Obesity, Preserved Ejection Fraction Heart Failure, and Left Ventricular Remodeling
Abstract
1. Introduction
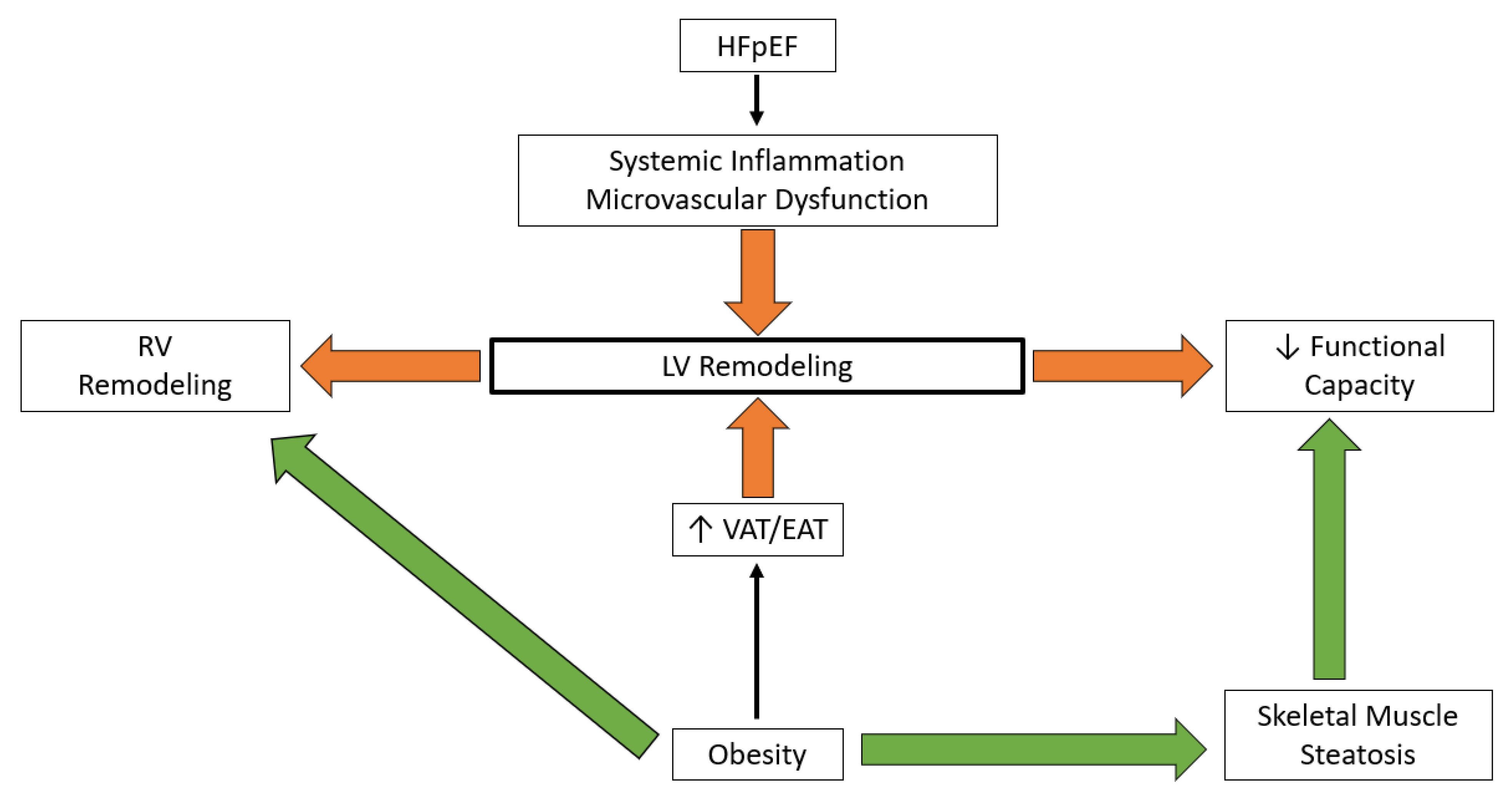
2. Cardiac Remodeling and Functional Capacity
2.1. Preserved Ejection Fraction Heart Failure
2.2. Obesity
3. Inflammation
3.1. Preserved Ejection Fraction Heart Failure
3.2. Obesity
4. Circulation
4.1. Preserved Ejection Fraction Heart Failure
4.1.1. Coronary Artery Disease
4.1.2. Microvasculature
4.1.3. Coronary Vascular Endothelium
4.2. Obesity
4.2.1. Coronary Artery Disease
4.2.2. Microvasculature
4.2.3. Coronary Vascular Endothelium
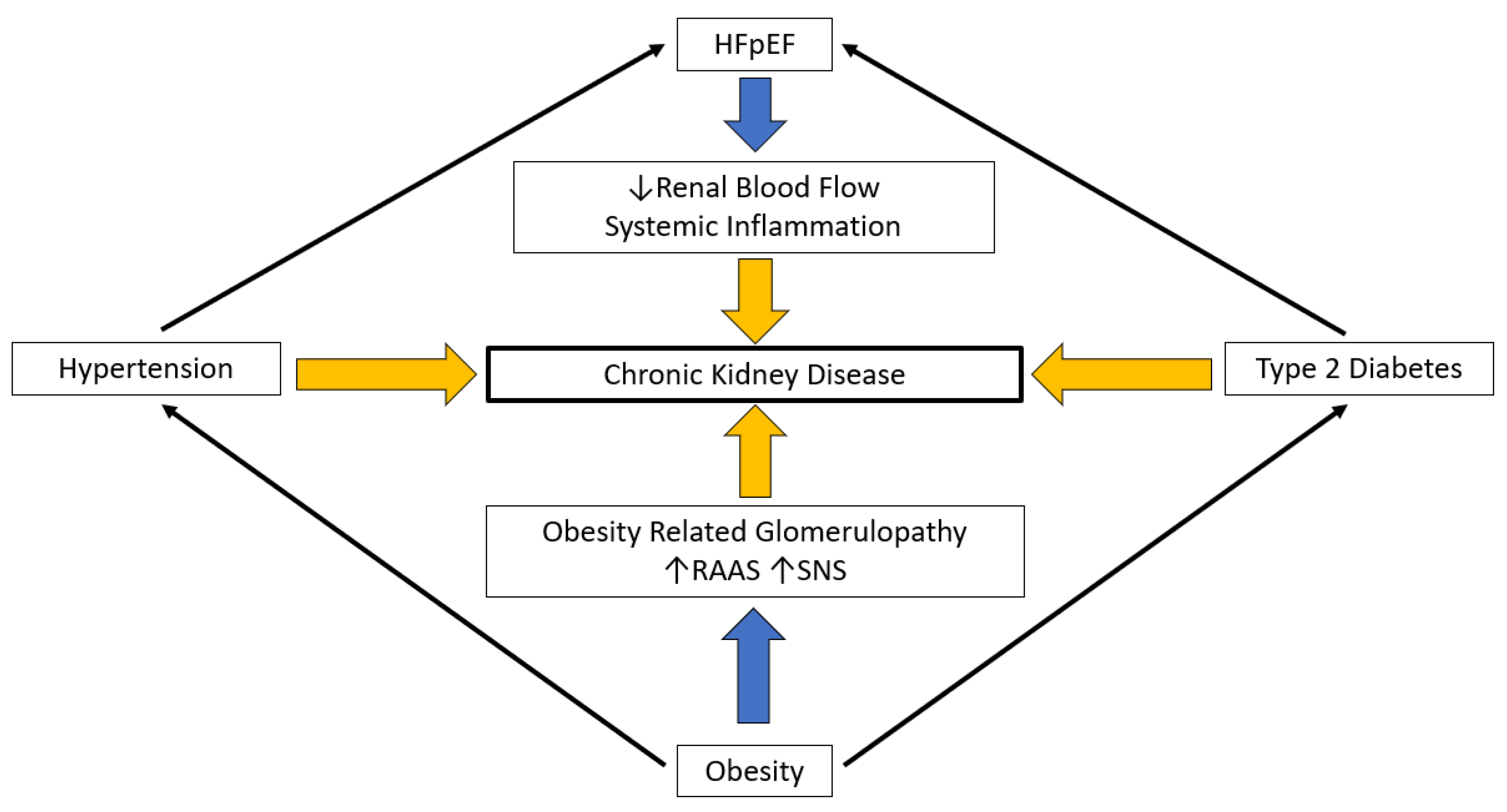
5. Renal Function
5.1. Preserved Ejection Fraction Heart Failure
5.2. Obesity
6. Moving Forward: Metabolic Bariatric Surgery in Patients with Obesity and Preserved Ejection Heart Failure
6.1. Metabolic Bariatric Surgery and Left Ventricular Mass
6.2. Incidence of Heart Failure after Metabolic Bariatric Surgery
7. Selection of Patients for Metabolic Bariatric Surgery
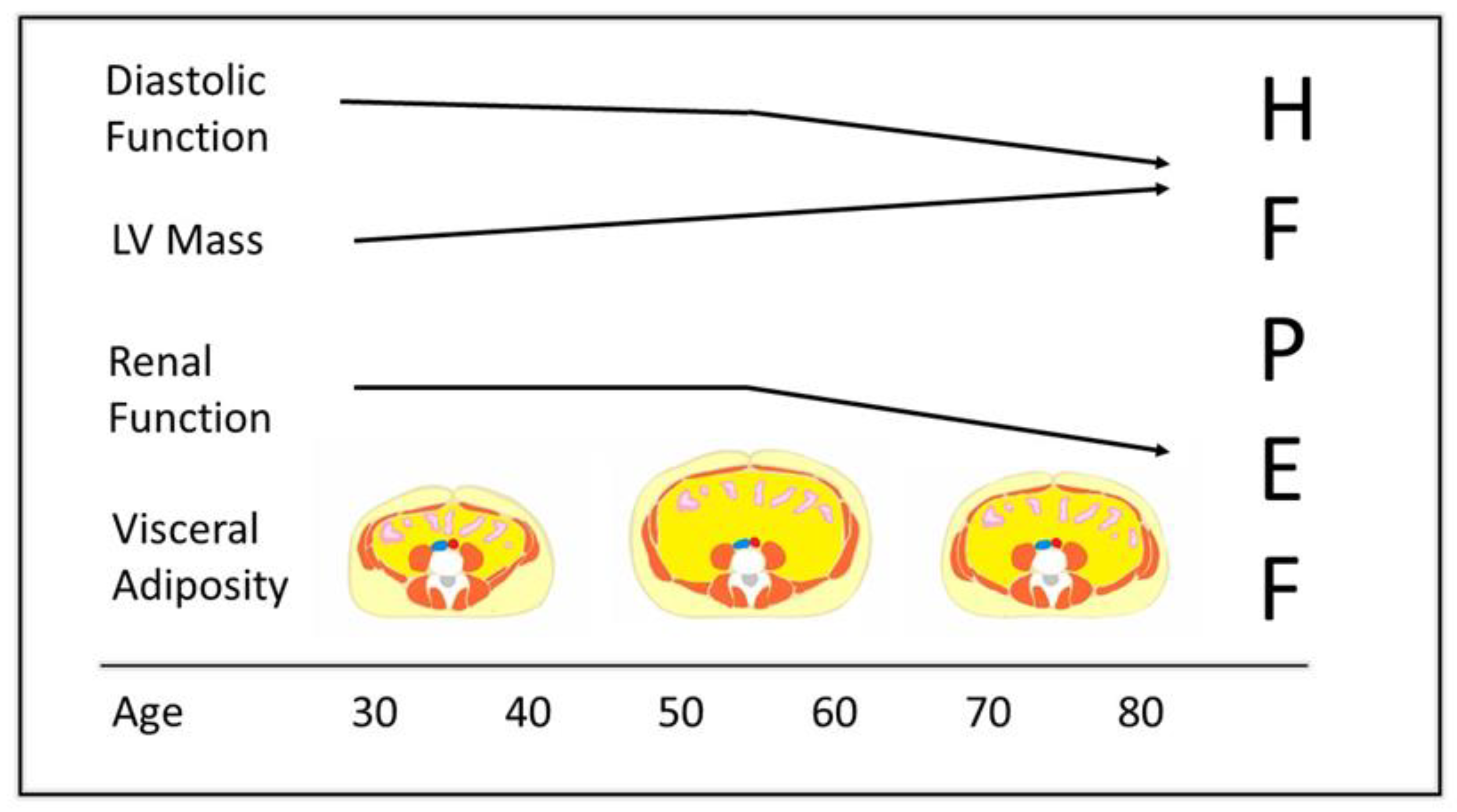
7.1. Duration of Obesity and Preserved Ejection Fraction Heart Failure
7.2. Obesity Exposure, Cardiac Remodeling, and Cardiovascular Outcomes
8. Conclusions
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Conflicts of Interest
References
- Hales, C.M.; Carroll, M.D.; Fryar, C.D.; Ogden, C.L. Prevalence of Obesity and Severe Obesity Among Adults: United States, 2017–2018; CDC National Center for Health Statistics: Hyattsville, MD, USA, 2020; pp. 1–8. [Google Scholar]
- Ward, Z.J.; Bleich, S.N.; Cradock, A.L.; Barrett, J.L.; Giles, C.M.; Flax, C.; Long, M.W.; Gortmaker, S.L. Projected U.S. State-Level Prevalence of Adult Obesity and Severe Obesity. N. Engl. J. Med. 2019, 381, 2440–2450. [Google Scholar] [CrossRef] [PubMed]
- Finkelstein, E.A.; Khavjou, O.A.; Thompson, H.; Trogdon, J.G.; Pan, L.; Sherry, B.; Dietz, W. Obesity and severe obesity forecasts through 2030. Am. J. Prev. Med. 2012, 42, 563–570. [Google Scholar] [CrossRef] [PubMed]
- Doumouras, A.G.; Wong, J.A.; Paterson, J.M.; Lee, Y.; Sivapathasundaram, B.; Tarride, J.-E.; Thabane, L.; Hong, D.; Yusuf, S.; Anvari, M. Bariatric Surgery and Cardiovascular Outcomes in Patients with Obesity and Cardiovascular Disease: A Population-Based Retrospective Cohort Study. Circulation 2021, 143, 1468–1480. [Google Scholar] [CrossRef] [PubMed]
- Redfield, M.M.; Borlaug, B.A.; Lewis, G.D.; Mohammed, S.F.; Semigran, M.J.; LeWinter, M.M.; Deswal, A.; Hernandez, A.F.; Lee, K.L.; Braunwald, E.; et al. PhosphdiesteRasE-5 Inhibition to Improve CLinical Status and EXercise Capacity in Diastolic Heart Failure (RELAX) trial: Rationale and design. Circ. Heart Fail. 2012, 5, 653–659. [Google Scholar] [CrossRef] [PubMed]
- Redfield, M.M.; Anstrom, K.J.; Levine, J.A.; Koepp, G.A.; Borlaug, B.A.; Chen, H.H.; LeWinter, M.M.; Joseph, S.M.; Shah, S.J.; Semigran, M.J.; et al. Isosorbide Mononitrate in Heart Failure with Preserved Ejection Fraction. N. Engl. J. Med. 2015, 373, 2314–2324. [Google Scholar] [CrossRef] [PubMed]
- Borlaug, B.A.; Anstrom, K.J.; Lewis, G.D.; Shah, S.J.; Levine, J.A.; Koepp, G.A.; Givertz, M.M.; Felker, G.M.; LeWinter, M.M.; Mann, D.L.; et al. Effect of Inorganic Nitrite vs Placebo on Exercise Capacity Among Patients With Heart Failure With Preserved Ejection Fraction: The INDIE-HFpEF Randomized Clinical Trial. JAMA 2018, 320, 1764–1773. [Google Scholar] [CrossRef] [PubMed]
- Solomon, S.D.; McMurray, J.J.; Claggett, B.; de Boer, R.A.; DeMets, D.; Hernandez, A.F.; Inzucchi, S.E.; Kosiborod, M.N.; Lam, C.S.; Martinez, F.; et al. Dapagliflozin in Heart Failure with Mildly Reduced or Preserved Ejection Fraction. N. Engl. J. Med. 2022, 387, 1089–1098. [Google Scholar] [CrossRef] [PubMed]
- Anker, S.D.; Butler, J.; Filippatos, G.; Ferreira, J.P.; Bocchi, E.; Böhm, M.; Brunner–La Rocca, H.-P.; Choi, D.-J.; Chopra, V.; Chuquiure-Valenzuela, E.; et al. Empagliflozin in Heart Failure with a Preserved Ejection Fraction. N. Engl. J. Med. 2021, 385, 1451–1461. [Google Scholar] [CrossRef]
- Cleland, J.G.; Tendera, M.; Adamus, J.; Freemantle, N.; Polonski, L.; Taylor, J. The perindopril in elderly people with chronic heart failure (PEP-CHF) study. Eur. Heart J. 2006, 27, 2338–2345. [Google Scholar] [CrossRef]
- Pitt, B.; Pfeffer, M.A.; Assmann, S.F.; Boineau, R.; Anand, I.S.; Claggett, B.; Clausell, N.; Desai, A.S.; Diaz, R.; Fleg, J.L.; et al. Spironolactone for heart failure with preserved ejection fraction. N. Engl. J. Med. 2014, 370, 1383–1392. [Google Scholar] [CrossRef]
- Solomon, S.D.; McMurray, J.J.V.; Anand, I.S.; Junbo Ge, D.P.; Lam, C.S.P.; Maggioni, A.P.; Martinez, F.; Packer, M.; Pfeffer, M.A.; Pieske, B.; et al. Angiotensin–Neprilysin Inhibition in Heart Failure with Preserved Ejection Fraction. N. Engl. J. Med. 2019, 381, 1609–1620. [Google Scholar] [CrossRef] [PubMed]
- Van Tassell, B.W.; Trankle, C.R.; Canada, J.M.; Carbone, S.; Buckley, L.; Kadariya, D.; Del Buono, M.G.; Billingsley, H.; Wohlford, G.; Viscusi, M.; et al. IL-1 Blockade in Patients with Heart Failure with Preserved Ejection Fraction. Circ. Heart Fail. 2018, 11, e005036. [Google Scholar] [CrossRef] [PubMed]
- Massie, B.M.; Carson, P.E.; McMurray, J.J.; Komajda, M.; McKelvie, R.; Zile, M.R.; Anderson, S.; Donovan, M.; Iverson, E.; Staiger, C.; et al. Irbesartan in patients with heart failure and preserved ejection fraction. N. Engl. J. Med. 2008, 359, 2456–2467. [Google Scholar] [CrossRef] [PubMed]
- Pieske, B.; Maggioni, A.P.; Lam, C.S.; Pieske-Kraigher, E.; Filippatos, G.; Butler, J.; Ponikowski, P.; Shah, S.; Solomon, S.D.; Scalise, A.-V.; et al. Vericiguat in patients with worsening chronic heart failure and preserved ejection fraction: Results of the SOluble guanylate Cyclase stimulatoR in heArT failurE patientS with PRESERVED EF (SOCRATES-PRESERVED) study. Eur. Heart J. 2017, 38, 1119–1127. [Google Scholar] [CrossRef] [PubMed]
- Solomon, S.D.; Janardhanan, R.; Verma, A.; Bourgoun, M.; Daley, W.L.; Purkayastha, D.; Lacourcière, Y.; E Hippler, S.; Fields, H.; Naqvi, T.Z.; et al. Effect of angiotensin receptor blockade and antihypertensive drugs on diastolic function in patients with hypertension and diastolic dysfunction: A randomised trial. Lancet 2007, 369, 2079–2087. [Google Scholar] [CrossRef] [PubMed]
- Stavrakis, S.; Elkholey, K.; Morris, L.; Niewiadomska, M.; Asad, Z.U.A.; Humphrey, M.B. Neuromodulation of Inflammation to Treat Heart Failure with Preserved Ejection Fraction: A Pilot Randomized Clinical Trial. J. Am. Heart Assoc. 2022, 11, e023582. [Google Scholar] [CrossRef] [PubMed]
- Kitzman, D.W.; Brubaker, P.H.; Morgan, T.M.; Haykowsky, M.J.; Hundley, G.; Kraus, W.E.; Eggebeen, J.; Nicklas, B.J. Effect of Caloric Restriction or Aerobic Exercise Training on Peak Oxygen Consumption and Quality of Life in Obese Older Patients with Heart Failure with Preserved Ejection Fraction. JAMA 2016, 315, 36–46. [Google Scholar] [CrossRef]
- Kitzman, D.W.; Nicklas, B.; Kraus, W.E.; Lyles, M.F.; Eggebeen, J.; Morgan, T.M.; Haykowsky, M. Skeletal muscle abnormalities and exercise intolerance in older patients with heart failure and preserved ejection fraction. Am. J. Physiol. Heart Circ. Physiol. 2014, 306, H1364–H1370. [Google Scholar] [CrossRef]
- Kitzman, D.W.; Hundley, W.G.; Brubaker, P.H.; Morgan, T.M.; Moore, J.B.; Stewart, K.P.; Little, W.C. A randomized double-blind trial of enalapril in older patients with heart failure and preserved ejection fraction: Effects on exercise tolerance and arterial distensibility. Circ. Heart Fail. 2010, 3, 477–485. [Google Scholar] [CrossRef]
- Shah, S.J.; A Borlaug, B.; Chung, E.S.; E Cutlip, D.; Debonnaire, P.; Fail, P.S.; Gao, Q.; Hasenfuß, G.; Kahwash, R.; Kaye, D.M.; et al. Atrial shunt device for heart failure with preserved and mildly reduced ejection fraction (REDUCE LAP-HF II): A randomised, multicentre, blinded, sham-controlled trial. Lancet 2022, 399, 1130–1140. [Google Scholar] [CrossRef]
- Borlaug, B.A.; Olson, T.P.; Lam, C.S.; Flood, K.S.; Lerman, A.; Johnson, B.D.; Redfield, M.M. Global cardiovascular reserve dysfunction in heart failure with preserved ejection fraction. J. Am. Coll. Cardiol. 2010, 56, 845–854. [Google Scholar] [CrossRef] [PubMed]
- Reddy, Y.N.; Andersen, M.J.; Obokata, M.; Koepp, K.E.; Kane, G.C.; Melenovsky, V.; Olson, T.P.; Borlaug, B.A. Arterial Stiffening with Exercise in Patients with Heart Failure and Preserved Ejection Fraction. J. Am. Coll. Cardiol. 2017, 70, 136–148. [Google Scholar] [CrossRef] [PubMed]
- Reddy, Y.N.V.; Carter, R.E.; Obokata, M.; Redfield, M.M.; Borlaug, B.A. A Simple, Evidence-Based Approach to Help Guide Diagnosis of Heart Failure with Preserved Ejection Fraction. Circulation 2018, 138, 861–870. [Google Scholar] [CrossRef] [PubMed]
- Reddy, Y.N.V.; Kaye, D.M.; Handoko, M.L.; van de Bovenkamp, A.A.; Tedford, R.J.; Keck, C.; Andersen, M.J.; Sharma, K.; Trivedi, R.K.; Carter, R.E.; et al. Diagnosis of Heart Failure with Preserved Ejection Fraction Among Patients with Unexplained Dyspnea. JAMA Cardiol. 2022, 7, 891–899. [Google Scholar] [CrossRef] [PubMed]
- Reddy, Y.N.; Obokata, M.; Testani, J.M.; Felker, G.M.; Tang, W.W.; Abou-Ezzeddine, O.F.; Sun, J.-L.; Chakrabothy, H.; McNulty, S.; Shah, S.J.; et al. Adverse Renal Response to Decongestion in the Obese Phenotype of Heart Failure with Preserved Ejection Fraction. J. Card. Fail. 2020, 26, 101–107. [Google Scholar] [CrossRef]
- Borlaug, B.A.; Nishimura, R.A.; Sorajja, P.; Lam, C.S.; Redfield, M.M. Exercise hemodynamics enhance diagnosis of early heart failure with preserved ejection fraction. Circ. Heart Fail. 2010, 3, 588–595. [Google Scholar] [CrossRef]
- Sorimachi, H.; Burkhoff, D.; Verbrugge, F.H.; Omote, K.; Obokata, M.; Reddy, Y.N.; Takahashi, N.; Sunagawa, K.; Borlaug, B.A. Obesity, venous capacitance, and venous compliance in heart failure with preserved ejection fraction. Eur. J. Heart Fail. 2021, 23, 1648–1658. [Google Scholar] [CrossRef]
- Obokata, M.; Reddy, Y.; Pislaru, S.; Melenovsky, V.; Borlaug, B.A. Evidence Supporting the Existence of a Distinct Obese Phenotype of Heart Failure with Preserved Ejection Fraction. Circulation 2017, 136, 6–19. [Google Scholar] [CrossRef]
- Haykowsky, M.J.; Brubaker, P.H.; John, J.M.; Stewart, K.P.; Morgan, T.M.; Kitzman, D.W. Determinants of exercise intolerance in elderly heart failure patients with preserved ejection fraction. J. Am. Coll. Cardiol. 2011, 58, 265–274. [Google Scholar] [CrossRef]
- Haykowsky, M.J.; Nicklas, B.J.; Brubaker, P.H.; Hundley, W.G.; Brinkley, T.E.; Upadhya, B.; Becton, J.T.; Nelson, M.D.; Chen, H.; Kitzman, D.W. Regional Adipose Distribution and its Relationship to Exercise Intolerance in Older Obese Patients Who Have Heart Failure with Preserved Ejection Fraction. JACC Heart Fail. 2018, 6, 640–649. [Google Scholar] [CrossRef]
- Dhakal, B.P.; Malhotra, R.; Murphy, R.M.; Pappagianopoulos, P.P.; Baggish, A.L.; Weiner, R.B.; Houstis, N.E.; Eisman, A.S.; Hough, S.S.; Lewis, G.D. Mechanisms of exercise intolerance in heart failure with preserved ejection fraction: The role of abnormal peripheral oxygen extraction. Circ. Heart Fail. 2015, 8, 286–294. [Google Scholar] [CrossRef]
- Borlaug, B.A.; Blair, J.; Bergmann, M.W.; Bugger, H.; Burkhoff, D.; Bruch, L.; Celermajer, D.S.; Claggett, B.; Cleland, J.G.; Cutlip, D.E.; et al. Latent Pulmonary Vascular Disease May Alter the Response to Therapeutic Atrial Shunt Device in Heart Failure. Circulation 2022, 145, 1592–1604. [Google Scholar] [CrossRef] [PubMed]
- Kitzman, D.W.; Brubaker, P.H.; Herrington, D.M.; Morgan, T.M.; Stewart, K.P.; Hundley, W.G.; Abdelhamed, A.; Haykowsky, M.J. Effect of endurance exercise training on endothelial function and arterial stiffness in older patients with heart failure and preserved ejection fraction: A randomized, controlled, single-blind trial. J. Am. Coll. Cardiol. 2013, 62, 584–592. [Google Scholar] [CrossRef] [PubMed]
- Vaishnav, J.; Chasler, J.E.; Lee, Y.J.; Ndumele, C.E.; Hu, J.-R.; Schulman, S.P.; Russell, S.D.; Sharma, K. Highest Obesity Category Associated with Largest Decrease in N-Terminal Pro-B-Type Natriuretic Peptide in Patients Hospitalized with Heart Failure with Preserved Ejection Fraction. J. Am. Heart Assoc. 2020, 9, e015738. [Google Scholar] [CrossRef] [PubMed]
- Harada, T.; Kagami, K.; Kato, T.; Obokata, M. Echocardiography in the diagnostic evaluation and phenotyping of heart failure with preserved ejection fraction. J. Cardiol. 2021, 79, 679–690. [Google Scholar] [CrossRef]
- Harada, T.; Obokata, M. Obesity-Related Heart Failure with Preserved Ejection Fraction: Pathophysiology, Diagnosis, and Potential Therapies. Heart Fail. Clin. 2020, 16, 357–368. [Google Scholar] [CrossRef] [PubMed]
- Haidar, A.; Taegtmeyer, H. Strategies for Imaging Metabolic Remodeling of the Heart in Obesity and Heart Failure. Curr. Cardiol. Rep. 2022, 24, 327–335. [Google Scholar] [CrossRef]
- Li, A.; Zheng, N.; Ding, X. Mitochondrial abnormalities: A hub in metabolic syndrome-related cardiac dysfunction caused by oxidative stress. Heart Fail. Rev. 2022, 27, 1387–1394. [Google Scholar] [CrossRef]
- van Woerden, G.; van Veldhuisen, D.J.; Westenbrink, B.D.; de Boer, R.A.; Rienstra, M.; Gorter, T.M. Connecting epicardial adipose tissue and heart failure with preserved ejection fraction: Mechanisms, management and modern perspectives. Eur. J. Heart Fail. 2022, 24, 2238–2250. [Google Scholar] [CrossRef]
- Elsanhoury, A.; Nelki, V.; Kelle, S.; Van Linthout, S.; Tschöpe, C. Epicardial Fat Expansion in Diabetic and Obese Patients with Heart Failure and Preserved Ejection Fraction—A Specific HFpEF Phenotype. Front. Cardiovasc. Med. 2021, 8, 720690. [Google Scholar] [CrossRef]
- Kasiakogias, A.; Rosei, E.A.; Camafort, M.; Ehret, G.; Faconti, L.; Ferreira, J.P.; Brguljan, J.; Januszewicz, A.; Kahan, T.; Manolis, A.; et al. Hypertension and heart failure with preserved ejection fraction: Position paper by the European Society of Hypertension. J. Hypertens. 2021, 32, 1522–1545. [Google Scholar] [CrossRef] [PubMed]
- Koepp, K.E.; Obokata, M.; Reddy, Y.N.; Olson, T.P.; Borlaug, B.A. Hemodynamic and Functional Impact of Epicardial Adipose Tissue in Heart Failure with Preserved Ejection Fraction. JACC Heart Fail. 2020, 8, 657–666. [Google Scholar] [CrossRef] [PubMed]
- Samuel, T.J.; Kitzman, D.W.; Haykowsky, M.J.; Upadhya, B.; Brubaker, P.; Nelson, M.B.; Hundley, W. Left ventricular diastolic dysfunction and exercise intolerance in obese heart failure with preserved ejection fraction. Am. J. Physiol. Heart Circ. Physiol. 2021, 320, H1535–H1542. [Google Scholar] [CrossRef] [PubMed]
- Gorter, T.M.; van Woerden, G.; Rienstra, M.; Dickinson, M.G.; Hummel, Y.M.; Voors, A.A.; Hoendermis, E.S.; van Veldhuisen, D.J. Epicardial Adipose Tissue and Invasive Hemodynamics in Heart Failure with Preserved Ejection Fraction. JACC Heart Fail. 2020, 8, 667–676. [Google Scholar] [CrossRef] [PubMed]
- Pugliese, N.R.; Paneni, F.; Mazzola, M.; De Biase, N.; Del Punta, L.; Gargani, L.; Mengozzi, A.; Virdis, A.; Nesti, L.; Taddei, S.; et al. Impact of epicardial adipose tissue on cardiovascular haemodynamics, metabolic profile, and prognosis in heart failure. Eur. J. Heart Fail. 2021, 23, 1858–1871. [Google Scholar] [CrossRef]
- Haykowsky, M.J.; Tomczak, C.R.; Scott, J.M.; Paterson, D.I.; Kitzman, D.W. Determinants of exercise intolerance in patients with heart failure and reduced or preserved ejection fraction. J. Appl. Physiol. 2015, 119, 739–744. [Google Scholar] [CrossRef]
- Zamani, P.; Proto, E.A.; Mazurek, J.A.; Prenner, S.B.; Margulies, K.B.; Townsend, R.R.; Kelly, D.P.; Arany, Z.; Poole, D.C.; Wagner, P.D.; et al. Peripheral Determinants of Oxygen Utilization in Heart Failure with Preserved Ejection Fraction: Central Role of Adiposity. JACC Basic Transl. Sci. 2020, 5, 211–225. [Google Scholar] [CrossRef]
- Katz, S.D.; Maskin, C.; Jondeau, G.; Cocke, T.; Berkowitz, R.; LeJemtel, T. Near-maximal fractional oxygen extraction by active skeletal muscle in patients with chronic heart failure. J. Appl. Physiol. 2000, 88, 2138–2142. [Google Scholar] [CrossRef]
- Neeland, I.J.; Gupta, S.; Ayers, C.R.; Turer, A.T.; Rame, J.E.; Das, S.R.; Berry, J.D.; Khera, A.; McGuire, D.K.; Vega, G.L.; et al. Relation of regional fat distribution to left ventricular structure and function. Circ. Cardiovasc. Imaging 2013, 6, 800–807. [Google Scholar] [CrossRef]
- Abbasi, S.; Hundley, W.; Bluemke, D.; Jerosch-Herold, M.; Blankstein, R.; Petersen, S.; Rider, O.J.; Lima, J.; Allison, M.; Murthy, V.; et al. Visceral adiposity and left ventricular remodeling: The Multi-Ethnic Study of Atherosclerosis. Nutr. Metab. Cardiovasc. Dis. 2015, 25, 667–676. [Google Scholar] [CrossRef]
- Campbell, D.J.; Gong, F.F.; Jelinek, M.V.; Castro, J.M.; Coller, J.M.; McGrady, M.; Boffa, U.; Shiel, L.; Liew, D.; Stewart, S.; et al. Threshold body mass index and sex-specific waist circumference for increased risk of heart failure with preserved ejection fraction. Eur. J. Prev. Cardiol. 2019, 26, 1594–1602. [Google Scholar] [CrossRef] [PubMed]
- Rao, V.; Zhao, D.; Allison, M.A.; Guallar, E.; Sharma, K.; Criqui, M.H.; Cushman, M.; Blumenthal, R.S.; Michos, E.D. Adiposity and Incident Heart Failure and its Subtypes: MESA (Multi-Ethnic Study of Atherosclerosis). JACC Heart Fail. 2018, 6, 999–1007. [Google Scholar] [CrossRef] [PubMed]
- Sorimachi, H.; Obokata, M.; Takahashi, N.; Reddy, Y.N.V.; Jain, C.C.; Verbrugge, F.H.; E Koepp, K.; Khosla, S.; Jensen, M.D.; A Borlaug, B. Pathophysiologic importance of visceral adipose tissue in women with heart failure and preserved ejection fraction. Eur. Heart J. 2020, 42, 1595–1605. [Google Scholar] [CrossRef] [PubMed]
- Lauer, M.S.; Anderson, K.M.; Kannel, W.B.; Levy, D. The impact of obesity on left ventricular mass and geometry. The Framingham Heart Study. JAMA 1991, 266, 231–236. [Google Scholar] [CrossRef] [PubMed]
- Peterson, L.R.; Waggoner, A.D.; Schechtman, K.B.; Meyer, T.; Gropler, R.J.; Barzilai, B.; Dávila-Román, V.G. Alterations in left ventricular structure and function in young healthy obese women: Assessment by echocardiography and tissue Doppler imaging. J. Am. Coll. Cardiol. 2004, 43, 1399–1404. [Google Scholar] [CrossRef]
- Powell, B.D.; Redfield, M.M.; Bybee, K.A.; Freeman, W.K.; Rihal, C.S. Association of obesity with left ventricular remodeling and diastolic dysfunction in patients without coronary artery disease. Am. J. Cardiol. 2006, 98, 116–120. [Google Scholar] [CrossRef]
- Wong, C.Y.; O’moore-Sullivan, T.; Leano, R.; Byrne, N.; Beller, E.; Marwick, T.H. Alterations of left ventricular myocardial characteristics associated with obesity. Circulation 2004, 110, 3081–3087. [Google Scholar] [CrossRef]
- Avelar, E.; Cloward, T.V.; Walker, J.M.; Farney, R.J.; Strong, M.; Pendleton, R.C.; Segerson, N.; Adams, T.D.; Gress, R.E.; Hunt, S.C.; et al. Left ventricular hypertrophy in severe obesity: Interactions among blood pressure, nocturnal hypoxemia, and body mass. Hypertension 2007, 49, 34–39. [Google Scholar] [CrossRef]
- Woodiwiss, A.J.; Libhaber, C.D.; Majane, O.H.; Libhaber, E.; Maseko, M.; Norton, G. Obesity promotes left ventricular concentric rather than eccentric geometric remodeling and hypertrophy independent of blood pressure. Am. J. Hypertens. 2008, 21, 1144–1151. [Google Scholar] [CrossRef]
- Reis, J.P.; Allen, N.; Gibbs, B.B.; Gidding, S.S.; Lee, J.M.; Lewis, C.E.; Lima, J.; Lloyd-Jones, D.; Loria, C.M.; Powell-Wiley, T.M.; et al. Association of the degree of adiposity and duration of obesity with measures of cardiac structure and function: The CARDIA study. Obesity 2014, 22, 2434–2440. [Google Scholar] [CrossRef]
- Gidding, S.S.; Liu, K.; Colangelo, L.A.; Cook, N.L.; Goff, D.C.; Glasser, S.P.; Gardin, J.M.; Lima, J.A. Longitudinal determinants of left ventricular mass and geometry: The Coronary Artery Risk Development in Young Adults (CARDIA) Study. Circ. Cardiovasc. Imaging 2013, 6, 769–775. [Google Scholar] [CrossRef]
- Bello, N.; Cheng, S.; Claggett, B.; Shah, A.M.; Ndumele, C.E.; Roca, G.Q.; Santos, A.B.; Gupta, D.; Vardeny, O.; Aguilar, D.; et al. Association of Weight and Body Composition on Cardiac Structure and Function in the ARIC Study (Atherosclerosis Risk in Communities). Circ. Heart Fail. 2016, 9, e002978. [Google Scholar] [CrossRef] [PubMed]
- Turkbey, E.B.; McClelland, R.L.; Kronmal, R.A.; Burke, G.L.; Bild, D.E.; Tracy, R.P.; Arai, A.; Lima, J.A.; Bluemke, D.A. The impact of obesity on the left ventricle: The Multi-Ethnic Study of Atherosclerosis (MESA). JACC Cardiovasc. Imaging 2010, 3, 266–274. [Google Scholar] [CrossRef] [PubMed]
- Yan, Y.; Li, S.; Guo, Y.; Fernandez, C.; A Bazzano, L.; He, J.; Mi, J.; Chen, W.; The International Childhood Cardiovascular Cohort Consortium Investigators. Life-Course Cumulative Burden of Body Mass Index and Blood Pressure on Progression of Left Ventricular Mass and Geometry in Midlife: The Bogalusa Heart Study. Circ. Res. 2020, 126, 633–643. [Google Scholar] [CrossRef]
- Kishi, S.; Armstrong, A.C.; Gidding, S.S.; Colangelo, L.A.; Venkatesh, B.A.; Jacobs, D.R.; Carr, J.J.; Terry, J.G.; Liu, K.; Goff, D.C.; et al. Association of obesity in early adulthood and middle age with incipient left ventricular dysfunction and structural remodeling: The CARDIA study (Coronary Artery Risk Development in Young Adults). JACC Heart Fail. 2014, 2, 500–508. [Google Scholar] [CrossRef] [PubMed]
- Razavi, A.C.; Bazzano, L.A.; He, J.; Fernandez, C.; Whelton, S.P.; Krousel-Wood, M.; Li, S.; Nierenberg, J.L.; Shi, M.; Li, C.; et al. Novel Findings from a Metabolomics Study of Left Ventricular Diastolic Function: The Bogalusa Heart Study. J. Am. Heart Assoc. 2020, 9, e015118. [Google Scholar] [CrossRef]
- Fliotsos, M.; Zhao, D.; Rao, V.N.; Ndumele, C.E.; Guallar, E.; Burke, G.L.; Vaidya, D.; Delaney, J.A.; Michos, E.D. Body Mass Index from Early-, Mid-, and Older-Adulthood and Risk of Heart Failure and Atherosclerotic Cardiovascular Disease: MESA. J. Am. Heart Assoc. 2018, 7, e009599. [Google Scholar] [CrossRef]
- Woodiwiss, A.J.; Norton, G.R. Obesity and left ventricular hypertrophy: The hypertension connection. Curr. Hypertens. Rep. 2015, 17, 539. [Google Scholar] [CrossRef]
- Aurigemma, G.P.; de Simone, G.; Fitzgibbons, T.P. Cardiac remodeling in obesity. Circ. Cardiovasc. Imaging 2013, 6, 142–152. [Google Scholar] [CrossRef]
- Szabo, L.; McCracken, C.; Cooper, J.; Rider, O.J.; Vago, H.; Merkely, B.; Harvey, N.C.; Neubauer, S.; E Petersen, S.; Raisi-Estabragh, Z. The role of obesity-related cardiovascular remodelling in mediating incident cardiovascular outcomes: A population-based observational study. Eur. Heart J.—Cardiovasc. Imaging 2023. ahead of print. [Google Scholar] [CrossRef]
- Venkateshvaran, A.; Faxen, U.L.; Hage, C.; Michaëlsson, E.; Svedlund, S.; Saraste, A.; Beussink-Nelson, L.; Fermer, M.L.; Gan, L.; Tromp, J.; et al. Association of epicardial adipose tissue with proteomics, coronary flow reserve, cardiac structure and function, and quality of life in heart failure with preserved ejection fraction: Insights from the PROMIS-HFpEF study. Eur. J. Heart Fail. 2022, 24, 2251–2260. [Google Scholar] [CrossRef] [PubMed]
- van Woerden, G.; van Veldhuisen, D.J.; Manintveld, O.C.; van Empel, V.P.; Willems, T.P.; de Boer, R.A.; Rienstra, M.; Westenbrink, B.D.; Gorter, T.M. Epicardial Adipose Tissue and Outcome in Heart Failure with Mid-Range and Preserved Ejection Fraction. Circ. Heart Fail. 2022, 15, e009238. [Google Scholar] [CrossRef] [PubMed]
- Takahari, K.; Utsunomiya, H.; Itakura, K.; Yamamoto, H.; Nakano, Y. Impact of the distribution of epicardial and visceral adipose tissue on left ventricular diastolic function. Heart Vessel. 2022, 37, 250–261. [Google Scholar] [CrossRef]
- Foppa, M.; Arora, G.; Gona, P.; Ashrafi, A.; Salton, C.J.; Yeon, S.B.; Blease, S.J.; Levy, D.; O’donnell, C.J.; Manning, W.J.; et al. Right Ventricular Volumes and Systolic Function by Cardiac Magnetic Resonance and the Impact of Sex, Age, and Obesity in a Longitudinally Followed Cohort Free of Pulmonary and Cardiovascular Disease: The Framingham Heart Study. Circ. Cardiovasc. Imaging 2016, 9, e003810. [Google Scholar] [CrossRef]
- Wong, C.Y.; O’moore-Sullivan, T.; Leano, R.; Hukins, C.; Jenkins, C.; Marwick, T.H. Association of subclinical right ventricular dysfunction with obesity. J. Am. Coll. Cardiol. 2006, 47, 611–616. [Google Scholar] [CrossRef] [PubMed]
- Rider, O.J.; Lewis, A.J.; Lewandowski, A.J.; Ntusi, N.; Nethononda, R.; Petersen, S.E.; Francis, J.M.; Pitcher, A.; Banerjee, R.; Leeson, P.; et al. Obese subjects show sex-specific differences in right ventricular hypertrophy. Circ. Cardiovasc. Imaging 2015, 8, e002454. [Google Scholar] [CrossRef]
- Gorter, T.M.; Hoendermis, E.S.; Van Veldhuisen, D.J.; Voors, A.A.; Lam, C.S.P.; Geelhoed, B.; Willems, T.P.; Van Melle, J.P. Right ventricular dysfunction in heart failure with preserved ejection fraction: A systematic review and meta-analysis. Eur. J. Heart Fail. 2016, 18, 1472–1487. [Google Scholar] [CrossRef]
- Nwabuo, C.C.; Vasan, R.S. Pathophysiology of Hypertensive Heart Disease: Beyond Left Ventricular Hypertrophy. Curr. Hypertens. Rep. 2020, 22, 11. [Google Scholar] [CrossRef]
- Wohlfahrt, P.; Redfield, M.M.; Lopez-Jimenez, F.; Melenovsky, V.; Kane, G.C.; Rodeheffer, R.J.; Borlaug, B.A. Impact of general and central adiposity on ventricular-arterial aging in women and men. JACC Heart Fail. 2014, 2, 489–499. [Google Scholar] [CrossRef]
- Liu, Z.; Hu, W.; Zhang, H.; Tao, H.; Lei, P.; Liu, J.; Yu, Y.; Dong, Q.; Gao, L.; Zhang, D. EAT Thickness as a Predominant Feature for Evaluating Arterial Stiffness in Patients with Heart Failure with Preserved Ejection Fraction. Diabetes Metab. Syndr. Obes 2022, 15, 1217–1226. [Google Scholar] [CrossRef]
- Levy, D.; Murabito, J.M.; Anderson, K.M.; Christiansen, J.C.; Castelli, W.P. echocardiographic left ventricular hypertrophy: Clinical characteristics. The Framingham Heart Study. Clin. Exp. Hypertens. A 1992, 14, 85–97. [Google Scholar] [CrossRef] [PubMed]
- Izzo, R.; Losi, M.-A.; Stabile, E.; Lönnebakken, M.T.; Canciello, G.; Esposito, G.; Barbato, E.; De Luca, N.; Trimarco, B.; de Simone, G. Development of Left Ventricular Hypertrophy in Treated Hypertensive Outpatients: The Campania Salute Network. Hypertension 2017, 69, 136–142. [Google Scholar] [CrossRef] [PubMed]
- Lønnebakken, M.; Mancusi, C.; Losi, M.; Gerdts, E.; Izzo, R.; Manzi, M.; De Luca, N.; de Simone, G.; Trimarco, B. Weight loss facilitates reduction of left ventricular mass in obese hypertensive patients: The Campania Salute Network. Nutr. Metab. Cardiovasc. Dis. 2019, 29, 185–190. [Google Scholar] [CrossRef] [PubMed]
- Lønnebakken, M.T.; Izzo, R.; Mancusi, C.; Gerdts, E.; Losi, M.A.; Canciello, G.; Giugliano, G.; De Luca, N.; Trimarco, B.; de Simone, G. Left Ventricular Hypertrophy Regression During Antihypertensive Treatment in an Outpatient Clinic (the Campania Salute Network). J. Am. Heart Assoc. 2017, 6, e004152. [Google Scholar] [CrossRef]
- MacMahon, S.W.; Wilcken, D.E.; Macdonald, G.J. The effect of weight reduction on left ventricular mass. A randomized controlled trial in young, overweight hypertensive patients. N. Engl. J. Med. 1986, 314, 334–339. [Google Scholar] [CrossRef]
- Donini, L.M.; Poggiogalle, E.; Mosca, V.; Pinto, A.; Brunani, A.; Capodaglio, P. Disability affects the 6-minute walking distance in obese subjects (BMI > 40 kg/m2). PLoS ONE 2013, 8, e75491. [Google Scholar] [CrossRef]
- Andrianopoulos, V.; E Holland, A.; Singh, S.J.; Franssen, F.M.; Pennings, H.-J.; Michels, A.J.; Smeenk, F.W.; Vogiatzis, I.; Wouters, E.F.; A Spruit, M. Six-minute walk distance in patients with chronic obstructive pulmonary disease: Which reference equations should we use? Chronic Respir. Dis. 2015, 12, 111–119. [Google Scholar] [CrossRef]
- Pataky, Z.; Armand, S.; Müller-Pinget, S.; Golay, A.; Allet, L. Effects of obesity on functional capacity. Obesity 2013, 22, 56–62. [Google Scholar] [CrossRef]
- Sabbah, M.S.; Fayyaz, A.U.; De Denus, S.; Felker, G.M.; Borlaug, B.A.; Dasari, S.; Carter, R.E.; Redfield, M.M. Obese-Inflammatory Phenotypes in Heart Failure with Preserved Ejection Fraction. Circ. Heart Fail. 2020, 13, e006414. [Google Scholar] [CrossRef]
- Wijk, S.S.-V.; Tromp, J.; Beussink-Nelson, L.; Hage, C.; Svedlund, S.; Saraste, A.; Swat, S.A.; Sanchez, C.; Njoroge, J.; Tan, R.-S.; et al. Proteomic Evaluation of the Comorbidity-Inflammation Paradigm in Heart Failure with Preserved Ejection Fraction: Results from the PROMIS-HFpEF Study. Circulation 2020, 142, 2029–2044. [Google Scholar] [CrossRef]
- Albar, Z.; Albakri, M.; Hajjari, J.; Karnib, M.; Janus, S.E.; Al-Kindi, S.G. Inflammatory Markers and Risk of Heart Failure with Reduced to Preserved Ejection Fraction. Am. J. Cardiol. 2022, 167, 68–75. [Google Scholar] [CrossRef] [PubMed]
- Zhao, L.; Cheng, G.; Jin, R.; Afzal, M.R.; Samanta, A.; Xuan, Y.-T.; Girgis, M.; Elias, H.; Zhu, Y.; Davani, A.; et al. Deletion of Interleukin-6 Attenuates Pressure Overload-Induced Left Ventricular Hypertrophy and Dysfunction. Circ. Res. 2016, 118, 1918–1929. [Google Scholar] [CrossRef]
- Glezeva, N.; Voon, V.; Watson, C.; Horgan, S.; McDonald, K.; Ledwidge, M.; Baugh, J. exaggerated inflammation and monocytosis associate with diastolic dysfunction in heart failure with preserved ejection fraction: Evidence of M2 macrophage activation in disease pathogenesis. J. Card. Fail. 2014, 21, 167–177. [Google Scholar] [CrossRef] [PubMed]
- DeBerge, M.; Shah, S.J.; Wilsbacher, L.; Thorp, E.B. Macrophages in Heart Failure with Reduced versus Preserved Ejection Fraction. Trends Mol. Med. 2019, 25, 328–340. [Google Scholar] [CrossRef] [PubMed]
- Hahn, V.S.; Yanek, L.R.; Vaishnav, J.; Ying, W.; Vaidya, D.; Lee, Y.Z.J.; Riley, S.J.; Subramanya, V.; Brown, E.E.; Hopkins, C.D.; et al. Endomyocardial Biopsy Characterization of Heart Failure with Preserved Ejection Fraction and Prevalence of Cardiac Amyloidosis. JACC Heart Fail. 2020, 8, 712–724. [Google Scholar] [CrossRef] [PubMed]
- Westermann, D.; Lindner, D.; Kasner, M.; Zietsch, C.; Savvatis, K.; Escher, F.; von Schlippenbach, J.; Skurk, C.; Steendijk, P.; Riad, A.; et al. Cardiac inflammation contributes to changes in the extracellular matrix in patients with heart failure and normal ejection fraction. Circ. Heart Fail. 2011, 4, 44–52. [Google Scholar] [CrossRef] [PubMed]
- Roh, J.; Hill, J.A.; Singh, A.; Valero-Muñoz, M.; Sam, F. Heart Failure with Preserved Ejection Fraction: Heterogeneous Syndrome, Diverse Preclinical Models. Circ. Res. 2022, 130, 1906–1925. [Google Scholar] [CrossRef]
- Kass, D.A. Understanding HFpEF with Obesity: Will Pigs Come to the Rescue? JACC Basic Transl. Sci. 2021, 6, 171–173. [Google Scholar] [CrossRef]
- Kawai, T.; Autieri, M.V.; Scalia, R. Adipose tissue inflammation and metabolic dysfunction in obesity. Am. J. Physiol. Physiol. 2021, 320, C375–C391. [Google Scholar] [CrossRef]
- Brestoff, J.R.; Artis, D. Immune regulation of metabolic homeostasis in health and disease. Cell 2015, 161, 146–160. [Google Scholar] [CrossRef]
- Asterholm, I.W.; Tao, C.; Morley, T.S.; Wang, Q.A.; Delgado-Lopez, F.; Wang, Z.V.; Scherer, P.E. adipocyte inflammation is essential for healthy adipose tissue expansion and remodeling. Cell Metab. 2014, 20, 103–118. [Google Scholar] [CrossRef]
- Koenen, M.; Hill, M.A.; Cohen, P.; Sowers, J.R. Obesity, Adipose Tissue and Vascular Dysfunction. Circ. Res. 2021, 128, 951–968. [Google Scholar] [CrossRef] [PubMed]
- Aron-Wisnewsky, J.; Tordjman, J.; Poitou, C.; Darakhshan, F.; Hugol, D.; Basdevant, A.; Aissat, A.; Guerre-Millo, M.; Clément, K. Human adipose tissue macrophages: m1 and m2 cell surface markers in subcutaneous and omental depots and after weight loss. J. Clin. Endocrinol. Metab. 2009, 94, 4619–4623. [Google Scholar] [CrossRef] [PubMed]
- Snel, M.; Jonker, J.T.; Schoones, J.W.; Lamb, H.; De Roos, A.; Pijl, H.; Smit, J.W.A.; Meinders, A.E.; Jazet, I.M. Ectopic fat and insulin resistance: Pathophysiology and effect of diet and lifestyle interventions. Int. J. Endocrinol. 2012, 2012, 983814. [Google Scholar] [CrossRef]
- Shi, H.; Kokoeva, M.V.; Inouye, K.; Tzameli, I.; Yin, H.; Flier, J.S. TLR4 links innate immunity and fatty acid–induced insulin resistance. J. Clin. Investig. 2006, 116, 3015–3025. [Google Scholar] [CrossRef]
- Lee, Y.S.; Kim, J.-W.; Osborne, O.; Oh, D.Y.; Sasik, R.; Schenk, S.; Chen, A.; Chung, H.; Murphy, A.; Watkins, S.M.; et al. Increased adipocyte O2 consumption triggers HIF-1α, causing inflammation and insulin resistance in obesity. Cell 2014, 157, 1339–1352. [Google Scholar] [CrossRef]
- Stienstra, R.; Tack, C.J.; Kanneganti, T.-D.; Joosten, L.A.; Netea, M.G. The inflammasome puts obesity in the danger zone. Cell Metab. 2012, 15, 10–18. [Google Scholar] [CrossRef]
- Lindhorst, A.; Raulien, N.; Wieghofer, P.; Eilers, J.; Rossi, F.M.V.; Bechmann, I.; Gericke, M. Adipocyte death triggers a pro-inflammatory response and induces metabolic activation of resident macrophages. Cell Death Dis. 2021, 12, 579. [Google Scholar] [CrossRef]
- Saltiel, A.R.; Olefsky, J.M. Inflammatory mechanisms linking obesity and metabolic disease. J. Clin. Investig. 2017, 127, 1–4. [Google Scholar] [CrossRef]
- Henning, R.J. Obesity and obesity-induced inflammatory disease contribute to atherosclerosis: A review of the pathophysiology and treatment of obesity. Am J Cardiovasc Dis. 2021, 11, 504–529. [Google Scholar]
- Rizzoni, D.; De Ciuceis, C.; Szczepaniak, P.; Paradis, P.; Schiffrin, E.L.; Guzik, T.J. Immune System and Microvascular Remodeling in Humans. Hypertension 2022, 79, 691–705. [Google Scholar] [CrossRef] [PubMed]
- Rana, M.N.; Neeland, I.J. Adipose Tissue Inflammation and Cardiovascular Disease: An Update. Curr. Diabetes Rep. 2022, 22, 27–37. [Google Scholar] [CrossRef] [PubMed]
- Neeland, I.J.; Marso, S.P.; Ayers, C.R.; Lewis, B.; Oslica, R.; Francis, W.; Rodder, S.; Pandey, A.; Joshi, P.H. Effects of liraglutide on visceral and ectopic fat in adults with overweight and obesity at high cardiovascular risk: A randomised, double-blind, placebo-controlled, clinical trial. Lancet Diabetes Endocrinol. 2021, 9, 595–605. [Google Scholar] [CrossRef] [PubMed]
- Martens, P.; Nguyen, C.; Tang, W.W. Is epicardial adipose tissue a key pathophysiologic target in heart failure with preserved ejection? J. Mol. Cell Cardiol. 2022, 171, 69–70. [Google Scholar] [CrossRef] [PubMed]
- Ayton, S.L.; Gulsin, G.S.; McCann, G.P.; Moss, A.J. Epicardial adipose tissue in obesity-related cardiac dysfunction. Heart 2022, 108, 339–344. [Google Scholar] [CrossRef] [PubMed]
- Ohara, T.; Little, W.C. Evolving focus on diastolic dysfunction in patients with coronary artery disease. Curr. Opin. Cardiol. 2010, 25, 613–621. [Google Scholar] [CrossRef]
- Dunlay, S.M.; Roger, V.L.; Redfield, M.M. Epidemiology of heart failure with preserved ejection fraction. Nat. Rev. Cardiol. 2017, 14, 591–602. [Google Scholar] [CrossRef]
- Gerber, Y.; Weston, S.A.; Enriquez-Sarano, M.; Manemann, S.M.; Chamberlain, A.M.; Jiang, R.; Roger, V.L. Atherosclerotic Burden and Heart Failure After Myocardial Infarction. JAMA Cardiol. 2016, 1, 156–162. [Google Scholar] [CrossRef]
- Lamblin, N.; Meurice, T.; Tricot, O.; de Groote, P.; Lemesle, G.; Bauters, C. First Hospitalization for Heart Failure in Outpatients with Stable Coronary Artery Disease: Determinants, Role of Incident Myocardial Infarction, and Prognosis. J. Card. Fail. 2018, 24, 815–822. [Google Scholar] [CrossRef]
- Ho, J.E.; Enserro, D.; Brouwers, F.P.; Kizer, J.R.; Shah, S.J.; Psaty, B.M.; Bartz, T.M.; Santhanakrishnan, R.; Lee, D.S.; Chan, C.; et al. Predicting Heart Failure with Preserved and Reduced Ejection Fraction: The International Collaboration on Heart Failure Subtypes. Circ. Heart Fail. 2016, 9, e003116. [Google Scholar] [CrossRef]
- John, J.E.; Claggett, B.; Skali, H.; Solomon, S.D.; Cunningham, J.W.; Matsushita, K.; Konety, S.H.; Kitzman, D.W.; Mosley, T.H.; ClarkIII, D.; et al. Coronary Artery Disease and Heart Failure With Preserved Ejection Fraction: The ARIC Study. J. Am. Heart Assoc. 2022, 11, e021660. [Google Scholar] [CrossRef] [PubMed]
- Badar, A.A.; Perez-Moreno, A.C.; Hawkins, N.M.; Jhund, P.S.; Brunton, A.P.; Anand, I.; McKelvie, R.S.; Komajda, M.; Zile, M.R.; Carson, P.E.; et al. Clinical Characteristics and Outcomes of Patients with Coronary Artery Disease and Angina: Analysis of the Irbesartan in Patients with Heart Failure and Preserved Systolic Function. Circ. Heart Fail. 2015, 8, 717–724. [Google Scholar] [CrossRef] [PubMed]
- Rush, C.J.; Berry, C.; Oldroyd, K.G.; Rocchiccioli, J.P.; Lindsay, M.M.; Touyz, R.M.; Murphy, C.L.; Ford, T.J.; Sidik, N.; McEntegart, M.B.; et al. Prevalence of Coronary Artery Disease and Coronary Microvascular Dysfunction in Patients with Heart Failure with Preserved Ejection Fraction. JAMA Cardiol. 2021, 6, 1130–1143. [Google Scholar] [CrossRef] [PubMed]
- Srivaratharajah, K.; Coutinho, T.; Dekemp, R.; Liu, P.; Haddad, H.; Stadnick, E.; Davies, R.A.; Chih, S.; Dwivedi, G.; Guo, A.; et al. Reduced Myocardial Flow in Heart Failure Patients with Preserved Ejection Fraction. Circ. Heart Fail. 2016, 9, e002562. [Google Scholar] [CrossRef] [PubMed]
- Dryer, K.; Gajjar, M.; Narang, N.; Lee, M.; Paul, J.; Shah, A.P.; Nathan, S.; Butler, J.; Davidson, C.J.; Fearon, W.F.; et al. Coronary microvascular dysfunction in patients with heart failure with preserved ejection fraction. Am. J. Physiol. Heart Circ. Physiol. 2018, 314, H1033–H1042. [Google Scholar] [CrossRef]
- Tromp, J.; Lim, S.L.; Tay, W.T.; Teng, T.-H.K.; Chandramouli, C.; Ouwerkerk, W.; Wander, G.S.; Sawhney, J.P.; Yap, J.; MacDonald, M.R.; et al. Microvascular Disease in Patients with Diabetes with Heart Failure and Reduced Ejection Versus Preserved Ejection Fraction. Diabetes Care 2019, 42, 1792–1799. [Google Scholar] [CrossRef]
- Weerts, J.; Mourmans, S.G.J.; Aizpurua, A.B.; Schroen, B.L.M.; Knackstedt, C.; Eringa, E.; Houben, A.J.H.M.; van Empel, V.P.M. The Role of Systemic Microvascular Dysfunction in Heart Failure with Preserved Ejection Fraction. Biomolecules 2022, 12, 278. [Google Scholar] [CrossRef]
- Yang, J.H.; Obokata, M.; Reddy, Y.N.; Redfield, M.M.; Lerman, A.; Borlaug, B.A. Endothelium-dependent and independent coronary microvascular dysfunction in patients with heart failure with preserved ejection fraction. Eur. J. Heart Fail. 2020, 22, 432–441. [Google Scholar] [CrossRef]
- Saavedra-Alvarez, A.; Pereyra, K.V.; Toledo, C.; Iturriaga, R.; Del Rio, R. Vascular dysfunction in HFpEF: Potential role in the development, maintenance, and progression of the disease. Front. Cardiovasc. Med. 2022, 9, 1070935. [Google Scholar] [CrossRef]
- Mohammed, S.F.; Hussain, S.; Mirzoyev, S.A.; Edwards, W.D.; Maleszewski, J.J.; Redfield, M.M. Coronary microvascular rarefaction and myocardial fibrosis in heart failure with preserved ejection fraction. Circulation 2015, 131, 550–559. [Google Scholar] [CrossRef]
- Markley, R.; Del Buono, M.G.; Mihalick, V.; Pandelidis, A.; Trankle, C.; Jordan, J.H.; Decamp, K.; Winston, C.; Carbone, S.; Billingsley, H.; et al. Abnormal left ventricular subendocardial perfusion and diastolic function in women with obesity and heart failure and preserved ejection fraction. Int. J. Cardiovasc. Imaging 2023, 39, 811–819. [Google Scholar] [CrossRef]
- Elgendy, I.Y.; Pepine, C.J. Heart Failure with Preserved Ejection Fraction: Is Ischemia Due to Coronary Microvascular Dysfunction a Mechanistic Factor? Am. J. Med. 2019, 132, 692–697. [Google Scholar] [CrossRef] [PubMed]
- Cornuault, L.; Rouault, P.; Duplàa, C.; Couffinhal, T.; Renault, M.-A. Endothelial Dysfunction in Heart Failure with Preserved Ejection Fraction: What are the Experimental Proofs? Front. Physiol. 2022, 13, 906272. [Google Scholar] [CrossRef] [PubMed]
- Boutagy, N.E.; Singh, A.K.; Sessa, W.C. Targeting the vasculature in cardiometabolic disease. J. Clin. Investig. 2022, 132, e148556. [Google Scholar] [CrossRef] [PubMed]
- Libby, P. The changing landscape of atherosclerosis. Nature 2021, 592, 524–533. [Google Scholar] [CrossRef]
- Bapat, S.P.; Whitty, C.; Mowery, C.T.; Liang, Y.; Yoo, A.; Jiang, Z.; Peters, M.C.; Zhang, L.-J.; Vogel, I.; Zhou, C.; et al. Obesity alters pathology and treatment response in inflammatory disease. Nature 2022, 604, 337–342. [Google Scholar] [CrossRef]
- Cypess, A.M. Reassessing Human Adipose Tissue. N. Engl. J. Med. 2022, 386, 768–779. [Google Scholar] [CrossRef] [PubMed]
- Aroor, A.R.; Jia, G.; Sowers, J.R. Cellular mechanisms underlying obesity-induced arterial stiffness. Am. J. Physiol. Regul. Integr. Comp. Physiol. 2018, 314, R387–R398. [Google Scholar] [CrossRef]
- Mazzotta, C.; Basu, S.; Gower, A.C.; Karki, S.; Farb, M.G.; Sroczynski, E.; Zizza, E.; Sarhan, A.; Pande, A.N.; Walsh, K.; et al. Perivascular Adipose Tissue Inflammation in Ischemic Heart Disease. Arter. Thromb. Vasc. Biol. 2021, 41, 1239–1250. [Google Scholar] [CrossRef]
- McGill, H.C.; McMahan, C.A.; Herderick, E.E.; Zieske, A.W.; Malcom, G.T.; Tracy, R.E.; Strong, J.P. Obesity accelerates the progression of coronary atherosclerosis in young men. Circulation 2002, 105, 2712–2718. [Google Scholar] [CrossRef]
- Lakka, H.-M.; Lakka, T.; Tuomilehto, J.; Salonen, J. Abdominal obesity is associated with increased risk of acute coronary events in men. Eur. Heart J. 2002, 23, 706–713. [Google Scholar] [CrossRef]
- Sorop, O.; Olver, T.D.; van de Wouw, J.; Heinonen, I.; van Duin, R.; Duncker, D.J.; Merkus, D. The microcirculation: A key player in obesity-associated cardiovascular disease. Cardiovasc. Res. 2017, 113, 1035–1045. [Google Scholar] [CrossRef] [PubMed]
- Campbell, D.J.; Somaratne, J.B.; Prior, D.L.; Yii, M.; Kenny, J.F.; Newcomb, A.E.; Kelly, D.J.; Black, M.J. Obesity is associated with lower coronary microvascular density. PLoS ONE 2013, 8, e81798. [Google Scholar] [CrossRef] [PubMed]
- Bajaj, N.S.; Osborne, M.T.; Gupta, A.; Tavakkoli, A.; Bravo, P.E.; Vita, T.; Bibbo, C.F.; Hainer, J.; Dorbala, S.; Blankstein, R.; et al. Coronary Microvascular Dysfunction and Cardiovascular Risk in Obese Patients. J. Am. Coll. Cardiol. 2018, 72, 707–717. [Google Scholar] [CrossRef] [PubMed]
- Al Suwaidi, J.; Higano, S.T.; Holmes, D.R.; Lennon, R.; Lerman, A. Obesity is independently associated with coronary endothelial dysfunction in patients with normal or mildly diseased coronary arteries. J. Am. Coll. Cardiol. 2001, 37, 1523–1528. [Google Scholar] [CrossRef] [PubMed]
- Steinberg, H.; Chaker, H.; Leaming, R.; Johnson, A.; Brechtel, G.; Baron, A.D. Obesity/insulin resistance is associated with endothelial dysfunction. Implications for the syndrome of insulin resistance. J. Clin. Investig. 1996, 97, 2601–2610. [Google Scholar] [CrossRef]
- Schindler, T.H.; Cardenas, J.; Prior, J.O.; Facta, A.D.; Kreissl, M.C.; Zhang, X.-L.; Sayre, J.; Dahlbom, M.; Licinio, J.; Schelbert, H.R. Relationship between increasing body weight, insulin resistance, inflammation, adipocytokine leptin, and coronary circulatory function. J. Am. Coll. Cardiol. 2006, 47, 1188–1195. [Google Scholar] [CrossRef] [PubMed]
- Pi, X.; Xie, L.; Patterson, C. Emerging Roles of Vascular Endothelium in Metabolic Homeostasis. Circ. Res. 2018, 123, 477–494. [Google Scholar] [CrossRef] [PubMed]
- Li, M.; Qian, M.; Kyler, K.; Xu, J. Adipose Tissue-Endothelial Cell Interactions in Obesity-Induced Endothelial Dysfunction. Front. Cardiovasc. Med. 2021, 8, 681581. [Google Scholar] [CrossRef]
- Paavonsalo, S.; Hariharan, S.; Lackman, M.H.; Karaman, S. Capillary Rarefaction in Obesity and Metabolic Diseases—Organ-Specificity and Possible Mechanisms. Cells 2020, 9, 2683. [Google Scholar] [CrossRef]
- Bondareva, O.; Rodríguez-Aguilera, J.R.; Oliveira, F.; Liao, L.; Rose, A.; Gupta, A.; Singh, K.; Geier, F.; Schuster, J.; Boeckel, J.-N.; et al. Single-cell profiling of vascular endothelial cells reveals progressive organ-specific vulnerabilities during obesity. Nat. Metab. 2022, 4, 1591–1610. [Google Scholar] [CrossRef]
- Fang, J.C. Heart Failure with Preserved Ejection Fraction: A Kidney Disorder? Circulation 2016, 134, 435–437. [Google Scholar] [CrossRef] [PubMed]
- Sharma, K.; Hill, T.; Grams, M.; Daya, N.R.; Hays, A.G.; Fine, D.; Thiemann, D.R.; Weiss, R.G.; Tedford, R.J.; Kass, D.A.; et al. Outcomes and worsening renal function in patients hospitalized with heart failure with preserved ejection fraction. Am. J. Cardiol. 2015, 116, 1534–1540. [Google Scholar] [CrossRef]
- van de Wouw, J.; Broekhuizen, M.; Sorop, O.; Joles, J.A.; Verhaar, M.C.; Duncker, D.J.; Danser, A.H.J.; Merkus, D. Chronic Kidney Disease as a Risk Factor for Heart Failure with Preserved Ejection Fraction: A Focus on Microcirculatory Factors and Therapeutic Targets. Front. Physiol. 2019, 10, 1108. [Google Scholar] [CrossRef]
- Mark, P.B.; Mangion, K.; Rankin, A.J.; Rutherford, E.; Lang, N.N.; Petrie, M.C.; Stoumpos, S.; Patel, R.K. Left ventricular dysfunction with preserved ejection fraction: The most common left ventricular disorder in chronic kidney disease patients. Clin. Kidney J. 2022, 15, 2186–2199. [Google Scholar] [CrossRef] [PubMed]
- Joslin, J.R.; Lioudaki, E.; Androulakis, E. Interrelation between heart failure with preserved ejection fraction and renal impairment. Rev. Cardiovasc. Med. 2022, 23, 69. [Google Scholar] [CrossRef] [PubMed]
- Gori, M.; Senni, M.; Gupta, D.K.; Charytan, D.; Kraigher-Krainer, E.; Pieske, B.; Claggett, B.; Shah, A.M.; Santos, A.B.S.; Zile, M.; et al. Association between renal function and cardiovascular structure and function in heart failure with preserved ejection fraction. Eur. Heart J. 2014, 35, 3442–3451. [Google Scholar] [CrossRef]
- Katz, D.H.; Burns, J.A.; Aguilar, F.G.; Beussink, L.; Shah, S.J. Albuminuria is independently associated with cardiac remodeling, abnormal right and left ventricular function, and worse outcomes in heart failure with preserved ejection fraction. JACC Heart Fail. 2014, 2, 586–596. [Google Scholar] [CrossRef]
- Selvaraj, S.; Shah, S.J.; Ommerborn, M.J.; Clark, C.R.; Hall, M.E.; Mentz, R.J.; Qazi, S.; Robbins, J.M.; Skelton, T.N.; Chen, J.; et al. Pulmonary Hypertension Is Associated with a Higher Risk of Heart Failure Hospitalization and Mortality in Patients with Chronic Kidney Disease: The Jackson Heart Study. Circ Heart Fail. Circ. Heart Fail. 2017, 10, e003940. [Google Scholar] [CrossRef]
- ter Maaten, J.M.; Damman, K.; Verhaar, M.C.; Paulus, W.J.; Duncker, D.J.; Cheng, C.; Heerebeek, L.; Hillege, H.L.; Lam, C.S.; Navis, G.; et al. Connecting heart failure with preserved ejection fraction and renal dysfunction: The role of endothelial dysfunction and inflammation. Eur. J. Heart Fail. 2016, 18, 588–598. [Google Scholar] [CrossRef]
- Carlström, M. Nitric oxide signalling in kidney regulation and cardiometabolic health. Nat. Rev. Nephrol. 2021, 17, 575–590. [Google Scholar] [CrossRef] [PubMed]
- Wang, M.; Wang, Z.; Chen, Y.; Dong, Y. Kidney Damage Caused by Obesity and Its Feasible Treatment Drugs. Int. J. Mol. Sci. 2022, 23, 747. [Google Scholar] [CrossRef] [PubMed]
- D’Agati, V.D.; Chagnac, A.; de Vries, A.; Levi, M.; Porrini, E.; Herman-Edelstein, M.; Praga, M. Obesity-related glomerulopathy: Clinical and pathologic characteristics and pathogenesis. Nat. Rev. Nephrol. 2016, 12, 453–471. [Google Scholar] [CrossRef] [PubMed]
- García-Carro, C.; Vergara, A.; Bermejo, S.; Azancot, M.A.; Sellarés, J.; Soler, M.J. A Nephrologist Perspective on Obesity: From Kidney Injury to Clinical Management. Front. Med. 2021, 8, 655871. [Google Scholar] [CrossRef] [PubMed]
- Chagnac, A.; Zingerman, B.; Rozen-Zvi, B.; Herman-Edelstein, M. Consequences of Glomerular Hyperfiltration: The Role of Physical Forces in the Pathogenesis of Chronic Kidney Disease in Diabetes and Obesity. Nephron 2019, 143, 38–42. [Google Scholar] [CrossRef]
- Hall, J.E.; do Carmo, J.M.; da Silva, A.A.; Wang, Z.; Hall, M.E. Obesity, kidney dysfunction and hypertension: Mechanistic links. Nat. Rev. Nephrol. 2019, 15, 367–385. [Google Scholar] [CrossRef] [PubMed]
- Arabi, T.; Shafqat, A.; Sabbah, B.N.; Fawzy, N.A.; Shah, H.; Abdulkader, H.; Razak, A.; Sabbah, A.N.; Arabi, Z. Obesity-related kidney disease: Beyond hypertension and insulin-resistance. Front. Endocrinol. 2023, 13, 1095211. [Google Scholar] [CrossRef] [PubMed]
- Hashimoto, Y.; Tanaka, M.; Okada, H.; Senmaru, T.; Hamaguchi, M.; Asano, M.; Yamazaki, M.; Oda, Y.; Hasegawa, G.; Toda, H.; et al. Metabolically healthy obesity and risk of incident CKD. Clin. J. Am. Soc. Nephrol. 2015, 10, 578–583. [Google Scholar] [CrossRef]
- Kotsis, V.; Martinez, F.; Trakatelli, C.; Redon, J. Impact of Obesity in Kidney Diseases. Nutrients 2021, 13, 4482. [Google Scholar] [CrossRef]
- Jam, S.A.; Moloudpour, B.; Najafi, F.; Darbandi, M.; Pasdar, Y. Metabolic obesity phenotypes and chronic kidney disease: A cross-sectional study from the RaNCD cohort study. BMC Nephrol. 2022, 23, 233. [Google Scholar] [CrossRef]
- Wang, J.; Niratharakumar, K.; Gokhale, K.; Tahrani, A.A.; Taverner, T.; Thomas, G.N.; Dasgupta, I. Obesity Without Metabolic Abnormality and Incident CKD: A Population-Based British Cohort Study. Am. J. Kidney Dis. 2022, 79, 24–35.e1. [Google Scholar] [CrossRef] [PubMed]
- Hsu, C.-Y.; McCulloch, C.E.; Iribarren, C.; Darbinian, J.; Go, A.S. Body mass index and risk for end-stage renal disease. Ann. Intern. Med. 2006, 144, 21–28. [Google Scholar] [CrossRef] [PubMed]
- Yu, Z.; Grams, M.E.; Ndumele, C.E.; Wagenknecht, L.; Boerwinkle, E.; North, K.E.; Rebholz, C.M.; Giovannucci, E.L.; Coresh, J. Association Between Midlife Obesity and Kidney Function Trajectories: The Atherosclerosis Risk in Communities (ARIC) Study. Am. J. Kidney Dis. 2021, 77, 376–385. [Google Scholar] [CrossRef] [PubMed]
- Ybarra, J.; Sánchez-Hernández, J.; Vilallonga, R.; Romeo, J.H. Differential associations between glomerular filtration rate and duration of obesity depending on the presence or absence of left ventricular diastolic dysfunction. Eur. J. Intern. Med. 2016, 32, 47–52. [Google Scholar] [CrossRef]
- Redfield, M.M.; Borlaug, B.A. Heart Failure with Preserved Ejection Fraction: A Review. JAMA 2023, 329, 827–838. [Google Scholar] [CrossRef] [PubMed]
- Maciejewski, M.L.; Arterburn, D.E.; Van Scoyoc, L.; Smith, V.A.; Yancy, W.S., Jr.; Weidenbacher, H.J.; Livingston, E.H.; Olsen, M.K. Bariatric Surgery and Long-term Durability of Weight Loss. JAMA Surg. 2016, 151, 1046–1055. Available online: https://pubmed.ncbi.nlm.nih.gov/27579793 (accessed on 18 November 2021). [CrossRef]
- Järvholm, K.; Janson, A.; Peltonen, M.; Neovius, M.; Gronowitz, E.; Engström, M.; Laurenius, A.; Beamish, A.J.; Dahlgren, J.; Sjögren, L.; et al. Metabolic and bariatric surgery versus intensive non-surgical treatment for adolescents with severe obesity (AMOS2): A multicentre, randomised, controlled trial in Sweden. Lancet Child Adolesc. Health 2023, 7, 249–260. [Google Scholar] [CrossRef] [PubMed]
- Myerson, S.; Montgomery, H.; World, M.J.; Pennell, D.J. Left ventricular mass: Reliability of M-mode and 2-dimensional echocardiographic formulas. Hypertension 2002, 40, 673–678. [Google Scholar] [CrossRef]
- Le Jemtel, T.H.; Richardson, W.; Samson, R.; Jaiswal, A.; Oparil, S. Pathophysiology and Potential Non-Pharmacologic Treatments of Obesity or Kidney Disease Associated Refractory Hypertension. Curr. Hypertens. Rep. 2017, 19, 18. [Google Scholar] [CrossRef]
- Henry, J.A.; Abdesselam, I.; Deal, O.; Lewis, A.J.; Rayner, J.; Bernard, M.; Dutour, A.; Gaborit, B.; Kober, F.; Soghomonian, A.; et al. Changes in epicardial and visceral adipose tissue depots following bariatric surgery and their effect on cardiac geometry. Front. Endocrinol. 2023, 14, 18. [Google Scholar] [CrossRef]
- Rider, O.J.; Francis, J.M.; Ali, M.; Petersen, S.; Robinson, M.; Robson, M.D.; Byrne, J.; Clarke, K.; Neubauer, S. Beneficial cardiovascular effects of bariatric surgical and dietary weight loss in obesity. J. Am. Coll. Cardiol. 2009, 54, 718–726. [Google Scholar] [CrossRef] [PubMed]
- Jhaveri, R.R.; Pond, K.K.; Hauser, T.H.; Kissinger, K.V.; Goepfert, L.; Schneider, B.; Jones, D.B.; Manning, W.J. Cardiac remodeling after substantial weight loss: A prospective cardiac magnetic resonance study after bariatric surgery. Surg. Obes. Relat. Dis. 2009, 5, 648–652. [Google Scholar] [CrossRef] [PubMed]
- de Witte, D.; Wijngaarden, L.H.; van Houten, V.A.A.; Dorpel, M.A.V.D.; Bruning, T.A.; van der Harst, E.; Klaassen, R.A.; Niezen, R.A. Improvement of Cardiac Function After Roux-en-Y Gastric Bypass in Morbidly Obese Patients Without Cardiac History Measured by Cardiac MRI. Obes. Surg. 2020, 30, 2475–2481. [Google Scholar] [CrossRef] [PubMed]
- Leichman, J.G.; Aguilar, D.; King, T.M.; Mehta, S.; Majka, C.; Scarborough, T.; Wilson, E.B.; Taegtmeyer, H. Improvements in systemic metabolism, anthropometrics, and left ventricular geometry 3 months after bariatric surgery. Surg. Obes. Relat. Dis. 2006, 2, 592–599. [Google Scholar] [CrossRef] [PubMed]
- Gaborit, B.; Jacquier, A.; Kober, F.; Abdesselam, I.; Cuisset, T.; Boullu-Ciocca, S.; Emungania, O.; Alessi, M.-C.; Clément, K.; Bernard, M.; et al. Effects of bariatric surgery on cardiac ectopic fat: Lesser decrease in epicardial fat compared to visceral fat loss and no change in myocardial triglyceride content. J. Am. Coll. Cardiol. 2012, 60, 1381–1389. [Google Scholar] [CrossRef] [PubMed]
- Schneiter, S.M.; Warrier, R.; Lefkovits, L.; Laurie, C.; O’brien, P.E.; Taylor, A.J. Effects of Weight Loss on Pericardial Fat and Left Ventricular Mass Assessed with Cardiac Magnetic Resonance Imaging in Morbid Obesity. Int. J. Clin. Med. 2011, 2, 360–366. [Google Scholar] [CrossRef]
- van Schinkel, L.D.; Sleddering, M.A.; Lips, M.A.; Jonker, J.T.; de Roos, A.; Lamb, H.J.; Jazet, I.M.; Pijl, H.; Smit, J.W.A. Effects of bariatric surgery on pericardial ectopic fat depositions and cardiovascular function. Clin. Endocrinol. 2014, 81, 689–695. [Google Scholar] [CrossRef] [PubMed]
- Grapsa, J.; Tan, T.C.; Paschou, S.A.; Kalogeropoulos, A.S.; Shimony, A.; Kaier, T.; Demir, O.M.; Mikhail, S.; Hakky, S.; Purkayastha, S.; et al. The effect of bariatric surgery on echocardiographic indices: A review of the literature. Eur. J. Clin. Investig. 2013, 43, 1224–1230. [Google Scholar] [CrossRef]
- Huang, S.; Lan, Y.; Zhang, C.; Zhang, J.; Zhou, Z. The Early Effects of Bariatric Surgery on Cardiac Structure and Function: A Systematic Review and Meta-Analysis. Obes. Surg. 2023, 33, 453–468. [Google Scholar] [CrossRef]
- Mikhalkova, D.; Holman, S.R.; Jiang, H.; Saghir, M.; Novak, E.; Coggan, A.R.; O’Connor, R.; Bashir, A.; Jamal, A.; Ory, D.S.; et al. Bariatric Surgery-Induced Cardiac and Lipidomic Changes in Obesity-Related Heart Failure with Preserved Ejection Fraction. Obesity 2018, 26, 284–290. [Google Scholar] [CrossRef]
- Persson, C.E.; Björck, L.; Lagergren, J.; Lappas, G.; Giang, K.W.; Rosengren, A. Risk of Heart Failure in Obese Patients with and without Bariatric Surgery in Sweden—A Registry-Based Study. J. Card. Fail. 2017, 23, 530–537. [Google Scholar] [CrossRef] [PubMed]
- Sundström, J.; Bruze, G.; Ottosson, J.; Marcus, C.; Näslund, I.; Neovius, M. Weight Loss and Heart Failure: A Nationwide Study of Gastric Bypass Surgery Versus Intensive Lifestyle Treatment. Circulation 2017, 135, 1577–1585. [Google Scholar] [CrossRef] [PubMed]
- Seravalle, G.; Colombo, M.; Perego, P.; Giardini, V.; Volpe, M.; Dell’oro, R.; Mancia, G.; Grassi, G. Long-term sympathoinhibitory effects of surgically induced weight loss in severe obese patients. Hypertension 2014, 64, 431–437. [Google Scholar] [CrossRef] [PubMed]
- Pandey, A.; Patel, K.V.; Vaduganathan, M.; Sarma, S.; Haykowsky, M.J.; Berry, J.D.; Lavie, C.J. Physical Activity, Fitness, and Obesity in Heart Failure with Preserved Ejection Fraction. JACC Heart Fail. 2018, 6, 975–982. [Google Scholar] [CrossRef]
- Tromp, J.; MacDonald, M.R.; Tay, W.T.; Teng, T.-H.K.; Hung, C.-L.; Narasimhan, C.; Shimizu, W.; Ling, L.H.; Ng, T.P.; Yap, J.; et al. Heart Failure with Preserved Ejection Fraction in the Young. Circulation 2018, 138, 2763–2773. [Google Scholar] [CrossRef]
- Zacharias, M.; Joffe, S.; Konadu, E.; Meyer, T.; Kiernan, M.; Lessard, D.; Goldberg, R.J. Clinical epidemiology of heart failure with preserved ejection fraction (HFpEF) in comparatively young hospitalized patients. Int. J. Cardiol. 2016, 202, 918–921. [Google Scholar] [CrossRef]
- Tromp, J.; Shen, L.; Jhund, P.S.; Anand, I.S.; Carson, P.E.; Desai, A.S.; Granger, C.B.; Komajda, M.; McKelvie, R.S.; Pfeffer, M.A.; et al. Age-Related Characteristics and Outcomes of Patients with Heart Failure with Preserved Ejection Fraction. J. Am. Coll. Cardiol. 2019, 74, 601–612. [Google Scholar] [CrossRef]
- Klapholz, M.; Maurer, M.; Lowe, A.M.; Messineo, F.; Meisner, J.S.; Mitchell, J.; Kalman, J.; Phillips, R.A.; Steingart, R.; Brown, E.J.; et al. Hospitalization for heart failure in the presence of a normal left ventricular ejection fraction: Results of the New York Heart Failure Registry. J. Am. Coll. Cardiol. 2004, 43, 1432–1438. [Google Scholar] [CrossRef]
- Melenovsky, V.; Borlaug, B.A.; Rosen, B.; Hay, I.; Ferruci, L.; Morell, C.H.; Lakatta, E.; Najjar, S.S.; Kass, D.A. Cardiovascular features of heart failure with preserved ejection fraction versus nonfailing hypertensive left ventricular hypertrophy in the urban baltimore community: The role of atrial remodeling/dysfunction. J. Am. Coll. Cardiol. 2007, 49, 198–207. [Google Scholar] [CrossRef]
- Borlaug, B.A.; Melenovsky, V.; Russell, S.D.; Kessler, K.; Pacak, K.; Becker, L.C.; Kass, D.A. Impaired chronotropic and vasodilator reserves limit exercise capacity in patients with heart failure and a preserved ejection fraction. Circulation 2006, 114, 2138–2147. [Google Scholar] [CrossRef]
- Ortega, F.B.; Lavie, C.J.; Blair, S.N. Obesity and Cardiovascular Disease. Circ. Res. 2016, 118, 1752–1770. [Google Scholar] [CrossRef] [PubMed]
- Nakajima, T.; Fujioka, S.; Tokunaga, K.; Hirobe, K.; Matsuzawa, Y.; Tarui, S. Noninvasive study of left ventricular performance in obese patients: Influence of duration of obesity. Circulation 1985, 71, 481–486. [Google Scholar] [CrossRef] [PubMed]
- Myasoedova, V.A.; Parisi, V.; Moschetta, D.; Valerio, V.; Conte, M.; Massaiu, I.; Bozzi, M.; Celeste, F.; Leosco, D.; Iaccarino, G.; et al. Efficacy of cardiometabolic drugs in reduction of epicardial adipose tissue: A systematic review and meta-analysis. Cardiovasc. Diabetol. 2023, 22, 23. [Google Scholar] [CrossRef] [PubMed]
- Alpert, M.A.; Lambert, C.R.; Terry, B.E.; Cohen, M.V.; Mulekar, M.; Massey, C.V.; Hashimi, M.; Panayiotou, H.; Mukerji, V. Effect of weight loss on left ventricular diastolic filling in morbid obesity. Am. J. Cardiol. 1995, 76, 1198–1201. [Google Scholar] [CrossRef] [PubMed]
- Alpert, M.A.; Terry, B.E.; Mulekar, M.; Cohen, M.V.; Massey, C.V.; Fan, T.; Panayiotou, H.; Mukerji, V. Cardiac Morphology and left ventricular function in normotensive morbidly obese patients with and without congestive heart failure, and effect of weight loss. Am. J. Cardiol. 1997, 80, 736–740. [Google Scholar] [CrossRef]
- Mørkedal, B.; Vatten, L.J.; Romundstad, P.R.; Laugsand, L.E.; Janszky, I. Risk of myocardial infarction and heart failure among metabolically healthy but obese individuals: HUNT (Nord-Trøndelag Health Study), Norway. J. Am. Coll. Cardiol. 2014, 63, 1071–1078. [Google Scholar] [CrossRef]
- Raffield, L.M.; Howard, A.G.; Graff, M.; Lin, D.; Cheng, S.; Demerath, E.; Ndumele, C.; Palta, P.; Rebholz, C.M.; Seidelmann, S.; et al. Obesity Duration, Severity, and Distribution Trajectories and Cardiovascular Disease Risk in the Atherosclerosis Risk in Communities Study. J. Am. Heart Assoc. 2021, 10, e019946. [Google Scholar] [CrossRef]
- Abdullah, A.; Wolfe, R.; Stoelwinder, J.U.; De Courten, M.; Stevenson, C.; Walls, H.L.; Peeters, A. The number of years lived with obesity and the risk of all-cause and cause-specific mortality. Int. J. Epidemiol. 2011, 40, 985–996. [Google Scholar] [CrossRef]
- Reis, J.P.; Allen, N.; Gunderson, E.P.; Lee, J.M.; Lewis, C.E.; Loria, C.M.; Powell-Wiley, T.M.; Rana, J.S.; Sidney, S.; Wei, G.; et al. Excess body mass index- and waist circumference-years and incident cardiovascular disease: The CARDIA study. Obesity 2015, 23, 879–885. [Google Scholar] [CrossRef]
- Ndumele, C.E.; Cobb, L.; Lazo, M.; Bello, N.; Shah, A.; Nambi, V.; Blumenthal, R.S.; Gerstenblith, G.; Solomon, S.D.; Ballantyne, C.M.; et al. Weight History and Subclinical Myocardial Damage. Clin. Chem. 2018, 64, 201–209. [Google Scholar] [CrossRef]
- Messerli, F.H. Cardiopathy of obesity—A not-so-victorian disease. N. Engl. J. Med. 1986, 314, 378–380. [Google Scholar] [CrossRef] [PubMed]
- Li, H.; Hastings, M.H.; Rhee, J.; Trager, L.E.; Roh, J.D.; Rosenzweig, A. Targeting Age-Related Pathways in Heart Failure. Circ. Res. 2020, 126, 533–551. [Google Scholar] [CrossRef] [PubMed]
- Reddy, Y.N.; Lewis, G.D.; Shah, S.; Obokata, M.; Abou-Ezzedine, O.F.; Fudim, M.; Sun, J.-L.; Chakraborty, H.; McNulty, S.; LeWinter, M.M.; et al. Characterization of the Obese Phenotype of Heart Failure with Preserved Ejection Fraction: A RELAX Trial Ancillary Study. Mayo Clin. Proc. 2019, 94, 1199–1209. [Google Scholar] [CrossRef] [PubMed]
- Adams, K.F.; Leitzmann, M.F.; Ballard-Barbash, R.; Albanes, D.; Harris, T.B.; Hollenbeck, A.; Kipnis, V. Body mass and weight change in adults in relation to mortality risk. Am. J. Epidemiol. 2014, 179, 135–144. [Google Scholar] [CrossRef] [PubMed]
- Zheng, H.; Echave, P.; Mehta, N.; Myrskylä, M. Life-long body mass index trajectories and mortality in two generations. Ann. Epidemiol. 2021, 56, 18–25. [Google Scholar] [CrossRef]

| BMI (kg/m2) | 30–35 | 35–40 | 40–45 | 45–50 |
|---|---|---|---|---|
| Distance (meters) | 561 | 475 | 455 | 417 |
| Study | Study Population | Percent Weight Loss | LVM Decrease | Length of Study |
|---|---|---|---|---|
| Jhaveri et al. [183] | 17 | 32% | 32% | 17 months |
| De Witte et al. [184] | 13 | 31.2% | 15.2% | 12 months |
| Leichman et al. [185] | 22 | 15% | 7.8% | 3 months |
| Rider et al. [182] | 13 | 19% | 10% | 12 months |
| Henry et al. [181] | 62 | 29% | 12% | 1030 Days (33.8 months) |
| Gaborit et al. [186] | 23 | 14.4% | 14.5% | 6 months |
| Schneiter et al. [187] | 11 | 54.7% * | 10% | 15.4 months |
| Van Schinkel et al. [188] | 9 | 17.2% | 4.9% | 16 weeks (3.7 months) |
| Total/Mean | 170 α | 22.5% Ϯ | 13.3% β | 12.9 months β |
Disclaimer/Publisher’s Note: The statements, opinions and data contained in all publications are solely those of the individual author(s) and contributor(s) and not of MDPI and/or the editor(s). MDPI and/or the editor(s) disclaim responsibility for any injury to people or property resulting from any ideas, methods, instructions or products referred to in the content. |
© 2023 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Stencel, J.; Alai, H.R.; Dhore-patil, A.; Urina-Jassir, D.; Le Jemtel, T.H. Obesity, Preserved Ejection Fraction Heart Failure, and Left Ventricular Remodeling. J. Clin. Med. 2023, 12, 3341. https://doi.org/10.3390/jcm12093341
Stencel J, Alai HR, Dhore-patil A, Urina-Jassir D, Le Jemtel TH. Obesity, Preserved Ejection Fraction Heart Failure, and Left Ventricular Remodeling. Journal of Clinical Medicine. 2023; 12(9):3341. https://doi.org/10.3390/jcm12093341
Chicago/Turabian StyleStencel, Jason, Hamid R. Alai, Aneesh Dhore-patil, Daniela Urina-Jassir, and Thierry H. Le Jemtel. 2023. "Obesity, Preserved Ejection Fraction Heart Failure, and Left Ventricular Remodeling" Journal of Clinical Medicine 12, no. 9: 3341. https://doi.org/10.3390/jcm12093341
APA StyleStencel, J., Alai, H. R., Dhore-patil, A., Urina-Jassir, D., & Le Jemtel, T. H. (2023). Obesity, Preserved Ejection Fraction Heart Failure, and Left Ventricular Remodeling. Journal of Clinical Medicine, 12(9), 3341. https://doi.org/10.3390/jcm12093341





