Survival and Recurrence of Endocarditis following Mechanical vs. Biological Aortic Valve Replacement for Endocarditis in Patients Aged 40 to 65 Years: Data from the INFECT-Registry
Abstract
:1. Introduction
2. Materials and Methods
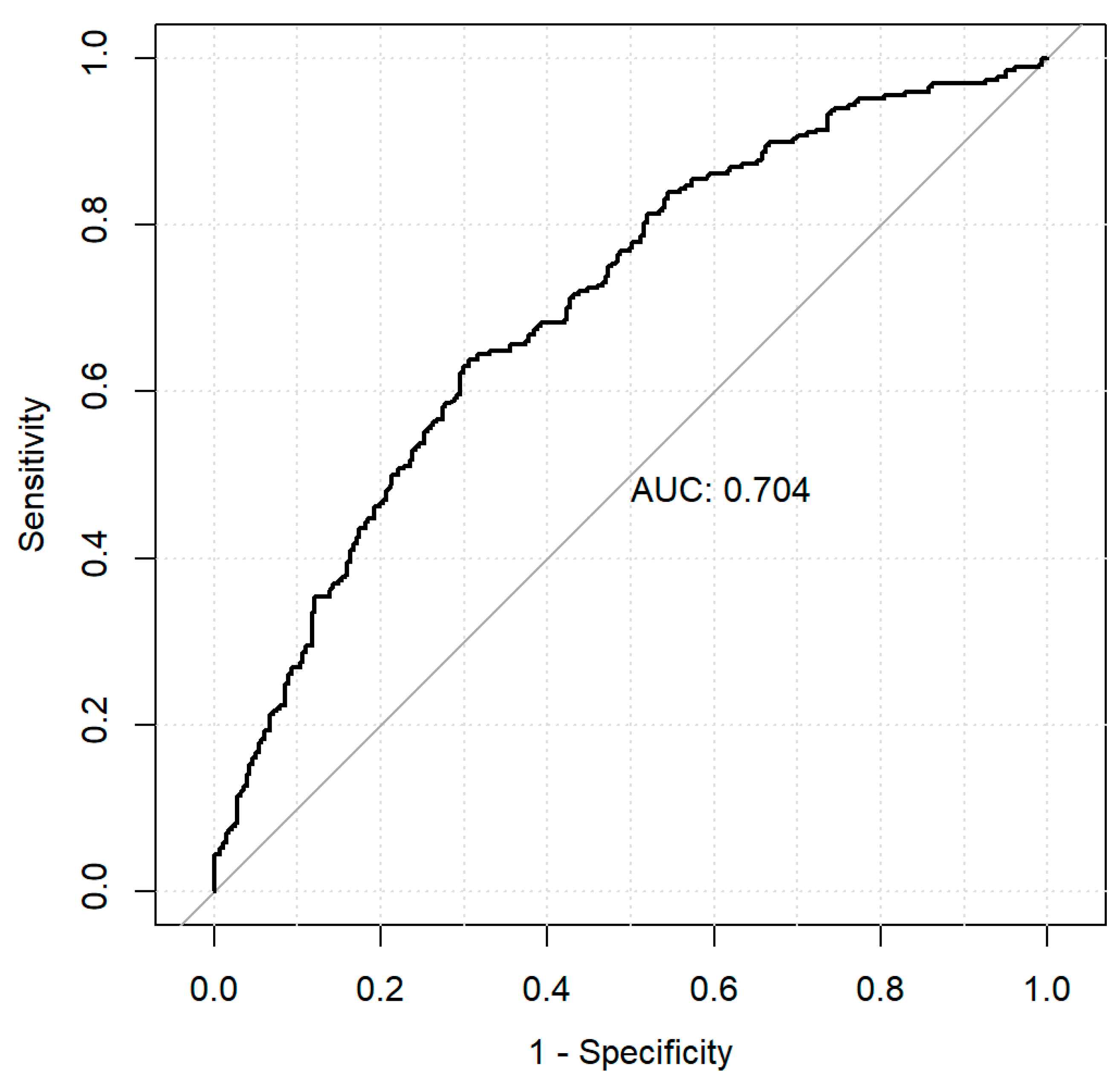
Statistical Analysis
3. Results
3.1. Trends in AVR with Mechanical vs. Biological Valves in Middle-Aged Patients
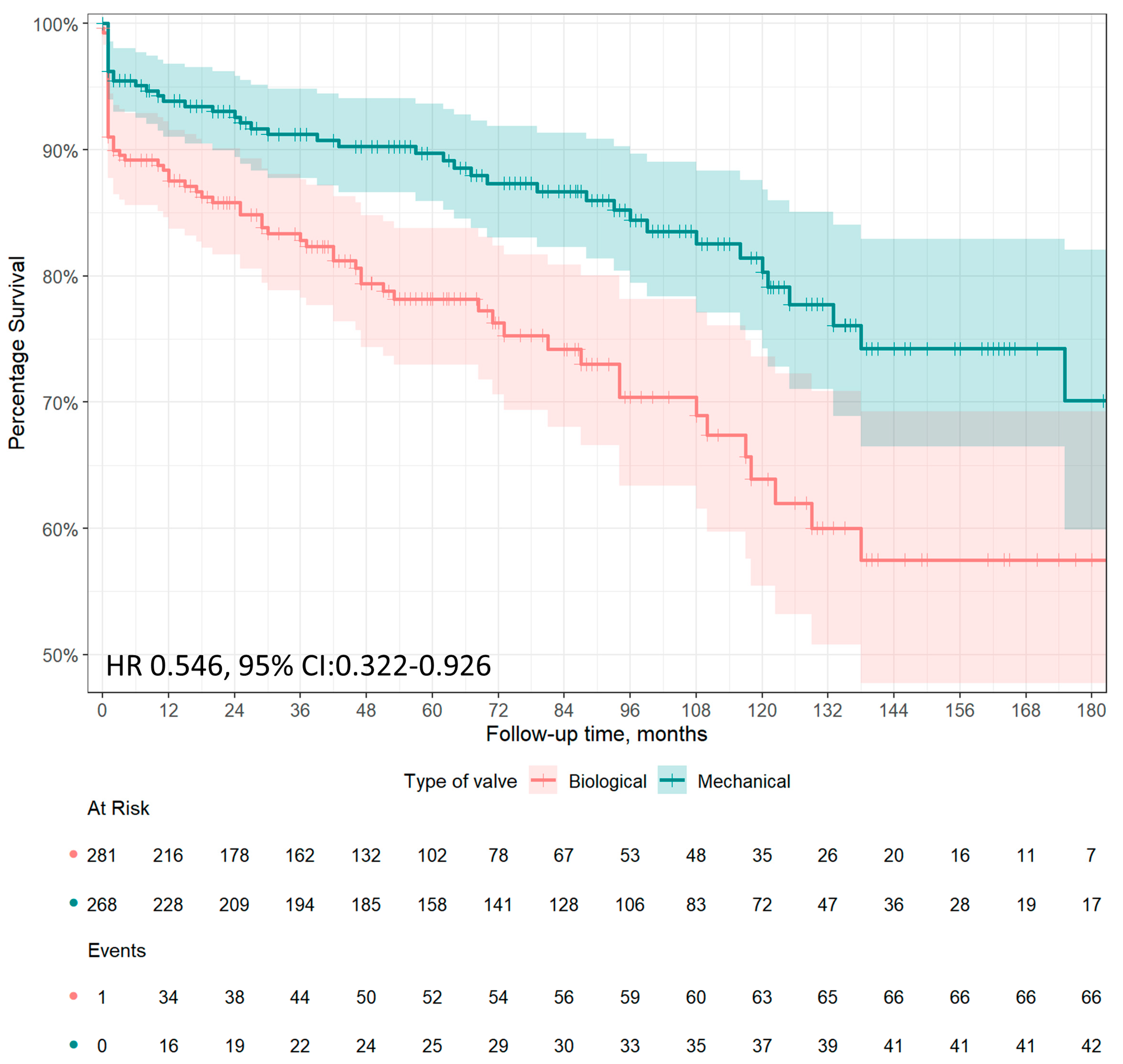
3.2. Long Term Survival
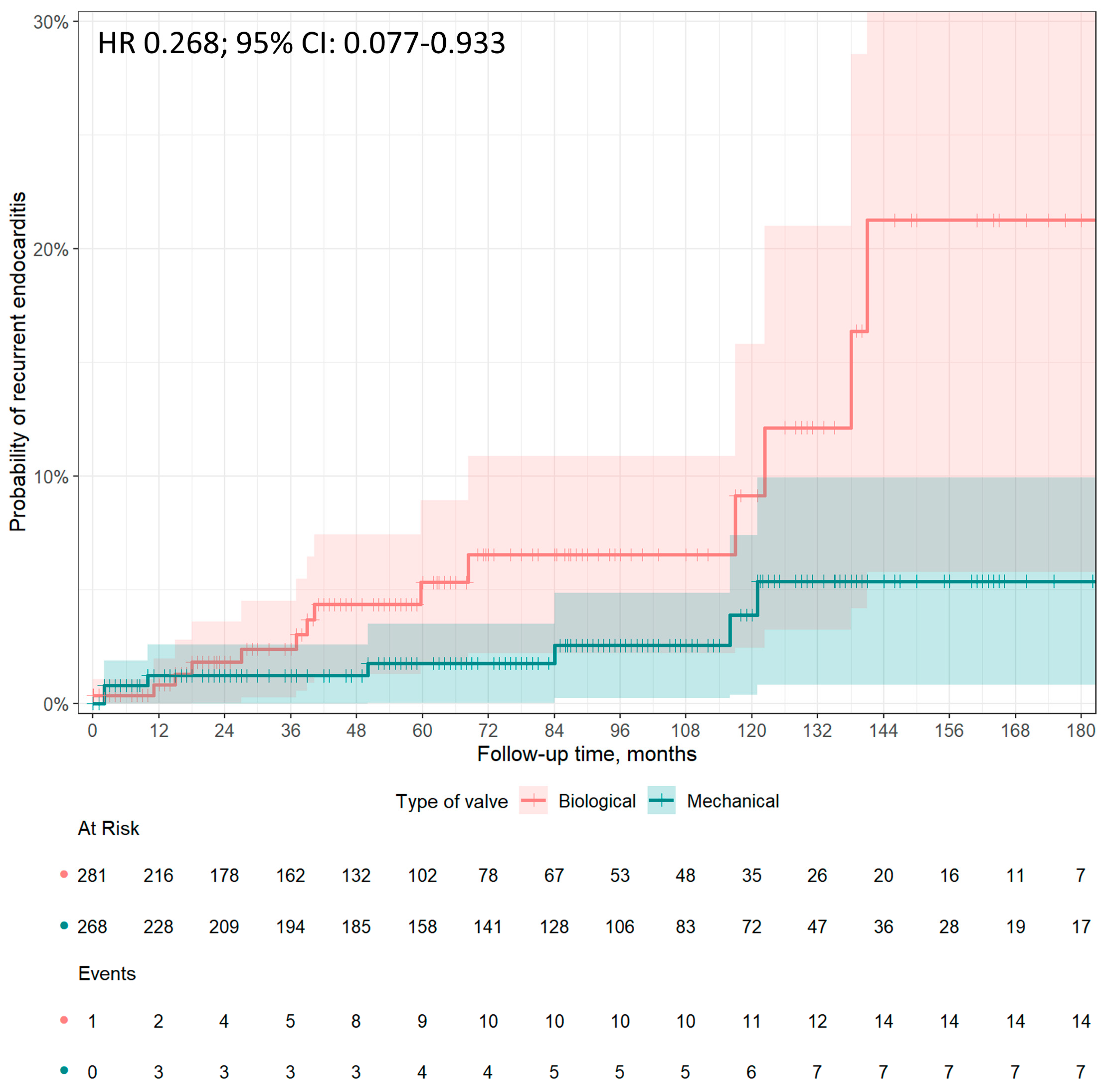
3.3. Recurrence of Endocarditis
3.4. Early Postoperative Complications
4. Discussion
4.1. Preference of Prosthetic Valve Types in Middle-Aged Patients
4.2. Perioperative Outcomes, Long-Term Survival, and Recurrence of IE after AVR for IE in Middle-Aged Patients
4.3. Infective Endocarditis Registries
4.4. Study Limitations
5. Conclusions
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Acknowledgments
Conflicts of Interest
Appendix A
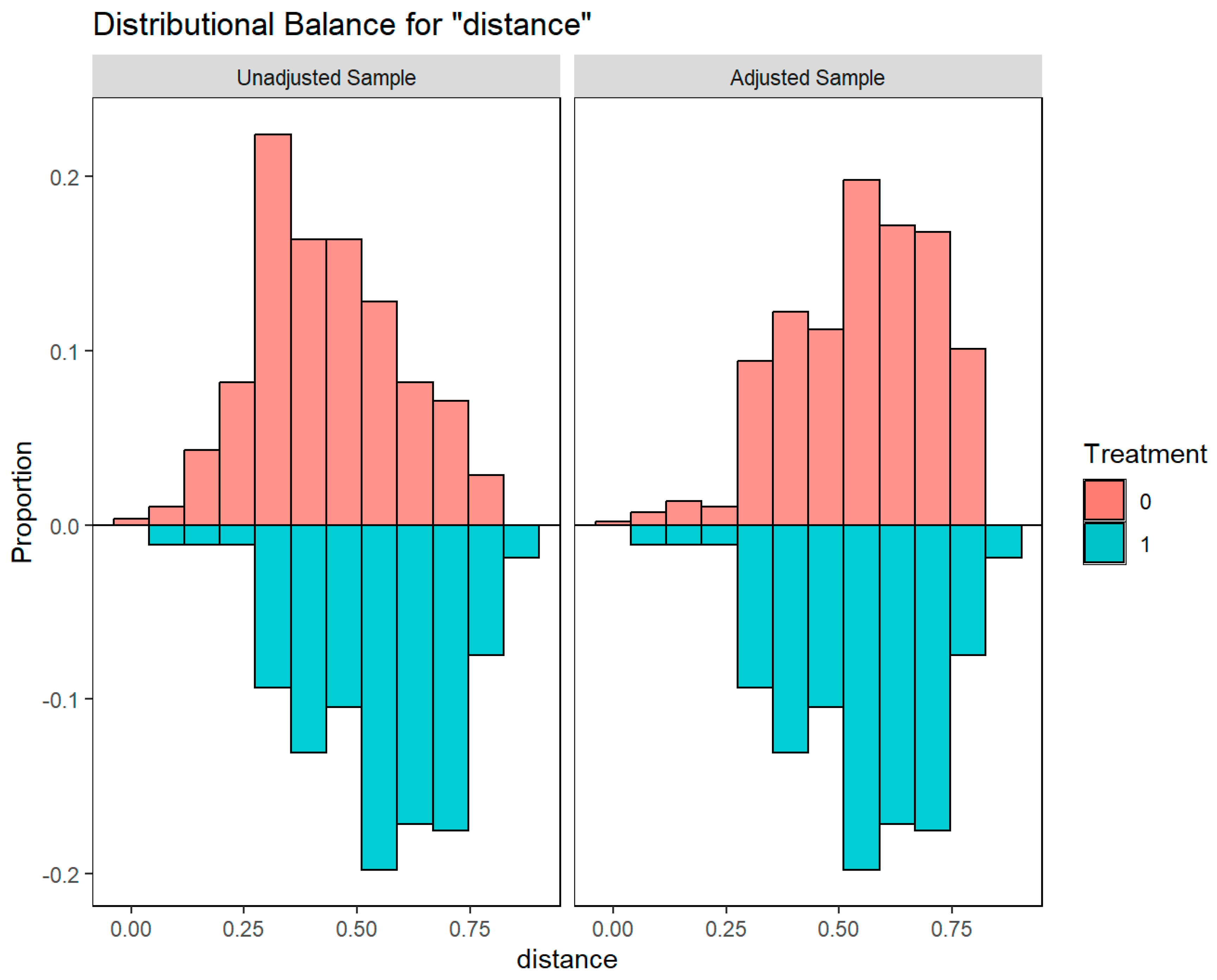

| Variable | Type | Unadjusted Sample | Adjusted Sample | ||||||||||||
|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|
| Biological Valve 281 pts | Mechanical Valve 268 pts | Balance Measures | Biological Valve 281 pts | Mechanical Valve 268 pts | Balance Measures | ||||||||||
| Mean | Standard Deviation | Mean | Standard Deviation | Mean Difference | Variance Ratio | KS | Mean | Standard Deviation | Mean | Standard Deviation | Mean Difference | Variance Ratio | KS | ||
| Distance | 0.4302 | 0.1604 | 0.5489 | 0.1602 | 0.7407 | 0.9974 | 0.3320 | 0.5471 | 0.1577 | 0.5489 | 0.1602 | 0.0109 | 1.0319 | 0.0448 | |
| Age | Contin. | 55.2723 | 7.3493 | 51.7304 | 7.1413 | −0.4960 | 0.9442 | 0.2355 | 51.2162 | 7.1479 | 51.7304 | 7.1413 | 0.0720 | 0.9982 | 0.1008 |
| Female gender | Binary | 0.1423 | . | 0.2388 | . | 0.0965 | . | 0.0965 | 0.2397 | . | 0.2388 | . | −0.0009 | . | 0.0009 |
| S. aureus | Binary | 0.1459 | . | 0.1269 | . | -0.0190 | . | 0.0190 | 0.1712 | . | 0.1269 | . | −0.0443 | . | 0.0443 |
| Hypertension | Binary | 0.2669 | . | 0.2388 | . | −0.0281 | . | 0.0281 | 0.2618 | . | 0.2388 | . | −0.0230 | . | 0.0230 |
| Diabetes | Binary | 0.1139 | . | 0.0858 | . | −0.0281 | . | 0.0281 | 0.0898 | . | 0.0858 | . | −0.0040 | . | 0.0040 |
| Obesity | Binary | 0.0783 | . | 0.0672 | . | −0.0111 | . | 0.0111 | 0.0805 | . | 0.0672 | . | −0.0133 | . | 0.0133 |
| COPD | Binary | 0.0569 | . | 0.0485 | . | −0.0084 | . | 0.0084 | 0.0483 | . | 0.0485 | . | 0.0002 | . | 0.0002 |
| LVEF | Contin. | 54.2206 | 9.4673 | 54.9440 | 8.4539 | 0.0856 | 0.7974 | 0.0925 | 54.4560 | 9.6088 | 54.9440 | 8.4539 | 0.0577 | 0.7741 | 0.0726 |
| Drug abuse | Binary | 0.0463 | . | 0.0522 | . | 0.0060 | . | 0.0060 | 0.0441 | . | 0.0522 | . | 0.0082 | . | 0.0082 |
| Previous cardiac operation | Binary | 0.0498 | . | 0.0299 | . | −0.0200 | . | 0.0200 | 0.0252 | . | 0.0299 | . | 0.0046 | . | 0.0046 |
| IABP | Binary | 0.0178 | . | 0.0037 | . | −0.0141 | . | 0.0141 | 0.0083 | . | 0.0037 | . | −0.0045 | . | 0.0045 |
| Peripheral artery disease | Binary | 0.0463 | . | 0.0299 | . | −0.0164 | . | 0.0164 | 0.0386 | . | 0.0299 | . | −0.0087 | . | 0.0087 |
| Preoperative stroke | Binary | 0.1210 | . | 0.1119 | . | −0.0091 | . | 0.0091 | 0.1172 | . | 0.1119 | . | −0.0052 | . | 0.0052 |
| Cardiogenic shock | Binary | 0.0961 | . | 0.0485 | . | −0.0476 | . | 0.0476 | 0.0920 | . | 0.0485 | . | −0.0434 | . | 0.0434 |
| AMI | Binary | 0.0142 | . | 0.0112 | . | −0.0030 | . | 0.0030 | 0.0270 | . | 0.0112 | . | −0.0158 | . | 0.0158 |
| Active endocarditis | Binary | 0.8043 | . | 0.7649 | . | −0.0393 | . | 0.0393 | 0.8177 | . | 0.7649 | . | −0.0527 | . | 0.0527 |
| Preoperative MV | Binary | 0.0996 | . | 0.0299 | . | −0.0698 | . | 0.0698 | 0.0611 | . | 0.0299 | . | −0.0312 | . | 0.0312 |
| Pulmonary hypertension | Binary | 0.0676 | . | 0.0560 | . | −0.0116 | . | 0.0116 | 0.0526 | . | 0.0560 | . | 0.0034 | . | 0.0034 |
| CKD | Binary | 0.0996 | . | 0.0970 | . | −0.0026 | . | 0.0026 | 0.0980 | . | 0.0970 | . | −0.0010 | . | 0.0010 |
| Abscess | Binary | 0.1530 | . | 0.1007 | . | −0.0523 | . | 0.0523 | 0.1016 | . | 0.1007 | . | −0.0009 | . | 0.0009 |
References
- Citro, R.; Chan, K.-L.; Miglioranza, M.H.; Laroche, C.; Benvenga, R.M.; Furnaz, S.; Magne, J.; Olmos, C.; Paelinck, B.P.; Pasquet, A.; et al. Clinical profile and outcome of recurrent infective endocarditis. Heart 2022, 108, 1729–1736. [Google Scholar] [CrossRef] [PubMed]
- Delgado, V.; Marsan, N.A.; de Waha, S.; Bonaros, N.; Brida, M.; Burri, H.; Caselli, S.; Doenst, T.; Ederhy, S.; Erba, P.A.; et al. 2023 ESC Guidelines for the management of endocarditis. Eur. Heart J. 2023, 44, 3948–4042. [Google Scholar] [CrossRef] [PubMed]
- Vahanian, A.; Beyersdorf, F.; Praz, F.; Milojevic, M.; Baldus, S.; Bauersachs, J.; Capodanno, D.; Conradi, L.; De Bonis, M.; De Paulis, R.; et al. 2021 ESC/EACTS Guidelines for the management of valvular heart disease. Eur. Heart J. 2022, 43, 561–632. [Google Scholar] [CrossRef] [PubMed]
- Kytö, V.; Ahtela, E.; Sipilä, J.; Rautava, P.; Gunn, J. Mechanical versus biological valve prosthesis for surgical aortic valve replacement in patients with infective endocarditis. Interact. Cardiovasc. Thorac. Surg. 2019, 29, 386–392. [Google Scholar] [CrossRef] [PubMed]
- Delahaye, F.; Chu, V.H.; Altclas, J.; Barsic, B.; Delahaye, A.; Freiberger, T.; Gordon, D.L.; Hannan, M.M.; Hoen, B.; Kanj, S.S.; et al. One-year outcome following biological or mechanical valve replacement for infective endocarditis. Int. J. Cardiol. 2015, 78, 117–123. [Google Scholar] [CrossRef] [PubMed]
- Toyoda, N.; Itagaki, S.; Tannous, H.; Egorova, N.N.; Chikwe, J. Bioprosthetic Versus Mechanical Valve Replacement for Infective Endocarditis: Focus on Recurrence Rates. Ann. Thorac. Surg. 2018, 106, 99–106. [Google Scholar] [CrossRef] [PubMed]
- Havers-Borgersen, E.; Butt, J.H.; Østergaard, L.; Bundgaard, H.; Smerup, M.; Bruun, N.E.; Gislason, G.H.; Torp-Pedersen, C.; Køber, L.; Fosbøl, E.L. Recurrent infective endocarditis versus first-time infective endocarditis after heart valve surgery. Clin. Res. Cardiol. 2020, 109, 1342–1351. [Google Scholar] [CrossRef]
- Caus, T.; Chabry, Y.; Nader, J.; Fusellier, J.F.; De Brux, J.L.; for the EpiCard investigators. Trends in SAVR with biological vs. mechanical valves in middle-aged patients: Results from a French large multi-centric survey. Front. Cardiovasc. Med. 2023, 10, 1205770. [Google Scholar] [CrossRef]
- Li, J.S.; Sexton, D.J.; Mick, N.; Nettles, R.; Fowler, V.G., Jr.; Ryan, T.; Bashore, T.; Corey, G.R. Proposed Modifications to the Duke Criteria for the Diagnosis of Infective Endocarditis. Clin. Infect. Dis. 2000, 30, 633–638. [Google Scholar] [CrossRef]
- Nashef, S.; Roques, F.; Michel, P.; Gauducheau, E.; Lemeshow, S.; Salamon, R. European system for cardiac operative risk evaluation (EuroSCORE). Eur. J. Cardio-Thoracic Surg. 1999, 16, 9–13. [Google Scholar] [CrossRef]
- Zhao, Q.-Y.; Luo, J.-C.; Su, Y.; Zhang, Y.-J.; Tu, G.-W.; Luo, Z. Propensity score matching with R: Conventional methods and new features. Ann. Transl. Med. 2021, 9, 812. [Google Scholar] [CrossRef] [PubMed]
- Austin, P.C.; A Stuart, E. Estimating the effect of treatment on binary outcomes using full matching on the propensity score. Stat. Methods Med. Res. 2015, 26, 2505–2525. [Google Scholar] [CrossRef] [PubMed]
- Kong, W.K.; Salsano, A.; Giacobbe, D.R.; A Popescu, B.; Laroche, C.; Duval, X.; Schueler, R.; Moreo, A.; Colonna, P.; Piper, C.; et al. Outcomes of culture-negative vs. culture-positive infective endocarditis: The ESC-EORP EURO-ENDO registry. Eur. Heart J. 2022, 43, 2770–2780. [Google Scholar] [CrossRef] [PubMed]
- Salsano, A.; Giacobbe, D.R.; Sportelli, E.; Olivieri, G.M.; Natali, R.; Prevosto, M.; Del Bono, V.; Viscoli, C.; Santini, F. Aortic cross-clamp time and cardiopulmonary bypass time: Prognostic implications in patients operated on for infective endocarditis. Interact. Cardiovasc. Thorac. Surg. 2018, 27, 328–335. [Google Scholar] [CrossRef] [PubMed]
- Nappi, F.; Nenna, A.; Spadaccio, C.; Singh, S.S.A.; Almazil, A.; Acar, C. The Use of the Cryopreserved Aortic Homograft for Aortic Valve Replacement: Is It Still an Option? J. Cardiovasc. Dev. Dis. 2023, 10, 248. [Google Scholar] [CrossRef] [PubMed]
- Chiang, Y.P.; Chikwe, J.; Moskowitz, A.J.; Itagaki, S.; Adams, D.H.; Egorova, N.N. Survival and Long-term Outcomes Following Bioprosthetic vs. Mechanical Aortic Valve Replacement in Patients Aged 50 to 69 Years. JAMA 2014, 312, 1323–1329. [Google Scholar] [CrossRef] [PubMed]
- Raschpichler, M.; de Waha, S.; Holzhey, D.; Schwarzer, G.; Flint, N.; Kaewkes, D.; Bräuchle, P.T.; Dvir, D.; Makkar, R.; Ailawadi, G.; et al. Valve-in-Valve Transcatheter Aortic Valve Replacement Versus Redo Surgical Aortic Valve Replacement for Failed Surgical Aortic Bioprostheses: A Systematic Review and Meta-Analysis. J. Am. Heart Assoc. 2022, 11, e7965. [Google Scholar] [CrossRef]
- Savage, E.B.; Saha-Chaudhuri, P.; Asher, C.R.; Brennan, J.M.; Gammie, J.S. Outcomes and Prosthesis Choice for Active Aortic Valve Infective Endocarditis: Analysis of The Society of Thoracic Surgeons Adult Cardiac Surgery Database. Ann. Thorac. Surg. 2014, 98, 806–814. [Google Scholar] [CrossRef]
- Formica, F.; Maestri, F.; Gripshi, F.; Gallingani, A.; Grossi, S.; Nicolini, F. Long-Term Outcome of Mechanical and Biological Prostheses in Patients with Left-Side Infective Endocarditis: A Systematic Review and Meta-Analysis. J. Clin. Med. 2021, 10, 4356. [Google Scholar] [CrossRef]
- Nguyen, D.T.; Delahaye, F.; Obadia, J.-F.; Duval, X.; Selton-Suty, C.; Carteaux, J.-P.; Hoen, B.; Alla, F.; for the AEPEI Study Group. Aortic valve replacement for active infective endocarditis: 5-year survival comparison of bioprostheses, homografts and mechanical prostheses. Eur. J. Cardio-Thorac. Surg. 2010, 37, 1025–1032. [Google Scholar] [CrossRef]
- Rubino, A.S.; Della Ratta, E.E.; Galbiati, D.; Ashurov, R.; Galgano, V.L.; Montella, A.P.; De Feo, M.; Della Corte, A. Can prosthesis type influence the recurrence of infective endocar-ditis after surgery for native valve endocarditis? A propensity weighted comparison. Eur. J. Cardiothorac. Surg. 2021, 60, 1388–1394. [Google Scholar] [CrossRef] [PubMed]
- Said, S.M.; Abdelsattar, Z.M.; Schaff, H.V.; Greason, K.L.; Daly, R.C.; Pochettino, A.; Joyce, L.D.; Dearani, J.A. Outcomes of surgery for infective endocarditis: A single-centre experience of 801 patients. Eur. J. Cardio-Thorac. Surg. 2018, 53, 435–439. [Google Scholar] [CrossRef] [PubMed]
- Moon, M.R.; Miller, D.C.; Moore, K.A.; Oyer, P.E.; Mitchell, R.S.; Robbins, R.C.; Stinson, E.B.; Shumway, N.E.; Reitz, B.A. Treatment of endocarditis with valve replacement: The question of tissue versus mechanical prosthesis. Ann. Thorac. Surg. 2001, 71, 1164–1171. [Google Scholar] [CrossRef]
- Potter, D.D.; Sundt, T.M.; Zehr, K.J.; Dearani, J.A.; Daly, R.C.; Mullany, C.J.; McGregor, C.G.; Puga, F.J.; Schaff, H.V.; Orszulak, T.A. Operative risk of reoperative aortic valve replacement. J. Thorac. Cardiovasc. Surg. 2005, 129, 94–103. [Google Scholar] [CrossRef] [PubMed]
- Attias, D.; Nejjari, M.; Nappi, F.; Dreyfus, J.; Eleid, M.F.; Rihal, C.S. How to treat severe symptomatic structural valve deterioration of aortic surgical bioprosthesis: Transcatheter valve-in-valve implantation or redo valve surgery? Eur. J. Cardio-Thorac. Surg. 2018, 54, 977–985. [Google Scholar] [CrossRef] [PubMed]
- Flameng, W.; Herregods, M.-C.; Vercalsteren, M.; Herijgers, P.; Bogaerts, K.; Meuris, B. Prosthesis-Patient Mismatch Predicts Structural Valve Degeneration in Bioprosthetic Heart Valves. Circulation 2010, 121, 2123–2129. [Google Scholar] [CrossRef] [PubMed]
- Kossar, A.P.; George, I.; Gordon, R.; Ferrari, G. Bacterial infiltration and bioprosthetic valve failure: Emerging diagnostics for emerging therapies. J. Thorac. Cardiovasc. Surg. 2019, 159, 1279–1282. [Google Scholar] [CrossRef]
- Escolà-Vergé, L.; Ribera, A.; Ferreira-González, I.; Pericàs, J.M.; Fernández-Hidalgo, N. Strengths and limitations of patient registries in infective endocarditis. Clin. Microbiol. Infect. 2022, 29, 587–592. [Google Scholar] [CrossRef]
- Gaca, J.G.; Sheng, S.; Daneshmand, M.A.; O’brien, S.; Rankin, J.S.; Brennan, J.M.; Hughes, G.C.; Glower, D.D.; Gammie, J.S.; Smith, P.K. Outcomes for endocarditis surgery in North America: A simplified risk scoring system. J. Thorac. Cardiovasc. Surg. 2011, 141, 98–106.e2. [Google Scholar] [CrossRef]
- Bläckberg, A.; Morenius, C.; Olaison, L.; Berge, A.; Rasmussen, M. Infective endocarditis caused by HACEK group bacteria—A registry-based comparative study. Eur. J. Clin. Microbiol. Infect. Dis. 2021, 40, 1919–1924. [Google Scholar] [CrossRef]
- Muñoz, P.; Kestler, M.; De Alarcon, A.; Miro, J.M.; Bermejo, J.; Rodríguez-Abella, H.; Fariñas, M.C.; Belaustegui, M.C.; Mestres, C.; Llinares, P.; et al. Current Epidemiology and Outcome of Infective Endocarditis: A Multicenter, Prospective, Cohort Study. Medicine 2015, 94, e1816. [Google Scholar] [CrossRef] [PubMed]
- Austin, P.C.; Stuart, E.A. Moving towards best practice when using inverse probability of treatment weighting (IPTW) using the propensity score to estimate causal treatment effects in observational studies. Stat. Med. 2015, 34, 3661–3679. [Google Scholar] [CrossRef] [PubMed]

| Variables | Mechanical Valve (N = 268) | Biological Valve (N = 281) | p Value |
|---|---|---|---|
| Age (years, median [IQR]) | 52.00 [45.37, 57.56] | 57.00 [48.74, 62.00] | <0.001 |
| Female gender, n (%) | 64 (23.9) | 40 (14.2) | 0.006 |
| Hypertension, n (%) | 64 (23.9) | 75 (26.7) | 0.510 |
| Diabetes, n (%) | 23 (8.6) | 32 (11.4) | 0.341 |
| Obesity, n (%) | 18 (6.7) | 22 (7.8) | 0.736 |
| COPD, n (%) | 13 (4.9) | 16 (5.7) | 0.802 |
| Drug abuse, n (%) | 14 (5.2) | 13 (4.6) | 0.900 |
| Previous cardiac surgery, n (%) | 8 (3.0) | 14 (5.0) | 0.330 |
| LVEF (%, mean (SD)) | 54.94 (8.45) | 54.22 (9.47) | 0.346 |
| Peripheral arteriopathy, n (%) | 8 (3.0) | 13 (4.6) | 0.436 |
| Preoperative stroke, n (%) | 30 (11.2) | 34 (12.1) | 0.843 |
| Heart failure, n (%) | 28 (10.4) | 59 (21.0) | 0.001 |
| Cardiogenic shock, n (%) | 13 (4.9) | 27 (9.6) | 0.048 |
| Acute myocardial infarction (within 90 days), n (%) | 3 (1.1) | 4 (1.4) | 1.000 |
| Active endocarditis, n (%) | 205 (76.5) | 226 (80.4) | 0.309 |
| Preoperative MV, n (%) | 8 (3.0) | 28 (10.0) | 0.002 |
| Pulmonary hypertension (<50 mmHg), n (%) | 15 (5.6) | 19 (6.8) | 0.697 |
| CKD, n (%) | 26 (9.7) | 28 (10.0) | 1.000 |
| Dialysis, n (%) | 11 (4.1) | 11 (3.9) | 1.000 |
| IABP, n (%) | 1 (0.4) | 5 (1.8) | 0.241 |
| Preoperative pacemaker implantation, n (%) | 2 (0.7) | 6 (2.1) | 0.317 |
| NVE, n (%) | 267 (99.6) | 281 (100) | 1.000 |
| PVE, n (%) | 1 (0.4) | 0 (0.0) | 1.000 |
| Abscess, n (%) | 27 (10.1) | 43 (15.3) | 0.088 |
| Large vegetation (>1 cm), n (%) | 121 (45.1) | 102 (36.3) | 0.043 |
| Leaflet perforation, n (%) | 29 (10.8) | 50 (17.8) | 0.027 |
| Paravalvular leak, n (%) | 1 (0.4) | 1 (0.4) | 1.000 |
| CABG, n (%) | 0.367 | ||
| 0 | 257 (95.9) | 265 (94.3) | |
| 1 | 9 (3.3) | 12 (4.3) | |
| 2 | 1 (0.4) | 4 (1.4) | |
| ≥3 | 1 (0.4) | 0 (0.0) | |
| Logistic Euroscore (median [IQR]) | 4.68 [2.78, 8.90] | 6.45 [3.62, 13.61] | 0.005 |
| Cardiopulmonary bypass time (min, mean (SD)) | 79.26 (33.47) | 90.94 (49.47) | 0.004 |
| Aortic cross-clamp time (min, mean (SD)) | 63.53 (23.62) | 73.39 (34.97) | 0.001 |
| Causative Agent | Mechanical Valve (N = 268) | Biological Valve (N = 281) | p Value |
|---|---|---|---|
| Culture negative endocarditis, n (%) | 84 (31.3) | 83 (29.5) | 0.714 |
| Streptococci, n (%) | 55 (20.5) | 61 (21.7) | 0.814 |
| Staphylococcus aureus, n (%) | 34 (12.7) | 37 (13.5) | 0.600 |
| Viridans group streptococci *, n (%) | 30 (11.2) | 28 (10.0) | 0.742 |
| Coagulase-negative staphylococci *, n (%) | 23 (8.6) | 20 (7.1) | 0.632 |
| Gram-negative bacteria (non HACEK), n (%) | 5 (1.9) | 9 (3.2) | 0.470 |
| Nutritionally variant streptococci *, n (%) | 2 (0.7) | 3 (1.1) | 1.000 |
| Candida spp., n (%) | 2 (0.7) | 1 (0.4) | 0.967 |
| HACEK group *, n (%) | 1 (0.4) | 0 (0.0) | 0.981 |
| Enterococcus faecalis, n (%) | 1 (0.004) | 1 (0.004) | 1.000 |
| Other organisms, n (%) | 32 (11.9) | 37 (13.2) | 0.591 |
| Variables | Overall Series | Estimation in Matched Cohort § | ||||
|---|---|---|---|---|---|---|
| Mechanical Valve (N = 268) | Biological Valve (N = 281) | p Value | Odds Ratio | 95% CI | p Value | |
| Early mortality, n (%) | 11 (4.1) | 23 (8.2) | 0.071 | 0.480 | 0.229–1.005 | 0.052 |
| Sepsis, n (%) | 9 (3.4) | 11 (3.9) | 0.898 | 0.849 | 0.346–2.084 | 0.722 |
| MOF, n (%) | 1 (0.4) | 7 (2.6) | 0.088 | 0.147 | 0.018–1.207 | 0.074 |
| Reoperation for bleeding, n (%) | 7 (2.6) | 11 (3.9) | 0.537 | 0.658 | 0.251–1.724 | 0.395 |
| Pacemaker implantation, n (%) | 4 (1.5) | 7 (2.5) | 0.592 | 0.591 | 0.171–2.042 | 0.406 |
| Atrial fibrillation, n (%) | 16 (6.3) | 42 (15.6) | 0.001 | 0.362 | 0.198–0.662 | <0.0001 |
| IABP, n (%) | 3 (1.1) | 6 (2.1) | 0.544 | 0.517 | 0.128–2.088 | 0.354 |
| Stroke, n (%) | 6 (2.2) | 3 (1.1) | 0.460 | 0.712 | 0.523–8.541 | 0.293 |
| Acute kidney injury, n (%) | 7 (2.6) | 20 (7.1) | 0.024 | 0.349 | 0.145–0.839 | 0.019 |
| Dialysis, n (%) | 1 (0.4) | 4 (1.5) | 0.401 | 0.261 | 0.029–2.350 | 0.231 |
| MV (hours, mean (SD)) | 23.74 (76.34) | 33.56 (82.75) | 0.315 | −9.819 § | 9.763 § | 0.315 § |
| ICU stay (days, median [IQR]) | 2.00 [1.00, 3.00] | 4.00 [2.00, 9.00] | <0.001 | −17.700 § | 13.599 § | 0.194 § |
| Hospital stay (median [IQR]) | 12.00 [8.50, 17.00] | 12.50 [8.00, 19.00] | 0.356 | −2.041 § | 1.367 § | 0.136 § |
Disclaimer/Publisher’s Note: The statements, opinions and data contained in all publications are solely those of the individual author(s) and contributor(s) and not of MDPI and/or the editor(s). MDPI and/or the editor(s) disclaim responsibility for any injury to people or property resulting from any ideas, methods, instructions or products referred to in the content. |
© 2023 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Salsano, A.; Di Mauro, M.; Labate, L.; Della Corte, A.; Lo Presti, F.; De Bonis, M.; Trumello, C.; Rinaldi, M.; Cura Stura, E.; Actis Dato, G.; et al. Survival and Recurrence of Endocarditis following Mechanical vs. Biological Aortic Valve Replacement for Endocarditis in Patients Aged 40 to 65 Years: Data from the INFECT-Registry. J. Clin. Med. 2024, 13, 153. https://doi.org/10.3390/jcm13010153
Salsano A, Di Mauro M, Labate L, Della Corte A, Lo Presti F, De Bonis M, Trumello C, Rinaldi M, Cura Stura E, Actis Dato G, et al. Survival and Recurrence of Endocarditis following Mechanical vs. Biological Aortic Valve Replacement for Endocarditis in Patients Aged 40 to 65 Years: Data from the INFECT-Registry. Journal of Clinical Medicine. 2024; 13(1):153. https://doi.org/10.3390/jcm13010153
Chicago/Turabian StyleSalsano, Antonio, Michele Di Mauro, Laura Labate, Alessandro Della Corte, Federica Lo Presti, Michele De Bonis, Cinzia Trumello, Mauro Rinaldi, Erik Cura Stura, Guglielmo Actis Dato, and et al. 2024. "Survival and Recurrence of Endocarditis following Mechanical vs. Biological Aortic Valve Replacement for Endocarditis in Patients Aged 40 to 65 Years: Data from the INFECT-Registry" Journal of Clinical Medicine 13, no. 1: 153. https://doi.org/10.3390/jcm13010153








