Safety and Feasibility of Intraoperative High PEEP Titrated to the Lowest Driving Pressure (ΔP)—Interim Analysis of DESIGNATION
Abstract
:1. Introduction
2. Materials and Methods
2.1. Design
2.2. Inclusion and Exclusion Criteria
2.3. Data Collected
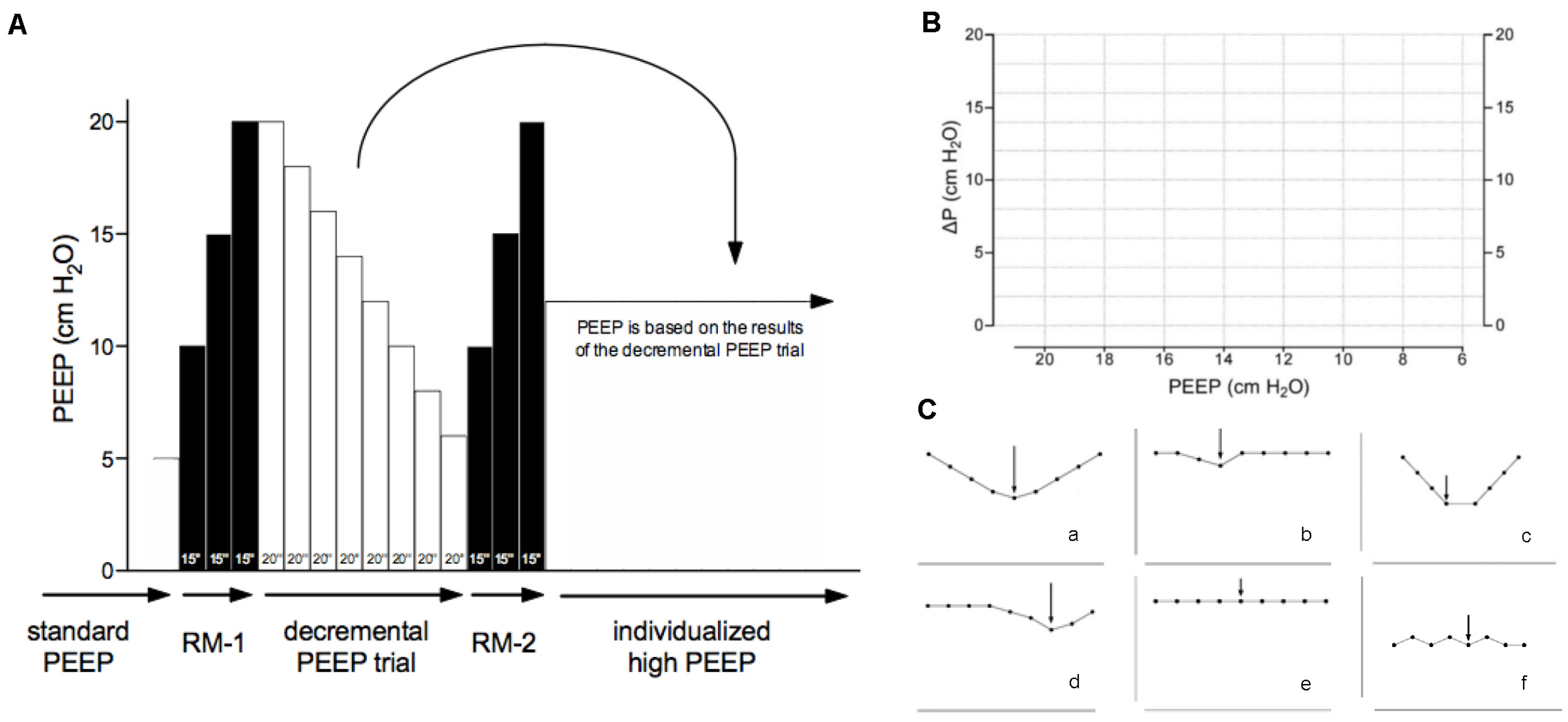
2.4. Interventions
2.5. Rescue Therapies
2.6. Predefined and Allowed Protocol Deviations
2.7. Definitions
2.8. Endpoints
2.9. Sample Size
2.10. Analysis Plan
3. Results
3.1. Patients
3.2. Safety
3.3. Feasibility
3.4. Ventilator Management and Ventilation Parameters
4. Discussion
5. Conclusions
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Conflicts of Interest
Appendix A. The DESIGNATION Investigators
References
- Hemmes, S.N.; Gama de Abreu, M.; Pelosi, P.; Schultz, M.J. High versus low positive end-expiratory pressure during general anaesthesia for open abdominal surgery (PROVHILO trial): A multicentre randomised controlled trial. Lancet 2014, 384, 495–503. [Google Scholar] [CrossRef] [PubMed]
- PROBESE Investigators. Effect of Intraoperative High Positive End-Expiratory Pressure (PEEP) with Recruitment Maneuvers vs Low PEEP on Postoperative Pulmonary Complications in Obese Patients: A Randomized Clinical Trial. JAMA 2019, 321, 2292–2305. [Google Scholar] [CrossRef] [PubMed]
- Pereira, S.M.; Tucci, M.R.; Morais, C.C.A.; Simoes, C.M.; Tonelotto, B.F.F.; Pompeo, M.S.; Kay, F.U.; Pelosi, P.; Vieira, J.E.; Amato, M.B.P. Individual Positive End-expiratory Pressure Settings Optimize Intraoperative Mechanical Ventilation and Reduce Postoperative Atelectasis. Anesthesiology 2018, 129, 1070–1081. [Google Scholar] [CrossRef] [PubMed]
- Serpa Neto, A.; Barbas, C.S.V.; Simonis, F.D.; Artigas-Raventós, A.; Canet, J.; Determann, R.M.; Anstey, J.; Hedenstierna, G.; Hemmes, S.N.T.; Hermans, G.; et al. Epidemiological characteristics, practice of ventilation, and clinical outcome in patients at risk of acute respiratory distress syndrome in intensive care units from 16 countries (PRoVENT): An international, multicentre, prospective study. Lancet Respir. Med. 2016, 4, 882–893. [Google Scholar] [CrossRef] [PubMed]
- Serpa Neto, A.; Amato, M.B.P.; Schultz, M.J. Dissipated Energy is a Key Mediator of VILI: Rationale for Using Low Driving Pressures. In Annual Update in Intensive Care and Emergency Medicine 2016; Vincent, J.-L., Ed.; Springer International Publishing: Cham, Switzerland, 2016; pp. 311–321. [Google Scholar]
- Goligher, E.C.; Ferguson, N.D.; Brochard, L.J. Clinical challenges in mechanical ventilation. Lancet 2016, 387, 1856–1866. [Google Scholar] [CrossRef] [PubMed]
- Pinsky, M.R. The hemodynamic consequences of mechanical ventilation: An evolving story. Intensive Care Med. 1997, 23, 493–503. [Google Scholar] [CrossRef] [PubMed]
- Ferrando, C.; Soro, M.; Unzueta, C.; Suarez-Sipmann, F.; Canet, J.; Librero, J.; Pozo, N.; Peiró, S.; Llombart, A.; León, I.; et al. Individualised perioperative open-lung approach versus standard protective ventilation in abdominal surgery (iPROVE): A randomised controlled trial. Lancet Respir. Med. 2018, 6, 193–203. [Google Scholar] [CrossRef] [PubMed]
- The DESIGNATION–Investigators. Driving Pressure During General Anesthesia for Open Abdominal Surgery (DESIGNATION): Study protocol of a randomized clinical trial. Trials 2020, 21, 198. [Google Scholar] [CrossRef]
- Canet, J. Prediction of Postoperative Pulmonary Complications in a Population-based Surgical Cohort. (ARISCAT study). Anesthesiology 2010, 113, 1338–1350. [Google Scholar] [CrossRef]
- Pagel, P.F.N.; Pratt, P.; Warltier, D. Cardiovascular pharamacology. In Miller’s Anesthesia, 7th ed.; Miller, R.E.L., Fleisher, L., Wiener-Kronish, J., Young, W., Eds.; Elsevier: Philidelphia, PA, USA, 2009. [Google Scholar]
- Reves, J.G.P.; Lubarsky, D.; McEvoy, M.; Martinez-Ruiz, R. Intravenous anesthetics. In Miller’s Anesthesia, 7th ed.; Miller, R.E.L., Fleisher, L., Wiener-Kronish, J., Young, W., Eds.; Elsevier: Philadelphia, PA, USA, 2009; pp. 719–768. [Google Scholar]
- Brown, D. Spinal, epidural and caudal anesthesia. In Miller’s Anesthesia, 7th ed.; Miller, R.E.L., Fleisher, L., Wiener-Kronish, J., Young, W., Eds.; Elsevier: Philadelphia, PA, USA, 2009; pp. 1611–1638. [Google Scholar]
- Futier, E.; Lefrant, J.-Y.; Guinot, P.-G.; Godet, T.; Lorne, E.; Cuvillon, P.; Bertran, S.; Leone, M.; Pastene, B.; Piriou, V.; et al. Effect of Individualized vs Standard Blood Pressure Management Strategies on Postoperative Organ Dysfunction among High-Risk Patients Undergoing Major Surgery: A Randomized Clinical Trial. JAMA 2017, 318, 1346–1357. [Google Scholar] [CrossRef]
- Walsh, M.; Devereaux, P.J.; Garg, A.X.; Kurz, A.; Turan, A.; Rodseth, R.N.; Cywinski, J.; Thabane, L.; Sessler, D.I. Relationship between Intraoperative Mean Arterial Pressure and Clinical Outcomes after Noncardiac Surgery: Toward an Empirical Definition of Hypotension. Anesthesiology 2013, 119, 507–515. [Google Scholar] [CrossRef] [PubMed]
- van Waes, J.A.; van Klei, W.A.; Wijeysundera, D.N.; van Wolfswinkel, L.; Lindsay, T.F.; Beattie, W.S. Association between Intraoperative Hypotension and Myocardial Injury after Vascular Surgery. Anesthesiology 2016, 124, 35–44. [Google Scholar] [CrossRef] [PubMed]
- Salmasi, V.; Maheshwari, K.; Yang, D.; Mascha, E.J.; Singh, A.; Sessler, D.I.; Kurz, A. Relationship between Intraoperative Hypotension, Defined by Either Reduction from Baseline or Absolute Thresholds, and Acute Kidney and Myocardial Injury after Noncardiac Surgery: A Retrospective Cohort Analysis. Anesthesiology 2017, 126, 47–65. [Google Scholar] [CrossRef] [PubMed]
- Sun, L.Y.; Wijeysundera, D.N.; Tait, G.A.; Beattie, W.S. Association of intraoperative hypotension with acute kidney injury after elective noncardiac surgery. Anesthesiology 2015, 123, 515–523. [Google Scholar] [CrossRef] [PubMed]
- Mascha, E.J.; Yang, D.; Weiss, S.; Sessler, D.I. Intraoperative Mean Arterial Pressure Variability and 30-day Mortality in Patients Having Noncardiac Surgery. Anesthesiology 2015, 123, 79–91. [Google Scholar] [CrossRef]
- Monk, T.G.; Bronsert, M.R.; Henderson, W.G.; Mangione, M.P.; Sum-Ping, S.T.; Bentt, D.R.; Nguyen, J.D.; Richman, J.S.; Meguid, R.A.; Hammermeister, K.E. Association between Intraoperative Hypotension and Hypertension and 30-day Postoperative Mortality in Noncardiac Surgery. Anesthesiology 2015, 123, 307–319. [Google Scholar] [CrossRef]
- Bootsma, B.T.; Huisman, D.E.; Plat, V.D.; Schoonmade, L.J.; Stens, J.; Hubens, G.; van der Peet, D.L.; Daams, F. Towards optimal intraoperative conditions in esophageal surgery: A review of literature for the prevention of esophageal anastomotic leakage. Int. J. Surg. 2018, 54 Pt A, 113–123. [Google Scholar] [CrossRef]
- van Rooijen, S.J.; Huisman, D.; Stuijvenberg, M.; Stens, J.; Roumen, R.M.H.; Daams, F.; Slooter, G.D. Intraoperative modifiable risk factors of colorectal anastomotic leakage: Why surgeons and anesthesiologists should act together. Int. J. Surg. 2016, 36 Pt A, 183–200. [Google Scholar] [CrossRef]
- Investigators, L.V. Epidemiology, practice of ventilation and outcome for patients at increased risk of postoperative pulmonary complications: LAS VEGAS—An observational study in 29 countries. Eur. J. Anaesthesiol. 2017, 34, 492–507. [Google Scholar] [CrossRef]
- Park, M.; Ahn, H.J.; Kim, J.A.; Yang, M.; Heo, B.Y.; Choi, J.W.; Kim, Y.R.; Lee, S.H.; Jeong, H.; Choi, S.J.; et al. Driving Pressure during Thoracic Surgery: A Randomized Clinical Trial. Anesthesiology 2019, 130, 385–393. [Google Scholar] [CrossRef]
- Mini, G.; Ray, B.R.; Anand, R.K.; Muthiah, T.; Baidya, D.K.; Rewari, V.; Sahni, P.; Maitra, S. Effect of driving pressure-guided positive end-expiratory pressure (PEEP) titration on postoperative lung atelectasis in adult patients undergoing elective major abdominal surgery: A randomized controlled trial. Surgery 2021, 170, 277–283. [Google Scholar] [CrossRef] [PubMed]





| (A) Rescue strategy for desaturation by group | |||||
| Individualized high PEEP group | Standard low PEEP group | ||||
| Step | PEEP | FiO2 | Step | PEEP | FiO2 |
| 1 | 20 | 0.4 | 1 | 5 | 0.4 |
| 2 | 18 | 0.4 | 2 | 5 | 0.5 |
| 3 | 16 | 0.4 | 3 | 5 | 0.6 |
| 4 | 14 | 0.4 | 4 | 5 | 0.7 |
| 5 | 12 | 0.4 | 5 | 5 | 0.8 |
| 6 | 12 | 0.5 | 6 | 6 | 0.8 |
| 7 | 12 | 0.6 | 7 | RM | |
| 8 | 10 | 0.6 | |||
| 9 | 8 | 0.6 | |||
| 10 | 6 | 0.6 | |||
| 11 | 6 | 0.7 | |||
| 12 | 6 | 0.8 | |||
| Downtitration of PEEP as rescue of desaturation. Starts at level of PEEP set after decremental PEEP trial. | Uptitration of PEEP and recruitment maneuvers (RM) as rescue of desaturation. | ||||
| (B) Pre-approved protocol deviations | |||||
In both groups, the anesthesiologists were allowed to change the ventilation protocol at any time upon surgeons’ request or if there was any concern about the patient’s safety. If one of the following complications occur and are not responding to specific conventional therapy, the level of PEEP could be changed according to any of the following safety concerns that may occur:
| |||||
| Individualized High PEEP (N = 344) | Standard Low PEEP (N = 354) | |
|---|---|---|
| Age, years | 67.0 (57.0–73.0) | 66.0 (57.0–72.8) |
| Female gender | 171/344 (49.7) | 181/354 (51.1) |
| BMI, kg/m2 | 25.5 (23.0–28.7) | 25.4 (22.5–28.4) |
| ARISCAT score | ||
| Intermediate (26–44) | 282/344 (82.0) | 278/354 (78.5) |
| High (>44) | 62/344 (18.0) | 76/354 (21.5) |
| Smoking status | ||
| Never | 147/344 (42.7) | 163/353 (46.2) |
| Former | 138/344 (40.1) | 136/353 (38.5) |
| Current smoker | 59/344 (17.2) | 54/353 (15.3) |
| ASA physical status classification system | ||
| 1 | 23/344 (6.7) | 25/354 (7.1) |
| 2 | 179/344 (52.0) | 205/354 (57.9) |
| 3 | 140/344 (40.7) | 118/354 (33.3) |
| 4 | 2/344 (0.6) | 6/354 (1.7) |
| NYHA classification | ||
| I | 111/344 (32.3) | 100/354 (28.2) |
| II | 23/344 (6.7) | 29/354 (8.2) |
| III | 3/344 (0.9) | 1/354 (0.3) |
| IV | 0/344 (0.0) | 0/354 (0.0) |
| Not applicable | 207/344 (60.2) | 224/354 (63.3) |
| Functional status | ||
| Non-dependent | 324/344 (94.2) | 338/354 (95.5) |
| Partly dependent | 19/344 (5.5) | 13/354 (3.7) |
| Totally dependent | 1/344 (0.3) | 3/354 (0.8) |
| History of active cancer | 248/344 (72.1) | 249/354 (70.3) |
| History of chronic obstructive pulmonary disease | 20/344 (5.8) | 21/354 (5.9) |
| With inhalation therapy | 15/20 (75.0) | 10/21 (47.6) |
| With systemic steroids | 1/20 (5.0) | 2/19 (10.5) |
| History of diabetes mellitus. | 40/344 (11.6) | 50/354 (14.1) |
| Dietary adjustments | 3/40 (7.5) | 1/50 (2.0) |
| With oral medication | 21/40 (52.5) | 22/50 (44.0) |
| With insulin | 8/40 (20.0) | 13/50 (26.0) |
| No medication | 2/40 (5.0) | 3/50 (6.0) |
| Combination of oral and insulin | 7/40 (17.5) | 10/50 (20.0) |
| History of coronary disease | 13/344 (3.8) | 10/354 (2.8) |
| History of persistent ventricular tachycardia’s | 0/343 (0.0) | 1/353 (0.3) |
| Preoperative testing | ||
| Blood test | ||
| Hb, mmol/L | 8.1 (7.3–8.9) | 8.1 (7.0–8.9) |
| Creatinine, µmol/L | 75.0 (63.0–91.0) | 72.0 (61.0–87.0) |
| Urea, mmol/L | 6.0 (4.8–7.8) | 6.3 (4.5–8.1) |
| White Blood Cell count, ×109 cells/L | 7.1 (5.9–8.8) | 7.1 (5.6–9.2) |
| Preoperative SpO2 *, % | 98.0 (96.0–99.0) | 98.0 (97.0–99.0) |
| Preoperative transfusion | 3/344 (0.9) | 1/354 (0.3) |
| Abnormalities on chest imaging | 12/119 (10.1) | 23/131 (17.6) |
| Perioperative variables | ||
| Duration of surgery ¥, minutes | 229.0 (153.5–311.5) | 211.5 (156.5–289.8) |
| Duration of anesthesia ≠, minutes | 270.0 (192.5–362.5) | 255.0 (190.3–338.0) |
| Type of anesthesia | ||
| Volatile | 84/344 (24.4) | 83/354 (23.4) |
| Totally intravenous | 204/344 (59.3) | 220/354 (62.1) |
| Mixed (volatile and intravenous) | 56/344 (16.3) | 51/354 (14.4) |
| Use of Epidural | 224/344 (65.1) | 241/354 (68.1) |
| Thoracic | 216/224 (96.4) | 229/241 (95.0) |
| Lumbar | 8/224 (3.6) | 11/241 (4.6) |
| Individualized High PEEP (N = 344) | Standard Low PEEP (N = 354) | Absolute Risk Difference (95% CI) | Relative Risk Ratio (95% CI) ¥ | p Value * | |
|---|---|---|---|---|---|
| Hypotension | 187/342 (54.7) | 156/354 (44.1) | 10.6 (3.2 to 18.0) | 1.2 (1.1 to 1.4) | 0.006 |
| Need for Vasopressors | 109/342 (31.9) | 71/351 (20.2) | 11.7 (5.1 to 18.2) | 1.6 (1.2 to 2.0) | 0.001 |
| Heart Arrhythmias | 4/342 (1.2) | 2/349 (0.6) | 0.6 (−0.8 to 2.0) | 2.0 (0.4 to 11.1) | 0.447 |
| Individualized High PEEP (N = 344) | Standard Low PEEP (N = 354) | |
|---|---|---|
| Overall compliance *, patients | ||
| no protocol violations, n/N (%) | 285/344 (82.8) | 345/354 (97.5) |
| protocol violations, n/N (%) | 59/344 (17.2) | 9/354 (2.5) |
| RM and PEEP titration, patients | ||
| first RM, n/N (%) | 344/344 (100) | NA |
| PEEP titration, n/N (%) | 342/344 (99.4) | NA |
| second RM, n/N (%) | 344/344 (100) | NA |
| RM before tracheal extubation, n/N (%) | 306/344 (89.0) | NA |
| RM after disconnection, n/N (%) | 10/344 (2.9) | NA |
| RM as rescue, n/N (%) | NA | 2/354 |
| Nadir in ΔP, patients, n/N (%) | 290/343 (84.5) | NA |
| ΔP at nadir, cm H2O | 7.0 (6.0–8.0) | NA |
| PEEP at nadir, cm H2O | 10.0 (10.0–12.0) | NA |
| PEEP settings, patients | ||
| PEEP set correctly, n/N (%) | 309/344 (89.8) | 350/354 (98.9) |
| PEEP, cm H2O | 10.0 (8.0–12.0) | 5.0 (5.0–5.0) |
| PEEP set too high, n/N (%) | 2/344 (0.6) | 3/354 (0.8) |
| 0–2 cm H2O, n/N (%) | 2/344 (0.6) | 2/354 (0.6) |
| PEEP, cm H2O | 15.0 (14.5–15.5) | 6.0 (6.0–6.0) |
| 2–4 cm H2O, n/N (%) | 0/344 (0.0) | 1/354 (0.3) |
| PEEP, cm H2O | NA | 8.0 (8.0–8.0) |
| 4–6 cm H2O, n/N (%) | 0/344 (0.0) | 0/354 (0.0) |
| PEEP, cm H2O | NA | NA |
| PEEP set too low, n/N (%) | 33/344 (9.6) | 1/354 (0.3) |
| 0–2 cm H2O, n/N (%) | 7/344 (2.0) | 1/354 (0.3) |
| PEEP, cm H2O | 10 (9.0–10.0) | 4.0 (4.0–4.0) |
| 2–4 cm H2O, n/N (%) | 12/344 (3.4) | 0/354 (0.0) |
| PEEP, cm H2O | 8.0 (7.5–8.0) | NA |
| 5–6 cm H2O, n/N (%) | 8/344 (2.3) | 0/354 (0.0) |
| PEEP, cm H2O | 6.0 (6.0–6.5) | NA |
| >6 cm H2O, n/N (%) | 6/344 (1.7) | 0/354 (0.0) |
| PEEP, cm H2O | 7.0 (6.0–8) | NA |
| Individualized High PEEP (N = 344) | Standard Low PEEP * (N = 354) | p Value | |
|---|---|---|---|
| PEEP, cm H2O | 10.0 (8.0–12.0) | 5.0 (5.0–5.0) | <0.001 |
| ΔP, cm H2O | 7.0 (6.0–8.8) | 9.0 (8.0–11.0) | <0.001 |
| Pplat, cm H2O | 17.0 (15.0–20.0) | 14.0 (13.0–16.0) | <0.001 |
| Ppeak, cm H2O | 21.0 (19.0–24.0) | 18.0 (16.0–20.0) | <0.001 |
| VT, mL/kg PBW | 8.0 (7.8–8.0) | 8.0 (7.8–8.0) | 0.398 |
| FiO2 | 0.4 (0.4–0.4) | 0.4 (0.4–0.5) | <0.001 |
| Respiratory Rate, /min | 12.0 (10.0–15.0) | 14.0 (12.0–15.0) | <0.001 |
| etCO2, kPa | 4.3 (4.0–4.6) | 4.6 (4.3–4.8) | <0.001 |
| Crs, mL/cm H2O | 71.7 (58.8–88.6) | 55.4 (44.9–67.9) | <0.001 |
Disclaimer/Publisher’s Note: The statements, opinions and data contained in all publications are solely those of the individual author(s) and contributor(s) and not of MDPI and/or the editor(s). MDPI and/or the editor(s) disclaim responsibility for any injury to people or property resulting from any ideas, methods, instructions or products referred to in the content. |
© 2023 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Nijbroek, S.G.L.H.; Hol, L.; Serpa Neto, A.; van Meenen, D.M.P.; Hemmes, S.N.T.; Hollmann, M.W.; Schultz, M.J., on behalf of the DESIGNATION Investigators. Safety and Feasibility of Intraoperative High PEEP Titrated to the Lowest Driving Pressure (ΔP)—Interim Analysis of DESIGNATION. J. Clin. Med. 2024, 13, 209. https://doi.org/10.3390/jcm13010209
Nijbroek SGLH, Hol L, Serpa Neto A, van Meenen DMP, Hemmes SNT, Hollmann MW, Schultz MJ on behalf of the DESIGNATION Investigators. Safety and Feasibility of Intraoperative High PEEP Titrated to the Lowest Driving Pressure (ΔP)—Interim Analysis of DESIGNATION. Journal of Clinical Medicine. 2024; 13(1):209. https://doi.org/10.3390/jcm13010209
Chicago/Turabian StyleNijbroek, Sunny G. L. H., Liselotte Hol, Ary Serpa Neto, David M. P. van Meenen, Sabrine N. T. Hemmes, Markus W. Hollmann, and Marcus J. Schultz on behalf of the DESIGNATION Investigators. 2024. "Safety and Feasibility of Intraoperative High PEEP Titrated to the Lowest Driving Pressure (ΔP)—Interim Analysis of DESIGNATION" Journal of Clinical Medicine 13, no. 1: 209. https://doi.org/10.3390/jcm13010209
APA StyleNijbroek, S. G. L. H., Hol, L., Serpa Neto, A., van Meenen, D. M. P., Hemmes, S. N. T., Hollmann, M. W., & Schultz, M. J., on behalf of the DESIGNATION Investigators. (2024). Safety and Feasibility of Intraoperative High PEEP Titrated to the Lowest Driving Pressure (ΔP)—Interim Analysis of DESIGNATION. Journal of Clinical Medicine, 13(1), 209. https://doi.org/10.3390/jcm13010209





