Determining Factors of Alarm Fatigue among Nurses in Intensive Care Units—A Polish Pilot Study
Abstract
1. Introduction
2. Methods
2.1. Study Design
2.2. Setting and Ethical Considerations
2.3. Participants
2.4. Variables
2.5. Outcomes
2.6. Study Size
2.7. Data Analysis
3. Results
3.1. Characteristics of Participants
3.2. Nurses’ Alarm Fatigue Questionnaire Responses
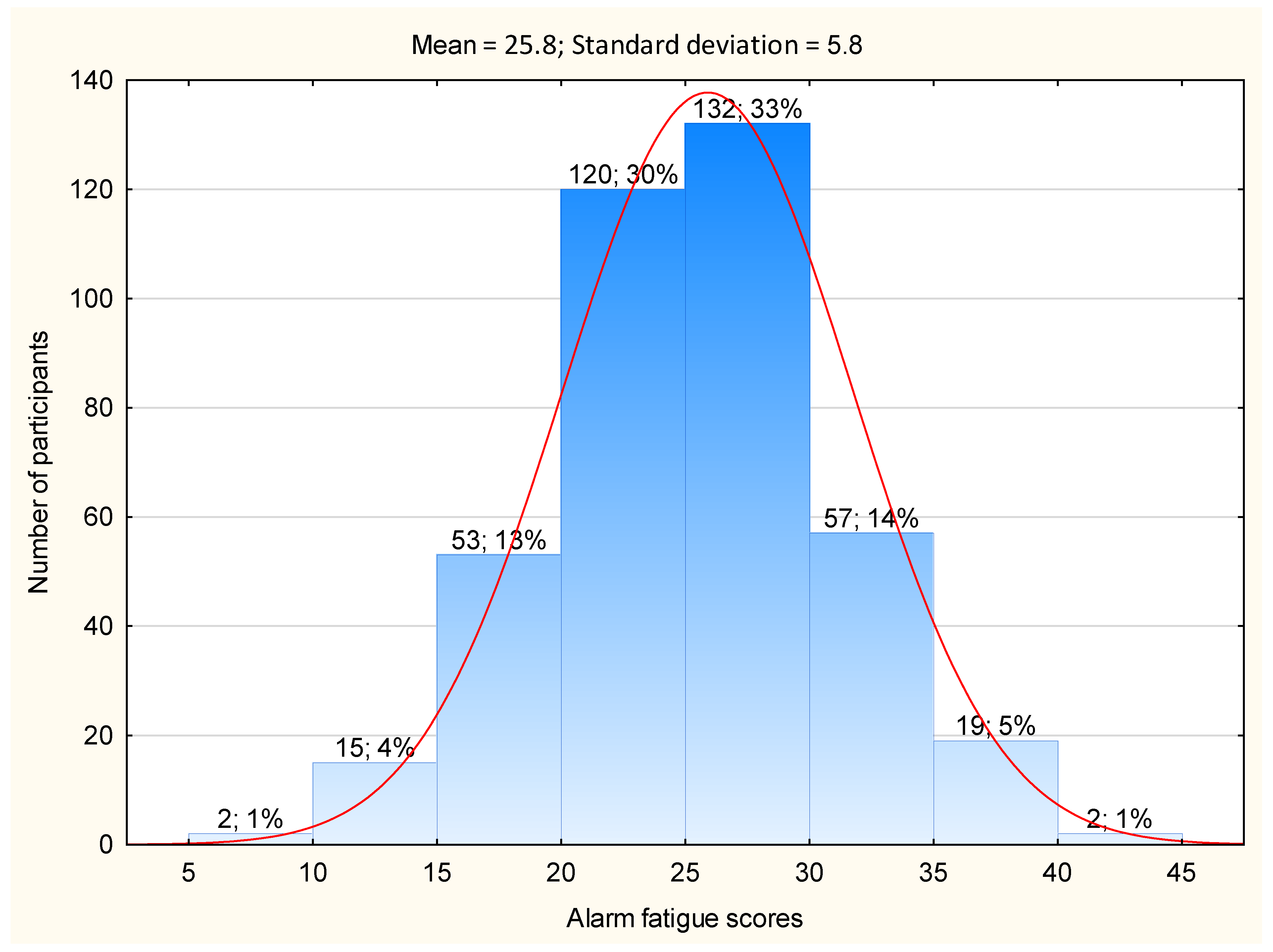
3.3. Overall Alarm Fatigue Scores
3.4. Factors Related to Nurses’ Alarm Fatigue
4. Discussion
5. Conclusions
5.1. Strengths and Limitations
5.2. Implications for Clinical Practice
Supplementary Materials
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Acknowledgments
Conflicts of Interest
References
- Shaban Aysha, Z.M.; Sayed Ahmed, S.E. The Effect of Implementing Clinical Alarm Nursing Intervention Program on Nurses’ Knowledge, Practice and Patient Outcomes at Intensive Care Unit. Am. J. Nurs. Res. 2019, 7, 824–835. [Google Scholar] [CrossRef]
- Bi, J.; Yin, X.; Li, H.; Gao, R.; Zhang, Q.; Zhong, T.; Zan, T.; Guan, B.; Li, Z. Effects of monitor alarm management training on nurses’ alarm fatigue: A randomised controlled trial. J. Clin. Nurs. 2020, 29, 4203–4216. [Google Scholar] [CrossRef] [PubMed]
- Keller, J.P. Clinical alarm hazards: A “top ten” health technology safety concern. J. Electrocardiol. 2012, 45, 588–591. [Google Scholar] [CrossRef]
- Bitan, Y.; Meyer, J.; Shinar, D.; Zmora, E. Nurses’ reactions to alarms in a neonatal intensive care unit. Cogn. Technol. Work 2004, 6, 239–246. [Google Scholar] [CrossRef]
- Ruskin, K.J.; Hueske-Kraus, D. Alarm fatigue: Impacts on Patient Safety. Curr. Opin. Anaesthesiol. 2015, 28, 685–690. [Google Scholar] [CrossRef]
- Paine, C.W.; Goel, V.V.; Ely, E.; Stave, C.D.; Stemler, S.; Zander, M.; Bonafide, C.P. Systematic Review of Physiologic Monitor Alarm Characteristics and Pragmatic Interventions to Reduce Alarm Frequency. J. Hosp. Med. 2015, 11, 136–144. [Google Scholar] [CrossRef]
- Fernandes, C.; Miles, S.; Lucena, C.J.P. Detecting False Alarms by Analyzing Alarm-Context Information: Algorithm Development and Validation. JMIR Med. Inform. 2020, 8, e15407. [Google Scholar] [CrossRef]
- Imhoff, M.; Kuhls, S. Alarm Algorithms in Critical Care Monitoring. Obstet. Anesthesia 2006, 102, 1525–1537. [Google Scholar] [CrossRef]
- Petersen, E.M.; Costanzo, C.L. Assessment of Clinical Alarms Influencing Nurses’ Perceptions of Alarm Fatigue. Dimens. Crit. Care Nurs. 2017, 36, 36–44. [Google Scholar] [CrossRef]
- Nyarko, B.A.; Nie, H.; Yin, Z.; Chai, X.; Yue, L. The effect of educational interventions in managing nurses’ alarm fatigue: An integrative review. J. Clin. Nurs. 2022, 1–13. [Google Scholar] [CrossRef]
- Al-Mugheed, K.; Bayraktar, N. Patient safety attitudes among critical care nurses: A case study in North Cyprus. Int. J. Health Plan. Manag. 2020, 35, 910–921. [Google Scholar] [CrossRef]
- Al-Mugheed, K.; Bayraktar, N.; Al-Bsheish, M.; AlSyouf, A.; Jarrar, M.; AlBaker, W.; Aldhmadi, B.K. Patient Safety Attitudes among Doctors and Nurses: Associations with Workload, Adverse Events, Experience. Healthcare 2022, 10, 631. [Google Scholar] [CrossRef] [PubMed]
- Cvach, M. Monitor Alarm Fatigue: An Integrative Review. Biomed. Instrum. Technol. 2012, 46, 268–277. [Google Scholar] [CrossRef] [PubMed]
- Christensen, M.; Dodds, A.; Sauer, J.; Watts, N. Alarm setting for the critically ill patient: A descriptive pilot survey of nurses’ perceptions of current practice in an Australian Regional Critical Care Unit. Intensiv. Crit. Care Nurs. 2014, 30, 204–210. [Google Scholar] [CrossRef] [PubMed]
- Claudio, D.; Deb, S.; Diegel, E.M. A Framework to Assess Alarm Fatigue Indicators in Critical Care Staff. Crit. Care Explor. 2021, 3, e0464. [Google Scholar] [CrossRef] [PubMed]
- Bourji, H.; Sabbah, H.; Al’jamil, A.; Khamis, R.; Sabbah, S.; Droubi, N.; Sabbah, I.M. Evaluating the Alarm Fatigue and its Associated Factors among Clinicians in Critical Care Units. Eur. J. Clin. Med. 2020, 1, 1–9. [Google Scholar] [CrossRef]
- Despins, L.A. Factors influencing when intensive care unit nurses go to the bedside to investigate patient related alarms: A descriptive qualitative study. Intensiv. Crit. Care Nurs. 2017, 43, 101–107. [Google Scholar] [CrossRef] [PubMed]
- Torabizadeh, C.; Yousefinya, A.; Zand, F.; Rakhshan, M.; Fararooei, M. A nurses’ alarm fatigue questionnaire: Development and psychometric properties. J. Clin. Monit. Comput. 2016, 31, 1305–1312. [Google Scholar] [CrossRef]
- Mishra, P.; Singh, U.; Pandey, C.M.; Mishra, P.; Pandey, G. Application of student’s t-test, analysis of variance, and covariance. Ann. Card. Anaesth. 2019, 22, 407–411. [Google Scholar] [CrossRef]
- Bazdaric, K.; Sverko, D.; Salaric, I.; Martinovic, A.; Lucijanic, M. The ABC of linear regression analysis: What every author and editor should know. Eur. Sci. Ed. 2021, 47, e63780. [Google Scholar] [CrossRef]
- Lewis, C.L.; Oster, C.A. Research Outcomes of Implementing CEASE: An Innovative, Nurse-Driven, Evidence-Based, Patient-Customized Monitoring Bundle to Decrease Alarm Fatigue in the Intensive Care Unit/Step-down Unit. Dimens. Crit. Care Nurs. 2019, 38, 160–173. [Google Scholar] [CrossRef] [PubMed]
- Honan, L.; Funk, M.; Maynard, M.; Fahs, D.; Clark, J.T.; David, Y. Nurses’ Perspectives on Clinical Alarms. Am. J. Crit. Care 2015, 24, 387–395. [Google Scholar] [CrossRef] [PubMed]
- ECRI Institute Top 10 Health Technology Hazards for 2020 Expert Insights from Health Devices EXECUTIVE BRIEF. Available online: www.ecri.org/2020hazards (accessed on 1 January 2023).
- Hravnak, M.; Pellathy, T.; Chen, L.; Dubrawski, A.; Wertz, A.; Clermont, G.; Pinsky, M.R. A call to alarms: Current state and future directions in the battle against alarm fatigue. J. Electrocardiol. 2018, 51, S44–S48. [Google Scholar] [CrossRef] [PubMed]
- Mira, J.J.; Lorenzo, S.; Carrillo, I.; Ferrús, L.; Silvestre, C.; Astier, P.; Iglesias-Alonso, F.; Maderuelo, J.A.; Pérez-Pérez, P.; Torijano, M.L.; et al. Lessons learned for reducing the negative impact of adverse events on patients, health professionals and healthcare organizations. Int. J. Qual. Health Care 2017, 29, 450–460. [Google Scholar] [CrossRef] [PubMed]
- Asadi, N.; Salmani, F.; Asgari, N.; Salmani, M. Alarm fatigue and moral distress in ICU nurses in COVID-19 pandemic. BMC Nurs. 2022, 21, 1–7. [Google Scholar] [CrossRef] [PubMed]
- Seifert, M.; Tola, D.H.; Thompson, J.; McGugan, L.; Smallheer, B. Effect of bundle set interventions on physiologic alarms and alarm fatigue in an intensive care unit: A quality improvement project. Intensiv. Crit. Care Nurs. 2021, 67, 103098. [Google Scholar] [CrossRef]
- Cho, O.M.; Kim, H.; Lee, Y.W.; Cho, I. Clinical Alarms in Intensive Care Units: Perceived Obstacles of Alarm Management and Alarm Fatigue in Nurses. Health Inform. Res. 2016, 22, 46–53. [Google Scholar] [CrossRef]
- Winters, B.D.; Cvach, M.M.; Bonafide, C.P.; Hu, X.; Konkani, A.; O’Connor, M.F.; Rothschild, J.M.; Selby, N.M.; Pelter, M.M.; McLean, B.; et al. Technologic Distractions (Part 2): A Summary of Approaches to Manage Clinical Alarms with Intent to Reduce Alarm Fatigue. Crit. Care Med. 2018, 46, 130–137. [Google Scholar] [CrossRef]
- Lewandowska, K.; Weisbrot, M.; Cieloszyk, A.; Mędrzycka-Dąbrowska, W.; Krupa, S.; Ozga, D. Impact of Alarm Fatigue on the Work of Nurses in an Intensive Care Environment—A Systematic Review. Int. J. Environ. Res. Public Health 2020, 17, 8409. [Google Scholar] [CrossRef]
- Zhao, Y.; Wan, M.; Liu, H.; Ma, M. The Current Situation and Influencing Factors of the Alarm Fatigue of Nurses’ Medical Equipment in the Intensive Care Unit Based on Intelligent Medical Care. J. Health Eng. 2021, 2021, 1–13. [Google Scholar] [CrossRef]
- Weeks, K.; Timalonis, J.; Donovan, L. Does Alarm Fatigue Start in Nursing School? Nursing 2021, 51, 59–63. [Google Scholar] [CrossRef] [PubMed]
- Storm, J.; Chen, H. The relationships among alarm fatigue, compassion fatigue, burnout and compassion satisfaction in critical care and step-down nurses. J. Clin. Nurs. 2020, 30, 443–453. [Google Scholar] [CrossRef] [PubMed]
- Tirvienė, G.; Spirgienė, L.; Šimatonienė, V. Fatigue among Intensive Care Unit Nurses. NERP 2020, 10, 4–9. [Google Scholar]
- Huo, J.; Wung, S.-F.; Roveda, J.; Li, A. Reducing False Alarms in Intensive Care Units: A Scoping Review. Explor. Res. Hypothesis Med. 2023, 8, 57–64. [Google Scholar] [CrossRef]
- Schmidt, N.; Gerber, S.M.; Zante, B.; Gawliczek, T.; Chesham, A.; Gutbrod, K.; Müri, R.M.; Nef, T.; Schefold, J.C.; Jeitziner, M.-M. Effects of intensive care unit ambient sounds on healthcare professionals: Results of an online survey and noise exposure in an experimental setting. Intensiv. Care Med. Exp. 2020, 8, 34. [Google Scholar] [CrossRef]
- Souza, R.C.M.d.S.; Calache, A.L.S.C.; Oliveira, E.G.B.; Nascimento, J.C.D.B.; da Silva, N.D.B.; Poveda, V.D.B. Noise reduction in the ICU: A best practice implementation project. JBI Évid. Implement. 2022, 20, 385–393. [Google Scholar] [CrossRef] [PubMed]
- Kol, E.; Demircan, A.; Erdoğan, A.; Gencer, Z.; Erengin, H. The Effectiveness of Measures Aimed at Noise Reduction in an Intensive Care Unit. Work. Health Saf. 2015, 63, 539–545. [Google Scholar] [CrossRef]
- Scott, J.B.; De Vaux, L.; Dills, C.; Strickland, S.L. Mechanical Ventilation Alarms and Alarm Fatigue. Respir. Care 2019, 64, 1308–1313. [Google Scholar] [CrossRef]
- Simpson, K.R.; Lyndon, A. False Alarms and Overmonitoring: Major Factors in Alarm Fatigue among Labor Nurses. J. Nurs. Care Qual. 2019, 34, 66–72. [Google Scholar] [CrossRef]
- Liu, P.; Xu, M.; Wang, H.; Pi, H.; Xie, P.; Li, Y. A Survey of Patient Monitoring Alarms in Cardiac Care Units. Chin. J. Med. Instrum. 2021, 45, 450–453. [Google Scholar] [CrossRef]
- He, X.; Liu, M.; Liu, S.; Sun, Z.; Wang, C.; Li, Y. Research on Patient Monitoring Alarms in ICU and NICU. Chin. J. Med. Instrum. 2021, 30, 585–590. [Google Scholar] [CrossRef]
- Watanakeeree, K.; Suba, S.; Mackin, L.A.; Badilini, F.; Pelter, M.M. ECG alarms during left ventricular assist device (LVAD) therapy in the ICU. Hear. Lung 2021, 50, 763–769. [Google Scholar] [CrossRef] [PubMed]
- Carayon, P.; Alvarado, C.J. Workload and Patient Safety Among Critical Care Nurses. Crit. Care Nurs. Clin. N. Am. 2007, 19, 121–129. [Google Scholar] [CrossRef] [PubMed]
- Melnyk, B.M.; Tan, A.; Hsieh, A.P.; Gawlik, K.; Arslanian-Engoren, C.; Braun, L.T.; Dunbar, S.; Dunbar-Jacob, J.; Lewis, L.M.; Millan, A.; et al. Critical Care Nurses’ Physical and Mental Health, Worksite Wellness Support, and Medical Errors. Am. J. Crit. Care 2021, 30, 176–184. [Google Scholar] [CrossRef]
| No. | Statement | Always | Usually | Sometimes | Rarely | Never |
|---|---|---|---|---|---|---|
| 1 | I regularly readjust the limits of alarms based on the clinical symptoms of patients | 90 (22.5) | 160 (40.0) | 87 (21.7) | 54 (13.5) | 9 (2.2) |
| 2 | I turn off the alarms at the beginning of every shift | 8 (2.0) | 30 (7.5) | 49 (12.2) | 82 (20.5) | 231 (57.7) |
| 3 | Generally, I hear a certain amount of noise in the ward | 151 (37.7) | 139 (34.7) | 68 (17.0) | 37 (9.2) | 5 (1.2) |
| 4 | I believe much of the noise in the ward is from the alarms of the monitoring equipment | 88 (22.0) | 214 (53.5) | 76 (19) | 22 (5.5) | 0 (0.0) |
| 5 | I pay more attention to the alarms in certain shifts | 100 (25.0) | 149 (37.2) | 113 (28.2) | 26 (6.5) | 12 (3.0) |
| 6 | In some shifts the heavy workload in the ward prevents my quick response to alarms | 41 (10.2) | 110 (27.5) | 160 (40.0) | 69 (17.2) | 20 (5.0) |
| 7 | When alarms go off repeatedly, I become indifferent to them | 11 (2.7) | 80 (20.0) | 123 (30.7) | 114 (28.5) | 72 (18.0) |
| 8 | Alarm sounds make me nervous | 61 (15.2) | 92 (23.0) | 163 (40.7) | 68 (17.0) | 16 (4.0) |
| 9 | I react differently to the low-volume (yellow) and high-volume (red) alarms of the ventilator | 124 (31.0) | 140 (35.0) | 73 (18.2) | 43 (10.7) | 20 (5.0) |
| 10 | When I’m upset and nervous, I’m more responsive to alarm sounds | 105 (26.2) | 132 (33.0) | 95 (23.7) | 51 (12.7) | 17 (4.2) |
| 11 | When alarms go off repeatedly and continuously, I lose my patience | 42 (10.5) | 116 (29.0) | 142 (35.5) | 68 (17.0) | 32 (8.0) |
| 12 | Alarm sounds prevent me from focusing on my professional duties | 34 (8.5) | 102 (25.5) | 142 (35.5) | 89 (22.2) | 33 (8.2) |
| 13 | At visiting hours, I pay less attention to the alarms of the equipment | 7 (1.7) | 24 (6.0) | 59 (14.7) | 127 (31.7) | 183 (45.7) |
| Variable | Frequency (Percent) | Mean (Standard Deviation) | Test Statistic, p Value |
|---|---|---|---|
| Gender | |||
| • Female | 352 (88.0) | 26.0 ± 5.8 | t = 1.67 p = 0.09 |
| • Male | 48 (12.0) | 24.5 ± 5.4 | |
| Education | |||
| • Registered Nurse | 28 (7.0) | 24.6 ± 5.7 | F = 0.65 p = 0.52 |
| • Bachelor in Nursing | 132 (33.0) | 26.0 ± 5.9 | |
| • Master of Science in Nursing | 240 (60.0) | 25.8 ± 5.7 | |
| Specialization in “Anesthesiology nursing and intensive care” | |||
| • Yes | 176 (44.0) | 25.6 ± 6.1 | t = 0.47 p = 0.64 |
| • No | 224 (56.0) | 25.9 ± 5.6 | |
| Type of ward | |||
| • Department of Anaesthesiology and Intensive Care (adults) | 252 (63.0) | 25.4 ± 6.0 | F = 1.46 p = 0.21 |
| • Intensive Cardiac Surveillance Unit (including Cardiac Surgery) | 64 (16.0) | 27.1 ± 5.1 | |
| • Post-Operative Intensive Care Unit | 32 (8.0) | 26.2 ± 4.3 | |
| • Neurological Intensive Care Unit (including Neurosurgery) | 25 (6.2) | 26.9 ± 6.5 | |
| • Department of Anesthesiology and Pediatric Intensive Care | 27 (6.7) | 24.8 ± 5.9 | |
| The structure of ward | |||
| • Open | 137 (34.2) | 27.3 ± 6.2 | F = 2.26 p = 0.10 |
| • Close | 104 (26.0) | 25.9 ± 5.9 | |
| • Mixed | 159 (39.7) | 26.3 ± 5.4 | |
| Shift length | |||
| • 8 h shifts | 19 (4.7) | 25.3 ± 6.5 | F = 2.42 p = 0.09 |
| • 12 h shifts | 307 (76.7) | 26.1 ± 5.6 | |
| • 24 h shifts | 74 (18.5) | 24.5 ± 6.4 | |
| The ward has alarm management systems for monitoring devices | |||
| • Yes | 317 (79.2) | 25.6 ± 5.7 | t = −1.54 p = 0.12 |
| • No | 83 (20.8) | 26.7 ± 6.2 | |
| Participation in training programs related to use of monitoring devices available in the ward | |||
| • Regularly | 60 (15.0) | 23.8 ± 5.3 | F = 10.93 p = 0.00002 Post-hoc test: Regularly vs. No p = 0.0007 Once vs. No p = 0.0002 |
| • No | 183 (45.7) | 27.2 ± 5.9 | |
| • Once | 157 (39.2) | 24.9 ± 5.4 |
| Factors | Simple Regression ß (95% CI) | Multiple Regression ß (95% Cl) | Partial R2 |
|---|---|---|---|
| Participation in training programs related to use of monitoring devices available in the ward—regularly reference category: No | −0.14 (−0.24 to −0.04) * | −0.21 (−0.31 to −0.11) ** | 0.04 |
| Participation in training programs related to use of monitoring devices available in the ward—once reference category: No | −0.12 (−0.22 to −0.02) * | −0.17 (−0.27 to −0.07) ** | 0.03 |
| Intensive Cardiac Surveillance Unit—including Cardiac Surgery reference category: other ICU | 0.10 (0.005 to 0.20) | 0.10 (0.009 to 0.20) * | 0.01 |
| 12-h shifts reference category: 8 and 24-h shifts | 0.11 (0.01 to 0.20) * | 0.11 (0.02 to 0.21) * | 0.01 |
| 24-h shifts reference category: 8 and 12-h shifts | −0.10 (−0.20 to −0.007) | Model: R2 = 0.06; F (4,395) = 7.82; p = 0.000004 | |
| The structure of ward—open reference category: closed and mixed | 0.10 (−0.006 to 0.20) | ||
| Department of Anaesthesiology and Intensive Care (adults) reference category: other ICU | −0.09 (−0.19 to 0.005) | ||
| Female gender reference category: male | 0.10 (−0.01 to 0.19) | ||
Disclaimer/Publisher’s Note: The statements, opinions and data contained in all publications are solely those of the individual author(s) and contributor(s) and not of MDPI and/or the editor(s). MDPI and/or the editor(s) disclaim responsibility for any injury to people or property resulting from any ideas, methods, instructions or products referred to in the content. |
© 2023 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Lewandowska, K.; Mędrzycka-Dąbrowska, W.; Tomaszek, L.; Wujtewicz, M. Determining Factors of Alarm Fatigue among Nurses in Intensive Care Units—A Polish Pilot Study. J. Clin. Med. 2023, 12, 3120. https://doi.org/10.3390/jcm12093120
Lewandowska K, Mędrzycka-Dąbrowska W, Tomaszek L, Wujtewicz M. Determining Factors of Alarm Fatigue among Nurses in Intensive Care Units—A Polish Pilot Study. Journal of Clinical Medicine. 2023; 12(9):3120. https://doi.org/10.3390/jcm12093120
Chicago/Turabian StyleLewandowska, Katarzyna, Wioletta Mędrzycka-Dąbrowska, Lucyna Tomaszek, and Magdalena Wujtewicz. 2023. "Determining Factors of Alarm Fatigue among Nurses in Intensive Care Units—A Polish Pilot Study" Journal of Clinical Medicine 12, no. 9: 3120. https://doi.org/10.3390/jcm12093120
APA StyleLewandowska, K., Mędrzycka-Dąbrowska, W., Tomaszek, L., & Wujtewicz, M. (2023). Determining Factors of Alarm Fatigue among Nurses in Intensive Care Units—A Polish Pilot Study. Journal of Clinical Medicine, 12(9), 3120. https://doi.org/10.3390/jcm12093120








