Interocular Symmetry of Choroidal Parameters in Patients with Diabetic Retinopathy with and without Diabetic Macular Edema
Abstract
:1. Introduction
2. Materials and Methods
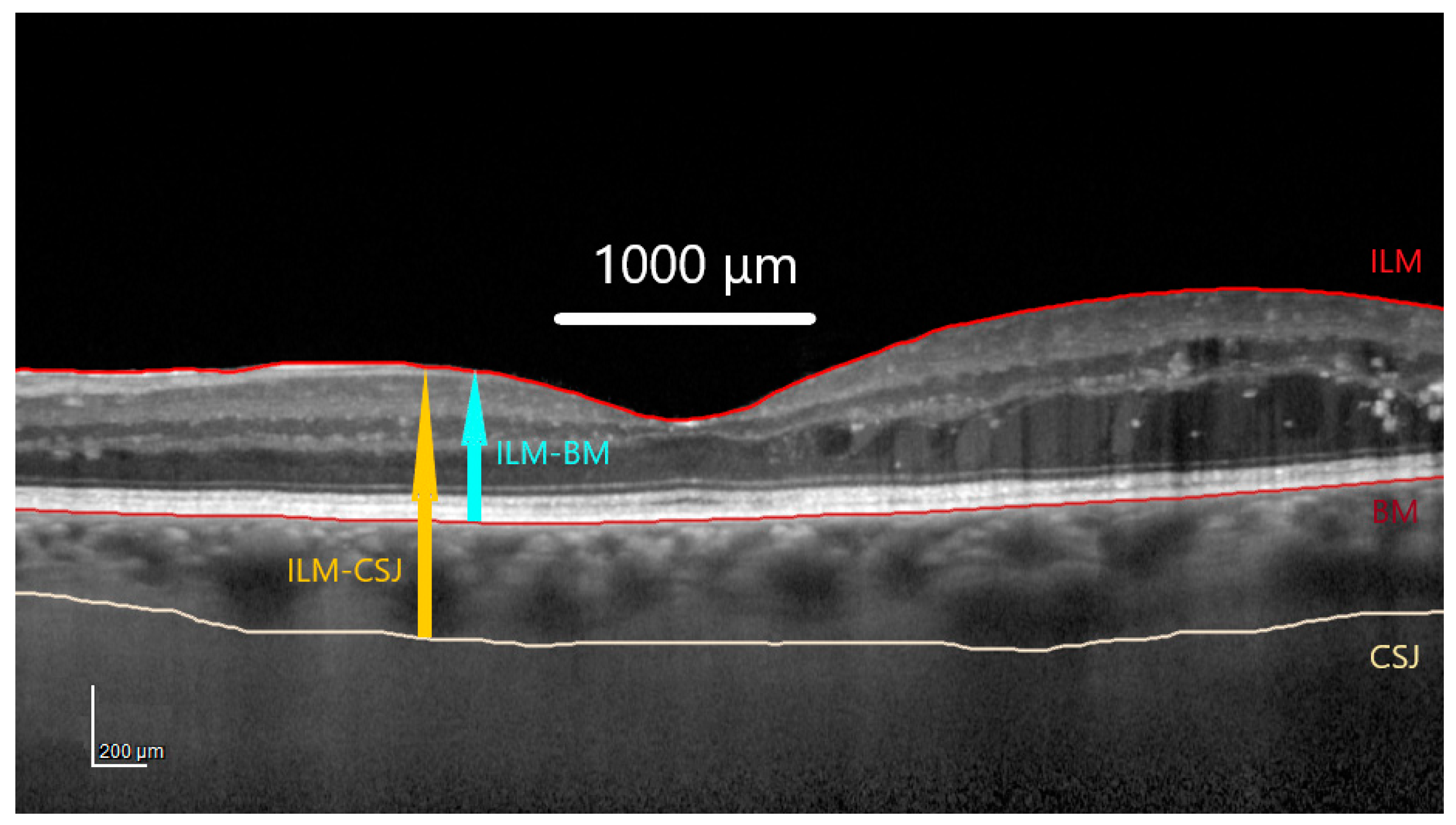
2.1. Optical Coherence Tomography Images Acquisition and Analysis
2.2. Binarization of Subfoveal Choroidal Images
2.3. Statistical Analysis
3. Results
3.1. Baseline Characteristics
3.2. Between-Group Comparison of Choroidal Parameters
4. Discussion
5. Conclusions
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Conflicts of Interest
References
- Hamada, H. Molecular and cellular basis of left-right asymmetry in vertebrates. Proc. Jpn. Acad. Ser. B Phys. Biol. Sci. 2020, 96, 273–296. [Google Scholar] [CrossRef]
- Cameron, J.R.; Megaw, R.D.; Tatham, A.J.; McGrory, S.; MacGillivray, T.J.; Doubal, F.N.; Wardlaw, J.M.; Trucco, E.; Chandran, S.; Dhillon, B. Lateral thinking—Interocular symmetry and asymmetry in neurovascular patterning, in health and disease. Prog. Retin. Eye Res. 2017, 59, 131–157. [Google Scholar] [CrossRef]
- Jiang, J.H.; Pan, X.F.; Lin, Z.; Moonasar, N.; Ye, C.; Zhang, S.D.; Feng, K.M.; Liang, Y.B. Interocular Asymmetry of Visual Field Loss, Intraocular Pressure, and Corneal Parameters in Primary Open-Angle Glaucoma. Ophthalmic Res. 2021, 64, 857–862. [Google Scholar] [CrossRef]
- Sullivan-Mee, M.; Gentry, J.M.; Qualls, C. Relationship between asymmetric central corneal thickness and glaucomatous visual field loss within the same patient. Optom. Vis. Sci. 2006, 83, 516–519. [Google Scholar] [CrossRef]
- Jacobsen, A.G.; Bendtsen, M.D.; Vorum, H.; Bøgsted, M.; Hargitai, J. Normal Value Ranges for Central Retinal Thickness Asymmetry in Healthy Caucasian Adults Measured by SPECTRALIS SD-OCT Posterior Pole Asymmetry Analysis. Investig. Ophthalmol. Vis. Sci. 2015, 56, 3875–3882. [Google Scholar] [CrossRef]
- Song, M.Y.; Hwang, Y.H. Interocular symmetry of optical coherence tomography parameters in healthy children and adolescents. Sci. Rep. 2022, 12, 653. [Google Scholar] [CrossRef]
- Albarrán-Diego, C.; Poyales, F.; López-Artero, E.; Garzón, N.; García-Montero, M. Interocular biometric parameters comparison measured with swept-source technology. Int. Ophthalmol. 2022, 42, 239–251. [Google Scholar] [CrossRef]
- Mann, S.S.; Rutishauser-Arnold, Y.; Peto, T.; Jenkins, S.A.; Leung, I.; Xing, W.; Bird, A.C.; Bunce, C.; Webster, A.R. The symmetry of phenotype between eyes of patients with early and late bilateral age-related macular degeneration (AMD). Graefe’s Arch. Clin. Exp. Ophthalmol. 2011, 249, 209–214. [Google Scholar] [CrossRef]
- Uretmen, O.; Akkin, C.; Erakgün, T.; Killi, R. Color Doppler imaging of choroidal circulation in patients with asymmetric age-related macular degeneration. Ophthalmologica 2003, 217, 137–142. [Google Scholar] [CrossRef] [PubMed]
- Taliaferro, A.S.; Fayed, M.A.; Tsikata, E.; De Luna, R.A.; Jassim, F.; Pandit, S.; Park, E.A.; Aparicio, M.A.G.; Poon, L.Y.; Que, C.; et al. Facilitating glaucoma diagnosis with intereye neuroretinal rim asymmetry analysis using spectral-domain optical coherence tomography. Digit. J. Ophthalmol. 2022, 28, 100–109. [Google Scholar] [CrossRef] [PubMed]
- Fernández-Vigo, J.I.; Rego-Lorca, D.; Moreno-Morillo, F.J.; Burgos-Blasco, B.; Valverde-Megías, A.; Méndez-Hernández, C.; López-Guajardo, L.; Donate-López, J. Intervortex Venous Anastomosis in the Macula in Central Serous Chorioretinopathy Imaged by En Face Optical Coherence Tomography. J. Clin. Med. 2023, 12, 2088. [Google Scholar] [CrossRef] [PubMed]
- Breher, K.; Ohlendorf, A.; Wahl, S. Myopia induces meridional growth asymmetry of the retina: A pilot study using wide-field swept-source OCT. Sci. Rep. 2020, 10, 10886. [Google Scholar] [CrossRef]
- Jiang, Z.; Shen, M.; Xie, R.; Qu, J.; Xue, A.; Lu, F. Interocular evaluation of axial length and retinal thickness in people with myopic anisometropia. Eye Contact Lens. 2013, 39, 277–282. [Google Scholar] [CrossRef] [PubMed]
- Speilburg, A.M.; Teitelbaum, B.; Pang, Y.; Ittiara, S. Symmetry of peripheral retinal nonperfusion in diabetic retinopathy by ischemic index. J. Optom. 2018, 11, 262–267. [Google Scholar] [CrossRef] [PubMed]
- Taylor, E.; Adnitt, P.I.; Jennings, A.M. An analysis of diabetic retinopathy. Q. J. Med. 1973, 42, 305–315. [Google Scholar] [PubMed]
- Laron, M.; Bearse, M.A.; Bronson-Castain, K.; Jonasdottir, S.; King-Hooper, B.; Barez, S.; Schneck, M.E.; Adams, A.J. Interocular symmetry of abnormal multifocal electroretinograms in adolescents with diabetes and no retinopathy. Investig. Ophthalmol. Vis. Sci. 2012, 53, 316–321. [Google Scholar] [CrossRef]
- Iino, K.; Yoshinari, M.; Kaku, K.; Yamamoto, M.; Sato, Y.; Kodama, T.; Iwase, M.; Fujishima, M. Prospective study of asymmetric retinopathy as a predictor of brain infarction in diabetes mellitus. Diabetes Care 1993, 16, 1405–1406. [Google Scholar] [CrossRef]
- Browning, D.J.; Flynn, H.W.; Blankenship, G.W. Asymmetric retinopathy in patients with diabetes mellitus. Am. J. Ophthalmol. 1988, 105, 584–589. [Google Scholar] [CrossRef]
- El Hindy, N.; Ong, J.M. Asymmetric diabetic retinopathy. J. Diabetes 2010, 2, 125–126. [Google Scholar] [CrossRef]
- Choi, J.; Kim, S.J.; Kang, S.W.; Son, K.Y.; Hwang, S. Local ocular factors associated with the development of diabetic macular edema: An inter-eye study. Sci. Rep. 2023, 13, 14868. [Google Scholar] [CrossRef]
- Alsaloum, P.; Russell, M.W.; Blaga, V.; Kuo, B.L.; Wu, A.K.; Liu, B.J.; Valentim, C.C.S.; Xu, C.M.; Muste, J.C.; Kumar, M.; et al. Time to fellow eye involvement in patients with unilateral diabetic macular oedema. Eye 2023, 37, 2761–2767. [Google Scholar] [CrossRef] [PubMed]
- Christoffersen, N.; Larsen, M. Unilateral diabetic macular oedema secondary to central retinal vein congestion. Acta Ophthalmol. Scand. 2004, 82, 591–595. [Google Scholar] [CrossRef] [PubMed]
- Larsen, M. Unilateral macular oedema secondary to retinal venous congestion without occlusion in patients with diabetes mellitus. Acta Ophthalmol. Scand. 2005, 83, 428–435. [Google Scholar] [CrossRef] [PubMed]
- Krasnicki, P.; Dmuchowska, D.A.; Proniewska-Skretek, E.; Dobrzycki, S.; Mariak, Z. Ocular haemodynamics in patients with type 2 diabetes and coronary artery disease. Br. J. Ophthalmol. 2014, 98, 675–678. [Google Scholar] [CrossRef] [PubMed]
- Dmuchowska, D.A.; Krasnicki, P.; Mariak, Z. Can optical coherence tomography replace fluorescein angiography in detection of ischemic diabetic maculopathy? Graefes Arch. Clin. Exp. Ophthalmol. 2014, 252, 731–738. [Google Scholar] [CrossRef]
- Melancia, D.; Vicente, A.; Cunha, J.P.; Abegão Pinto, L.; Ferreira, J. Diabetic choroidopathy: A review of the current literature. Graefes Arch. Clin. Exp. Ophthalmol. 2016, 254, 1453–1461. [Google Scholar] [CrossRef]
- Sidorczuk, P.; Pieklarz, B.; Konopinska, J.; Saeed, E.; Mariak, Z.; Dmuchowska, D. Foveal Avascular Zone Does Not Correspond to Choroidal Characteristics in Patients with Diabetic Retinopathy: A Single-Center Cross-Sectional Analysis. Diabetes Metab. Syndr. Obes. 2021, 14, 2893–2903. [Google Scholar] [CrossRef]
- Pichi, F.; Aggarwal, K.; Neri, P.; Salvetti, P.; Lembo, A.; Nucci, P.; Cheung, C.M.G.; Gupta, V. Choroidal biomarkers. Indian. J. Ophthalmol. 2018, 66, 1716–1726. [Google Scholar] [CrossRef]
- Agrawal, R.; Gupta, P.; Tan, K.A.; Cheung, C.M.; Wong, T.Y.; Cheng, C.Y. Choroidal vascularity index as a measure of vascular status of the choroid: Measurements in healthy eyes from a population-based study. Sci. Rep. 2016, 6, 21090. [Google Scholar] [CrossRef]
- Lu, J.; Zhou, H.; Shi, Y.; Choe, J.; Shen, M.; Wang, L.; Chen, K.; Zhang, Q.; Feuer, W.J.; Gregori, G.; et al. Interocular asymmetry of choroidal thickness and vascularity index measurements in normal eyes assessed by swept-source optical coherence tomography. Quant. Imaging Med. Surg. 2022, 12, 781–795. [Google Scholar] [CrossRef]
- Kim, M.S.; Lim, H.B.; Lee, W.H.; Kim, K.M.; Nam, K.Y.; Kim, J.Y. Wide-Field Swept-Source Optical Coherence Tomography Analysis of Interocular Symmetry of Choroidal Thickness in Healthy Young Individuals. Investig. Ophthalmol. Vis. Sci. 2021, 62, 5. [Google Scholar] [CrossRef] [PubMed]
- Chen, F.K.; Yeoh, J.; Rahman, W.; Patel, P.J.; Tufail, A.; Da Cruz, L. Topographic variation and interocular symmetry of macular choroidal thickness using enhanced depth imaging optical coherence tomography. Investig. Ophthalmol. Vis. Sci. 2012, 53, 975–985. [Google Scholar] [CrossRef] [PubMed]
- Yang, M.; Wang, W.; Xu, Q.; Tan, S.; Wei, S. Interocular symmetry of the peripapillary choroidal thickness and retinal nerve fibre layer thickness in healthy adults with isometropia. BMC Ophthalmol. 2016, 16, 182. [Google Scholar] [CrossRef] [PubMed]
- Al-Haddad, C.; El Chaar, L.; Antonios, R.; El-Dairi, M.; Noureddin, B. Interocular symmetry in macular choroidal thickness in children. J. Ophthalmol. 2014, 2014, 472391. [Google Scholar] [CrossRef] [PubMed]
- Ruiz-Medrano, J.; Flores-Moreno, I.; Peña-García, P.; Montero, J.A.; Duker, J.S.; Ruiz-Moreno, J.M. Asymmetry in macular choroidal thickness profile between both eyes in a healthy population measured by swept-source optical coherence tomography. Retina 2015, 35, 2067–2073. [Google Scholar] [CrossRef] [PubMed]
- Goud, A.; Singh, S.R.; Sahoo, N.K.; Rasheed, M.A.; Vupparaboina, K.K.; Ankireddy, S.; Lupidi, M.; Chhablani, J. New Insights on Choroidal Vascularity: A Comprehensive Topographic Approach. Investig. Ophthalmol. Vis. Sci. 2019, 60, 3563–3569. [Google Scholar] [CrossRef] [PubMed]
- Pietrowska, K.; Dmuchowska, D.A.; Godlewski, A.; Grochowski, E.T.; Wojnar, M.; Gosk, W.; Konopinska, J.; Kretowski, A.; Ciborowski, M. Extent of interocular (a)symmetry based on the metabolomic profile of human aqueous humor. Front. Mol. Biosci. 2023, 10, 1166182. [Google Scholar] [CrossRef] [PubMed]
- Wu, H.; Zhang, G.; Shen, M.; Xu, R.; Wang, P.; Guan, Z.; Xie, Z.; Jin, Z.; Chen, S.; Mao, X.; et al. Assessment of Choroidal Vascularity and Choriocapillaris Blood Perfusion in Anisomyopic Adults by SS-OCT/OCTA. Investig. Ophthalmol. Vis. Sci. 2021, 62, 8. [Google Scholar] [CrossRef]
- Zhao, T.; Laotaweerungsawat, S.; Chen, Y.; Liu, X.; Liu, D.; Stewart, J.M. Right versus left eye asymmetry of microvasculature in diabetes revealed by optical coherence tomography angiography. Sci. Rep. 2023, 13, 9332. [Google Scholar] [CrossRef]
- Grading diabetic retinopathy from stereoscopic color fundus photographs—An extension of the modified Airlie House classification. ETDRS report number 10. Early Treatment Diabetic Retinopathy Study Research Group. Ophthalmology 1991, 98 (Suppl. S5), 786–806.
- Classification of diabetic retinopathy from fluorescein angiograms. ETDRS report number 11. Early Treatment Diabetic Retinopathy Study Research Group. Ophthalmology 1991, 98 (Suppl. S5), 807–822.
- Virgili, G.; Menchini, F.; Casazza, G.; Hogg, R.; Das, R.R.; Wang, X.; Michelessi, M. Optical coherence tomography (OCT) for detection of macular oedema in patients with diabetic retinopathy. Cochrane Database Syst. Rev. 2015, 1, CD008081. [Google Scholar] [CrossRef] [PubMed]
- Dmuchowska, D.A.; Sidorczuk, P.; Pieklarz, B.; Konopińska, J.; Mariak, Z.; Obuchowska, I. Quantitative Assessment of Choroidal Parameters in Patients with Various Types of Diabetic Macular Oedema: A Single-Centre Cross-Sectional Analysis. Biology 2021, 10, 725. [Google Scholar] [CrossRef] [PubMed]
- Sonoda, S.; Sakamoto, T.; Yamashita, T.; Uchino, E.; Kawano, H.; Yoshihara, N.; Terasaki, H.; Shirasawa, M.; Tomita, M.; Ishibashi, T. Luminal and stromal areas of choroid determined by binarization method of optical coherence tomographic images. Am. J. Ophthalmol. 2015, 159, 1123–1131.e1. [Google Scholar] [CrossRef] [PubMed]
- Sonoda, S.; Sakamoto, T.; Yamashita, T.; Shirasawa, M.; Uchino, E.; Terasaki, H.; Tomita, M. Choroidal structure in normal eyes and after photodynamic therapy determined by binarization of optical coherence tomographic images. Investig. Ophthalmol. Vis. Sci. 2014, 55, 3893–3899. [Google Scholar] [CrossRef]
- Sidorczuk, P.; Obuchowska, I.; Konopinska, J.; Dmuchowska, D.A. Correlation between Choroidal Vascularity Index and Outer Retina in Patients with Diabetic Retinopathy. J. Clin. Med. 2022, 11, 3882. [Google Scholar] [CrossRef]
- Agrawal, R.; Ding, J.; Sen, P.; Rousselot, A.; Chan, A.; Nivison-Smith, L.; Wei, X.; Mahajan, S.; Kim, R.; Mishra, C.; et al. Exploring choroidal angioarchitecture in health and disease using choroidal vascularity index. Prog. Retin. Eye Res. 2020, 77, 100829. [Google Scholar] [CrossRef]
- Armstrong, R.A. Statistical guidelines for the analysis of data obtained from one or both eyes. Ophthalmic Physiol. Opt. 2013, 33, 7–14. [Google Scholar] [CrossRef]
- Koo, T.K.; Li, M.Y. A Guideline of Selecting and Reporting Intraclass Correlation Coefficients for Reliability Research. J. Chiropr. Med. 2016, 15, 155–163. [Google Scholar] [CrossRef]
- Chan, Y.H. Biostatistics 104: Correlational analysis. Singapore Med. J. 2003, 44, 614–619. [Google Scholar]
- Iovino, C.; Pellegrini, M.; Bernabei, F.; Borrelli, E.; Sacconi, R.; Govetto, A.; Vagge, A.; Di Zazzo, A.; Forlini, M.; Finocchio, L.; et al. Choroidal Vascularity Index: An In-Depth Analysis of This Novel Optical Coherence Tomography Parameter. J. Clin. Med. 2020, 9, 595. [Google Scholar] [CrossRef] [PubMed]
- Gerendas, B.S.; Waldstein, S.M.; Simader, C.; Deak, G.; Hajnajeeb, B.; Zhang, L.; Bogunovic, H.; Abramoff, M.D.; Kundi, M.; Sonka, M.; et al. Three-dimensional automated choroidal volume assessment on standard spectral-domain optical coherence tomography and correlation with the level of diabetic macular edema. Am. J. Ophthalmol. 2014, 158, 1039–1048. [Google Scholar] [CrossRef] [PubMed]
- Eliwa, T.F.; Hegazy, O.S.; Mahmoud, S.S.; Almaamon, T. Choroidal Thickness Change in Patients with Diabetic Macular Edema. Ophthalmic Surg. Lasers Imaging Retina 2017, 48, 970–977. [Google Scholar] [CrossRef] [PubMed]
- Regatieri, C.V.; Branchini, L.; Carmody, J.; Fujimoto, J.G.; Duker, J.S. Choroidal thickness in patients with diabetic retinopathy analyzed by spectral-domain optical coherence tomography. Retina 2012, 32, 563–568. [Google Scholar] [CrossRef] [PubMed]
- Gupta, C.; Tan, R.; Mishra, C.; Khandelwal, N.; Raman, R.; Kim, R.; Agrawal, R.; Sen, P. Choroidal structural analysis in eyes with diabetic retinopathy and diabetic macular edema-A novel OCT based imaging biomarker. PLoS ONE 2018, 13, e0207435. [Google Scholar] [CrossRef] [PubMed]
- Kase, S.; Endo, H.; Takahashi, M.; Ito, Y.; Saito, M.; Yokoi, M.; Katsuta, S.; Sonoda, S.; Sakamoto, T.; Ishida, S.; et al. Alteration of choroidal vascular structure in diabetic macular edema. Graefe’s Arch. Clin. Exp. Ophthalmol. 2020, 258, 971–977. [Google Scholar] [CrossRef] [PubMed]
- Rewbury, R.; Want, A.; Varughese, R.; Chong, V. Subfoveal choroidal thickness in patients with diabetic retinopathy and diabetic macular oedema. Eye 2016, 30, 1568–1572. [Google Scholar] [CrossRef] [PubMed]
- Vujosevic, S.; Martini, F.; Cavarzeran, F.; Pilotto, E.; Midena, E. Macular and peripapillary choroidal thickness in diabetic patients. Retina 2012, 32, 1781–1790. [Google Scholar] [CrossRef]
- Tan, K.A.; Laude, A.; Yip, V.; Loo, E.; Wong, E.P.; Agrawal, R. Choroidal vascularity index—A novel optical coherence tomography parameter for disease monitoring in diabetes mellitus? Acta Ophthalmol. 2016, 94, e612–e616. [Google Scholar] [CrossRef]
- Cunha-Vaz, J.; Ribeiro, L.; Lobo, C. Phenotypes and biomarkers of diabetic retinopathy. Prog. Retin. Eye Res. 2014, 41, 90–111. [Google Scholar] [CrossRef]
- Daruich, A.; Matet, A.; Moulin, A.; Kowalczuk, L.; Nicolas, M.; Sellam, A.; Rothschild, P.-R.; Omri, S.; Gélizé, E.; Jonet, L.; et al. Mechanisms of macular edema: Beyond the surface. Prog. Retin. Eye Res. 2018, 63, 20–68. [Google Scholar] [CrossRef] [PubMed]
- Singh, S.R.; Vupparaboina, K.K.; Goud, A.; Dansingani, K.K.; Chhablani, J. Choroidal imaging biomarkers. Surv. Ophthalmol. 2019, 64, 312–333. [Google Scholar] [CrossRef] [PubMed]
| Correlation Coefficient (r) | Interpretation | |
|---|---|---|
| +1 | −1 | Perfect |
| +0.9 | −0.9 | Very strong |
| +0.8 | −0.8 | Very strong |
| +0.7 | −0.7 | Moderate |
| +0.6 | −0.6 | Moderate |
| +0.5 | −0.5 | Fair |
| +0.4 | −0.4 | Fair |
| +0.3 | −0.3 | Fair |
| +0.2 | −0.2 | Poor |
| +0.1 | −0.1 | Poor |
| 0 | 0 | None |
| Variables | Overall | Group | p | |||
|---|---|---|---|---|---|---|
| DR+DME− | DR+DME+ | Unilateral DME | Controls | |||
| N of patients | 102 | 40 | 21 | 17 | 24 | - |
| N of eyes | 204 | 80 | 42 | 34 | 48 | - |
| Sex, male (%) | 49 (48.0) | 22 (55.0) | 9 (42.9) | 9 (52.9) | 9 (37.5) | 0.525 |
| Age, years, median (Q1; Q3) | 62.50 (52.00; 68.00) | 59.00 (51.00; 68.00) | 64.50 (55.50; 67.50) | 69.00 (61.00; 71.00) | 58.50 (45.50; 67.25) | 0.113 |
| Spherical equivalent, median (Q1; Q3) | 0.15 (−0.09; 0.85) | 0.06 (−0.25; 0.30) A | 0.02 (−0.12; 1.10) | 0.44 (0.00; 1.51) B | 0.44 (−0.04; 1.13) B | 0.001 |
| DR severity, n (%) | ||||||
| NPDR | 115 (73.7) | 55 (68.8) | 30 (71.4) | 30 (88.2) | - | 0.089 |
| PDR | 41 (26.3) | 25 (31.2) | 12 (28.6) | 4 (11.8) | - | |
| PRP, n (%) | ||||||
| No | 115 (73.7) | 59 (73.8) | 30 (71.4) | 26 (76.5) | - | 0.884 |
| Yes | 41 (26.3) | 21 (26.3) | 12 (28.6) | 8 (23.5) | - | |
| Group | Variable | Mean ± SD Left Eyes | Mean ± SD Right Eyes | Median (Q1; Q3) Left Eyes | Median (Q1; Q3) Right Eyes | Relative Mean Difference (%) between Left and Right Eyes |
|---|---|---|---|---|---|---|
| DR+DME− | Central macular choroidal thickness (µm) | 273.35 ± 58.13 | 269.75 ± 65.17 | 287.00 (239.25; 306.50) | 277.00 (224.75; 321.75) | −4.49 |
| SFCT (µm) | 274.62 ± 59.20 | 267.62 ± 68.57 | 285.00 (252.00; 307.00) | 267.00 (221.25; 317.00) | −5.60 | |
| Central macular choroidal volume (mm3) | 0.22 ± 0.05 | 0.21 ± 0.05 | 0.22 (0.19; 0.24) | 0.22 (0.18; 0.25) | −4.65 | |
| Total choroidal volume (mm3) | 7.40 ± 1.67 | 7.38 ± 1.64 | 7.61 (6.21; 8.36) | 7.63 (6.22; 8.30) | −3.17 | |
| CVI | 0.62 ± 0.05 | 0.60 ± 0.06 | 0.62 (0.58; 0.66) | 0.60 (0.55; 0.64) | −3.33 | |
| LA (mm2) | 1.42 ± 0.43 | 1.38 ± 0.43 | 1.47(1.11; 1.67) | 1.42 (1.05; 1.67) | −5.92 | |
| SCA (mm2) | 0.86 ± 0.21 | 0.92 ± 0.24 | 0.86 (0.75; 1.02) | 0.91 (0.76; 1.1) | 1.72 | |
| TCA (mm2) | 2.29 ± 0.59 | 2.30 ± 0.61 | 2.38 (1.86; 2.69) | 2.32 (1.85; 2.64) | −2.91 | |
| DR+DME+ | Central macular choroidal thickness (µm) | 244.76 ± 51.33 | 250.43 ± 43.66 | 238.00 (220.00; 274.00) | 259.00 (220.00; 276.00) | 2.29 |
| SFCT (µm) | 247.05 ± 54.99 | 252.14 ± 51.15 | 245.00 (214.00; 274.00) | 260.00 (219.00; 283.00) | 2.04 | |
| Central macular choroidal volume (mm3) | 0.19 ± 0.04 | 0.20 ± 0.03 | 0.18 (0.18; 0.21) | 0.20 (0.18; 0.22) | 5.13 | |
| Total choroidal volume (mm3) | 6.66 ± 1.39 | 6.80 ± 1.13 | 6.62 (6.09; 7.41) | 6.78 (6.08; 7.57) | 2.08 | |
| CVI | 0.58 ± 0.05 | 0.57 ± 0.05 | 0.60 (0.52; 0.61) | 0.57 (0.55; 0.61) | −1.74 | |
| LA (mm2) | 1.29 ± 0.39 | 1.29 ± 0.33 | 1.31 (1.03; 1.45) | 1.28 (1.05; 1.6) | 0.46 | |
| SCA (mm2) | 0.93 ± 0.22 | 0.95 ± 0.18 | 0.91 (0.76; 1.05) | 0.91 (0.83; 1.09) | 2.51 | |
| TCA (mm2) | 2.21 ± 0.57 | 2.24 ± 0.46 | 2.2 (1.9; 2.50) | 2.31 (1.87; 2.64) | 1.32 | |
| Unilateral DME * | Central macular choroidal thickness (µm) | * eye with DME 258.53 ± 48.95 | * eye without DME 240.88 ± 59.83 | 255.00 (244.00; 294.00) | 251.00 (185.00; 292.00) | 7.07 |
| SFCT (µm) | 262.71 ± 51.52 | 242.06 ± 59.95 | 263.00 (230.00; 301.00) | 261.00 (190.00; 292.00) | 8.18 | |
| Central macular choroidal volume (mm3) | 0.20 ± 0.04 | 0.19 ± 0.05 | 0.20 (0.19; 0.23) | 0.20 (0.15; 0.23) | 5.41 | |
| Total choroidal volume (mm3) | 6.70 ± 1.45 | 6.49 ± 1.51 | 6.78 (6.00; 7.54) | 6.67 (5.27; 7.32) | 3.23 | |
| CVI | 0.59 ± 0.05 | 0.58 ± 0.05 | 0.60 (0.55; 0.63) | 0.59 (0.56; 0.62) | 0.91 | |
| LA (mm2) | 1.28 ± 0.31 | 1.31 ± 0.34 | 1.23 (1.09; 1.41) | 1.3(1.15; 1.46) | −1.61 | |
| SCA (mm2) | 0.91 ± 0.24 | 0.94 ± 0.26 | 0.99 (0.77; 1.12) | 0.89 (0.81; 1.14) | −3.69 | |
| TCA (mm2) | 2.19 ± 0.51 | 2.25 ± 5.48 | 2.17 (1.80; 2.4) | 2.22 (2.01; 2.53) | −2.47 | |
| Controls | Central macular choroidal thickness (µm) | 306.54 ± 70.51 | 309.08 ± 67.91 | 302.50 (268.00; 348.50) | 310.50 (244.50; 359.00) | 0.83 |
| SFCT (µm) | 304.67 ± 72.33 | 305.38 ± 69.62 | 297.00 (264.50; 332.75) | 303.50 (247.50; 362.75) | 0.23 | |
| Central macular choroidal volume (mm3) | 0.24 ± 0.06 | 0.24 ± 0.05 | 0.24 (0.21; 0.28) | 0.24 (0.19; 0.28) | 0.00 | |
| Total choroidal volume (mm3) | 8.33 ± 1.92 | 8.56 ± 1.92 | 8.25 (7.09; 9.71) | 8.83 (6.96; 10.41) | 2.72 | |
| CVI | 0.63 ± 0.06 | 0.63 ± 0.05 | 0.64 (0.59; 0.68) | 0.63 (0.60; 0.68) | 0.00 | |
| LA (mm2) | 1.58 ± 0.36 | 1.63 ± 0.39 | 1.63 (1.32; 1.81) | 1.67 (1.34; 1.81) | 2.99 | |
| SCA (mm2) | 0.9 ± 0.17 | 0.93 ± 0.184 | 0.88 (0.79; 0.99) | 0.87 (0.79; 1.05) | 3.33 | |
| TCA (mm2) | 2.48 ± 0.45 | 2.56 ± 0.52 | 2.53 (2.35; 2.75) | 2.56 (2.26; 2.82) | 3.11 |
| Variable | ICC between Left and Right Eyes | 95% CI for ICC | r between Left and Right Eyes | p Value for r | p-Value of Wilcoxon Test (w/o Correction) | p-Value of Wilcoxon Test (with Correction) | |
|---|---|---|---|---|---|---|---|
| DR+DME− | Central macular choroidal thickness | 0.803 | 0.657; 0.890 | 0.758 | <0.001 | 0.391 | 0.919 |
| SFCT | 0.705 | 0.509; 0.832 | 0.634 | <0.001 | 0.216 | 0.919 | |
| Central macular choroidal volume | 0.802 | 0.656; 0.890 | 0.768 | <0.001 | 0.488 | 0.919 | |
| Total choroidal volume | 0.906 | 0.827; 0.950 | 0.855 | <0.001 | 0.255 | 0.919 | |
| CVI | 0.774 | 0.489; 0.893 | 0.850 | <0.001 | 0.001 | 0.024 | |
| LA | 0.856 | 0.745; 0.921 | 0.859 | <0.001 | 0.289 | 0.919 | |
| SCA | 0.604 | 0.367; 0.768 | 0.612 | <0.001 | 0.079 | 0.919 | |
| TCA | 0.781 | 0.622; 0.878 | 0.739 | <0.001 | 0.868 | 0.919 | |
| DR+DME+ | Central macular choroidal thickness | 0.842 | 0.656; 0.932 | 0.859 | <0.001 | 0.244 | 0.919 |
| SFCT | 0.817 | 0.605; 0.921 | 0.745 | <0.001 | 0.677 | 0.919 | |
| Central macular choroidal volume | 0.793 | 0.562; 0.910 | 0.796 | <0.001 | 0.267 | 0.919 | |
| Total choroidal volume | 0.880 | 0.727; 0.950 | 0.923 | <0.001 | 0.349 | 0.919 | |
| CVI | 0.522 | 0.119; 0.775 | 0.447 | 0.044 | 0.919 | 0.919 | |
| LA | 0.691 | 0.373; 0.862 | 0.714 | <0.001 | 0.708 | 0.919 | |
| SCA | 0.529 | 0.133; 0.779 | 0.490 | 0.026 | 0.633 | 0.919 | |
| TCA | 0.674 | 0.347; 0.854 | 0.738 | <0.001 | 0.838 | 0.919 | |
| Unilateral DME * | Central macular choroidal thickness | 0.629 | 0.247; 0.846 | 0.639 | 0.007 | 0.187 | 0.374 |
| SFCT | 0.518 | 0.095; 0.790 | 0.539 | 0.028 | 0.170 | 0.374 | |
| Central macular choroidal volume | 0.621 | 0.232; 0.842 | 0.582 | 0.014 | 0.345 | 0.513 | |
| Total choroidal volume | 0.868 | 0.680; 0.950 | 0.787 | <0.001 | 0.449 | 0.513 | |
| CVI | 0.478 | 0.000; 0.775 | 0.333 | 0.191 | 0.963 | 0.963 | |
| LA | 0.727 | 0.387; 0.892 | 0.804 | <0.001 | 0.098 | 0.374 | |
| SCA | 0.837 | 0.614; 0.937 | 0.850 | <0.001 | 0.404 | 0.513 | |
| TCA | 0.849 | 0.638; 0.942 | 0.860 | <0.001 | 0.120 | 0.374 | |
| Controls | Central macular choroidal thickness | 0.802 | 0.593; 0.909 | 0.759 | <0.001 | 0.864 | 0.919 |
| SFCT | 0.761 | 0.519; 0.889 | 0.765 | <0.001 | 0.891 | 0.919 | |
| Central macular choroidal volume | 0.818 | 0.623; 0.917 | 0.800 | <0.001 | 0.881 | 0.919 | |
| Total choroidal volume | 0.854 | 0.696; 0.934 | 0.855 | <0.001 | 0.456 | 0.919 | |
| CVI | 0.724 | 0.457; 0.871 | 0.775 | <0.001 | 0.565 | 0.919 | |
| LA | 0.748 | 0.504; 0.882 | 0.798 | <0.001 | 0.509 | 0.919 | |
| SCA | 0.373 | −0.029; 0.671 | 0.331 | 0.114 | 0.790 | 0.919 | |
| TCA | 0.619 | 0.299; 0.815 | 0.732 | <0.001 | 0.663 | 0.919 |
Disclaimer/Publisher’s Note: The statements, opinions and data contained in all publications are solely those of the individual author(s) and contributor(s) and not of MDPI and/or the editor(s). MDPI and/or the editor(s) disclaim responsibility for any injury to people or property resulting from any ideas, methods, instructions or products referred to in the content. |
© 2023 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Raciborska, A.; Sidorczuk, P.; Konopińska, J.; Dmuchowska, D.A. Interocular Symmetry of Choroidal Parameters in Patients with Diabetic Retinopathy with and without Diabetic Macular Edema. J. Clin. Med. 2024, 13, 176. https://doi.org/10.3390/jcm13010176
Raciborska A, Sidorczuk P, Konopińska J, Dmuchowska DA. Interocular Symmetry of Choroidal Parameters in Patients with Diabetic Retinopathy with and without Diabetic Macular Edema. Journal of Clinical Medicine. 2024; 13(1):176. https://doi.org/10.3390/jcm13010176
Chicago/Turabian StyleRaciborska, Anna, Patryk Sidorczuk, Joanna Konopińska, and Diana Anna Dmuchowska. 2024. "Interocular Symmetry of Choroidal Parameters in Patients with Diabetic Retinopathy with and without Diabetic Macular Edema" Journal of Clinical Medicine 13, no. 1: 176. https://doi.org/10.3390/jcm13010176
APA StyleRaciborska, A., Sidorczuk, P., Konopińska, J., & Dmuchowska, D. A. (2024). Interocular Symmetry of Choroidal Parameters in Patients with Diabetic Retinopathy with and without Diabetic Macular Edema. Journal of Clinical Medicine, 13(1), 176. https://doi.org/10.3390/jcm13010176








