Gastric Outlet Obstruction from Stomach-Containing Groin Hernias: Case Report and a Systematic Review
Abstract
1. Introduction
2. Case Presentation
Case Report
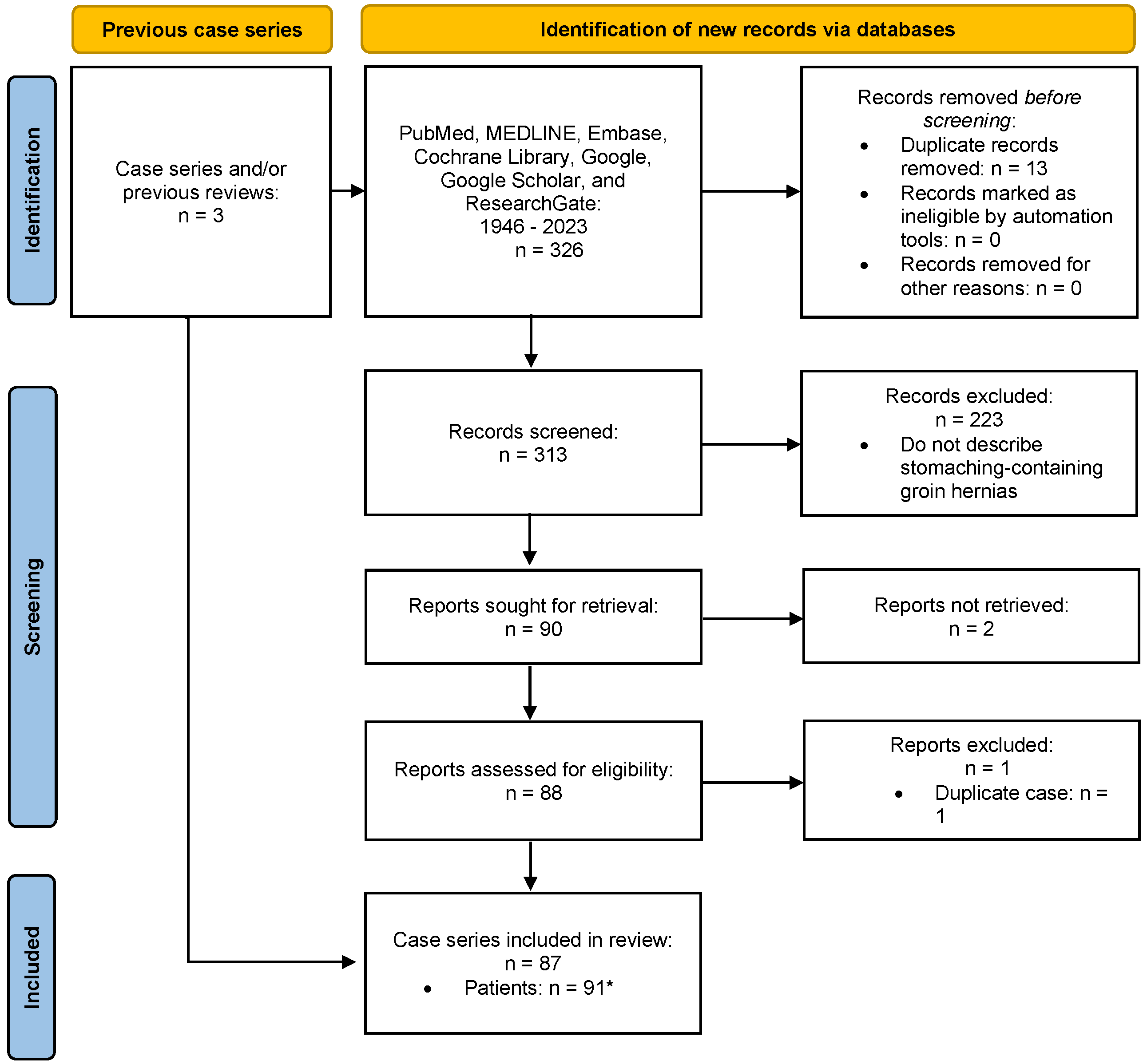
3. Review of the Literature
4. Results
4.1. Review of the Literature
4.1.1. History
4.1.2. Mechanism of Migration
4.1.3. Patient Demographics
| Characteristics | Inguinal (n = 85) | Femoral (n = 6) |
|---|---|---|
| Age [Years (SD) *] | 74.2 (13.0) | 62.0 (11.5) |
| Sex [male (%)] | 95.2 | 33.3 |
| Laterality [Left (%)] | 78.0 | 100.0 |
4.1.4. Management
4.1.5. Complications
4.1.6. Mortality
| n | Reference, Year | Age | Sex | Laterality | Clinical Presentation |
|---|---|---|---|---|---|
| 1 | Lallement, 1802 [21] | 64 | Male | NR | Abdominal pain/discomfort and vomiting |
| 2 | Yvan, 1830 [39] | NR | Male | NR | Vomiting |
| 3 | Febre, 1832 [40] | 73 | Male | Right | No symptoms |
| 4 | Fogt, 1884 [41] | 60 | Male | Left | Vomiting |
| 5 | Schmidt, 1885 [42] | 65 | Male | Left | Hematemesis and inguinal pain |
| 6 | Chiari, 1888 [43] | 74 | Male | Right | No symptoms |
| 7 | Lewin, 1893 [44] | 53 | Male | Left | Emesis and pain |
| 8 | Chevereau, 1894 [45] | 77 | Male | Left | Emesis and pain |
| 9 | Souligoux, 1896 [46] | NR | Male | Left | NR |
| 10 | Brunner, 1897 [30] | 28 | Male | NR | NR |
| 11 | Hilgeneriner, 1910 [47] | 52 | Female | Left | Pain and vomiting |
| 12 | Chambard, 1912 [19] | 62 | Male | Left | Vomiting, pain, and an incarcerated hernia |
| 13 | Rieder, 1915 [48] | 62 | Male | Left | Hematemesis and melena |
| 14 | Ahrens, 1920 [49] | 40 | Male | Right | Pain |
| 15 | Maag, 1920 [50] | 81 | Male | Left | No symptoms |
| 16 | Stokes, 1922 [51] | 42 | Male | Right | Vomiting and an incarcerated hernia |
| 17 | Elischer, 1923 [31] | 53 | Male | Left | Nausea and an incarcerated hernia |
| 18 | Elischer, 1923 [31] | 70 | Male | Left | Incarcerated hernia |
| 19 | Dressen, 1925 [52] | 62 | Male | Left | Vomiting, pain, and inguinal symptoms when eating |
| 20 | de Vernejoul, 1925 [32] | 57 | Female | Left | NR |
| 21 | Sicot, 1927 [33] | 59 | Male | Left | Pain, vomiting, and dyspepsia |
| 22 | Lipkin, 1928 [53] | 60 | Male | Left | Incarcerated hernia |
| 23 | Siegmund, 1929 [54] | NR | Male | Right | NR |
| 24 | Novaro, 1930 [34] | 53 | Male | Right | Vomiting, pain, and an irreducible hernia |
| 25 | Rodzevich, 1935 [55] | 54 | Male | Left | Vomiting and abdominal pain |
| 26 | Oakley, 1937 [56] | 81 | Male | Right | Abdominal and groin pain |
| 27 | Herrmann, 1937 [57] | 80 | Male | Left | Vomiting |
| 28 | Lemaitre, 1937 [58] | 51 | Male | Left | Dyspepsia |
| 29 | Lust, 1937 [59] | 62 | Male | Left | NR |
| 30 | Alexsandrovskiv, 1940 [60] | 73 | Male | Left | Incarcerated hernia |
| 31 | Feldman, 1943 [61] | 66 | Male | Right | No symptoms |
| 32 | Hartley, 1945 [62] | 67 | Male | Left | Dyspepsia |
| 33 | Simmons, 1949 [63] | 66 | Male | Left | Nausea, vomiting, and abdominal pain |
| 34 | Lewis, 1950 [64] | 69 | Male | Right | Occasional vomiting |
| 35 | Anger, 1952 [65] | 74 | Male | Left | Vague symptoms |
| 36 | Bernard, 1953 [66] | NR | NR | NR | NR |
| 37 | Meinterz, 1953 [67] | NR | NR | NR | NR |
| 38 | Davey, 1954 [25] | 61 | Male | Left | Vomiting with markedly distended and tense abdomen |
| 39 | Legrand, 1955 [68] | NR | NR | NR | NR |
| 40 | D’Eshougues, 1956 [69] | NR | NR | NR | NR |
| 41 | Allende, 1956 [70] | NR | NR | NR | NR |
| 42 | Kislenskii, 1959 [71] | NR | NR | Left | NR |
| 43 | Hagarty, 1959 [72] | NR | NR | NR | NR |
| 44 | Ship, 1960 [26] | 83 | Male | Left | Persistent nausea and vomiting |
| 45 | Herrera, 1960 [73] | NR | NR | NR | NR |
| 46 | Jackson, 1964 [74] | NR | NR | NR | Strangulation and perforation of the stomach in the inguinal canal |
| 47 | Falugiani, 1968 a | NR | NR | NR | NR |
| 48 | Gue, 1970 [75] | NR | NR | NR | NR |
| 49 | Soudek, 1975 [76] | NR | NR | NR | NR |
| 50 | Padmanabhan, 1976 [77] | 65 | Male | Left | NR |
| 51 | Nagendran, 1977 [78] | NR | NR | NR | NR |
| 52 | Rozencwajg, 1981 [79] | NR | NR | NR | NR |
| 53 | Udwadia, 1984 [80] | NR | NR | NR | Hematemesis |
| 54 | Quaranta, 1984 [81] | NR | NR | NR | NR |
| 55 | Resente,1986 [82] | NR | NR | NR | NR |
| 56 | Naraynsingh, 1987 [83] | 62 | Male | Left | Recurrent bouts of vomiting, recurrent GOO |
| 57 | Levy, 1987 [84] | 49 | Male | Left | Abdominal pain, nausea, and weight loss |
| 58 | Loizate, 1988 [85] | NR | NR | NR | Upper gastrointestinal tract hemorrhage |
| 59 | Broquet, 1992 [86] | 64 | Female | Bilateral | Perforation of gastric ulcer within the hernia sac |
| 60 | Diaz, 1997 [27] | NR | NR | NR | NR |
| 61 | Diaz, 1997 [27] | NR | NR | NR | NR |
| 62 | Walgenbach, 2001 [87] | 72 | Male | Left | A 6-h history of abdominal distension and pain |
| 63 | Birnbaum, 2011 [88] | 86 | Male | Right | Nausea and vomiting |
| 64 | Dogar, 2011 [89] | 65 | Male | Left | Irreducible groin bulge, abdominal pain, distention, darkish red vomitus, and obstipation |
| 65 | Kerschaever, 2012 [90] | 79 | Male | Left | Anorexia, vomiting, and abdominal distension |
| 66 | Ogul, 2013 [28] | 56 | Male | Left | Recurrent vomiting and bilateral incarcerated groin bulges |
| 67 | Ferdinand, 2013 [38] | 73 | Male | Right | Iron deficiency anemia and gastric volvulus |
| 68 | Fazekas, 2014 [37] | 85 | Male | Left | Three-day history of gastrointestinal obstructive symptoms |
| 69 | Creedon, 2014 [91] | 87 | Male | Left | Colicky abdominal pain for 48 h and vomiting |
| 70 | Patel, 2014 [92] | 85 | Male | Left | 3-day history of profuse vomiting and abdominal pain |
| 71 | Lajevardi, 2015 [35] | 83 | Male | Left | Four-day history of vomiting and constipation |
| 72 | Fitz, 2016 [14] | 46 | Male | Bilateral | Severe abdominal pain after dinner brought in by ambulance to the emergency department |
| 73 | Mora-Guzman, 2016 [93] | 79 | Male | Right | Abdominal pain and vomiting |
| 74 | Periz-Pueyo, 2016 [94] | 61 | Male | Left | Gastric necrosis secondary to an incarcerated inguinal hernia |
| 75 | Nugud, 2017 [95] | 67 | Male | Left | Bilious vomiting with abdominal pain |
| 76 | Sayad, 2019 [96] | 50 | Male | NR | Severe abdominal pain |
| 77 | Junge, 2019 [97] | 75 | Male | Left | Abdominal pain and nausea |
| 78 | Mehta, 2019 [98] | 75 | Male | Left | 5-day history of hematemesis |
| 79 | Heylen, 2020 [36] | 74 | Male | Left | Dark vomitus and generalized abdominal tenderness |
| 80 | Patel, 2021 a | 84 | Male | NR | Nausea, vomiting, constipation, GOO, peritonitis |
| 81 | Vinod, 2021 [99] | 49 | Male | Left | Acute abdominal pain with nausea and dysuria |
| 82 | Alexandre, 2022 [100] | 71 | Male | Left | Nausea, vomiting, constipation, and GOO |
| 83 | Grantham, 2022 [18] | 81 | Male | Lett | Coffee ground emesis |
| 84 | Abbakar, 2022 [101] | 84 | Male | Right | Double GOO, abdominal pain and vomiting |
| 85 | Huerta, 2023 a | 77 | Male | Left | Abdominal pain, nausea, vomiting, and GOO |
| Reference, Year | Age | Sex | Laterality | Clinical Presentation |
|---|---|---|---|---|
| Keller, 1885 [29] | 47 | Female | Left | Abdominal pain and vomiting |
| Spiegel, 1920 [102] | 55 | Female | Left | Gastric strangulation |
| Cave, 1948 [103] | 56 | Female | Left | Dyspepsia |
| Davey, 1954 [25] | 68 | Male | Left | No symptoms |
| Cade, 1984 [104] | 79 | Female | Left | Abdominal pain, emesis, and hematemesis |
| Natsis, 2008 [20] | 67 | Male | Left | Findings at autopsy |
5. Discussion
6. Conclusions
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Conflicts of Interest
References
- Kingsnorth, A.; LeBlanc, K. Hernias: Inguinal and incisional. Lancet 2003, 362, 1561–1571. [Google Scholar] [CrossRef]
- Rutkow, I.M. Epidemiologic, economic, and sociologic aspects of hernia surgery in the United States in the 1990s. Surg. Clin. N. Am. 1998, 78, 941–951. [Google Scholar] [CrossRef]
- Isernia, R.M.; De Luca, G.M.; De Luca, A.; Franzoso, L.; Navazio, L.R.; Caruso, R.; Ferri, V.; Ielpo, B.; Giungato, S. Sliding ureteral inguinal hernia: An uncommon embryological trick. Case report and literature review. Int. J. Surg. Case Rep. 2022, 94, 107006. [Google Scholar] [CrossRef] [PubMed]
- Sugumar, K.; Gupta, M. Anatomy, Abdomen and Pelvis: Inguinal Ligament (Crural Ligament. Poupart Ligament). In StatPearls; StatPearls Publishing: Treasure Island, FL, USA, 2023. [Google Scholar]
- Ponka, J.L.; Brush, B.E. Sliding inguinal hernia in patients over 70 years of age. J. Am. Geriatr. Soc. 1978, 26, 68–73. [Google Scholar] [CrossRef]
- Huerta, S.; Fairbanks, T.; Cinat, M. Incarcerated vesicoinguinal hernia presenting with gross hematuria. J. Am. Coll. Surg. 2005, 201, 992–993. [Google Scholar] [CrossRef] [PubMed]
- Dunn, T.M.; Markgraf, W.H. Littre hernia—Incarcerated Meckel’s diverticulum. Am. J. Surg. 1962, 103, 144–145. [Google Scholar] [CrossRef]
- Michalinos, A.; Moris, D.; Vernadakis, S. Amyand’s hernia: A review. Am. J. Surg. 2014, 207, 989–995. [Google Scholar] [CrossRef] [PubMed]
- Goyal, S.; Shrivastva, M.; Verma, R.; Goyal, S. “Uncommon contents of inguinal hernial sac”: A surgical dilemma. Indian J. Surg. 2015, 77, 305–309. [Google Scholar] [CrossRef]
- Ganesaratnam, M. Maydl’s hernia: Report of a series of seven cases and review of the literature. Br. J. Surg. 1985, 72, 737–738. [Google Scholar] [CrossRef]
- Taveras, L.R.; Huerta, S. A case report of a de Garengeot hernia in a nonagenarian veteran. Int. J. Surg. Case Rep. 2017, 41, 301–303. [Google Scholar] [CrossRef]
- Sidiqi, M.M.; Menezes, G. Asymptomatic herniation of ureter in the routine inguinal hernia: A dangerous trap for general surgeons. Int. J. Surg. Case Rep. 2018, 49, 244–246. [Google Scholar] [CrossRef]
- Aldhafar, A.; Mohammed, A.; Alwabari, M.; Aldhafar, R. A Strangulated Right Inguinal Hernia Containing the Transverse Colon: An Unusual Case Report. Asian J. Case Rep. Surg. 2020, 5, 10–13. [Google Scholar]
- Fitz, E.; Chihara, R.; Stanton-Maxey, K.J. Gastric Perforation Associated with Bilateral Inguinal Hernias. J. Am. Coll. Surg. 2016, 222, e12–e13. [Google Scholar] [CrossRef][Green Version]
- Tajti, J., Jr.; Pieler, J.; Abraham, S.; Simonka, Z.; Paszt, A.; Lazar, G. Incarcerated gallbladder in inguinal hernia: A case report and literature review. BMC Gastroenterol. 2020, 20, 425. [Google Scholar] [CrossRef] [PubMed]
- Chen, G.; Wang, X.; Zhao, Y.; Zhu, L.; Tang, D. Splenogonadal fusion: A case report and review of the literature. BMC Urol. 2021, 21, 16. [Google Scholar] [CrossRef] [PubMed]
- Arredondo Montero, J.; Guillen Redondo, P.; Antona, G.; Bronte Anaut, M. Newborn inguinal hernia containing uterus, ovary and Fallopian tube. An. Pediatría (Engl. Ed.) 2023, 98, 232–233. [Google Scholar] [CrossRef]
- Grantham, T.A.; Ramachandran, R.; Parvataneni, S.; Gaduputi, V. Stomach within a Large Inguinal Hernia. Cureus 2022, 14, e24783. [Google Scholar] [CrossRef] [PubMed]
- Chambard, M.E. La hernie inguinale de l’estomac. Rev. Gynec. d’Obst. 1912, 19, 61–79. [Google Scholar]
- Natsis, K.; Apostolidis, S.; Papadopoulou, A.; Vlasis, K.; Totlis, T.; Skandalakis, P. Gastric femoral hernia in a male cadaver with gastroptosis: Case report and review of the literature. Hernia 2008, 12, 205–208. [Google Scholar] [CrossRef]
- Lallement, L. Observation d’un entero-gastrocele. J. Med. Chir. Pharm. 1802, 1, 329. [Google Scholar]
- Ochoa-Hernandez, A.; Timmerman, C.; Ortiz, C.; Huertas, V.L.; Huerta, S. Emergent groin hernia repair at a County Hospital in Guatemala: Patient-related issues vs. health care system limitations. Hernia 2020, 24, 625–632. [Google Scholar] [CrossRef]
- McInnes, M.D.; Moher, D.; Thombs, B.D.; McGrath, T.A.; Bossuyt, P.M.; Clifford, T.; Cohen, J.F.; Deeks, J.J.; Gatsonis, C.; Hooft, L. Preferred reporting items for a systematic review and meta-analysis of diagnostic test accuracy studies: The PRISMA-DTA statement. JAMA 2018, 319, 388–396. [Google Scholar] [CrossRef]
- Heylen, J.; Campioni-Norman, D.; Lowcock, D.; Varatharajan, L.; Kostalas, M.; Irukulla, M.; Ratnasingham, K. Inguinoscrotal hernias containing stomach: Risk of emergency presentation. Ann. R. Coll. Surg. Engl. 2021, 103, 713–717. [Google Scholar] [CrossRef] [PubMed]
- Davey, W.; Strange, S. The stomach as a content of inguinal and femoral herniae. Br. J. Surg. 1954, 41, 651–658. [Google Scholar] [CrossRef]
- Ship, A.G.; Glick, A.H.; Goldenson, A.B. Incarceration of the stomach in an inguinal hernia: Report of a case. N. Engl. J. Med. 1960, 262, 78–80. [Google Scholar] [CrossRef] [PubMed]
- Diaz Oller, J.; Medina Dominguez, M.T.; Arcos Navarro, A.; Alia Diaz, J.J.; Asanza Llorente, J.A.; Numancia Andreu, M.B.; Nevado Infante, A.; Martos Torres, J.; Moya Vazquez, R.J. Stomach in inguinal-scrotal hernia. Rev. Esp. Enferm. Dig. 1997, 89, 325–328. [Google Scholar]
- Ogul, H.; Yuce, I.; Eren, S.; Kantarci, M. Bilateral inguinal hernia with uncommon content. Can. J. Gastroenterol. 2013, 27, 14. [Google Scholar] [CrossRef] [PubMed]
- Keller, O. Schenkelhernie mit Magen als Inhalt. Inag. Diss. Bern. 1885. [Google Scholar]
- Brunner, F. Kleinere Mittheilungen: Ein Fall von Hernia ventriculi inguinalis incarcerata. Zentralbl. Chir. 1897, 24, 919–921. [Google Scholar]
- Elisscher, E.V. Ibid 1923, 50, 1814.
- de Vernejoul, M.C.; de Luna, D. Sociétés de province: Société de Chirurgie de Marseille: Volumineuse hernie inguinale renfermant l’estomac et les annexes gauches. Pr. Med. 1925, 33, 208. [Google Scholar]
- Sicot, R. Contribu a l’Etude des Hernies inguinales de l’Etomc. These de Paris 1927. [Google Scholar]
- Novaro, N. Arch. Ital. Chir. 1920, 27, 483.
- Lajevardi, S.S.; Gundara, J.S.; Collins, S.A.; Samra, J.S. Acute Gastric Rupture in a Giant Inguinoscrotal Hernia. J. Gastrointest. Surg. 2015, 19, 2283–2285. [Google Scholar] [CrossRef] [PubMed]
- Heylen, J.; Campioni-Norman, D. Bilateral inguinoscrotal hernia with gastric contents and subsequent perforation: Lessons in operative management. Int. J. Surg. Case Rep. 2020, 77, 853–856. [Google Scholar] [CrossRef] [PubMed]
- Fazekas, B.; Frecker, P.; Francis, L.; Patel, K. Aspiration pneumonia as a complication of a rare type of hernia. Int. J. Surg. Case Rep. 2014, 5, 1061–1063. [Google Scholar] [CrossRef] [PubMed][Green Version]
- Ferdinand, E.; Amir, R.; Manjunath, S. Serendipity of giant proportions. Clin. Gastroenterol. Hepatol. 2013, 11, A25–A26. [Google Scholar] [CrossRef]
- Yvan. Arch. Gen. Med. 1830, 22, 139.
- Febre, J.A. These de Paris 1832, 132.
- Fogt, L. Arztl. Zntelligenzbl 1884, 31, 285.
- Schmidt, M. Berl. Klin. Wschr. 1885, 22.
- Chiari, H. Prag. Med. Wschr. 1888, 13, 115.
- Lewin, T.F. Ann. Soc. Belge Chir. 1893, 1.
- Chevereau, P. Bull. Soc. Anat. Paris 1894, 8.
- Souligoux. Bull. Soc. Anat. Paris 1896, 10.
- Hilgenreiner, H. Siltene und bemerkenswerte Hernien. Beitr. Klin. Chir. 1910, 69, 333–430. [Google Scholar]
- Rieder, H. Fortschr. Riintgensrr. 1915, 23.
- Ahrens, P. Zbl. Chir. 1920, 47.
- Maag, O. Dtsh. Z. Chir. 1920, 152.
- Stokes, A.F. Med. F. Aust. 1922, 2.
- Dressen, J. Stomach in Inguinal Hernia. Edinb. Med. J. 1925, 32, 774. [Google Scholar]
- Lipkin, L.N. Odessky Med. J. 1928, 3.
- Siegmund, H. Hand Book de Spesillen Paht. Anat. U. Histo 1929, 4.
- Rodzevich, E.V. Vestn. Khir. Grekov. 1935, 41.
- Oakley, R.H. Strangulation of right inguinal hernia cotaining part of the stomach with simultaneus perforation of a gastric ulcer. Br. J. Surg. 1937, 25, 454–455. [Google Scholar] [CrossRef]
- Herrmann, J. Cas. Lek. Ces 1937, 76.
- Lemaitre, L. Bull. Soc. Radiol. Med. Paris 1937, 25.
- Lust, F.J. Herniation of the stomach into the scrotum. Am. J. Roentgenol. 1937, 37, 666–667. [Google Scholar]
- Alexsandrovskiy, D.G.; Degtyarev, I.G. Vrac. Dyelo 1940, 22.
- Feldman, J.J.M.; TIturrioz, T. Sem. Med. G. Aires 1943, 1.
- Hartley, J.B. Diverticulum of stomach found to enter left inguinal hernial sac. Br. J. Radiol. 1945, 18, 231–232. [Google Scholar] [CrossRef]
- Simmons, H. Perforation of stomach in scrotal hernia. Br. Med. J. 1949, 1, 808. [Google Scholar] [CrossRef] [PubMed][Green Version]
- Lewis, T.F.; Ross, P.S. Inguinal herniation of stomach: Case report. Ohio State Med. J. 1950, 46, 987–988. [Google Scholar] [PubMed][Green Version]
- Anger, H. Extreme Gastroenteroptose bei beiderseitben Scrotalhernien. Fortschr. Roentgenstr. 1952, 76. [Google Scholar] [CrossRef]
- Bernard, A. Inguino-scrotal hernia of the stomach. Arch. Mal. Appar. Dig. Mal. Nutr. 1953, 42, 1400–1403. [Google Scholar] [PubMed]
- Meinertz, O. Inguinal hernia with the stomach functioning as hernial sac content. Fortschr. Geb. Rontgenstr. 1953, 79, 400–401. [Google Scholar] [CrossRef] [PubMed]
- Legrand, J.; Tesson, A. Estomac et hernie scrotale: Présentation de clichés. J. Radiol. Electrol. 1955, 36, 246. [Google Scholar]
- Robert D’Eshougucs, J.; Miniconi, P.; Clerget, O.; Scotto, J.C. Une ptose gastrointestinale peu banale (hernie inguinale de l’estomac). Algérie Mèd. 1956, 60, 1043. [Google Scholar]
- Allende, C.I. Hernia escrotal de estómago. Bol. Trab. Soc. Cir. Buenos Aires 1956, 40, 548–551. [Google Scholar]
- Kislenskii, I.F. Left-sided scrotal inguinal hernia, containing the stomach, cecum, ascending & transverse colon. Khirurgiia 1959, 35, 99–100. [Google Scholar]
- Hagarty, G. The stomach in an inguinal hernia. Med. J. Aust. 1959, 46, 403. [Google Scholar] [CrossRef]
- Herrera, C.A. Large inguinoscrotal hernia containing the stomach. Prensa Med. Argent. 1960, 47, 2443. [Google Scholar]
- Jackson, F.C.; Brown, J.C.; Stiegel, D.D. Strangulation and perforation of the stomach in an inguinal hernia. Am. Surg. 1964, 30, 677–681. [Google Scholar] [PubMed]
- Gue, S. Spontaneous rupture of stomach, a rare complication of inguinal hernia. J. Br. Surg. 1970, 57, 154–155. [Google Scholar] [CrossRef] [PubMed]
- Soudek, K.; Súna, Z. Study of a rare ectopic localization ofthe stomach in a large scrotal hernial. Rozhl. Chir. 1975, 54, 336–337. [Google Scholar] [PubMed]
- Padmanabhan, A.I.; Lowenfels, A.B. Letter: An unusual hernia. JAMA 1976, 235, 2813. [Google Scholar] [CrossRef] [PubMed]
- Nagendran, T. Stomach contained in a giant scrotal hernia. Am. Surg. 1977, 43, 473–476. [Google Scholar] [PubMed]
- Rozencwajg, J. Stomach rupture in inguino-scrotal hernia. Acta Chir. Belg. 1981, 80, 159–160. [Google Scholar] [PubMed]
- Udwadia, T. Stomach strangulated in inguinal hernia presenting with hematemesis. Int. Surg. 1984, 69, 177–179. [Google Scholar]
- Quaranta, M.; Rivetti, R.; Cartia, Q. Rare case of inguino-scrotal hernia containing the stomach. Minerva Chir. 1984, 39, 1757–1759. [Google Scholar]
- Resente, F.; Corbetti, F.; Bettini, F. Inguinal hernia of the stomach. A case. Radiol. Med. 1986, 72, 597–598. [Google Scholar] [PubMed]
- Naraynsingh, V.; Sieunarine, K.; Raju, G. Recurrent gastric outlet obstruction due to an inguinal hernia. Postgrad. Med. J. 1987, 63, 905–906. [Google Scholar] [CrossRef] [PubMed][Green Version]
- Levy, I.; Ebbs, S.R. Inguinal hernia: An unusual cause of dyspepsia. Br. J. Surg. 1987, 74, 363. [Google Scholar] [CrossRef] [PubMed]
- Loizate Totoricaguena, A.; Lamíquiz Vallejo, A. Stomach incarcerated in an inguinal hernia as a cause of upper digestive hemorrhage. Rev. Esp. Enferm. Apar. Dig. 1988, 74, 172–174. [Google Scholar] [PubMed]
- Prêtre, R.; Broquet, P.E.; Robert, J.; Rohner, A. Perforation of gastric ulcer in inguinal hernia. J. Chir. 1992, 129, 218–220. [Google Scholar]
- Walgenbach, K.J.; Lauschke, H.; Brunagel, G.; Hirner, A. An uncommon form of gastric rupture in giant scrotal hernia. Zentralbl Chir. 2001, 126, 1015–1017. [Google Scholar] [CrossRef] [PubMed]
- Birnbaum, D.J.; Grègoire, E.; Campan, P.; Hardwigsen, J.; Le Treut, Y.P. A large inguinoscrotal hernia with stomach content. ANZ J. Surg. 2011, 81, 86–87. [Google Scholar] [CrossRef]
- Dogar, M.; Chaudhary, A. Inguinal hernia containing stomach, transverse colon and small bowel. Pak. J. Med. Health Sci. 2011, 5. [Google Scholar]
- Kerschaever, I.; Poelmans, S.; Vankeirsbilck, J.; Vandewoude, M. Rare cause of gastric outlet obstruction: Incarcerated pylorus within an inguinal hernia. Ann. R. Coll. Surg. Engl. 2012, 94, e46–e48. [Google Scholar] [CrossRef][Green Version]
- Creedon, L.; Peacock, O.; Singh, R.; Awan, A. Gastric outlet obstruction secondary to incarcerated pylorus in an inguinal hernia. Ann. R. Coll. Surg. Engl. 2014, 96, e26–e27. [Google Scholar] [CrossRef]
- Patel, K.; Francis, L.; Fazekas, B.; Panthagani, J. Unusual contents of a large incarcerated inguinal hernia. BMJ Case Rep. 2014. [Google Scholar] [CrossRef]
- Mora-Guzman, I.; Munoz de Nova, J.L.; di Martino, M.; Marin-Perez, E. Antro gástrico como contenido insólito de una hernia inguinal. Rev. Chil. Cir. 2016, 68, 281–282. [Google Scholar] [CrossRef]
- Pueyo Périz, E.M.; Andrés Pérez, S.; García Tejero, A.; García Fernández, C. Gastric necrosis secondary to inguinal incarceration. Cir. Esp. 2016, 94, 180. [Google Scholar] [CrossRef] [PubMed]
- Nugud, A.A.; Nugud, S. Long-standing asymptomatic Inguinoscrotal hernia. Sultan Qaboos Univ. Med. J. 2017, 17, 250–251. [Google Scholar] [CrossRef]
- Sayad, P.; Tan, A.Z. A case report of a gastric perforation in a giant inguinoscrotal hernia: A two-step approach. Int. J. Surg. Case Rep. 2019, 55, 174–178. [Google Scholar] [CrossRef] [PubMed]
- Junge, K.; Otto, J.; Oral, H. A Rare Cause of Gastric Outlet Stenosis—Scrotal Hernia. Dtsch. Ärzteblatt Int. 2019, 116, 507. [Google Scholar] [CrossRef] [PubMed]
- Mehta, T.; Weissman, S.; Vash, A.; Yim, D.; Serrano, O. Gastric Inguinoscrotal Hernia. ACG Case Rep. J. 2019, 6, e00187. [Google Scholar] [CrossRef] [PubMed]
- Vinod, V.C.; Younis, M.U. Gastric strangulation and perforation caused by a giant inguinal-scrotal hernia. Turk. J. Emerg. Med. 2021, 21, 122–124. [Google Scholar] [CrossRef] [PubMed]
- Alexandre, K.; Vandeveer, Z.; Barnwell, J.M.; Vandeveer, Z.T. A Rare Case of Left Inguinoscrotal Hernia Containing Stomach. Cureus 2022, 14, e30838. [Google Scholar] [CrossRef]
- Abbakar, M.; Ahmed, S.; Lim, M. EP-25 Double Gastric Outlet Obstruction Caused by an Incarcerated Right Inguinal Hernia, a Rare Presentation. Br. J. Surg. 2022, 109, znac245-006. [Google Scholar] [CrossRef]
- Spiegel, B. Einklemmung des Magens im Schenkelbruch. Zbl Chir. 1920, 16, 373–374. [Google Scholar]
- Cave, P. Stomach in a Femoral Hernia. Br. J. Radiol. 1948, 21, 143–145. [Google Scholar] [CrossRef]
- Cade, R.J.; Lane, R.H. Strangulated stomach within a femoral hernia. Postgrad. Med. J. 1984, 60, 376. [Google Scholar] [CrossRef][Green Version]

Disclaimer/Publisher’s Note: The statements, opinions and data contained in all publications are solely those of the individual author(s) and contributor(s) and not of MDPI and/or the editor(s). MDPI and/or the editor(s) disclaim responsibility for any injury to people or property resulting from any ideas, methods, instructions or products referred to in the content. |
© 2023 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Favela, J.G.; Argo, M.B.; McAllister, J.; Waldrop, C.L.; Huerta, S. Gastric Outlet Obstruction from Stomach-Containing Groin Hernias: Case Report and a Systematic Review. J. Clin. Med. 2024, 13, 155. https://doi.org/10.3390/jcm13010155
Favela JG, Argo MB, McAllister J, Waldrop CL, Huerta S. Gastric Outlet Obstruction from Stomach-Containing Groin Hernias: Case Report and a Systematic Review. Journal of Clinical Medicine. 2024; 13(1):155. https://doi.org/10.3390/jcm13010155
Chicago/Turabian StyleFavela, Juan G., Madison B. Argo, Jared McAllister, Caitlyn L. Waldrop, and Sergio Huerta. 2024. "Gastric Outlet Obstruction from Stomach-Containing Groin Hernias: Case Report and a Systematic Review" Journal of Clinical Medicine 13, no. 1: 155. https://doi.org/10.3390/jcm13010155
APA StyleFavela, J. G., Argo, M. B., McAllister, J., Waldrop, C. L., & Huerta, S. (2024). Gastric Outlet Obstruction from Stomach-Containing Groin Hernias: Case Report and a Systematic Review. Journal of Clinical Medicine, 13(1), 155. https://doi.org/10.3390/jcm13010155






