Augmentation-Mastopexy: Analysis of 95 Consecutive Patients and Critical Appraisal of the Procedure
Abstract
:1. Introduction
2. Materials and Methods
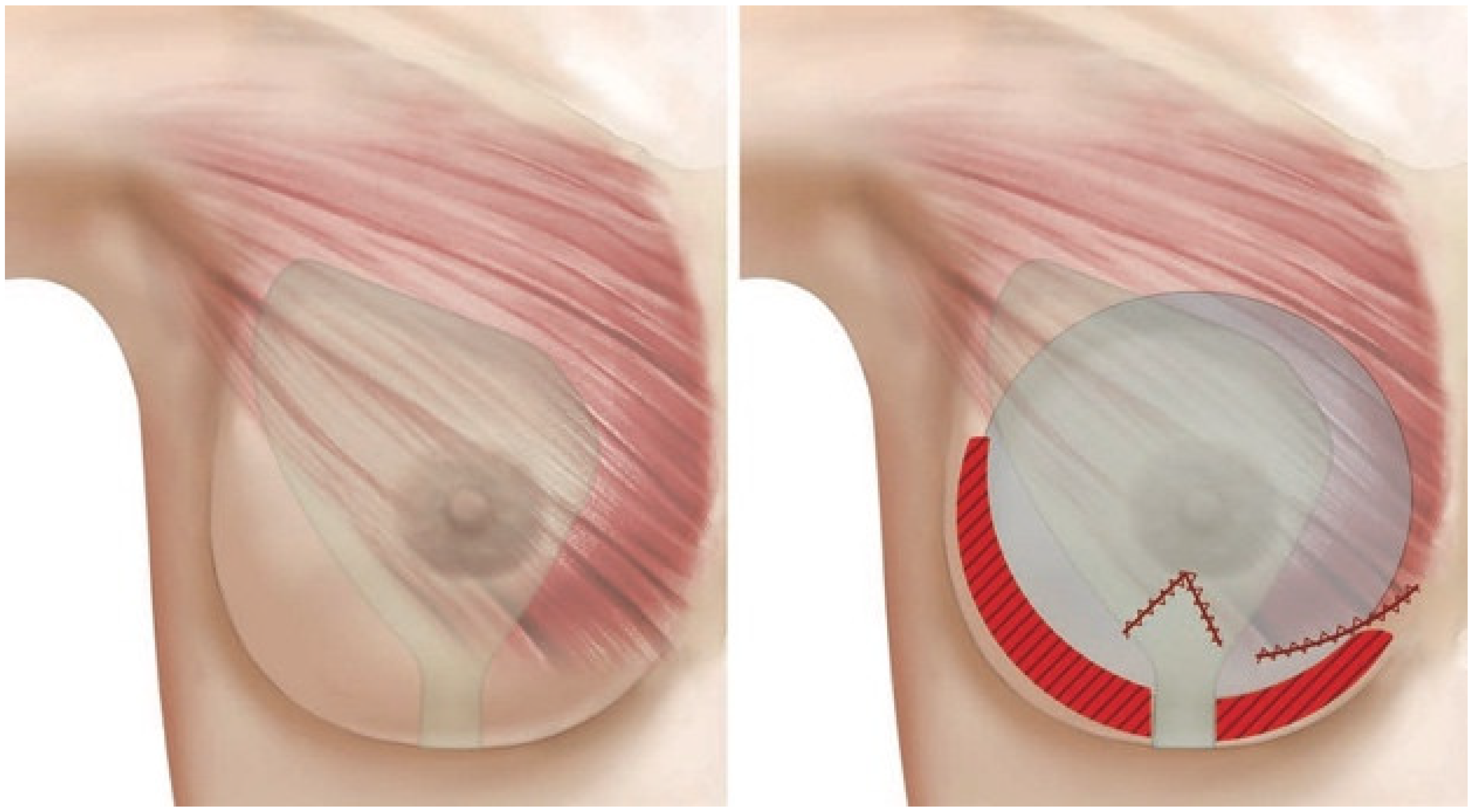
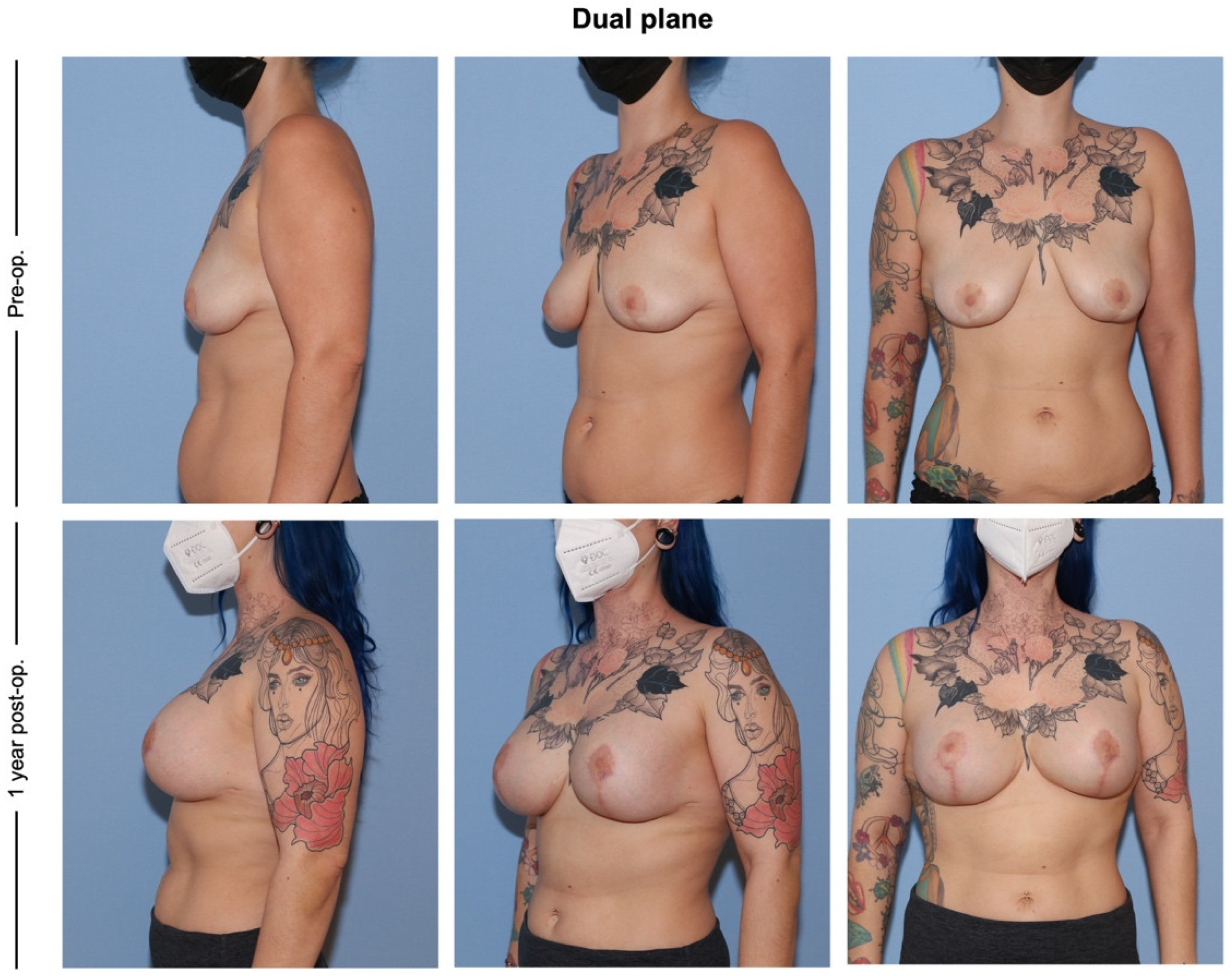
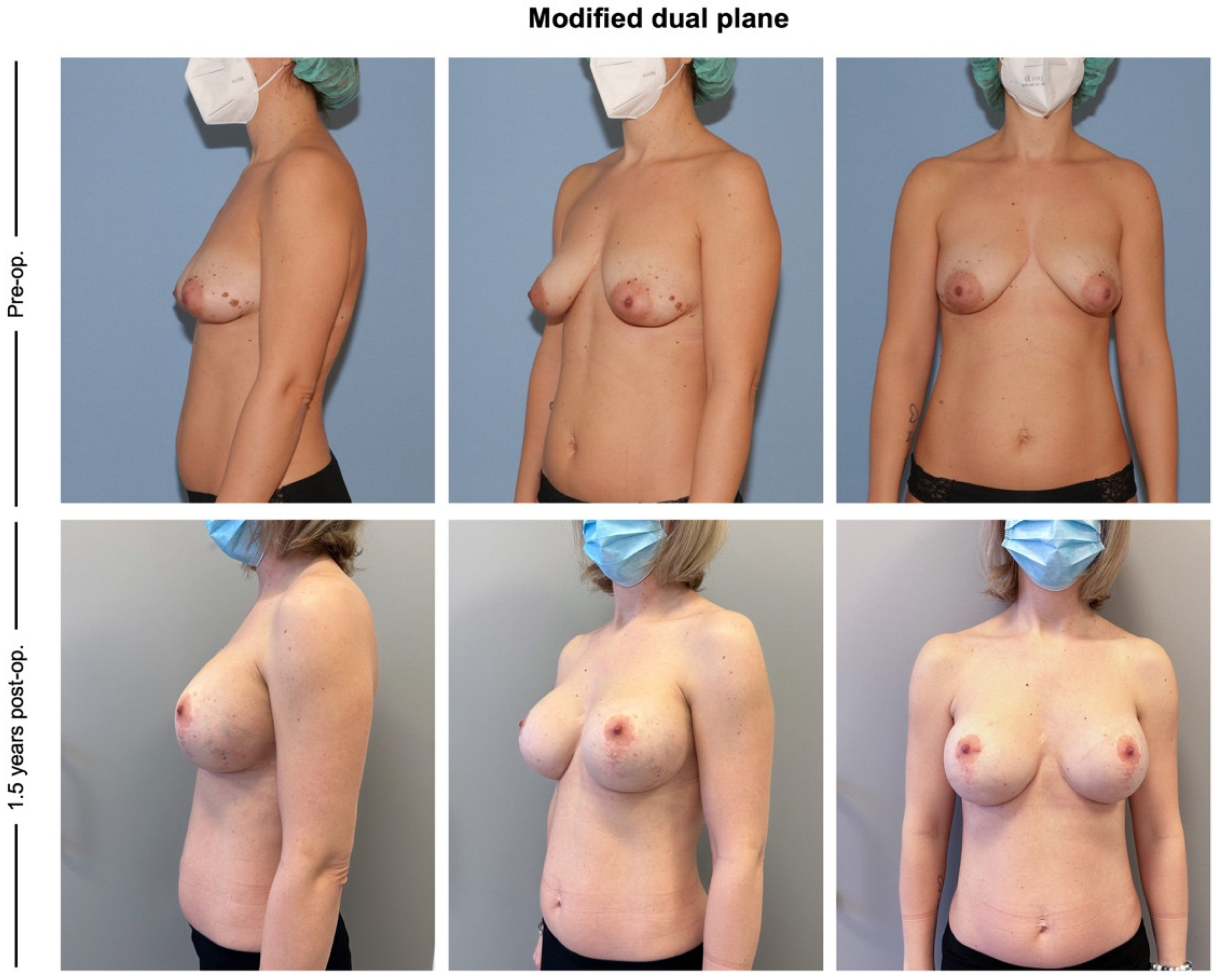
2.1. Surgical Technique Modified Dual Plane
2.2. Study Outcomes
2.3. Data Analysis
3. Results
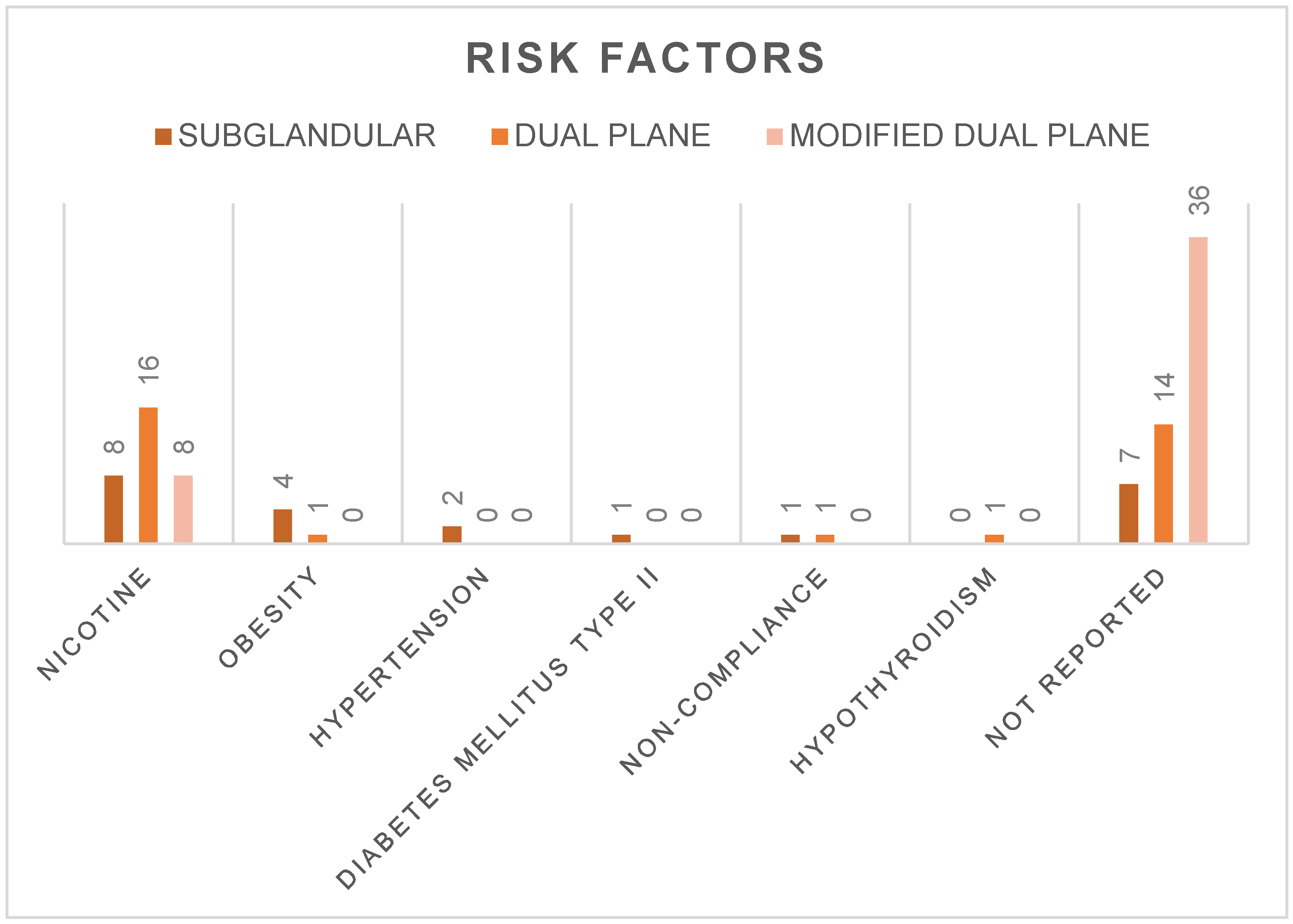
3.1. Demographics
3.2. Surgical Approaches and Hospitalization
3.3. Complications
4. Discussion
5. Conclusions
Supplementary Materials
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Conflicts of Interest
References
- Ikander, P.; Sørensen, J.A.; Thomsen, J.B. Mastopexy with Autologous Augmentation in Women After Massive Weight Loss: A Randomized Clinical Trial. Aesthet. Plast. Surg. 2021, 45, 127–134. [Google Scholar] [CrossRef] [PubMed]
- Stevens, W.G.; Macias, L.H.; Spring, M.; Stoker, D.A.; Chacón, C.O.; Eberlin, S.A. One-Stage Augmentation Mastopexy: A Review of 1192 Simultaneous Breast Augmentation and Mastopexy Procedures in 615 Consecutive Patients. Aesthet. Surg. J. 2014, 34, 723–732. [Google Scholar] [CrossRef] [PubMed]
- Di Summa, P.G.; Oranges, C.M.; Watfa, W.; Sapino, G.; Keller, N.; Tay, S.K.; Chew, B.K.; Schaefer, D.J.; Raffoul, W. Systematic review of outcomes and complications in nonimplant-based mastopexy surgery. J. Plast. Reconstr. Aesthet. Surg. 2019, 72, 243–272. [Google Scholar] [CrossRef] [PubMed]
- Gentile, P. Breast Silicone Gel Implants versus Autologous Fat Grafting: Biomaterials and Bioactive Materials in Comparison. J. Clin. Med. 2021, 10, 3310. [Google Scholar] [CrossRef] [PubMed]
- Qureshi, A.A.; Myckatyn, T.M.; Tenenbaum, M.M. Mastopexy and Mastopexy-Augmentation. Aesthet. Surg. J. 2018, 38, 374–384. [Google Scholar] [CrossRef]
- Pferdehirt, R.; Nahabedian, M.Y. Finesse in Mastopexy and Augmentation Mastopexy. Plast. Reconstr. Surg. 2021, 148, 451e–461e. [Google Scholar] [CrossRef]
- Gentile, P. Tuberous Breast, Deformities, and Asymmetries: A Retrospective Analysis Comparing Fat Grafting Versus Mastopexy and Breast Implants. Aesthet. Plast. Surg. 2022. online ahead of print. [Google Scholar] [CrossRef]
- Tebbetts, J.B. Dual plane breast augmentation: Optimizing implant-soft-tissue relationships in a wide range of breast types. Plast. Reconstr. Surg. 2001, 107, 1255–1272. [Google Scholar] [CrossRef]
- Huemer, G.M.; Wenny, R.; Aitzetmüller, M.M.; Duscher, D. Motiva Ergonomix Round SilkSurface Silicone Breast Implants: Outcome Analysis of 100 Primary Breast Augmentations over 3 Years and Technical Considerations. Plast. Reconstr. Surg. 2018, 141, 831e–842e. [Google Scholar] [CrossRef]
- Ebner, F.K.; Friedl, T.W.; Degregorio, N.; Reich, A.; Janni, W.; Rempen, A. Does Non-Placement of a Drain in Breast Surgery Increase the Rate of Complications and Revisions? Geburtshilfe Frauenheilkd. 2013, 73, 1128–1134. [Google Scholar] [CrossRef]
- Xiao, Y.; Hu, J.; Zhang, M.; Zhang, W.; Qin, F.; Zeng, A.; Wang, X.; Liu, Z.; Zhu, L.; Yu, N.; et al. To use indwelling drainage or not in dual-plane breast augmentation mammoplasty patients: A comparative study. Medicine 2020, 99, e21305. [Google Scholar] [CrossRef]
- Khan, S.M.; Smeulders, M.J.; Van der Horst, C.M. Wound drainage after plastic and reconstructive surgery of the breast. Cochrane Database Syst. Rev. 2015, 2015, CD007258. [Google Scholar] [CrossRef]
- Charles-de-Sá, L.; Gontijo-de-Amorim, N.F.; Rossi, J.K.; Messeder, A.; Jorge, L.N.A.; da Mota, D.S.C.; Aboudib, J.H. Drainage on augmentation mammoplasty: Does it work? J. Plast. Reconstr. Aesthet. Surg. 2021, 74, 1093–1100. [Google Scholar] [CrossRef]
- Ross, G.L. One stage mastopexy augmentation in the ptotic patient. The superiorly based dermal flap for autologous reinforcement of the inferior pole. J. Plast. Reconstr. Aesthet. Surg. 2015, 68, 1248–1254. [Google Scholar] [CrossRef]
- Watfa, W.; Zaugg, P.; Baudoin, J.; Bramhall, R.J.; Raffoul, W.; di Summa, P.G. Dermal Triangular Flaps to Prevent Pseudoptosis in Mastopexy Surgery: The Hammock Technique. Plast. Reconstr. Surg. Glob. Open 2019, 7, e2473. [Google Scholar] [CrossRef]
- Shridharani, S.M.; Bellamy, J.L.; Mofid, M.M.; Singh, N.K. Breast augmentation. Eplasty 2013, 13, ic46. [Google Scholar]
- Li, S.; Mu, D.; Liu, C.; Xin, M.; Fu, S.; Xu, B.; Li, Z.; Qi, J.; Luan, J. Complications Following Subpectoral Versus Prepectoral Breast Augmentation: A Meta-analysis. Aesthet. Plast. Surg. 2019, 43, 890–898. [Google Scholar] [CrossRef]
- Spear, S.L.; Carter, M.E.; Ganz, J.C. The correction of capsular contracture by conversion to “dual-plane” positioning: Technique and outcomes. Plast. Reconstr. Surg. 2006, 118, 103S–113S; discussion 114S. [Google Scholar] [CrossRef]
- Spear, S.L.; Low, M.; Ducic, I. Revision augmentation mastopexy: Indications, operations, and outcomes. Ann. Plast. Surg. 2003, 51, 540–546. [Google Scholar] [CrossRef]
- Mallucci, P.; Branford, O.A. Reply: Design for Natural Breast Augmentation: The ICE Principle. Plast. Reconstr. Surg. 2017, 139, 801e–802e. [Google Scholar] [CrossRef]
- Tebbetts, J.B. The greatest myths in breast augmentation. Plast. Reconstr. Surg. 2001, 107, 1895–1903. [Google Scholar] [CrossRef] [PubMed]
- Swanson, E. Underestimating Implant Volumes in Cosmetic Breast Augmentation. Plast. Reconstr. Surg. Glob. Open 2017, 5, e1483. [Google Scholar] [CrossRef] [PubMed]
- Swanson, E. Prospective comparative clinical evaluation of 784 consecutive cases of breast augmentation and vertical mammaplasty, performed individually and in combination. Plast. Reconstr. Surg. 2013, 132, 30e–45e. [Google Scholar] [CrossRef] [PubMed]
- Huang, G.J.; Wichmann, J.L.; Mills, D.C. Transaxillary subpectoral augmentation mammaplasty: A single surgeon’s 20-year experience. Aesthet. Surg. J. 2011, 31, 781–801. [Google Scholar] [CrossRef]
- Jackson, T.D.; Wannares, J.J.; Lancaster, R.T.; Rattner, D.W.; Hutter, M.M. Does speed matter? The impact of operative time on outcome in laparoscopic surgery. Surg. Endosc. 2011, 25, 2288–2295. [Google Scholar] [CrossRef]
- Cheng, H.; Chen, B.P.; Soleas, I.M.; Ferko, N.C.; Cameron, C.G.; Hinoul, P. Prolonged Operative Duration Increases Risk of Surgical Site Infections: A Systematic Review. Surg. Infect. 2017, 18, 722–735. [Google Scholar] [CrossRef]
- Khavanin, N.; Jordan, S.W.; Rambachan, A.; Kim, J.Y. A systematic review of single-stage augmentation-mastopexy. Plast. Reconstr. Surg. 2014, 134, 922–931. [Google Scholar] [CrossRef]
- Cárdenas-Camarena, L.; Ramírez-Macías, R.; International Confederation for Plastic Reconstructive and Aesthetic Surgery; International Society of Aesthetic Plastic Surgery; Iberolatinoamerican Plastic Surgery Federation; Mexican Association of Plastic Esthetic and Reconstructive Surgery; Western Mexican Association of Plastic, Esthetic and Reconstructive Surgery; Jalisco College of Plastic Surgeons. Augmentation/mastopexy: How to select and perform the proper technique. Aesthet. Plast. Surg. 2006, 30, 21–33. [Google Scholar] [CrossRef]
- Swanson, E. All Seasons Vertical Augmentation Mastopexy: A Simple Algorithm, Clinical Experience, and Patient-reported Outcomes. Plast. Reconstr. Surg. Glob. Open 2016, 4, e1170. [Google Scholar] [CrossRef]
- Coombs, D.M.; Srivastava, U.; Amar, D.; Rubin, J.P.; Gusenoff, J.A. The Challenges of Augmentation Mastopexy in the Massive Weight Loss Patient: Technical Considerations. Plast. Reconstr. Surg. 2017, 139, 1090–1099. [Google Scholar] [CrossRef]
- Benotti, P.; Wood, G.C.; Still, C.; Petrick, A.; Strodel, W. Obesity disease burden and surgical risk. Surg. Obes. Relat. Dis. 2006, 2, 600–606. [Google Scholar] [CrossRef]
- Wilson, J.A.; Clark, J.J. Obesity: Impediment to postsurgical wound healing. Adv. Skin. Wound Care 2004, 17, 426–435. [Google Scholar] [CrossRef]
- Pierpont, Y.N.; Dinh, T.P.; Salas, R.E.; Johnson, E.L.; Wright, T.G.; Robson, M.C.; Payne, W.G. Obesity and surgical wound healing: A current review. ISRN Obes. 2014, 2014, 638936. [Google Scholar] [CrossRef]
- Panayi, A.C.; Agha, R.A.; Sieber, B.A.; Orgill, D.P. Impact of Obesity on Outcomes in Breast Reconstruction: A Systematic Review and Meta-Analysis. J. Reconstr. Microsurg. 2018, 34, 363–375. [Google Scholar] [CrossRef]
- Larsen, O.A.; Lassen, N.A.; Quaade, F. Blood flow through human adipose tissue determined with radioactive xenon. Acta Physiol. Scand. 1966, 66, 337–345. [Google Scholar] [CrossRef]
- West, D.B.; Prinz, W.A.; Francendese, A.A.; Greenwood, M.R. Adipocyte blood flow is decreased in obese Zucker rats. Am. J. Physiol. 1987, 253, R228–R233. [Google Scholar] [CrossRef]
- Crandall, D.L.; Goldstein, B.M.; Huggins, F.; Cervoni, P. Adipocyte blood flow: Influence of age, anatomic location, and dietary manipulation. Am. J. Physiol. 1984, 247, R46–R51. [Google Scholar] [CrossRef]
- Ye, J.; Gao, Z.; Yin, J.; He, Q. Hypoxia is a potential risk factor for chronic inflammation and adiponectin reduction in adipose tissue of ob/ob and dietary obese mice. Am. J. Physiol. Endocrinol. Metab. 2007, 293, E1118–E1128. [Google Scholar] [CrossRef]
- Hosogai, N.; Fukuhara, A.; Oshima, K.; Miyata, Y.; Tanaka, S.; Segawa, K.; Furukawa, S.; Tochino, Y.; Komuro, R.; Matsuda, M.; et al. Adipose tissue hypoxia in obesity and its impact on adipocytokine dysregulation. Diabetes 2007, 56, 901–911. [Google Scholar] [CrossRef]
- Trayhurn, P.; Wood, I.S. Adipokines: Inflammation and the pleiotropic role of white adipose tissue. Br. J. Nutr. 2004, 92, 347–355. [Google Scholar] [CrossRef]
- Kaidar-Person, O.; Person, B.; Szomstein, S.; Rosenthal, R.J. Nutritional deficiencies in morbidly obese patients: A new form of malnutrition? Part A: Vitamins. Obes. Surg. 2008, 18, 870–876. [Google Scholar] [CrossRef] [PubMed]
- O’Brien, K.F.; Maiman, R.E.; DeWitt, C.A. Multiple Nutritional Deficiencies in a Morbidly Obese Patient. Am. J. Gastroenterol. 2019, 114, 11. [Google Scholar] [CrossRef] [PubMed]
- Russell, L. The importance of patients’ nutritional status in wound healing. Br. J. Nurs. 2001, 10, S42, S44–S49. [Google Scholar] [CrossRef]
- Anderson, B. Nutrition and wound healing: The necessity of assessment. Br. J. Nurs. 2005, 14, S30, S32, S34. [Google Scholar] [CrossRef] [PubMed]
- Hadad, E.; Klein, D.; Seligman, Y.; Wiser, I.; Heller, L. Sub-muscular plane for augmentation mammoplasty patients increases silicone gel implant rupture rate. J. Plast. Reconstr. Aesthet. Surg. 2019, 72, 419–423. [Google Scholar] [CrossRef]
- Zoumaras, J.; Lawrence, J. Inverted-T versus vertical scar breast reduction: One surgeon’s 5-year experience with consecutive patients. Aesthet. Surg. J. 2008, 28, 521–526. [Google Scholar] [CrossRef]

| Group (I–III): | I (Subglandular) | II (Dual Plane) | III (Modified Dual Plane) |
|---|---|---|---|
| No. (%) | 19 (20) | 32 (34) | 44 (46) |
| Patient Data (Mean ± SD) | Group I | Group II | Group III | p-Value |
|---|---|---|---|---|
| Age | 33.0 ± 12.2 | 32.8 ± 9.2 | 36.1 ± 9.4 | 0.29 |
| BMI | 26.2 ± 4.2 | 23.0 ± 3.0 | 23.5 ± 1.9 | <0.01 |
| Weight | 72.2 ± 11.8 | 64.3 ± 9.4 | 64.5 ± 5.5 | <0.01 |
| Incisional Techniques, No. (%) | Group I | Group II | Group III |
|---|---|---|---|
| Periareolar | 0 (0.0) | 6 (18.8) | 0 (0.0) |
| Circumvertical | 6 (31.6) | 16 (50.0) | 36 (81.8) |
| Inverted T | 13 (68.4) | 10 (31.3) | 8 (18.2) |
| Implant Type, No. (%) | Group I | Group II | Group III |
|---|---|---|---|
| Polytech® | 3 (15.8) | 5 (15.6) | 9 (20.5) |
| Mentor® | 11 (57.9) | 12 (37.5) | 5 (11.4) |
| Eurosilicone® | 5 (26.3) | 15 (46.9) | 0 (0.0) |
| Motiva® | 0 (0.0) | 0 (0.0) | 18 (40.9) |
| Allergan® | 0 (0.0) | 0 (0.0) | 4 (9.1) |
| Sebbin® | 0 (0.0) | 0 (0.0) | 7 (15.9) |
| Unknown | 0 (0.0) | 0 (0.0) | 1 (2.3) |
| Total | 19 | 32 | 44 |
| Complications, No. (%): | Group I | Group II | Group III | ORIII vs. I (95% CI) | ORIII vs. II (95% CI) |
|---|---|---|---|---|---|
| Patients with complications | 12 (63.2) | 15 (46.9) | 10 (22.7) | 0.09 (0.01–0.90) | 0.15 (0.02–1.25) |
| Revisions | 8 (42.1) | 10 (31.3) | 2 (4.5) | 0.05 (0.01–0.42) | 0.09 (0.01–0.72) |
| Implant loss/change | 7 (36.8) | 6 (18.8) | 0 (0.0) | 0.02 (0.00–0.35) * | 0.05 (0.00–0.85) * |
| Complication, No. (%) | Group I | Group II | Group III | ORIII vs. I (95% CI) | ORIII vs. II (95% CI) |
|---|---|---|---|---|---|
| Wound dehiscence | 8 (42.1) | 5 (15.6) | 5 (11.4) | 0.05 (0.00–1.15) | 0.29 (0.02–4.98) |
| Wound infection | 5 (26.3) | 3 (9.4) | 2 (4.5) | 0.33 (0.03–3.54) | 1.31 (0.12–14.90) |
| Hematoma | 2 (10.5) | 1 (3.1) | 1 (2.3) | 0.23 (0.01–4.91) | 0.98 (0.03–33.43) |
| Seroma | 1 (5.3) | 0 (0.0) | 1 (2.3) | 0.26 (0.00–511.43) | 2.24 (0.09–∞) * |
| Capsular contracture | 1 (5.3) | 3 (9.4) | 0 (0.0) | 0.14 (0.00–3.56) * | 0.09 (0.00–1.90) * |
| Double bubble deformity | 0 (0.0) | 2 (6.3) | 2 (4.5) | 2.29 (0.11–∞) * | 0.47 (0.03–6.91) |
| Dislocation | 2 (10.5) | 3 (9.4) | 1 (2.3) | 0.21 (0.01–4.46) | 0.27 (0.01–4.89) |
| Intense scarring | 2 (10.5) | 3 (9.4) | 0 (0.0) | 0.08 (0.00–1.72) * | 0.09 (0–1.90) * |
| Rupture | 0 (0.0) | 1 (3.1) | 0 (0.0) | 0.44 (0–∞) * | 0.24 (0.00–5.98) |
Disclaimer/Publisher’s Note: The statements, opinions and data contained in all publications are solely those of the individual author(s) and contributor(s) and not of MDPI and/or the editor(s). MDPI and/or the editor(s) disclaim responsibility for any injury to people or property resulting from any ideas, methods, instructions or products referred to in the content. |
© 2023 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Zucal, I.; Tremp, M.; Duscher, D.; Wenny, R.; Zaussinger, M.; Kutz, A.; Pagani, A.; Huemer, G.M. Augmentation-Mastopexy: Analysis of 95 Consecutive Patients and Critical Appraisal of the Procedure. J. Clin. Med. 2023, 12, 3213. https://doi.org/10.3390/jcm12093213
Zucal I, Tremp M, Duscher D, Wenny R, Zaussinger M, Kutz A, Pagani A, Huemer GM. Augmentation-Mastopexy: Analysis of 95 Consecutive Patients and Critical Appraisal of the Procedure. Journal of Clinical Medicine. 2023; 12(9):3213. https://doi.org/10.3390/jcm12093213
Chicago/Turabian StyleZucal, Isabel, Mathias Tremp, Dominik Duscher, Raphael Wenny, Maximilian Zaussinger, Alexander Kutz, Andrea Pagani, and Georg M. Huemer. 2023. "Augmentation-Mastopexy: Analysis of 95 Consecutive Patients and Critical Appraisal of the Procedure" Journal of Clinical Medicine 12, no. 9: 3213. https://doi.org/10.3390/jcm12093213
APA StyleZucal, I., Tremp, M., Duscher, D., Wenny, R., Zaussinger, M., Kutz, A., Pagani, A., & Huemer, G. M. (2023). Augmentation-Mastopexy: Analysis of 95 Consecutive Patients and Critical Appraisal of the Procedure. Journal of Clinical Medicine, 12(9), 3213. https://doi.org/10.3390/jcm12093213







