.9%) | 0.16 | <0.001 |
| Dual antiplatelet treatment | 6913 (56.3%) | 20,527 (64.2%) | 0.16 | <0.001 | 5040 (57.5%) | 6410 (62.5%) | 0.10 | <0.001 |
| Three out of four | 5966 (40.9%) | 17,709 (49.5%) | 0.17 | <0.001 | 4396 (42.1%) | 5507 (47.5%) | 0.11 | <0.001 |
| Cardiac controls | ||||||||
| Cardiologic visits | 14,461 (70.7%) | 32,350 (75.3%) | 0.10 | <0.001 | 10,330 (72.0%) | 10,597 (73.8%) | 0.04 | <0.001 |
| ECO-Electrocardiograms | 16,256 (79.5%) | 35,668 (83.0%) | 0.09 | <0.001 | 11,588 (80.7%) | 11,775 (82.0%) | 0.03 | <0.001 |
| Test for lipid profile | 16,524 (80.8%) | 34,982 (81.4%) | 0.01 | <0.001 | 11,690 (81.4%) | 11,708 (81.6%) | 0.00 | <0.001 |
| Two out of three | 16,230 (79.4%) | 35,689 (83.0%) | 0.09 | <0.001 | 11,581 (80.7%) | 11,779 (82.1%) | 0.04 | <0.001 |
| Cardiac rehabilitation | 413 (2.0%) | 2092 (4.9%) | 0.16 | <0.001 | 327 (2.3%) | 565 (3.9%) | 0.10 | <0.001 |
| Men | Women | p-Value * | |
|---|---|---|---|
| Out-of-hospital healthcare † | |||
| Drug therapies | 0.80 (0.75–0.85) | 0.85 (0.79–0.92) | 0.21 |
| Cardiac controls | 0.85 (0.79–0.91) | 0.81 (0.76–0.87) | 0.35 |
| Cardiac rehabilitation | 0.81 (0.67–0.97) | 0.65 (0.48–0.87) | 0.23 |
Disclaimer/Publisher’s Note: The statements, opinions and data contained in all publications are solely those of the individual author(s) and contributor(s) and not of MDPI and/or the editor(s). MDPI and/or the editor(s) disclaim responsibility for any injury to people or property resulting from any ideas, methods, instructions or products referred to in the content. |
© 2023 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Ronco, R.; Rea, F.; Filippelli, A.; Maggioni, A.P.; Corrao, G. Sex-Related Differences in Outpatient Healthcare of Acute Coronary Syndrome: Evidence from an Italian Real-World Investigation. J. Clin. Med. 2023, 12, 2972. https://doi.org/10.3390/jcm12082972
Ronco R, Rea F, Filippelli A, Maggioni AP, Corrao G. Sex-Related Differences in Outpatient Healthcare of Acute Coronary Syndrome: Evidence from an Italian Real-World Investigation. Journal of Clinical Medicine. 2023; 12(8):2972. https://doi.org/10.3390/jcm12082972
Chicago/Turabian StyleRonco, Raffaella, Federico Rea, Amelia Filippelli, Aldo Pietro Maggioni, and Giovanni Corrao. 2023. "Sex-Related Differences in Outpatient Healthcare of Acute Coronary Syndrome: Evidence from an Italian Real-World Investigation" Journal of Clinical Medicine 12, no. 8: 2972. https://doi.org/10.3390/jcm12082972
APA StyleRonco, R., Rea, F., Filippelli, A., Maggioni, A. P., & Corrao, G. (2023). Sex-Related Differences in Outpatient Healthcare of Acute Coronary Syndrome: Evidence from an Italian Real-World Investigation. Journal of Clinical Medicine, 12(8), 2972. https://doi.org/10.3390/jcm12082972








