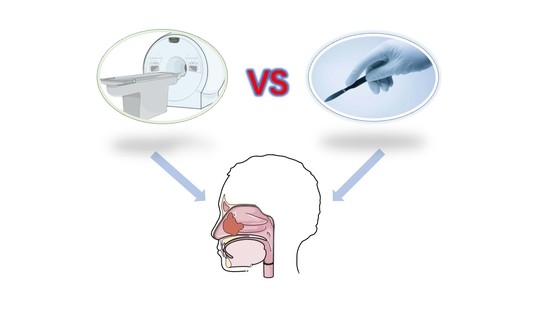
Comparison of Definitive Radiotherapy-Based Treatment and Surgical-Based Treatment for Locally Advanced Head and Neck Soft Tissue Sarcoma
Abstract
:1. Introduction
2. Methods and Materials
2.1. Patient Recruitment
2.2. Treatment
2.2.1. Definitive Radiotherapy-Based Treatment
2.2.2. Radical Surgery-Based Treatment
2.3. Data Collection and Follow-Up
2.4. Statistical Analysis
3. Results
3.1. Patients’ Characteristics
3.2. Abbreviations: CRT: Chemoradiotherapy; CT: Chemotherapy; RT: Radiotherapy, Objective Response Rate (ORR)
3.3. Survival Outcomes
3.4. Prognostic Analysis
3.5. Acute Toxicities
3.6. Representative Cases in the Definitive Radiotherapy-Based Treatment Group
4. Discussion
5. Limitations
6. Conclusions
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Acknowledgments
Conflicts of Interest
Abbreviations
References
- Galy-Bernadoy, C.; Garrel, R. Head and Neck Soft-Tissue Sarcoma in Adults. Eur. Ann. Otorhinolaryngol. Head Neck Dis. 2016, 133, 37–42. [Google Scholar] [CrossRef] [PubMed]
- Stiller, C.A.; Trama, A.; Serraino, D.; Rossi, S.; Navarro, C.; Chirlaque, M.D.; Casali, P.G.; RARECARE Working Group. Descriptive Epidemiology of Sarcomas in Europe: Report from the Rarecare Project. Eur. J. Cancer 2013, 49, 684–695. [Google Scholar] [CrossRef] [PubMed]
- Breakey, R.W.; Crowley, T.P.; Anderson, I.B.; Milner, R.H.; Ragbir, M. The Surgical Management of Head and Neck Sarcoma: The Newcastle Experience. J. Plast. Reconstr. Aesthetic Surg. 2017, 70, 78–84. [Google Scholar] [CrossRef] [PubMed]
- de Bree, R.; van der Waal, I.; de Bree, E.; Leemans, C.R. Management of Adult Soft Tissue Sarcomas of the Head and Neck. Oral Oncol. 2010, 46, 786–790. [Google Scholar] [CrossRef]
- Fayda, M.; Aksu, G.; Agaoglu, F.Y.; Karadeniz, A.; Darendeliler, E.; Altun, M.; Hafiz, G. The Role of Surgery and Radiotherapy in Treatment of Soft Tissue Sarcomas of the Head and Neck Region: Review of 30 Cases. J. Cranio-Maxillo-Facial Surg. 2009, 37, 42–48. [Google Scholar] [CrossRef] [PubMed]
- Tudor-Green, B.; Gomez, R.; Brennan, P.A. Current Update on the Diagnosis and Management of Head and Neck Soft Tissue Sarcomas. J. Oral Pathol. Med. 2017, 46, 674–679. [Google Scholar] [CrossRef] [PubMed]
- Colville, R.J.; Charlton, F.; Kelly, C.G.; Nicoll, J.J.; McLean, N.R. Multidisciplinary Management of Head and Neck Sarcomas. Head Neck 2005, 27, 814–824. [Google Scholar] [CrossRef] [PubMed]
- Edge, S.B.; Compton, C.C. The American Joint Committee on Cancer: The 7th Edition of the AJCC Cancer Staging Manual and the Future of TNM. Ann. Surg. Oncol. 2010, 17, 1471–1474. [Google Scholar] [CrossRef]
- Han, S.; Yin, X.; Xu, W.; Wang, Y.; Han, W. The Management of Head and Neck Sarcoma. J. Craniofacial Surg. 2020, 31, e189–e192. [Google Scholar] [CrossRef]
- Wen, Y.; Huang, D.; Zhang, W.; Zhang, Y.; Hu, H.; Li, J. Radiation Therapy is an Important Factor to Improve Survival in Pediatric Patients with Head and Neck Rhabdomyosarcoma by Enhancing Local Control: A Historical Cohort Study from a Single Center. BMC Pediatr. 2020, 20, 265. [Google Scholar] [CrossRef]
- Allignet, B.; Waissi, W.; Geets, X.; Dufresne, A.; Brahmi, M.; Ray-Coquard, I.; Blay, J.Y.; Bouhamama, A.; Meeus, P.; Vaz, G.; et al. Long-Term Outcomes after Definitive Radiotherapy with Modern Techniques for Unresectable Soft Tissue Sarcoma. Radiother. Oncol. 2022, 173, 55–61. [Google Scholar] [CrossRef] [PubMed]
- Combs, S.E.; Behnisch, W.; Kulozik, A.E.; Huber, P.E.; Debus, J.; Schulz-Ertner, D. Intensity Modulated Radiotherapy (IMRT) and Fractionated Stereotactic Radiotherapy (FSRT) for Children with Head-and-Neck-Rhabdomyosarcoma. BMC Cancer 2007, 7, 177. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Liang, W.; Li, L.; Wang, M.; Liu, Y.; Qiu, Y.; Zhang, B.; Wu, Q.; Wei, Y. Non-Inferior Efficacy of Non-Surgical Treatment to Surgical Treatment in Patients with Nonmetastatic Head and Neck Rhabdomyosarcoma: A Seer-Based Study. Clin. Transl. Oncol. 2023, 1–14. [Google Scholar] [CrossRef] [PubMed]
- Le Péchoux, C.; Llacer, C.; Sargos, P.; Moureau-Zabotto, L.; Ducassou, A.; Sunyach, M.P.; Biston, M.C.; Thariat, J. Conformal Radiotherapy in Management of Soft Tissue Sarcoma in Adults. Cancer Radiother. 2022, 26, 377–387. [Google Scholar] [CrossRef] [PubMed]
- Oertel, M.; Reinartz, G.; Scobioala, S.; Eich, H.T. Successful Treatment of a Rare Case of Ameloblastic Fibrosarcoma with Radiation Therapy. Strahlenther. Onkol. 2017, 193, 666–672. [Google Scholar] [CrossRef]
- Wygoda, A.; Rutkowski, T.; Ponikiewska, D.; Hejduk, B.; Składowski, K. Ewing’s Sarcoma of the Larynx. Effective Treatment with Organ Preservation. Strahlenther. Onkol. 2013, 189, 586–589. [Google Scholar] [CrossRef]
- Kim, J.K.; Verma, N.; McBride, S.; Riaz, N.; Boyle, J.O.; Bs, D.S.; Bs, C.S.; Bs, T.W.; Bs, T.B.; Alektiar, K.; et al. Patterns of Radiotherapy Use and Outcomes in Head and Neck Soft-Tissue Sarcoma in a National Cohort. Laryngoscope 2020, 130, 120–127. [Google Scholar] [CrossRef]
- Workman, A.D.; Farquhar, D.R.; Brody, R.M.; Parasher, A.K.; Carey, R.M.; Purkey, M.T.; Nagda, D.A.; Brooks, J.S.; Hartner, L.P.; Brant, J.; et al. Leiomyosarcoma of the Head and Neck: A 17-Year Single Institution Experience and Review of the National Cancer Data Base. Head Neck 2018, 40, 756–762. [Google Scholar] [CrossRef]
- Eeles, R.; Fisher, C.; A’Hern, R.P.; Robinson, M.E.; Rhys-Evans, P.; Henk, J.M.; Archer, D.R.; Harmer, C.L. Head and Neck Sarcomas: Prognostic Factors and Implications for Treatment. Br. J. Cancer 1993, 68, 201–207. [Google Scholar] [CrossRef] [Green Version]
- Moore, C.; McLister, C.; Cardwell, C.; O’Neill, C.; Donnelly, M.; McKenna, G. Dental Caries Following Radiotherapy for Head and Neck Cancer: A Systematic Review. Oral Oncol. 2020, 100, 104484. [Google Scholar] [CrossRef]
- Alfouzan, A.F. Radiation Therapy in Head and Neck Cancer. Saudi. Med. J. 2021, 42, 247–254. [Google Scholar] [CrossRef] [PubMed]
- Liu, J.; Du, J.; Fan, J.; Liu, K.; Zhang, B.; Wang, S.; Wang, W.; Wang, Z.; Cai, Y.; Li, C.; et al. The Neutrophil-to-Lymphocyte Ratio Correlates with Age in Patients with Papillary Thyroid Carcinoma. Orl 2015, 77, 109–116. [Google Scholar] [CrossRef] [PubMed]
- Li, J.; Chen, Q.; Luo, X.; Hong, J.; Pan, K.; Lin, X.; Liu, X.; Zhou, L.; Wang, H.; Xu, Y.; et al. Neutrophil-to-Lymphocyte Ratio Positively Correlates to Age in Healthy Population. J. Clin. Lab. Anal. 2015, 29, 437–443. [Google Scholar] [CrossRef] [PubMed]
- Ruggiero, C.; Metter, E.J.; Cherubini, A.; Maggio, M.; Sen, R.; Najjar, S.S.; Windham, G.B.; Ble, A.; Senin, U.; Ferrucci, L. White Blood Cell Count and Mortality in the Baltimore Longitudinal Study of Aging. J. Am. Coll. Cardiol. 2007, 49, 1841–1850. [Google Scholar] [CrossRef] [Green Version]
- Idowu, O.K.; Ding, Q.; Taktak, A.F.G.; Chandrasekar, C.R.; Yin, Q. Clinical Implication of Pretreatment Neutrophil to Lymphocyte Ratio in Soft Tissue Sarcoma. Biomarkers 2012, 17, 539–544. [Google Scholar] [CrossRef]
- Nakamura, T.; Matsumine, A.; Matsubara, T.; Asanuma, K.; Uchida, A.; Sudo, A. The Combined Use of the Neutrophil-Lymphocyte Ratio and C-Reactive Protein Level as Prognostic Predictors in Adult Patients with Soft Tissue Sarcoma. J. Surg. Oncol. 2013, 108, 481–485. [Google Scholar] [CrossRef]
- Szkandera, J.; Absenger, G.; Liegl-Atzwanger, B.; Pichler, M.; Stotz, M.; Samonigg, H.; Glehr, M.; Zacherl, M.; Stojakovic, T.; Gerger, A.; et al. Elevated Preoperative Neutrophil/Lymphocyte Ratio Is Associated with Poor Prognosis in Soft-Tissue Sarcoma Patients. Br. J. Cancer 2013, 108, 1677–1683. [Google Scholar] [CrossRef] [Green Version]
- Szkandera, J.; Gerger, A.; Liegl-Atzwanger, B.; Absenger, G.; Stotz, M.; Friesenbichler, J.; Trajanoski, S.; Stojakovic, T.; Eberhard, K.; Leithner, A.; et al. The Lymphocyte/Monocyte Ratio Predicts Poor Clinical Outcome and Improves the Predictive Accuracy in Patients with Soft Tissue Sarcomas. Int. J. Cancer 2014, 135, 362–370. [Google Scholar] [CrossRef]
- Jiang, L.; Jiang, S.; Situ, D.; Lin, Y.; Yang, H.; Li, Y.; Long, H.; Zhou, Z. Prognostic Value of Monocyte and Neutrophils to Lymphocytes Ratio in Patients with Metastatic Soft Tissue Sarcoma. Oncotarget 2015, 6, 9542–9550. [Google Scholar] [CrossRef] [Green Version]
- Que, Y.; Qiu, H.; Li, Y.; Chen, Y.; Xiao, W.; Zhou, Z.; Zhang, X. Preoperative Platelet-Lymphocyte Ratio Is Superior to Neutrophil-Lymphocyte Ratio as a Prognostic Factor for Soft-Tissue Sarcoma. BMC Cancer 2015, 15, 648. [Google Scholar] [CrossRef] [Green Version]
- Templeton, A.J.; Mcnamara, M.G.; Šeruga, B.; Vera-Badillo, F.E.; Aneja, P.; Ocaña, A.; Leibowitz-Amit, R.; Sonpavde, G.; Knox, J.J.; Tran, B.; et al. Prognostic Role of Neutrophil-to-Lymphocyte Ratio in Solid Tumors: A Systematic Review and Meta-Analysis. J. Natl. Cancer Inst. 2014, 106, dju124. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Kitamura, T.; Qian, B.-Z.; Pollard, J.W. Immune Cell Promotion of Metastasis. Nat. Rev. Immunol. 2015, 15, 73–86. [Google Scholar] [CrossRef] [Green Version]
- De Larco, J.E.; Wuertz, B.R.; Furcht, L.T. The Potential Role of Neutrophils in Promoting the Metastatic Phenotype of Tumors Releasing Interleukin-8. Clin. Cancer Res. 2004, 10, 4895–4900. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Petrie, H.T.; Klassen, L.W.; Kay, H.D. Inhibition of Human Cytotoxic T Lymphocyte Activity in Vitro by Autologous Peripheral Blood Granulocytes. J. Immunol. 1985, 134, 230–234. [Google Scholar] [CrossRef] [PubMed]
- SShau, H.Y.; Kim, A. Suppression of Lymphokine-Activated Killer Induction by Neutrophils. J. Immunol. 1988, 141, 4395–4402. [Google Scholar] [CrossRef]



| Characteristics | Definitive Radiotherapy-Based Treatment (n = 16) | Radical Surgery-Based Treatment (n = 8) | p-Value |
|---|---|---|---|
| Gender | 0.665 | ||
| Male (%) | 9 (56.2) | 3 (37.5) | |
| Female (%) | 7 (43.8) | 5 (62.5) | |
| Age (years) | 31.00 [24.75, 45.00] | 21.00 [15.25, 26.75] | 0.018 |
| PS score (%) | 0.513 | ||
| 0 | 3 (18.8) | 0 (0.0) | |
| 1 | 13 (81.2) | 8 (100.0) | |
| Pathological subtype (%) | 0.285 | ||
| Rhabdomyosarcoma | 8 (50.0) | 2 (25.0) | |
| Fibrosarcoma | 1 (6.2) | 3 (37.5) | |
| Synovial sarcoma | 3 (18.8) | 2 (25.0) | |
| Undifferentiated sarcoma | 2 (12.5) | 0 (0.0) | |
| Others | 2 (12.5) | 1 (12.5) | |
| T * (%) | 0.663 | ||
| T2 | 6 (37.5) | 2 (25.0) | |
| T3 | 5 (31.2) | 2 (25.0) | |
| T4 | 5 (31.2) | 4 (50.0) | |
| N * (%) | 1 | ||
| N0 | 6 (37.5) | 3 (37.5) | |
| N1 | 10 (62.5) | 5 (62.5) | |
| TNM stage * (%) | 1 | ||
| III | 6 (37.5) | 3 (37.5) | |
| IV | 10 (62.5) | 5 (62.5) | |
| BMI (kg/m2) | 22.90 [20.82, 23.52] | 19.23 [18.27, 21.03] | 0.098 |
| WBC (109/L) | 5.96 [4.82, 6.54] | 6.06 [4.65, 6.74] | 1 |
| RBC (1012/L) | 4.06 [3.67, 4.53] | 3.80 [3.52, 4.55] | 0.501 |
| Hb (mmol/L) | 123.15 [106.33, 132.15] | 113.40 [107.25, 127.52] | 0.624 |
| PLT (109/L) | 230.00 [219.00, 303.00] | 237.50 [197.25, 321.50] | 0.83 |
| NLR | 2.46 [1.96, 3.55] | 1.42 [1.13, 1.76] | 0.01 |
| PLR | 173.07 [151.29, 227.62] | 124.56 [109.31, 146.83] | 0.037 |
| Definitive Radiotherapy-Based Treatment (n = 16) | Radical Surgery-Based Treatment (n = 8) | |||
|---|---|---|---|---|
| Treatment protocols (%) | ||||
| RT alone | 3 (18.8) | Surgery alone | 0 (0) | |
| Induction CT + RT | 3 (18.8) | Surgery + adjuvant CT | 1 (12.5) | |
| Induction CT + concurrent CRT | 8 (50.0) | Surgery + adjuvant CRT | 3 (37.5) | |
| Concurrent CRT | 1 (6.3) | Surgery + adjuvant RT | 4 (50.0) | |
| Definitive Radiotherapy-Based Treatment (n = 16) | Radical Surgery-Based Treatment (n = 8) | |
|---|---|---|
| ORR (%) | ||
| CR | 6 (37.5) | 8 (100.0) |
| PR | 9 (56.3) | 0 (0) |
| SD | 0 (0) | 0 (0) |
| PD | 1 (6.3) | 0 (0) |
| Definitive Radiotherapy-Based Treatment (n = 16) | Radical Surgery-Based Treatment (n = 8) | p-Value | |
|---|---|---|---|
| Overall survival | 0.350 | ||
| 3-year OS rate (95%CI) | 0.642 (0.429–0.959) | 0.875 (0.673–1.000) | |
| Distant metastasis-free survival | 0.240 | ||
| 3-year DMFS rate (95%CI) | 0.639 (0.426–0.960) | 0.875 (0.673–1.000) | |
| Loco-regional recurrence-free survival | 0.480 | ||
| 3-year LRRFS rate (95%CI) | 0.938 (0.826–1.000) | 1 (1–1) | |
| Progression-free survival | 0.100 | ||
| 3-year PFS rate (95%CI) | 0.519 (0.313–0.862) | 0.875 (0.673–1.000) |
| Characteristics | OS HR (95% CI) | p-Value | DMFS HR (95% CI) | p-Value | PFS HR (95% CI) | p-Value |
|---|---|---|---|---|---|---|
| Gender (Female) | 0.449 (0.082–2.462) | 0.356 | 0.359 (0.069–1.858) | 0.222 | 0.396 (0.098–1.589) | 0.191 |
| Age(years) | 1.014 (0.96–1.07) | 0.62 | 1.018 (0.97–1.068) | 0.471 | 1.051 (1.002–1.102) | 0.043 |
| PS (1) | 0.671 (0.078–5.784) | 0.717 | 0.797 (0.095–6.673) | 0.834 | 0.516 (0.106–2.502) | 0.411 |
| BMI (kg/m2) | 1.204 (0.928–1.563) | 0.163 | 1.195 (0.938–1.522) | 0.15 | 1.148 (0.934–1.411) | 0.191 |
| NLR | 1.18 (0.9–1.549) | 0.231 | 1.143 (0.875–1.494) | 0.328 | 1.207 (0.974–1.497) | 0.086 |
| PLR | 0.998 (0.989–1.007) | 0.613 | 1 (0.993–1.006) | 0.885 | 1.001 (0.997–1.005) | 0.592 |
| T (T3-T4) | 0.866 (0.157–4.765) | 0.869 | 1.237 (0.237–6.451) | 0.8 | 0.516 (0.137–1.937) | 0.327 |
| N (N1) | 3.642 (0.424–31.269) | 0.239 | 1.815 (0.35–9.409) | 0.478 | 2.813 (0.581–13.619) | 0.199 |
| Treatment (Surgery) | 0.374 (0.044–3.207) | 0.37 | 0.298 (0.036–2.483) | 0.263 | 0.208 (0.026–1.669) | 0.139 |
| Induction CT (Yes) | 1.41 (0.282–7.05) | 0.676 | 1.108 (0.245–5.008) | 0.894 | 1.048 (0.279–3.931) | 0.945 |
| Concurrent CT (Yes) | 0.766 (0.14–4.208) | 0.759 | 0.682 (0.132–3.527) | 0.648 | 0.763 (0.19–3.061) | 0.703 |
| Adjuvant CT (Yes) | 1.247 (0.144–10.77) | 0.841 | 1.011 (0.121–8.443) | 0.992 | 0.701 (0.087–5.623) | 0.738 |
| Characteristics | OS HR (95% CI) | p-Value | DMFS HR (95% CI) | p-Value | PFS HR (95% CI) | p-Value |
|---|---|---|---|---|---|---|
| Age (years) | 1.015 (0.925–1.113) | 0.759 | 1.029 (0.949–1.115) | 0.491 | 1.074 (0.997–1.157) | 0.059 |
| PS (1) | 0.558 (0.033–9.48) | 0.686 | 0.639 (0.059–6.94) | 0.713 | 0.785 (0.119–5.189) | 0.802 |
| NLR | 1.484 (0.958–2.299) | 0.077 | 1.191 (0.829–1.712) | 0.344 | 1.236 (0.863–1.77) | 0.247 |
| PLR | 0.99 (0.974–1.006) | 0.204 | 0.996 (0.987–1.005) | 0.368 | 1 (0.994–1.007) | 0.924 |
| T (T3-T4) | 1.367 (0.123–15.209) | 0.799 | 3.063 (0.333–28.16) | 0.323 | 1.435 (0.243–8.464) | 0.69 |
| N (N1) | 3.053 (0.279–33.428) | 0.361 | 1.87 (0.311–11.243) | 0.494 | 4.961 (0.762–32.316) | 0.094 |
| Treatment (Surgery) | 0.455 (0.035–5.888) | 0.547 | 0.344 (0.031–3.808) | 0.384 | 0.52 (0.049–5.568) | 0.589 |
| Variables | Definitive Radiotherapy-Based Treatment (n = 16) | Radical Surgery-Based Treatment (n = 8) | p-Value |
|---|---|---|---|
| Leukocytopenia | 2 (12.5) | 1 (12.5) | 1 |
| Neutropenia | 2 (12.5) | 1 (12.5) | 1 |
| Anemia | 1 (6.2) | 1 (12.5) | 1 |
| Thrombocytopenia | 3 (18.8) | 0 (0.0) | 0.513 |
| ALT increase | 0 (0.0) | 0 (0.0) | 1 |
| AST increase | 0 (0.0) | 0 (0.0) | 1 |
| Total bilirubin increase | 0 (0.0) | 0 (0.0) | 1 |
| Gastrointestinal reaction | 3 (18.8) | 0 (0.0) | 0.513 |
| Radio-mucositis | 2 (12.5) | 1 (12.5) | 1 |
| Radiodermatitis | 2 (12.5) | 2 (25.0) | 0.846 |
Disclaimer/Publisher’s Note: The statements, opinions and data contained in all publications are solely those of the individual author(s) and contributor(s) and not of MDPI and/or the editor(s). MDPI and/or the editor(s) disclaim responsibility for any injury to people or property resulting from any ideas, methods, instructions or products referred to in the content. |
© 2023 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Wu, Q.; Wang, J.; Li, S.; Liu, J.; Cheng, Y.; Jin, J.; Zhong, Y. Comparison of Definitive Radiotherapy-Based Treatment and Surgical-Based Treatment for Locally Advanced Head and Neck Soft Tissue Sarcoma. J. Clin. Med. 2023, 12, 3099. https://doi.org/10.3390/jcm12093099
Wu Q, Wang J, Li S, Liu J, Cheng Y, Jin J, Zhong Y. Comparison of Definitive Radiotherapy-Based Treatment and Surgical-Based Treatment for Locally Advanced Head and Neck Soft Tissue Sarcoma. Journal of Clinical Medicine. 2023; 12(9):3099. https://doi.org/10.3390/jcm12093099
Chicago/Turabian StyleWu, Qiuji, Juan Wang, Shaojie Li, Jia Liu, Yanshuang Cheng, Jieying Jin, and Yahua Zhong. 2023. "Comparison of Definitive Radiotherapy-Based Treatment and Surgical-Based Treatment for Locally Advanced Head and Neck Soft Tissue Sarcoma" Journal of Clinical Medicine 12, no. 9: 3099. https://doi.org/10.3390/jcm12093099