A Comparative Analysis of Osteochondritis Dissecans and Avascular Necrosis: A Comprehensive Review
Abstract
1. Introduction
2. Etiology
3. Epidemiology
4. Clinical Presentation and Diagnosis
4.1. Clinical Picture
- Incidental finding in a symptom-free individual;
- Exercise-induced mechanical pain (most frequently observed);
- Persistent mechanical pain with joint swelling and/or locking.
4.2. Diagnosis
4.3. Differential Diagnosis
- Osteoarthritis;
- Osteoarthritis secondary to acetabular dysplasia;
- Ankylosing spondylitis of the hip joint;
- Transient osteoporosis or bone marrow edema;
- Chondroblastoma of the femoral head;
- Incomplete fracture in subchondral bone;
- Pigmented villonodular synovitis;
- Synovial herniation;
- Femoroacetabular impingement syndrome;
- Bone infarction of the metaphysis.
- Patellofemoral syndrome;
- Patellar tendonitis;
- Osgood-Schlatter disease;
- Sinding-Larsen-Johannson syndrome;
- Fat pad impingement;
- Symptomatic discoid meniscus;
- Symptomatic synovial plica;
- Patellofemoral pain;
- Knee osteoarthritis;
- Chondromalacia;
- Patellar tendonitis;
- Meniscal tear;
- Fat pad impingement;
- Symptomatic synovial plica.
4.4. Classifications
5. Management
5.1. Nonsurgical Treatment
5.2. Surgical Treatment
5.3. Biologic Treatment
6. Conclusions
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Conflicts of Interest
References
- Liu, S.; Wang, B.; Fan, S.; Wang, Y.; Zhan, Y.; Ye, D. Global burden of musculoskeletal disorders and attributable factors in 204 countries and territories: A secondary analysis of the Global Burden of Disease 2019 study. BMJ Open 2022, 12, e062183. [Google Scholar] [CrossRef]
- Gómez-Galán, M.; Pérez-Alonso, J.; Callejón-Ferre, Á.J.; López-Martínez, J. Musculoskeletal disorders: OWAS review. Ind. Health 2017, 55, 314–337. [Google Scholar] [CrossRef]
- Woolf, A.D.; Erwin, J.; March, L. The need to address the burden of musculoskeletal conditions. Best. Pract. Res. Clin. Rheumatol. 2012, 26, 183–224. [Google Scholar] [CrossRef]
- Safiri, S.; Kolahi, A.A.; Cross, M.; Hill, C.; Smith, E.; Carson-Chahhoud, K.; Mansournia, M.A.; Almasi-Hashiani, A.; Ashrafi-Asgarabad, A.; Kaufman, J.; et al. Prevalence, Deaths, and Disability-Adjusted Life Years Due to Musculoskeletal Disorders for 195 Countries and Territories 1990–2017. Arthritis Rheumatol. 2021, 73, 702–714. [Google Scholar] [CrossRef]
- Global, regional, and national disability-adjusted life-years (DALYs) for 359 diseases and injuries and healthy life expectancy (HALE) for 195 countries and territories, 1990–2017: A systematic analysis for the Global Burden of Disease Study 2017. Lancet 2018, 392, 1859–1922. [CrossRef]
- Konarski, W.; Poboży, T.; Śliwczyński, A.; Kotela, I.; Krakowiak, J.; Hordowicz, M.; Kotela, A. Avascular Necrosis of Femoral Head-Overview and Current State of the Art. Int. J. Environ. Res. Public. Health 2022, 19, 7348. [Google Scholar] [CrossRef]
- Matthews, A.H.; Davis, D.D.; Fish, M.J.; Stitson, D. Avascular Necrosis. In StatPearls; StatPearls Publishing LLC.: St. Petersburg, FL, USA, 2023. [Google Scholar]
- Tudisco, C.; Bernardi, G.; Manisera, M.T.; De Maio, F.; Gorgolini, G.; Farsetti, P. An update on osteochondritis dissecans of the knee. Orthop. Rev. 2022, 14, 38829. [Google Scholar] [CrossRef]
- Edmonds, E.W.; Polousky, J. A review of knowledge in osteochondritis dissecans: 123 years of minimal evolution from König to the ROCK study group. Clin. Orthop. Relat. Res. 2013, 471, 1118–1126. [Google Scholar] [CrossRef]
- Itha, R.; Vaishya, R.; Vaish, A.; Migliorini, F. Management of chondral and osteochondral lesions of the hip. Die Orthopädie. 2023; ahead of print. [Google Scholar] [CrossRef]
- De Smet, A.A. Osteochondritis and Osteonecrosis. In Imaging of the Knee: Techniques and Applications; Davies, A.M., Cassar-Pullicino, V., Eds.; Springer: Berlin/Heidelberg, Germany, 2003; pp. 293–306. [Google Scholar]
- Beckmann, R.; Shaheen, H.; Kweider, N.; Ghassemi, A.; Fragoulis, A.; Hermanns-Sachweh, B.; Pufe, T.; Kadyrov, M.; Drescher, W. Corrigendum to “Enoxaparin Prevents Steroid-Related Avascular Necrosis of the Femoral Head”. Sci. World J. 2015, 2015, 264241. [Google Scholar] [CrossRef]
- Shah, K.N.; Racine, J.; Jones, L.C.; Aaron, R.K. Pathophysiology and risk factors for osteonecrosis. Curr. Rev. Musculoskelet. Med. 2015, 8, 201–209. [Google Scholar] [CrossRef]
- James, J.; Steijn-Myagkaya, G.L. Death of osteocytes. Electron microscopy after in vitro ischaemia. J. Bone Jt. Surg. Br. 1986, 68, 620–624. [Google Scholar] [CrossRef]
- Schoutens, A.; Arlet, J.; Gardeniers, J.; Hughes, S. Bone Circulation and Vascularization in Normal and Pathological Conditions; Springer Science & Business Media: Berlin/Heidelberg, Germany, 2012. [Google Scholar]
- Kelley, W.N.; Harris, E.D.; Ruddy, S.; Sledge, C.B. Textbook of Rheumatology; Saunders: Philadelphia, PA, USA, 1997. [Google Scholar]
- Guggenbuhl, P.; Robin, F.; Cadiou, S.; Albert, J.D. Etiology of avascular osteonecrosis of the femoral head. Morphologie 2021, 105, 80–84. [Google Scholar] [CrossRef]
- Mankin, H.J. Nontraumatic necrosis of bone (osteonecrosis). N. Engl. J. Med. 1992, 326, 1473–1479. [Google Scholar]
- Konarski, W.; Poboży, T.; Kotela, A.; Śliwczyński, A.; Kotela, I.; Hordowicz, M.; Krakowiak, J. Does Diabetes Mellitus Increase the Risk of Avascular Osteonecrosis? A Systematic Review and Meta-Analysis. Int. J. Environ. Res. Public Health 2022, 19, 15219. [Google Scholar] [CrossRef]
- Fracture fixation in the operative management of hip fractures (FAITH): An international, multicentre, randomised controlled trial. Lancet 2017, 389, 1519–1527. [CrossRef]
- Widhalm, H.K.; Arnhold, R.; Beiglböck, H.; Munteanu, A.; Lang, N.W.; Hajdu, S. A Comparison of Dynamic Hip Screw and Two Cannulated Screws in the Treatment of Undisplaced Intracapsular Neck Fractures-Two-Year Follow-Up of 453 Patients. J. Clin. Med. 2019, 8, 1670. [Google Scholar] [CrossRef]
- Osarumwense, D.; Tissingh, E.; Wartenberg, K.; Aggarwal, S.; Ismail, F.; Orakwe, S.; Khan, F. The Targon FN system for the management of intracapsular neck of femur fractures: Minimum 2-year experience and outcome in an independent hospital. Clin. Orthop. Surg. 2015, 7, 22–28. [Google Scholar] [CrossRef]
- Perisano, C.; Greco, T.; Vitiello, R.; Maccauro, G.; Liuzza, F.; Tamburelli, F.C.; Forconi, F. Mueller-Weiss disease: Review of the literature. J. Biol. Regul. Homeost. Agents. 2018, 32 (Suppl. S1), 157–162. [Google Scholar]
- Uozumi, H.; Sugita, T.; Aizawa, T.; Takahashi, A.; Ohnuma, M.; Itoi, E. Histologic findings and possible causes of osteochondritis dissecans of the knee. Am. J. Sports Med. 2009, 37, 2003–2008. [Google Scholar] [CrossRef]
- Nissen, C.W. Osteochondritis dissecans of the elbow. Clin. Sports Med. 2014, 33, 251–265. [Google Scholar] [CrossRef] [PubMed]
- Fleisig, G.S.; Andrews, J.R.; Dillman, C.J.; Escamilla, R.F. Kinetics of Baseball Pitching with Implications About Injury Mechanisms. Am. J. Sports Med. 1995, 23, 233–239. [Google Scholar] [CrossRef] [PubMed]
- Baker, C.L.; Romeo, A.A.; Baker, C.L. Osteochondritis Dissecans of the Capitellum. Am. J. Sports Med. 2010, 38, 1917–1928. [Google Scholar] [CrossRef] [PubMed]
- Kocher, M.S.; Tucker, R.; Ganley, T.J.; Flynn, J.M. Management of Osteochondritis Dissecans of the Knee: Current Concepts Review. Am. J. Sports Med. 2006, 34, 1181–1191. [Google Scholar] [CrossRef] [PubMed]
- Kessler, J.I.; Jacobs, J.C.; Jr Cannamela, P.C.; Shea, K.G.; Weiss, J.M. Childhood Obesity is Associated With Osteochondritis Dissecans of the Knee, Ankle, and Elbow in Children and Adolescents. J. Pediatr. Orthop. 2018, 38, e296–e299. [Google Scholar] [CrossRef] [PubMed]
- Ishikawa, M.; Adachi, N.; Yoshikawa, M.; Nakamae, A.; Nakasa, T.; Ikuta, Y.; Hayashi, S.; Deie, M.; Ochi, M. Unique Anatomic Feature of the Posterior Cruciate Ligament in Knees Associated With Osteochondritis Dissecans. Orthop. J. Sports Med. 2016, 4, 2325967116648138. [Google Scholar] [CrossRef] [PubMed]
- Turati, M.; Anghilieri, F.M.; Accadbled, F.; Piatti, M.; Di Benedetto, P.; Moltrasio, F.; Zatti, G.; Zanchi, N.; Bigoni, M. Discoid meniscus in human fetuses: A systematic review. Knee 2021, 30, 205–213. [Google Scholar] [CrossRef] [PubMed]
- Deie, M.; Ochi, M.; Sumen, Y.; Kawasaki, K.; Adachi, N.; Yasunaga, Y.; Ishida, O. Relationship between osteochondritis dissecans of the lateral femoral condyle and lateral menisci types. J. Pediatr. Orthop. 2006, 26, 79–82. [Google Scholar] [CrossRef]
- Jacobi, M.; Wahl, P.; Bouaicha, S.; Jakob, R.P.; Gautier, E. Association between mechanical axis of the leg and osteochondritis dissecans of the knee: Radiographic study on 103 knees. Am. J. Sports Med. 2010, 38, 1425–1428. [Google Scholar] [CrossRef]
- Gonzalez-Herranz, P.; Rodriguez, M.L.; de la Fuente, C. Femoral osteochondritis of the knee: Prognostic value of the mechanical axis. J. Child. Orthop. 2017, 11, 1–5. [Google Scholar] [CrossRef]
- Zanon, G.; Vico, G.D.; Marullo, M. Osteochondritis dissecans of the talus. Joints 2014, 2, 115–123. [Google Scholar] [CrossRef] [PubMed]
- van Bergen, C.J.; van den Ende, K.I.; Ten Brinke, B.; Eygendaal, D. Osteochondritis dissecans of the capitellum in adolescents. World J. Orthop. 2016, 7, 102–108. [Google Scholar] [CrossRef] [PubMed]
- Edmonds, E.W.; Heyworth, B.E. Osteochondritis dissecans of the shoulder and hip. Clin. Sports Med. 2014, 33, 285–294. [Google Scholar] [CrossRef] [PubMed]
- Gornitzky, A.L.; Mistovich, J.R.; Atuahuene, B.; Storey, E.P.; Ganley, T.J. Osteochondritis Dissecans Lesions in Family Members: Does a Positive Family History Impact Phenotypic Potency? Clin. Orthop. Relat. Res. 2017, 475, 1573–1580. [Google Scholar] [CrossRef]
- Yellin, J.L.; Trocle, A.; Grant, S.F.A.; Hakonarson, H.; Shea, K.G.; Ganley, T.J. Candidate Loci are Revealed by an Initial Genome-wide Association Study of Juvenile Osteochondritis Dissecans. J. Pediatr. Orthop. 2017, 37, e32–e36. [Google Scholar] [CrossRef] [PubMed]
- Lefebvre, V.; Li, P.; de Crombrugghe, B. A new long form of Sox5 (L-Sox5), Sox6 and Sox9 are coexpressed in chondrogenesis and cooperatively activate the type II collagen gene. EMBO J. 1998, 17, 5718–5733. [Google Scholar] [CrossRef]
- Lespasio, M.J.; Sodhi, N.; Mont, M.A. Osteonecrosis of the Hip: A Primer. Perm. J. 2019, 23, 18–100. [Google Scholar] [CrossRef]
- Bergman, J.; Nordström, A.; Nordström, P. Epidemiology of osteonecrosis among older adults in Sweden. Osteoporos. Int. 2019, 30, 965–973. [Google Scholar] [CrossRef]
- Cooper, C.; Steinbuch, M.; Stevenson, R.; Miday, R.; Watts, N.B. The epidemiology of osteonecrosis: Findings from the GPRD and THIN databases in the UK. Osteoporos. Int. 2010, 21, 569–577. [Google Scholar] [CrossRef]
- Kessler, J.I.; Nikizad, H.; Shea, K.G.; Jacobs, J.C.; Bebchuk, J.D.; Weiss, J.M. The Demographics and Epidemiology of Osteochondritis Dissecans of the Knee in Children and Adolescents. Am. J. Sports Med. 2014, 42, 320–326. [Google Scholar] [CrossRef]
- Chau, M.M.; Klimstra, M.A.; Wise, K.L.; Ellermann, J.M.; Tóth, F.; Carlson, C.S.; Nelson, B.J.; Tompkins, M.A. Osteochondritis Dissecans: Current Understanding of Epidemiology, Etiology, Management, and Outcomes. J. Bone Jt. Surg. Am. 2021, 103, 1132–1151. [Google Scholar] [CrossRef]
- Weiss, J.M.; Shea, K.G.; Jacobs, J.C.; Jr Cannamela, P.C.; Becker, I.; Portman, M.; Kessler, J.I. Incidence of Osteochondritis Dissecans in Adults. Am. J. Sports Med. 2018, 46, 1592–1595. [Google Scholar] [CrossRef]
- Kessler, J.I.; Weiss, J.M.; Nikizad, H.; Gyurdzhyan, S.; Jacobs, J.C.; Jr Bebchuk, J.D.; Shea, K.G. Osteochondritis dissecans of the ankle in children and adolescents: Demographics and epidemiology. Am. J. Sports Med. 2014, 42, 2165–2171. [Google Scholar] [CrossRef]
- Kessler, J.I.; Jacobs, J.C.; Jr Cannamela, P.C.; Weiss, J.M.; Shea, K.G. Demographics and Epidemiology of Osteochondritis Dissecans of the Elbow Among Children and Adolescents. Orthop. J. Sports Med. 2018, 6, 2325967118815846. [Google Scholar] [CrossRef]
- Bauer, M.; Jonsson, K.; Lindén, B. Osteochondritis dissecans of the ankle. A 20-year follow-up study. J. Bone Jt. Surg. Br. 1987, 69, 93–96. [Google Scholar] [CrossRef]
- Turati, M.; Anghilieri, F.M.; Bigoni, M.; Rigamonti, L.; Tercier, S.; Nicolaou, N.; Accadbled, F. Osteochondritis dissecans of the knee: Epidemiology, etiology, and natural history. J. Child Orthop. 2023, 17, 40–46. [Google Scholar] [CrossRef]
- Nissen, C.W.; Albright, J.C.; Anderson, C.N.; Busch, M.T.; Carlson, C.; Carsen, S.; Chambers, H.G.; Edmonds, E.W.; Ellermann, J.M.; Ellis, H.B., Jr.; et al. Descriptive Epidemiology From the Research in Osteochondritis Dissecans of the Knee (ROCK) Prospective Cohort. Am. J. Sports Med. 2022, 50, 118–127. [Google Scholar] [CrossRef]
- Moya-Angeler, J.; Gianakos, A.L.; Villa, J.C.; Ni, A.; Lane, J.M. Current concepts on osteonecrosis of the femoral head. World J. Orthop. 2015, 6, 590–601. [Google Scholar] [CrossRef]
- Sibilska, A.; Góralczyk, A.; Hermanowicz, K.; Malinowski, K. Spontaneous osteonecrosis of the knee: What do we know so far? A literature review. Int. Orthop. 2020, 44, 1063–1069. [Google Scholar] [CrossRef]
- Parekh, S.G.; Kadakia, R.J. Avascular Necrosis of the Talus. J. Am. Acad. Orthop. Surg. 2021, 29, e267–e278. [Google Scholar] [CrossRef] [PubMed]
- Allan, C.H.; Joshi, A.; Lichtman, D.M. Kienbock’s disease: Diagnosis and treatment. J. Am. Acad. Orthop. Surg. 2001, 9, 128–136. [Google Scholar] [CrossRef]
- Kemmeren, L.A.M.; van Bergen, C.J.A.; Reijman, M.; Piscaer, T.M. Physician preferences in diagnostics and treatment of juvenile osteochondritis dissecans are diverse across the knee, ankle and elbow: An ESSKA survey. Knee Surg. Sports Traumatol. Arthrosc. 2023, 31, 5228–5237. [Google Scholar] [CrossRef]
- Barney, J.; Piuzzi, N.S.; Akhondi, H. Femoral Head Avascular Necrosis. In StatPearls; StatPearls Publishing: St. Petersburg, FL, USA, 2019. [Google Scholar]
- Tripathy, S.K.; Goyal, T.; Sen, R.K. Management of femoral head osteonecrosis: Current concepts. Indian J. Orthop. 2015, 49, 28–45. [Google Scholar] [CrossRef]
- Murphey, M.D.; Foreman, K.L.; Klassen-Fischer, M.K.; Fox, M.G.; Chung, E.M.; Kransdorf, M.J. From the radiologic pathology archives imaging of osteonecrosis: Radiologic-pathologic correlation. Radiographics 2014, 34, 1003–1028. [Google Scholar] [CrossRef]
- Conrad, J.M.; Stanitski, C.L. Osteochondritis dissecans: Wilson’s sign revisited. Am. J. Sports Med. 2003, 31, 777–778. [Google Scholar] [CrossRef]
- Bauer, K.L.; Polousky, J.D. Management of Osteochondritis Dissecans Lesions of the Knee, Elbow and Ankle. Clin. Sports Med. 2017, 36, 469–487. [Google Scholar] [CrossRef]
- Mubarak, S.J.; Carroll, N.C. Juvenile osteochondritis dissecans of the knee: Etiology. Clin. Orthop. Relat. Res. 1981, 200–211. [Google Scholar] [CrossRef]
- Cooper, T.; Boyles, A.; Samora, W.P.; Klingele, K.E. Prevalence of Bilateral JOCD of the Knee and Associated Risk Factors. J. Pediatr. Orthop. 2015, 35, 507–510. [Google Scholar] [CrossRef]
- Accadbled, F.; Turati, M.; Kocher, M.S. Osteochondritis dissecans of the knee: Imaging, instability concept, and criteria. J. Child. Orthop. 2023, 17, 47–53. [Google Scholar] [CrossRef] [PubMed]
- Quatman, C.E.; Quatman-Yates, C.C.; Schmitt, L.C.; Paterno, M.V. The clinical utility and diagnostic performance of MRI for identification and classification of knee osteochondritis dissecans. J. Bone Jt. Surg. Am. 2012, 94, 1036–1044. [Google Scholar] [CrossRef] [PubMed]
- Mohr, B.; Baldea, J.D. Knee Osteochondritis Dissecans; StatPearls Publishing LLC.: St. Petersburg, FL, USA, 2023. [Google Scholar]
- Jawad, M.U.; Haleem, A.A.; Scully, S.P. In brief: Ficat classification: Avascular necrosis of the femoral head. Clin. Orthop. Relat. Res. 2012, 470, 2636–2639. [Google Scholar] [CrossRef] [PubMed]
- Steinberg, M.E.; Hayken, G.D.; Steinberg, D.R. A quantitative system for staging avascular necrosis. J. Bone Jt. Surg. Br. 1995, 77, 34–41. [Google Scholar] [CrossRef] [PubMed]
- Dipaola, J.D.; Nelson, D.W.; Colville, M.R. Characterizing osteochondral lesions by magnetic resonance imaging. Arthroscopy 1991, 7, 101–104. [Google Scholar] [CrossRef] [PubMed]
- Berndt, A.L.; Harty, M. Transchondral fractures (osteochondritis dissecans) of the talus. J. Bone Jt. Surg. Am. 1959, 41, 988–1020. [Google Scholar] [CrossRef] [PubMed]
- Petek, D.; Hannouche, D.; Suva, D. Osteonecrosis of the femoral head: Pathophysiology and current concepts of treatment. EFORT Open Rev. 2019, 4, 85–97. [Google Scholar] [CrossRef]
- Dhillon, M.S.; Rana, B.; Panda, I.; Patel, S.; Kumar, P. Management Options in Avascular Necrosis of Talus. Indian J. Orthop. 2018, 52, 284–296. [Google Scholar] [CrossRef]
- Karim, A.R.; Cherian, J.J.; Jauregui, J.J.; Pierce, T.; Mont, M.A. Osteonecrosis of the knee: Review. Ann. Transl. Med. 2015, 3, 6. [Google Scholar]
- Lee, W.Q.; Lie, H.M.; Lie, D.T.T. Diagnosis and treatment of avascular necrosis of the humeral head: Current concepts. J. ISAKOS 2023, 8, 108–113. [Google Scholar] [CrossRef]
- Lai, K.A.; Shen, W.J.; Yang, C.Y.; Shao, C.J.; Hsu, J.T.; Lin, R.M. The use of alendronate to prevent early collapse of the femoral head in patients with nontraumatic osteonecrosis. A randomized clinical study. J. Bone Jt. Surg. Am. 2005, 87, 2155–2159. [Google Scholar]
- Chen, C.H.; Chang, J.K.; Lai, K.A.; Hou, S.M.; Chang, C.H.; Wang, G.J. Alendronate in the prevention of collapse of the femoral head in nontraumatic osteonecrosis: A two-year multicenter, prospective, randomized, double-blind, placebo-controlled study. Arthritis Rheum. 2012, 64, 1572–1578. [Google Scholar] [CrossRef]
- Ajmal, M.; Matas, A.J.; Kuskowski, M.; Cheng, E.Y. Does statin usage reduce the risk of corticosteroid-related osteonecrosis in renal transplant population? Orthop. Clin. N. Am. 2009, 40, 235–239. [Google Scholar] [CrossRef] [PubMed]
- Pritchett, J.W. Statin therapy decreases the risk of osteonecrosis in patients receiving steroids. Clin. Orthop. Relat. Res. 2001, 173–178. [Google Scholar] [CrossRef]
- Claßen, T.; Becker, A.; Landgraeber, S.; Haversath, M.; Li, X.; Zilkens, C.; Krauspe, R.; Jäger, M. Long-term Clinical Results after Iloprost Treatment for Bone Marrow Edema and Avascular Necrosis. Orthop. Rev. 2016, 8, 6150. [Google Scholar]
- Glueck, C.J.; Freiberg, R.A.; Sieve, L.; Wang, P. Enoxaparin prevents progression of stages I and II osteonecrosis of the hip. Clin. Orthop. Relat. Res. 2005, 435, 164–170. [Google Scholar] [CrossRef] [PubMed]
- Alves, E.M.; Angrisani, A.T.; Santiago, M.B. The use of extracorporeal shock waves in the treatment of osteonecrosis of the femoral head: A systematic review. Clin. Rheumatol. 2009, 28, 1247–1251. [Google Scholar] [CrossRef] [PubMed]
- Massari, L.; Fini, M.; Cadossi, R.; Setti, S.; Traina, G.C. Biophysical stimulation with pulsed electromagnetic fields in osteonecrosis of the femoral head. J. Bone Jt. Surg. Am. 2006, 88 (Suppl. S3), 56–60. [Google Scholar]
- Marcheggiani Muccioli, G.M.; Grassi, A.; Setti, S.; Filardo, G.; Zambelli, L.; Bonanzinga, T.; Rimondi, E.; Busacca, M.; Zaffagnini, S. Conservative treatment of spontaneous osteonecrosis of the knee in the early stage: Pulsed electromagnetic fields therapy. Eur. J. Radiol. 2013, 82, 530–537. [Google Scholar] [CrossRef] [PubMed]
- Camporesi, E.M.; Vezzani, G.; Bosco, G.; Mangar, D.; Bernasek, T.L. Hyperbaric oxygen therapy in femoral head necrosis. J. Arthroplast. 2010, 25 (Suppl. S6), 118–123. [Google Scholar] [CrossRef]
- Reis, N.D.; Schwartz, O.; Militianu, D.; Ramon, Y.; Levin, D.; Norman, D.; Melamed, Y.; Shupak, A.; Goldsher, D.; Zinman, C. Hyperbaric oxygen therapy as a treatment for stage-I avascular necrosis of the femoral head. J. Bone Jt. Surg. Br. 2003, 85, 371–375. [Google Scholar] [CrossRef]
- Smillie, I.S. Treatment of osteochondritis dissecans. J. Bone Jt. Surg. Br. 1957, 39, 248–260. [Google Scholar] [CrossRef]
- Tepolt, F.A.; Kalish, L.A.; Heyworth, B.E.; Kocher, M.S. Nonoperative treatment of stable juvenile osteochondritis dissecans of the knee: Effectiveness of unloader bracing. J. Pediatr. Orthop. B 2020, 29, 81–89. [Google Scholar] [CrossRef]
- Marker, D.R.; Seyler, T.M.; Ulrich, S.D.; Srivastava, S.; Mont, M.A. Do modern techniques improve core decompression outcomes for hip osteonecrosis? Clin. Orthop. Relat. Res. 2008, 466, 1093–1103. [Google Scholar] [CrossRef] [PubMed]
- Song, W.S.; Yoo, J.J.; Kim, Y.M.; Kim, H.J. Results of multiple drilling compared with those of conventional methods of core decompression. Clin. Orthop. Relat. Res. 2007, 454, 139–146. [Google Scholar] [CrossRef] [PubMed]
- Mont, M.A.; Schon, L.C.; Hungerford, M.W.; Hungerford, D.S. Avascular necrosis of the talus treated by core decompression. J. Bone Jt. Surg. Br. 1996, 78, 827–830. [Google Scholar] [CrossRef] [PubMed]
- Mont, M.; Maar, D.; Urquhart, M.; Lennox, D.; Hungerford, D. Avascular necrosis of the humeral head treated by core decompression.A retrospective review. J. Bone Jt. Surg. Br. Vol. 1993, 75, 785–788. [Google Scholar] [CrossRef] [PubMed]
- Forst, J.; Forst, R.; Heller, K.D.; Adam, G. Spontaneous osteonecrosis of the femoral condyle: Causal treatment by early core decompression. Arch. Orthop Trauma Surg. 1998, 117, 18–22. [Google Scholar] [CrossRef] [PubMed]
- Duany, N.G.; Zywiel, M.G.; McGrath, M.S.; Siddiqui, J.A.; Jones, L.C.; Bonutti, P.M.; Mont, M.A. Joint-preserving surgical treatment of spontaneous osteonecrosis of the knee. Arch. Orthop. Trauma Surg. 2010, 130, 11–16. [Google Scholar] [CrossRef] [PubMed]
- Salas, A.P.; Mazek, J.; O’Donnell, J.; Mendez-Perez, E.; Brizuela-Ventura, M.; Velasco-Vazquez, H.A.; Meza, F. Hip Arthroscopy and Core Decompression for Avascular Necrosis of the Femoral Head Using a Specific Aiming Guide: A Step-by-Step Surgical Technique. Arthrosc Tech. 2021, 10, e2775–e2782. [Google Scholar] [CrossRef]
- Meyers, M.H. Resurfacing of the femoral head with fresh osteochondral allografts. Long-term results. Clin. Orthop. Relat. Res. 1985, 197, 111–114. [Google Scholar] [CrossRef]
- Keizer, S.B.; Kock, N.B.; Dijkstra, P.D.; Taminiau, A.H.; Nelissen, R.G. Treatment of avascular necrosis of the hip by a non-vascularised cortical graft. J. Bone Jt. Surg. Br. 2006, 88, 460–466. [Google Scholar] [CrossRef]
- Buckley, P.D.; Gearen, P.F.; Petty, R.W. Structural bone-grafting for early atraumatic avascular necrosis of the femoral head. J. Bone Jt. Surg. Am. 1991, 73, 1357–1364. [Google Scholar] [CrossRef] [PubMed]
- Yu, X.G.; Zhao, D.W.; Sun, Q.; Wang, T.N.; Yu, H.B.; Su, Y.; Liu, J.B.; Zheng, J.F.; Wang, B.J.; Cui, D.P. Treatment of non-traumatic avascular talar necrosis by transposition of vascularized cuneiform bone flap plus iliac cancellous bone grafting. Zhonghua Yi Xue Za Zhi 2010, 90, 1035–1038. [Google Scholar] [PubMed]
- Miyazaki, A.N.; Silva, L.A.; Sella, G.d.V.; Checchia, C.S.; Simionato, M.C.; Checchia, S.L. Articular reconstruction of the humeral head with autogenous allograft in the treatment of the osteonecrosis. Rev. Bras. De Ortop. 2018, 53, 113–117. [Google Scholar] [CrossRef]
- Boyer, P.; Huten, D.; Loriaut, P.; Lestrat, V.; Jeanrot, C.; Massin, P. Is alumina-on-alumina ceramic bearings total hip replacement the right choice in patients younger than 50 years of age? A 7- to 15-year follow-up study. Orthop. Traumatol. Surg. Res. 2010, 96, 616–622. [Google Scholar] [CrossRef] [PubMed]
- Massin, P. Treatments of avascular osteonecrosis of the hip: Current treatments. Morphologie 2021, 105, 120–126. [Google Scholar] [CrossRef] [PubMed]
- Hervé, A.; Chelli, M.; Boileau, P.; Walch, G.; Favard, L.; Levigne, C.; Sirveaux, F.; Clavert, P.; Bonnevialle, N.; Collin, P. Clinical and radiological results of hemiarthroplasty and total shoulder arthroplasty for primary avascular necrosis of the humeral head in patients less than 60 years old. J. Clin. Med. 2021, 10, 3081. [Google Scholar] [CrossRef] [PubMed]
- Heyse, T.J.; Khefacha, A.; Fuchs-Winkelmann, S.; Cartier, P. UKA after spontaneous osteonecrosis of the knee: A retrospective analysis. Arch. Orthop. Trauma Surg. 2011, 131, 613–617. [Google Scholar] [CrossRef]
- Edmonds, E.W.; Albright, J.; Bastrom, T.; Chambers, H.G. Outcomes of extra-articular, intra-epiphyseal drilling for osteochondritis dissecans of the knee. J. Pediatr. Orthop. 2010, 30, 870–878. [Google Scholar] [CrossRef]
- Heyworth, B.E.; Edmonds, E.W.; Murnaghan, M.L.; Kocher, M.S. Drilling techniques for osteochondritis dissecans. Clin. Sports Med. 2014, 33, 305–312. [Google Scholar] [CrossRef]
- Donaldson, L.D.; Wojtys, E.M. Extraarticular drilling for stable osteochondritis dissecans in the skeletally immature knee. J. Pediatr. Orthop. 2008, 28, 831–835. [Google Scholar] [CrossRef]
- Taranow, W.S.; Bisignani, G.A.; Towers, J.D.; Conti, S.F. Retrograde drilling of osteochondral lesions of the medial talar dome. Foot Ankle Int. 1999, 20, 474–480. [Google Scholar] [CrossRef] [PubMed]
- Unal, P.; Samargandi, R.; Olejnik, R.; Lakhal, W.; Odent, T. Efficacy of the pridie drilling technique in knee osteochondritis dissecans among children and young adults: Follow-up of 41 cases. Eur. J. Orthop. Surg. Traumatol. 2023; ahead of print. [Google Scholar] [CrossRef] [PubMed]
- Masquijo, J.; Kothari, A. Juvenile osteochondritis dissecans (JOCD) of the knee: Current concepts review. EFORT Open Rev. 2019, 4, 201–212. [Google Scholar] [CrossRef] [PubMed]
- Melugin, H.P.; Desai, V.S.; Levy, B.A.; Tanaka, Y.; Horibe, S.; Nakamura, N.; Krych, A.J. Osteochondritis Dissecans of the Knee: Short-Term Outcomes of a Hybrid Technique to Restore a Partially Salvageable Progeny Fragment. Cartilage 2020, 11, 300–308. [Google Scholar] [CrossRef] [PubMed]
- Lintz, F.; Pujol, N.; Pandeirada, C.; Boisrenoult, P.; Beaufils, P. Hybrid fixation: Evaluation of a novel technique in adult osteochondritis dissecans of the knee. Knee Surg. Sports Traumatol. Arthrosc. 2011, 19, 568–571. [Google Scholar] [CrossRef] [PubMed]
- Chadli, L.; Steltzlen, C.; Toanen, C.; Boisrenoult, P.; Beaufils, P.; Pujol, N. Hybrid fixation in adult osteochondritis dissecans of the knee. Orthop. Traumatol. Surg. Res. 2018, 104, 223–225. [Google Scholar] [CrossRef] [PubMed]
- Murab, S.; Hawk, T.; Snyder, A.; Herold, S.; Totapally, M.; Whitlock, P.W. Tissue Engineering Strategies for Treating Avascular Necrosis of the Femoral Head. Bioengineering 2021, 8, 200. [Google Scholar] [CrossRef] [PubMed]
- Hernigou, P.; Beaujean, F. Treatment of osteonecrosis with autologous bone marrow grafting. Clin. Orthop. Relat. Res. 2002, 405, 14–23. [Google Scholar] [CrossRef]
- Gangji, V.; Hauzeur, J.P.; Matos, C.; De Maertelaer, V.; Toungouz, M.; Lambermont, M. Treatment of osteonecrosis of the femoral head with implantation of autologous bone-marrow cells. A pilot study. J. Bone Jt. Surg. Am. 2004, 86, 1153–1160. [Google Scholar] [CrossRef]
- Zhang, C.; Fang, X.; Huang, Z.; Li, W.; Zhang, W.; Lee, G.C. Addition of Bone Marrow Stem Cells Therapy Achieves Better Clinical Outcomes and Lower Rates of Disease Progression Compared With Core Decompression Alone for Early Stage Osteonecrosis of the Femoral Head: A Systematic Review and Meta-Analysis. J. Am. Acad. Orthop. Surg. 2020, 28, 973–979. [Google Scholar] [CrossRef]
- Wang, Z.; Sun, Q.-m.; Zhang, F.-q.; Zhang, Q.-l.; Wang, L.-g.; Wang, W.-j. Core decompression combined with autologous bone marrow stem cells versus core decompression alone for patients with osteonecrosis of the femoral head: A meta-analysis. Int. J. Surg. 2019, 69, 23–31. [Google Scholar] [CrossRef] [PubMed]




| Stage/Type | Radiography [70] | [69] |
|---|---|---|
| I | Small lesion, compression of subchondral bone | Articular cartilage thickening and low signal alterations, but no fractures detected |
| II | Partially detached OCD fragment | Articular cartilage breached, with a low-signal rim behind the fragment indicating fibrous attachment. |
| III | Completely separated OCD fragment, still located in the underlying crater | Articular cartilage breached, with a high-signal rim behind the fragment indicating synovial fluid between the fragment and the underlying subchondral bone |
| IV | Full detachment or loose body | Loose body |
| AVN | OCD | |
|---|---|---|
| Pathophysiology | Blockage and reduction in subchondral microcirculation leading to necrosis of hematopoietic cells and adipocytes with subsequential interstitial marrow edema and osteocyte death. | Subchondral bone injury progresses from resorption to collapse, leading to sequestration. This sequence may result in the separation of articular cartilage and the detachment of a subchondral bone fragment, forming a loose body. |
| Risk factors | Traumatic factors:
|
|
| Incidence | 0.1–4.3 cases/100,000 person-years—depending on the site | 2.3–31.6 cases per 100,000 individuals–depending on the site |
| Most common sites |
|
|
| Age | Typically, 30–65 years old | Typically, 11–20 years old |
| Clinical manifestation | In the early stages of AVN, symptoms are often absent. Typical signs of AVN may manifest as growing pain, stiffness, and crepitus. | Stable lesions cause nonspecific symptoms such as pain, especially during activities or during palpation, vague, crepitus, limited range of motion, and joint effusion. Unstable lesions or loose bodies may manifest by clicking or locking. |
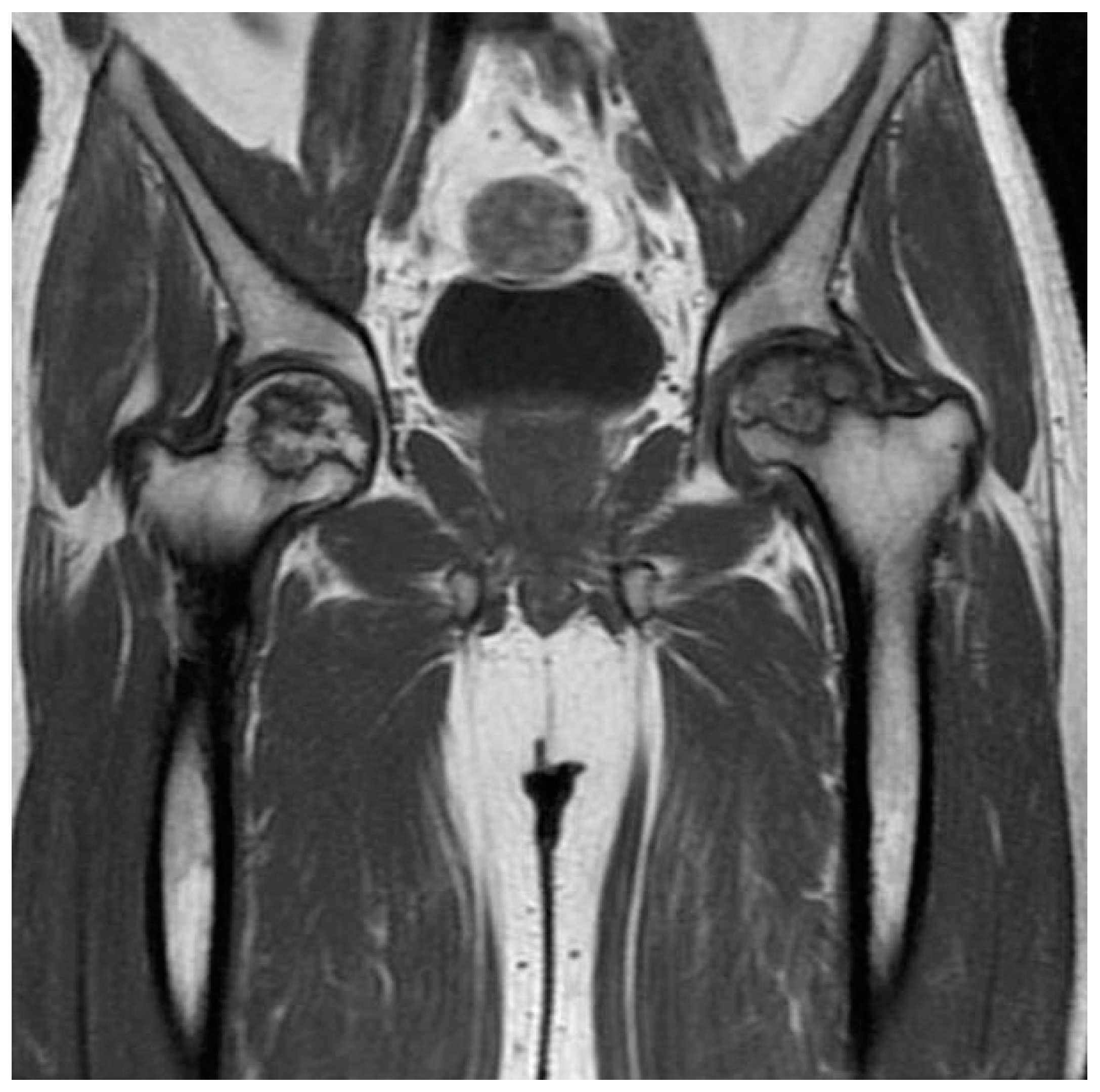
| Imaging | Radiography followed by MRI. | Radiography followed by MRI. |
| Radiographic features | Subchondral radiolucency, referred to as the “crescent sign” suggesting subchondral collapse. | Early lesions manifest as contour abnormalities. Advanced lesions show a circumscribed ossified fragment separated from the bone by a radiolucent line. |
| MRI features | T1-weighted images display a single-density, low-signal intensity line. T2-weighted images display a high-intensity line with early necrotic-viable bone interface. | In T1-weighted images, the progeny is typically hypointense. In T2-weighted images, the progeny is mostly heterogeneous; this sequence can assess the integrity of articular cartilage, reactive marrow edema in the parent bone, and fluid or cystic changes at the parent-progeny interface. |
| Rate of bilateral cases | Up to 70% | 14–30% |
| Conservative treatment |
|
|
| Surgical treatment |
|
|
Disclaimer/Publisher’s Note: The statements, opinions and data contained in all publications are solely those of the individual author(s) and contributor(s) and not of MDPI and/or the editor(s). MDPI and/or the editor(s) disclaim responsibility for any injury to people or property resulting from any ideas, methods, instructions or products referred to in the content. |
© 2024 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Konarski, W.; Poboży, T.; Konarska, K.; Śliwczyński, A.; Kotela, I.; Krakowiak, J. A Comparative Analysis of Osteochondritis Dissecans and Avascular Necrosis: A Comprehensive Review. J. Clin. Med. 2024, 13, 287. https://doi.org/10.3390/jcm13010287
Konarski W, Poboży T, Konarska K, Śliwczyński A, Kotela I, Krakowiak J. A Comparative Analysis of Osteochondritis Dissecans and Avascular Necrosis: A Comprehensive Review. Journal of Clinical Medicine. 2024; 13(1):287. https://doi.org/10.3390/jcm13010287
Chicago/Turabian StyleKonarski, Wojciech, Tomasz Poboży, Klaudia Konarska, Andrzej Śliwczyński, Ireneusz Kotela, and Jan Krakowiak. 2024. "A Comparative Analysis of Osteochondritis Dissecans and Avascular Necrosis: A Comprehensive Review" Journal of Clinical Medicine 13, no. 1: 287. https://doi.org/10.3390/jcm13010287
APA StyleKonarski, W., Poboży, T., Konarska, K., Śliwczyński, A., Kotela, I., & Krakowiak, J. (2024). A Comparative Analysis of Osteochondritis Dissecans and Avascular Necrosis: A Comprehensive Review. Journal of Clinical Medicine, 13(1), 287. https://doi.org/10.3390/jcm13010287







