Patent Foramen Ovale Percutaneous Closure: Evolution and Ongoing Challenges
Abstract
:1. Introduction
2. Historical Context
3. Change of Paradigm: Current Validated Indications for PFO Closure
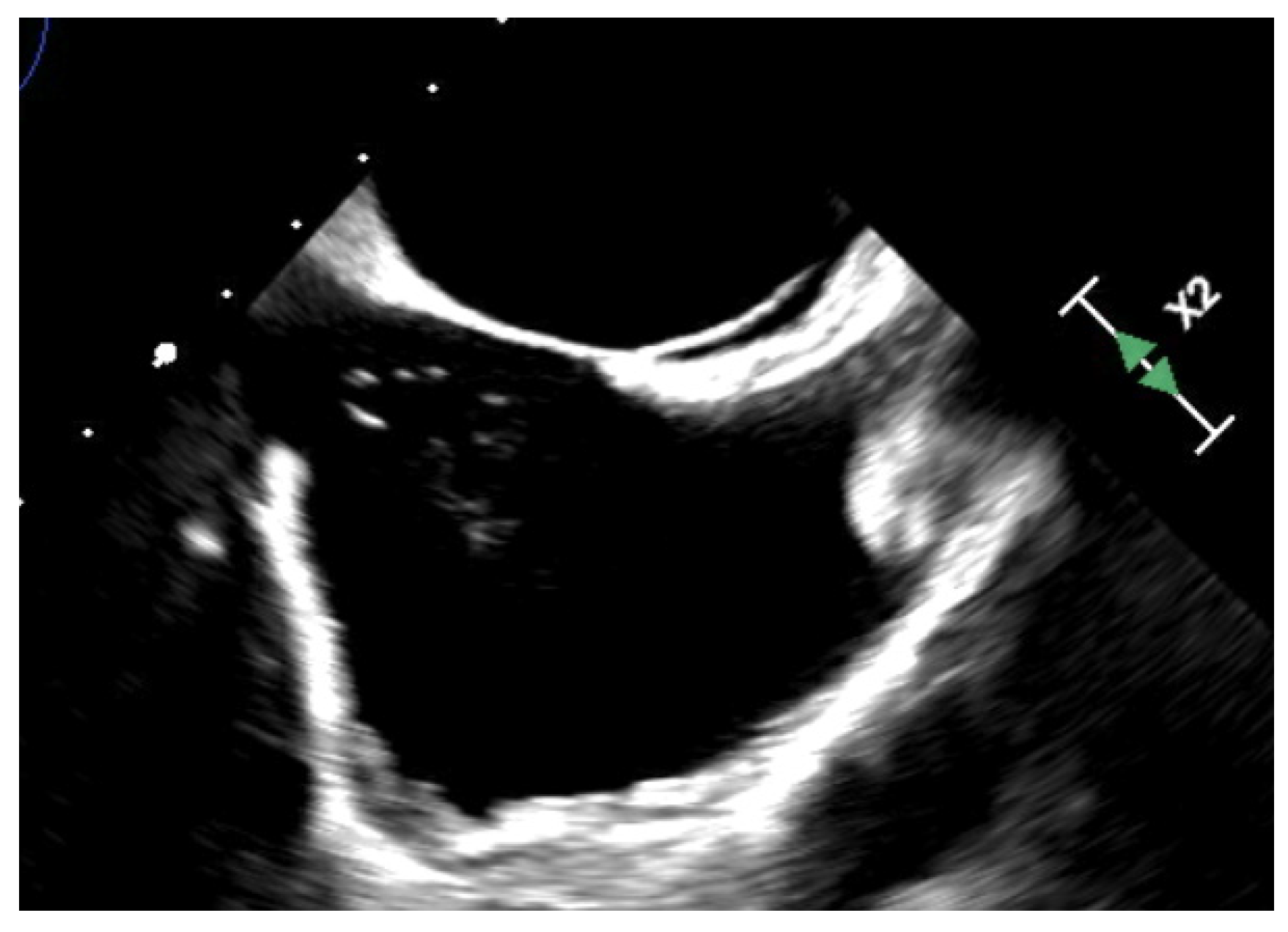
- Cortical infarcts are more commonly embolic in origin compared to white matter infarcts.
4. Other Pathogenic Conditions Associated with PFO
4.1. Migraine
4.2. Arterial Hypoxemia and Platypnea Orthodeoxia Syndrome
4.3. Decompression Sickness (DCS)
4.4. Neurosurgery in Sitting Position
5. Procedure
Complications
| Complications | Type |
|---|---|
| Frequent (up to 20–30%) [101] | Minor vascular complications Atrial fibrillation |
| Rare (<1% [96,102]. | PFO device embolization Device thrombosis |
| Very rare (<0.5%) [98]. | Cardiac tamponade Pneumothorax Hemothorax |
6. Ongoing Challenges
6.1. Antithrombotic Treatment
6.2. Residual Shunts
6.3. Post-Procedural Atrial Fibrillation
6.4. Patients > 60 Years-Old
6.5. Delay from Last Ischemic Event
7. Conclusions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Conflicts of Interest
References
- Koutroulou, I.; Tsivgoulis, G.; Tsalikakis, D.; Karacostas, D.; Grigoriadis, N.; Karapanayiotides, T. Epidemiology of Patent Foramen Ovale in General Population and in Stroke Patients: A Narrative Review. Front. Neurol. 2020, 11, 281. [Google Scholar] [CrossRef] [PubMed]
- Belvís, R.; Tizzano, E.F.; Martí-Fàbregas, J.; Leta, R.G.; Baena, M.; Carreras, F.; Pons-Lladó, G.; Baiget, M.; Martí-Vilalta, J.L. Mutations in the NKX2-5 Gene in Patients with Stroke and Patent Foramen Ovale. Clin. Neurol. Neurosurg. 2009, 111, 574–578. [Google Scholar] [CrossRef] [PubMed]
- Paolucci, M.; Vincenzi, C.; Romoli, M.; Amico, G.; Ceccherini, I.; Lattanzi, S.; Bersano, A.; Longoni, M.; Sacco, S.; Vernieri, F.; et al. The Genetic Landscape of Patent Foramen Ovale: A Systematic Review. Genes 2021, 12, 1953. [Google Scholar] [CrossRef] [PubMed]
- Lechat, P.H.; Mas, J.L.; Lascault, G.; Loron, P.H.; Theard, M.; Klimczac, M.; Drobinski, G.; Thomas, D.; Grosgogeat, Y. Prevalence of Patent Foramen Ovale in Patients with Stroke. N. Engl. J. Med. 1988, 318, 1148–1152. [Google Scholar] [CrossRef] [PubMed]
- Hara, H.; Virmani, R.; Ladich, E.; Mackey-Bojack, S.; Titus, J.; Reisman, M.; Gray, W.; Nakamura, M.; Mooney, M.; Poulose, A.; et al. Patent Foramen Ovale: Current Pathology, Pathophysiology, and Clinical Status. J. Am. Coll. Cardiol. 2005, 46, 1768–1776. [Google Scholar] [CrossRef] [PubMed]
- Webster, M.W.I.; Smith, H.J.; Sharpe, D.N.; Chancellor, A.M.; Swift, D.L.; Bass, N.M.; Glasgow, G.L. Patent foramen ovale in young stroke patients. Lancet 1988, 332, 11–12. [Google Scholar] [CrossRef] [PubMed]
- Hart, R.G.; Diener, H.-C.; Coutts, S.B.; Easton, J.D.; Granger, C.B.; O’Donnell, M.J.; Sacco, R.L.; Connolly, S.J.; Cryptogenic Stroke/ESUS International Working Group. Embolic Strokes of Undetermined Source: The Case for a New Clinical Construct. Lancet Neurol. 2014, 13, 429–438. [Google Scholar] [CrossRef] [PubMed]
- Rigatelli, G.; Zuin, M.; Bilato, C. Atrial Septal Aneurysm Contribution to the Risk of Cryptogenic Stroke in Patients with Patent Foramen Ovale: A Brief Updated Systematic Review and Meta-Analysis. Trends Cardiovasc. Med. 2023, 33, 329–333. [Google Scholar] [CrossRef]
- Mas, J.-L.; Arquizan, C.; Lamy, C.; Zuber, M.; Cabanes, L.; Derumeaux, G.; Coste, J. Recurrent Cerebrovascular Events Associated with Patent Foramen Ovale, Atrial Septal Aneurysm, or Both. N. Engl. J. Med. 2001, 345, 1740–1746. [Google Scholar] [CrossRef]
- Bridges, N.D.; Hellenbrand, W.; Latson, L.; Filiano, J.; Newburger, J.W.; Lock, J.E. Transcatheter Closure of Patent Foramen Ovale after Presumed Paradoxical Embolism. Circulation 1992, 86, 1902–1908. [Google Scholar] [CrossRef]
- Schuchlenz, H.W.; Weihs, W.; Berghold, A.; Lechner, A.; Schmidt, R. Secondary Prevention after Cryptogenic Cerebrovascular Events in Patients with Patent Foramen Ovale. Int. J. Cardiol. 2005, 101, 77–82. [Google Scholar] [CrossRef] [PubMed]
- Wahl, A.; Jüni, P.; Mono, M.-L.; Kalesan, B.; Praz, F.; Geister, L.; Räber, L.; Nedeltchev, K.; Mattle, H.P.; Windecker, S.; et al. Long-Term Propensity Score–Matched Comparison of Percutaneous Closure of Patent Foramen Ovale With Medical Treatment After Paradoxical Embolism. Circulation 2012, 125, 803–812. [Google Scholar] [CrossRef] [PubMed]
- Carroll, J.D.; Saver, J.L.; Thaler, D.E.; Smalling, R.W.; Berry, S.; MacDonald, L.A.; Marks, D.S.; Tirschwell, D.L. Closure of Patent Foramen Ovale versus Medical Therapy after Cryptogenic Stroke. N. Engl. J. Med. 2013, 368, 1092–1100. [Google Scholar] [CrossRef]
- Furlan, A.J.; Reisman, M.; Massaro, J.; Mauri, L.; Adams, H.; Albers, G.W.; Felberg, R.; Herrmann, H.; Kar, S.; Landzberg, M.; et al. Closure or Medical Therapy for Cryptogenic Stroke with Patent Foramen Ovale. N. Engl. J. Med. 2012, 366, 991–999. [Google Scholar] [CrossRef] [PubMed]
- Meier, B.; Kalesan, B.; Mattle, H.P.; Khattab, A.A.; Hildick-Smith, D.; Dudek, D.; Andersen, G.; Ibrahim, R.; Schuler, G.; Walton, A.S.; et al. Percutaneous Closure of Patent Foramen Ovale in Cryptogenic Embolism. N. Engl. J. Med. 2013, 368, 1083–1091. [Google Scholar] [CrossRef] [PubMed]
- Rengifo-Moreno, P.; Palacios, I.F.; Junpaparp, P.; Witzke, C.F.; Morris, D.L.; Romero-Corral, A. Patent Foramen Ovale Transcatheter Closure vs. Medical Therapy on Recurrent Vascular Events: A Systematic Review and Meta-Analysis of Randomized Controlled Trials. Eur. Heart J. 2013, 34, 3342–3352. [Google Scholar] [CrossRef]
- Lee, P.H.; Song, J.-K.; Kim, J.S.; Heo, R.; Lee, S.; Kim, D.-H.; Song, J.-M.; Kang, D.-H.; Kwon, S.U.; Kang, D.-W.; et al. Cryptogenic Stroke and High-Risk Patent Foramen Ovale: The DEFENSE-PFO Trial. J. Am. Coll. Cardiol. 2018, 71, 2335–2342. [Google Scholar] [CrossRef] [PubMed]
- Mas, J.-L.; Derumeaux, G.; Guillon, B.; Massardier, E.; Hosseini, H.; Mechtouff, L.; Arquizan, C.; Béjot, Y.; Vuillier, F.; Detante, O.; et al. Patent Foramen Ovale Closure or Anticoagulation vs. Antiplatelets after Stroke. N. Engl. J. Med. 2017, 377, 1011–1021. [Google Scholar] [CrossRef]
- Søndergaard, L.; Kasner, S.E.; Rhodes, J.F.; Andersen, G.; Iversen, H.K.; Nielsen-Kudsk, J.E.; Settergren, M.; Sjöstrand, C.; Roine, R.O.; Hildick-Smith, D.; et al. Patent Foramen Ovale Closure or Antiplatelet Therapy for Cryptogenic Stroke. N. Engl. J. Med. 2017, 377, 1033–1042. [Google Scholar] [CrossRef]
- Saver, J.L.; Carroll, J.D.; Thaler, D.E.; Smalling, R.W.; MacDonald, L.A.; Marks, D.S.; Tirschwell, D.L.; RESPECT Investigators. Long-Term Outcomes of Patent Foramen Ovale Closure or Medical Therapy after Stroke. N. Engl. J. Med. 2017, 377, 1022–1032. [Google Scholar] [CrossRef]
- Pristipino, C.; Sievert, H.; D’ascenzo, F.; Mas, J.-L.; Meier, B.; Scacciatella, P.; Hildick-Smith, D.; Gaita, F.; Toni, D.; Kyrle, P.; et al. European Position Paper on the Management of Patients with Patent Foramen Ovale. General Approach and Left Circulation Thromboembolism. Available online: https://eurointervention.pcronline.com/article/european-position-paper-on-the-management-of-patients-with-patent-foramen-ovale-general-approach-and-left-circulation-thromboembolism (accessed on 1 February 2023).
- Alsheikh-Ali, A.A.; Thaler, D.E.; Kent, D.M. Patent Foramen Ovale in Cryptogenic Stroke: Incidental or Pathogenic? Stroke 2009, 40, 2349–2355. [Google Scholar] [CrossRef] [PubMed]
- Handke, M.; Harloff, A.; Bode, C.; Geibel, A. Patent Foramen Ovale and Cryptogenic Stroke: A Matter of Age? Semin. Thromb. Hemost. 2009, 35, 505–514. [Google Scholar] [CrossRef] [PubMed]
- Schuchlenz, H.W.; Saurer, G.; Weihs, W.; Rehak, P. Persisting Eustachian Valve in Adults: Relation to Patent Foramen Ovale and Cerebrovascular Events. J. Am. Soc. Echocardiogr. 2004, 17, 231–233. [Google Scholar] [CrossRef] [PubMed]
- Schuchlenz, H.W.; Weihs, W.; Horner, S.; Quehenberger, F. The Association between the Diameter of a Patent Foramen Ovale and the Risk of Embolic Cerebrovascular Events. Am. J. Med. 2000, 109, 456–462. [Google Scholar] [CrossRef] [PubMed]
- Goel, S.S.; Tuzcu, E.M.; Shishehbor, M.H.; de Oliveira, E.I.; Borek, P.P.; Krasuski, R.A.; Rodriguez, L.L.; Kapadia, S.R. Morphology of the Patent Foramen Ovale in Asymptomatic versus Symptomatic (Stroke or Transient Ischemic Attack) Patients. Am. J. Cardiol. 2009, 103, 124–129. [Google Scholar] [CrossRef] [PubMed]
- De Castro, S.; Cartoni, D.; Fiorelli, M.; Rasura, M.; Anzini, A.; Zanette, E.M.; Beccia, M.; Colonnese, C.; Fedele, F.; Fieschi, C.; et al. Morphological and Functional Characteristics of Patent Foramen Ovale and Their Embolic Implications. Stroke 2000, 31, 2407–2413. [Google Scholar] [CrossRef] [PubMed]
- Clergeau, M.-R.; Hamon, M.; Morello, R.; Saloux, E.; Viader, F.; Hamon, M. Silent Cerebral Infarcts in Patients with Pulmonary Embolism and a Patent Foramen Ovale: A Prospective Diffusion-Weighted MRI Study. Stroke 2009, 40, 3758–3762. [Google Scholar] [CrossRef]
- Cramer, S.C.; Rordorf, G.; Maki, J.H.; Kramer, L.A.; Grotta, J.C.; Burgin, W.S.; Hinchey, J.A.; Benesch, C.; Furie, K.L.; Lutsep, H.L.; et al. Increased Pelvic Vein Thrombi in Cryptogenic Stroke: Results of the Paradoxical Emboli from Large Veins in Ischemic Stroke (PELVIS) Study. Stroke 2004, 35, 46–50. [Google Scholar] [CrossRef]
- Liberman, A.L.; Daruwalla, V.J.; Collins, J.D.; Maas, M.B.; Botelho, M.P.F.; Ayache, J.B.; Carr, J.; Ruff, I.; Bernstein, R.A.; Alberts, M.J.; et al. Diagnostic Yield of Pelvic Magnetic Resonance Venography in Patients with Cryptogenic Stroke and Patent Foramen Ovale. Stroke 2014, 45, 2324–2329. [Google Scholar] [CrossRef]
- Ozdemir, O.; Beletsky, V.; Hachinski, V.; Spence, J.D. Cerebrovascular Events on Awakening, Patent Foramen Ovale and Obstructive Sleep Apnea Syndrome. J. Neurol. Sci. 2008, 268, 193–194. [Google Scholar] [CrossRef]
- Ozdemir, A.O.; Tamayo, A.; Munoz, C.; Dias, B.; Spence, J.D. Cryptogenic Stroke and Patent Foramen Ovale: Clinical Clues to Paradoxical Embolism. J. Neurol. Sci. 2008, 275, 121–127. [Google Scholar] [CrossRef] [PubMed]
- Kent, D.M.; Ruthazer, R.; Weimar, C.; Mas, J.-L.; Serena, J.; Homma, S.; Di Angelantonio, E.; Di Tullio, M.R.; Lutz, J.S.; Elkind, M.S.V.; et al. An Index to Identify Stroke-Related vs. Incidental Patent Foramen Ovale in Cryptogenic Stroke. Neurology 2013, 81, 619–625. [Google Scholar] [CrossRef] [PubMed]
- Prefasi, D.; Martínez-Sánchez, P.; Fuentes, B.; Díez-Tejedor, E. The Utility of the RoPE Score in Cryptogenic Stroke Patients ≤50 Years in Predicting a Stroke-Related Patent Foramen Ovale. Int. J. Stroke 2016, 11, NP7-8. [Google Scholar] [CrossRef]
- Elgendy, A.Y.; Saver, J.L.; Amin, Z.; Boudoulas, K.D.; Carroll, J.D.; Elgendy, I.Y.; Grunwald, I.Q.; Gertz, Z.M.; Hijazi, Z.M.; Horlick, E.M.; et al. Proposal for Updated Nomenclature and Classification of Potential Causative Mechanism in Patent Foramen Ovale–Associated Stroke. JAMA Neurol. 2020, 77, 878–886. [Google Scholar] [CrossRef] [PubMed]
- Kavinsky, C.J.; Szerlip, M.; Goldsweig, A.M.; Amin, Z.; Boudoulas, K.D.; Carroll, J.D.; Coylewright, M.; Elmariah, S.; MacDonald, L.A.; Shah, A.P.; et al. SCAI Guidelines for the Management of Patent Foramen Ovale. J. Soc. Cardiovasc. Angiogr. Interv. 2022, 1, 100039. [Google Scholar] [CrossRef]
- Sanna, T.; Diener, H.-C.; Passman, R.S.; Di Lazzaro, V.; Bernstein, R.A.; Morillo, C.A.; Rymer, M.M.; Thijs, V.; Rogers, T.; Beckers, F.; et al. Cryptogenic Stroke and Underlying Atrial Fibrillation. N. Engl. J. Med. 2014, 370, 2478–2486. [Google Scholar] [CrossRef] [PubMed]
- Ziegler, P.D.; Rogers, J.D.; Ferreira, S.W.; Nichols, A.J.; Sarkar, S.; Koehler, J.L.; Warman, E.N.; Richards, M. Real-World Experience with Insertable Cardiac Monitors to Find Atrial Fibrillation in Cryptogenic Stroke. Cerebrovasc. Dis. 2015, 40, 175–181. [Google Scholar] [CrossRef]
- Christensen, L.M.; Krieger, D.W.; Højberg, S.; Pedersen, O.D.; Karlsen, F.M.; Jacobsen, M.D.; Worck, R.; Nielsen, H.; Ægidius, K.; Jeppesen, L.L.; et al. Paroxysmal Atrial Fibrillation Occurs Often in Cryptogenic Ischaemic Stroke. Final Results from the SURPRISE Study. Eur. J. Neurol. 2014, 21, 884–889. [Google Scholar] [CrossRef]
- Kishore, A.; Vail, A.; Majid, A.; Dawson, J.; Lees, K.R.; Tyrrell, P.J.; Smith, C.J. Detection of Atrial Fibrillation after Ischemic Stroke or Transient Ischemic Attack: A Systematic Review and Meta-Analysis. Stroke 2014, 45, 520–526. [Google Scholar] [CrossRef]
- Gladstone, D.J.; Spring, M.; Dorian, P.; Panzov, V.; Thorpe, K.E.; Hall, J.; Vaid, H.; O’Donnell, M.; Laupacis, A.; Côté, R.; et al. Atrial Fibrillation in Patients with Cryptogenic Stroke. N. Engl. J. Med. 2014, 370, 2467–2477. [Google Scholar] [CrossRef]
- Kernan, W.N.; Ovbiagele, B.; Black, H.R.; Bravata, D.M.; Chimowitz, M.I.; Ezekowitz, M.D.; Fang, M.C.; Fisher, M.; Furie, K.L.; Heck, D.V.; et al. Guidelines for the Prevention of Stroke in Patients with Stroke and Transient Ischemic Attack: A Guideline for Healthcare Professionals from the American Heart Association/American Stroke Association. Stroke 2014, 45, 2160–2236. [Google Scholar] [CrossRef] [PubMed]
- Wilmshurst, P.T.; Nightingale, S.; Walsh, K.P.; Morrison, W.L. Effect on Migraine of Closure of Cardiac Right-to-Left Shunts to Prevent Recurrence of Decompression Illness or Stroke or for Haemodynamic Reasons. Lancet 2000, 356, 1648–1651. [Google Scholar] [CrossRef] [PubMed]
- Anzola, G.P.; Morandi, E.; Casilli, F.; Onorato, E. Does Transcatheter Closure of Patent Foramen Ovale Really “Shut the Door?” A Prospective Study with Transcranial Doppler. Stroke 2004, 35, 2140–2144. [Google Scholar] [CrossRef]
- Azarbal, B.; Tobis, J.; Suh, W.; Chan, V.; Dao, C.; Gaster, R. Association of Interatrial Shunts and Migraine Headaches: Impact of Transcatheter Closure. J. Am. Coll. Cardiol. 2005, 45, 489–492. [Google Scholar] [CrossRef] [PubMed]
- Biasco, L.; Infantino, V.; Orzan, F.; Vicentini, S.; Rovera, C.; Longo, G.; Chinaglia, A.; Belli, R.; Allais, G.; Gaita, F. Impact of Transcatheter Closure of Patent Foramen Ovale in the Evolution of Migraine and Role of Residual Shunt. J. Cardiol. 2014, 64, 390–394. [Google Scholar] [CrossRef] [PubMed]
- Donti, A.; Giardini, A.; Salomone, L.; Formigari, R.; Picchio, F.M. Transcatheter Patent Foramen Ovale Closure Using the Premere PFO Occlusion System. Catheter. Cardiovasc. Interv. 2006, 68, 736–740. [Google Scholar] [CrossRef]
- Dubiel, M.; Bruch, L.; Schmehl, I.; Liebner, M.; Winkelmann, A.; Stretz, A.; Grad, M.O.; Kleber, F.X. Migraine Headache Relief after Percutaneous Transcatheter Closure of Interatrial Communications. J. Interv. Cardiol. 2008, 21, 32–37. [Google Scholar] [CrossRef]
- Giardini, A.; Donti, A.; Formigari, R.; Salomone, L.; Prandstraller, D.; Bonvicini, M.; Palareti, G.; Guidetti, D.; Gaddi, O.; Picchio, F.M. Transcatheter Patent Foramen Ovale Closure Mitigates Aura Migraine Headaches Abolishing Spontaneous Right-to-Left Shunting. Am. Heart J. 2006, 151, 922.e1–922.e5. [Google Scholar] [CrossRef]
- Jesurum, J.T.; Fuller, C.J.; Kim, C.J.; Krabill, K.A.; Spencer, M.P.; Olsen, J.V.; Likosky, W.H.; Reisman, M. Frequency of Migraine Headache Relief Following Patent Foramen Ovale “Closure” despite Residual Right-to-Left Shunt. Am. J. Cardiol. 2008, 102, 916–920. [Google Scholar] [CrossRef]
- Khessali, H.; Mojadidi, M.K.; Gevorgyan, R.; Levinson, R.; Tobis, J. The Effect of Patent Foramen Ovale Closure on Visual Aura without Headache or Typical Aura with Migraine Headache. JACC Cardiovasc. Interv. 2012, 5, 682–687. [Google Scholar] [CrossRef]
- Kimmelstiel, C.; Gange, C.; Thaler, D. Is Patent Foramen Ovale Closure Effective in Reducing Migraine Symptoms? A Controlled Study. Catheter. Cardiovasc. Interv. 2007, 69, 740–746. [Google Scholar] [CrossRef] [PubMed]
- Morandi, E.; Anzola, G.P.; Angeli, S.; Melzi, G.; Onorato, E. Transcatheter Closure of Patent Foramen Ovale: A New Migraine Treatment? J. Interv. Cardiol. 2003, 16, 39–42. [Google Scholar] [CrossRef] [PubMed]
- Papa, M.; Gaspardone, A.; Fragasso, G.; Ajello, S.; Gioffrè, G.; Iamele, M.; Iani, C.; Margonato, A. Usefulness of Transcatheter Patent Foramen Ovale Closure in Migraineurs with Moderate to Large Right-to-Left Shunt and Instrumental Evidence of Cerebrovascular Damage. Am. J. Cardiol. 2009, 104, 434–439. [Google Scholar] [CrossRef] [PubMed]
- Reisman, M.; Christofferson, R.D.; Jesurum, J.; Olsen, J.V.; Spencer, M.P.; Krabill, K.A.; Diehl, L.; Aurora, S.; Gray, W.A. Migraine Headache Relief after Transcatheter Closure of Patent Foramen Ovale. J. Am. Coll. Cardiol. 2005, 45, 493–495. [Google Scholar] [CrossRef] [PubMed]
- Vigna, C.; Marchese, N.; Inchingolo, V.; Giannatempo, G.M.; Pacilli, M.A.; Di Viesti, P.; Impagliatelli, M.; Natali, R.; Russo, A.; Fanelli, R.; et al. Improvement of Migraine After Patent Foramen Ovale Percutaneous Closure in Patients with Subclinical Brain Lesions: A Case-Control Study. JACC Cardiovasc. Interv. 2009, 2, 107–113. [Google Scholar] [CrossRef] [PubMed]
- Schwerzmann, M.; Wiher, S.; Nedeltchev, K.; Mattle, H.P.; Wahl, A.; Seiler, C.; Meier, B.; Windecker, S. Percutaneous Closure of Patent Foramen Ovale Reduces the Frequency of Migraine Attacks. Neurology 2004, 62, 1399–1401. [Google Scholar] [CrossRef] [PubMed]
- Pristipino, C.; Germonpre, P.; Toni, D.; Sievert, H.; Meier, B.; D’Ascenzo, F.; Berti, S.; Onorato, E.M.; Bedogni, F.; Mas, J.-L.; et al. European Position Paper on the Management of Patients with Patent Foramen Ovale. Part II—Decompression Sickness, Migraine, Arterial Deoxygenation Syndromes and Select High-Risk Clinical Conditions. Eur. Heart J. 2021, 42, 1545–1553. [Google Scholar] [CrossRef]
- Mojadidi, M.K.; Kumar, P.; Mahmoud, A.N.; Elgendy, I.Y.; Shapiro, H.; West, B.; Charles, A.C.; Mattle, H.P.; Sorensen, S.; Meier, B.; et al. Pooled Analysis of PFO Occluder Device Trials in Patients with PFO and Migraine. J. Am. Coll. Cardiol. 2021, 77, 667–676. [Google Scholar] [CrossRef]
- Anzola, G.P.; Frisoni, G.B.; Morandi, E.; Casilli, F.; Onorato, E. Shunt-Associated Migraine Responds Favorably to Atrial Septal Repair. Stroke 2006, 37, 430–434. [Google Scholar] [CrossRef]
- Post, M.C.; Thijs, V.; Herroelen, L.; Budts, W.I.H.L. Closure of a Patent Foramen Ovale Is Associated with a Decrease in Prevalence of Migraine. Neurology 2004, 62, 1439–1440. [Google Scholar] [CrossRef]
- Wahl, A.; Praz, F.; Tai, T.; Findling, O.; Walpoth, N.; Nedeltchev, K.; Schwerzmann, M.; Windecker, S.; Mattle, H.P.; Meier, B. Improvement of Migraine Headaches after Percutaneous Closure of Patent Foramen Ovale for Secondary Prevention of Paradoxical Embolism. Heart 2010, 96, 967–973. [Google Scholar] [CrossRef] [PubMed]
- Dowson, A.; Mullen, M.J.; Peatfield, R.; Muir, K.; Khan, A.A.; Wells, C.; Lipscombe, S.L.; Rees, T.; De Giovanni, J.V.; Morrison, W.L.; et al. Migraine Intervention With STARFlex Technology (MIST) Trial: A Prospective, Multicenter, Double-Blind, Sham-Controlled Trial to Evaluate the Effectiveness of Patent Foramen Ovale Closure with STARFlex Septal Repair Implant to Resolve Refractory Migraine Headache. Circulation 2008, 117, 1397–1404. [Google Scholar] [CrossRef] [PubMed]
- Tobis, J.M.; Charles, A.; Silberstein, S.D.; Sorensen, S.; Maini, B.; Horwitz, P.A.; Gurley, J.C. Percutaneous Closure of Patent Foramen Ovale in Patients with Migraine: The PREMIUM Trial. J. Am. Coll. Cardiol. 2017, 70, 2766–2774. [Google Scholar] [CrossRef] [PubMed]
- Mattle, H.P.; Evers, S.; Hildick-Smith, D.; Becker, W.J.; Baumgartner, H.; Chataway, J.; Gawel, M.; Göbel, H.; Heinze, A.; Horlick, E.; et al. Percutaneous Closure of Patent Foramen Ovale in Migraine with Aura, a Randomized Controlled Trial. Eur. Heart J. 2016, 37, 2029–2036. [Google Scholar] [CrossRef] [PubMed]
- Vavlitou, A.; Minas, G.; Zannetos, S.; Kyprianou, T.; Tsagourias, M.; Matamis, D. Hemodynamic and Respiratory Factors That Influence the Opening of Patent Foramen Ovale in Mechanically Ventilated Patients. Hippokratia 2016, 20, 209–213. [Google Scholar]
- Altman, M.; Robin, E. Platypnea (Diffuse Zone I Phenomenon?). N. Engl. J. Med. 1969, 281, 1347–1348. [Google Scholar] [CrossRef] [PubMed]
- Landzberg, M.J.; Sloss, L.J.; Faherty, C.E.; Morrison, B.J.; Bittl, J.A.; Bridges, N.D.; Casale, P.N.; Keane, J.F.; Lock, J.E. Orthodeoxia-Platypnea Due to Intracardiac Shunting--Relief with Transcatheter Double Umbrella Closure. Catheter. Cardiovasc. Diagn. 1995, 36, 247–250. [Google Scholar] [CrossRef]
- Blanche, C.; Noble, S.; Roffi, M.; Testuz, A.; Müller, H.; Meyer, P.; Bonvini, J.M.; Bonvini, R.F. Platypnea-Orthodeoxia Syndrome in the Elderly Treated by Percutaneous Patent Foramen Ovale Closure: A Case Series and Literature Review. Eur. J. Intern. Med. 2013, 24, 813–817. [Google Scholar] [CrossRef]
- Mojadidi, M.K.; Gevorgyan, R.; Noureddin, N.; Tobis, J.M. The Effect of Patent Foramen Ovale Closure in Patients with Platypnea-Orthodeoxia Syndrome. Catheter. Cardiovasc. Interv. 2015, 86, 701–707. [Google Scholar] [CrossRef]
- Guérin, P.; Lambert, V.; Godart, F.; Legendre, A.; Petit, J.; Bourlon, F.; De Geeter, B.; Petit, A.; Monrozier, B.; Rossignol, A.M.; et al. Transcatheter Closure of Patent Foramen Ovale in Patients with Platypnea-Orthodeoxia: Results of a Multicentric French Registry. CardioVascular Interv. Radiol. 2005, 28, 164–168. [Google Scholar] [CrossRef]
- Shah, A.H.; Osten, M.; Leventhal, A.; Bach, Y.; Yoo, D.; Mansour, D.; Benson, L.; Wilson, W.M.; Horlick, E. Percutaneous Intervention to Treat Platypnea-Orthodeoxia Syndrome: The Toronto Experience. JACC Cardiovasc. Interv. 2016, 9, 1928–1938. [Google Scholar] [CrossRef] [PubMed]
- De Cuyper, C.; Pauwels, T.; Derom, E.; De Pauw, M.; De Wolf, D.; Vermeersch, P.; Van Berendoncks, A.; Paelinck, B.; Vermeersch, G. Percutaneous Closure of PFO in Patients with Reduced Oxygen Saturation at Rest and during Exercise: Short- and Long-Term Results. J. Interv. Cardiol. 2020, 2020, 9813038. [Google Scholar] [CrossRef] [PubMed]
- Devendra, G.P.; Rane, A.A.; Krasuski, R.A. Provoked Exercise Desaturation in Patent Foramen Ovale and Impact of Percutaneous Closure. JACC Cardiovasc. Interv. 2012, 5, 416–419. [Google Scholar] [CrossRef] [PubMed]
- Rimoldi, S.F.; Ott, S.; Rexhaj, E.; de Marchi, S.F.; Allemann, Y.; Gugger, M.; Scherrer, U.; Seiler, C. Patent Foramen Ovale Closure in Obstructive Sleep Apnea Improves Blood Pressure and Cardiovascular Function. Hypertension 2015, 66, 1050–1057. [Google Scholar] [CrossRef] [PubMed]
- Bove, A.A. Risk of Decompression Sickness with Patent Foramen Ovale. Undersea Hyperb. Med. 1998, 25, 175–178. [Google Scholar] [PubMed]
- Torti, S.R.; Billinger, M.; Schwerzmann, M.; Vogel, R.; Zbinden, R.; Windecker, S.; Seiler, C. Risk of Decompression Illness among 230 Divers in Relation to the Presence and Size of Patent Foramen Ovale. Eur. Heart J. 2004, 25, 1014–1020. [Google Scholar] [CrossRef] [PubMed]
- Liou, K.; Wolfers, D.; Turner, R.; Bennett, M.; Allan, R.; Jepson, N.; Cranney, G. Patent Foramen Ovale Influences the Presentation of Decompression Illness in SCUBA Divers. Heart Lung Circ. 2015, 24. [Google Scholar] [CrossRef] [PubMed]
- Honěk, J.; Šrámek, M.; Honěk, T.; Tomek, A.; Šefc, L.; Januška, J.; Fiedler, J.; Horváth, M.; Novotný, Š.; Brabec, M.; et al. Screening and Risk Stratification Strategy Reduced Decompression Sickness Occurrence in Divers With Patent Foramen Ovale. JACC Cardiovasc. Imaging 2022, 15, 181–189. [Google Scholar] [CrossRef]
- Smart, D.; Mitchell, S.; Wilmshurst, P.; Turner, M.; Banham, N. Joint Position Statement on Persistent Foramen Ovale (PFO) and Diving. South Pacific Underwater Medicine Society (SPUMS) and the United Kingdom Sports Diving Medical Committee (UKSDMC). Diving Hyperb. Med. 2015, 45, 129–131. [Google Scholar]
- Vinay, B.; Sriganesh, K.; Gopala Krishna, K.N. An Abrupt Reduction in End-Tidal Carbon-Dioxide during Neurosurgery Is Not Always Due to Venous Air Embolism: A Capnograph Artefact. J. Clin. Monit. Comput. 2014, 28, 217–219. [Google Scholar] [CrossRef]
- Fathi, A.-R.; Eshtehardi, P.; Meier, B. Patent Foramen Ovale and Neurosurgery in Sitting Position: A Systematic Review. Br. J. Anaesth. 2009, 102, 588–596. [Google Scholar] [CrossRef] [PubMed]
- Laban, J.T.; Rasul, F.T.; Brecker, S.J.D.; Marsh, H.T.; Martin, A.J. Patent Foramen Ovale Closure Prior to Surgery in the Sitting Position. Br. J. Neurosurg. 2014, 28, 421–422. [Google Scholar] [CrossRef] [PubMed]
- Can Posterior Fossa Lesions Be a Place for Preventive Patent Foramen Ovale Transcatheter Closure? Available online: https://www.hmpgloballearningnetwork.com/site/jic/articles/can-posterior-fossa-lesions-be-place-preventive-patent-foramen-ovale-transcatheter-closure (accessed on 21 September 2023).
- Awadalla, H.; Boccalandro, F.; Majano, R.A.; Moustapha, A.; Salloum, J.G.; Smalling, R.W. Percutaneous Closure of Patent Foramen Ovale Guided by Intracardiac Echocardiography and Performed through the Transfemoral Approach in the Presence of Previously Placed Inferior Vena Cava Filters: A Case Series. Catheter. Cardiovasc. Interv. 2004, 63, 242–246. [Google Scholar] [CrossRef] [PubMed]
- Rigatelli, G.; Dell’Avvocata, F.; Ronco, F.; Giordan, M.; Cardaioli, P. Patent Oval Foramen Transcatheter Closure: Results of a Strategy Based on Tailoring the Device to the Specific Patient’s Anatomy. Cardiol. Young 2010, 20, 144–149. [Google Scholar] [CrossRef] [PubMed]
- von Bardeleben, R.S.; Richter, C.; Otto, J.; Himmrich, L.; Schnabel, R.; Kampmann, C.; Rupprecht, H.-J.; Marx, J.; Hommel, G.; Münzel, T.; et al. Long Term Follow up after Percutaneous Closure of PFO in 357 Patients with Paradoxical Embolism: Difference in Occlusion Systems and Influence of Atrial Septum Aneurysm. Int. J. Cardiol. 2009, 134, 33–41. [Google Scholar] [CrossRef] [PubMed]
- Vizzari, G.; Pizzino, F.; Bajwa, T.; Ammar, K.A.; Khandheria, B.K. Amplatzer® Septal Occluder Device Early Embolization to Left Ventricular Outflow Tract in Asymptomatic Patient. Eur. Heart J. Cardiovasc. Imaging 2014, 15, 925. [Google Scholar] [CrossRef] [PubMed]
- McMahon, C.J.; El Said, H.G.; Mullins, C.E. Use of the Transseptal Puncture in Transcatheter Closure of Long Tunnel-Type Patent Foramen Ovale. Heart 2002, 88, e3. [Google Scholar] [CrossRef] [PubMed]
- Thompson, A.J.; Hagler, D.J.; Taggart, N.W. Transseptal Puncture to Facilitate Device Closure of “Long-Tunnel” Patent Foramen Ovale. Catheter. Cardiovasc. Interv. 2015, 85, 1053–1057. [Google Scholar] [CrossRef]
- Echocardiographic Evaluation of Patent Foramen Ovale Prior to Device Closure|Elsevier Enhanced Reader. Available online: https://reader.elsevier.com/reader/sd/pii/S1936878X10001968?token=FAEF20DFAB22B1B75530C4EF88A7091EC13A2950A8616B87E7323474FEA5C8E936436F790A83A71D5104033C6D8CD6D0&originRegion=eu-west-1&originCreation=20230509130737 (accessed on 9 May 2023).
- Medford, B.A.; Taggart, N.W.; Cabalka, A.K.; Cetta, F.; Reeder, G.S.; Hagler, D.J.; Johnson, J.N. Intracardiac Echocardiography during Atrial Septal Defect and Patent Foramen Ovale Device Closure in Pediatric and Adolescent Patients. J. Am. Soc. Echocardiogr. 2014, 27, 984–990. [Google Scholar] [CrossRef]
- Alqahtani, F.; Bhirud, A.; Aljohani, S.; Mills, J.; Kawsara, A.; Runkana, A.; Alkhouli, M. Intracardiac versus Transesophageal Echocardiography to Guide Transcatheter Closure of Interatrial Communications: Nationwide Trend and Comparative Analysis. J. Interv. Cardiol. 2017, 30, 234–241. [Google Scholar] [CrossRef]
- Snijder, R.J.R.; Renes, L.E.; Swaans, M.J.; Suttorp, M.J.; Ten Berg, J.M.; Post, M.C. Microtransesophageal Echocardiographic Guidance during Percutaneous Interatrial Septal Closure without General Anaesthesia. J. Interv. Cardiol. 2020, 2020, 1462140. [Google Scholar] [CrossRef] [PubMed]
- Trabattoni, D.; Gaspardone, A.; Sgueglia, G.A.; Fabbiocchi, F.; Gioffrè, G.; Montorsi, P.; Calligaris, G.; Iamele, M.; De Santis, A.; Bartorelli, A.L. AMPLATZER versus Figulla Occluder for Transcatheter Patent Foramen Ovale Closure. EuroIntervention 2017, 12, 2092–2099. [Google Scholar] [CrossRef] [PubMed]
- Krumsdorf, U.; Ostermayer, S.; Billinger, K.; Trepels, T.; Zadan, E.; Horvath, K.; Sievert, H. Incidence and Clinical Course of Thrombus Formation on Atrial Septal Defect and Patient Foramen Ovale Closure Devices in 1,000 Consecutive Patients. J. Am. Coll. Cardiol. 2004, 43, 302–309. [Google Scholar] [CrossRef] [PubMed]
- Guedeney, P.; Hammoudi, N.; Duthoit, G.; Yan, Y.; Silvain, J.; Pousset, F.; Isnard, R.; Redheuil, A.; Kerneis, M.; Collet, J.-P.; et al. Intravenous Enoxaparin Anticoagulation in Percutaneous Left Atrial Cardiac Procedures. Available online: https://eurointervention.pcronline.com/article/intravenous-enoxaparin-anticoagulation-in-percutaneous-left-atrial-cardiac-procedures (accessed on 10 May 2023).
- Merkler, A.E.; Gialdini, G.; Yaghi, S.; Okin, P.M.; Iadecola, C.; Navi, B.B.; Kamel, H. Safety Outcomes After Percutaneous Transcatheter Closure of Patent Foramen Ovale. Stroke 2017, 48, 3073–3077. [Google Scholar] [CrossRef] [PubMed]
- Turc, G.; Calvet, D.; Guérin, P.; Sroussi, M.; Chatellier, G.; Mas, J. Closure, Anticoagulation, or Antiplatelet Therapy for Cryptogenic Stroke With Patent Foramen Ovale: Systematic Review of Randomized Trials, Sequential Meta-Analysis, and New Insights From the CLOSE Study. J. Am. Heart Assoc. 2018, 7, e008356. [Google Scholar] [CrossRef] [PubMed]
- Berdat, P.A.; Chatterjee, T.; Pfammatter, J.P.; Windecker, S.; Meier, B.; Carrel, T. Surgical Management of Complications after Transcatheter Closure of an Atrial Septal Defect or Patent Foramen Ovale. J. Thorac. Cardiovasc. Surg. 2000, 120, 1034–1039. [Google Scholar] [CrossRef]
- Guedeney, P.; Laredo, M.; Zeitouni, M.; Hauguel-Moreau, M.; Wallet, T.; Elegamandji, B.; Alamowitch, S.; Crozier, S.; Sabben, C.; Deltour, S.; et al. Supraventricular Arrhythmia Following Patent Foramen Ovale Percutaneous Closure. JACC Cardiovasc. Interv. 2022, 15, 2315–2322. [Google Scholar] [CrossRef]
- Goel, S.S.; Aksoy, O.; Tuzcu, E.M.; Krasuski, R.A.; Kapadia, S.R. Embolization of Patent Foramen Ovale Closure Devices: Incidence, Role of Imaging in Identification, Potential Causes, and Management. Tex. Heart Inst. J. 2013, 40, 439–444. [Google Scholar]
- Elmariah, S.; Furlan, A.J.; Reisman, M.; Burke, D.; Vardi, M.; Wimmer, N.J.; Ling, S.; Chen, X.; Kent, D.M.; Massaro, J.; et al. Predictors of Recurrent Events in Patients with Cryptogenic Stroke and Patent Foramen Ovale within the CLOSURE I (Evaluation of the STARFlex Septal Closure System in Patients with a Stroke and/or Transient Ischemic Attack Due to Presumed Paradoxical Embolism Through a Patent Foramen Ovale) Trial. JACC Cardiovasc. Interv. 2014, 7, 913–920. [Google Scholar] [CrossRef]
- Elgendy, A.Y.; Elgendy, I.Y.; Mojadidi, M.K.; Mahmoud, A.N.; Barry, J.S.; Jneid, H.; Wayangankar, S.A.; Tobis, J.M.; Meier, B. New-Onset Atrial Fibrillation Following Percutaneous Patent Foramen Ovale Closure: A Systematic Review and Meta-Analysis of Randomised Trials. EuroIntervention 2019, 14, 1788–1790. [Google Scholar] [CrossRef]
- Staubach, S.; Steinberg, D.H.; Zimmermann, W.; Wawra, N.; Wilson, N.; Wunderlich, N.; Sievert, H. New Onset Atrial Fibrillation after Patent Foramen Ovale Closure. Catheter. Cardiovasc. Interv. 2009, 74, 889–895. [Google Scholar] [CrossRef] [PubMed]
- Rabkin, D.G.; Whitehead, K.J.; Michaels, A.D.; Powell, D.L.; Karwande, S.V. Unusual Presentation of Nickel Allergy Requiring Explantation of an Amplatzer Atrial Septal Occluder Device. Clin. Cardiol. 2009, 32, E55–E57. [Google Scholar] [CrossRef] [PubMed]
- Reddy, B.T.; Patel, J.B.; Powell, D.L.; Michaels, A.D. Interatrial Shunt Closure Devices in Patients with Nickel Allergy. Catheter. Cardiovasc. Interv. 2009, 74, 647–651. [Google Scholar] [CrossRef] [PubMed]
- Dia, A.; Cifu, A.S.; Shah, A.P. Management of Patients with a Patent Foramen Ovale With History of Stroke or TIA. JAMA 2021, 325, 81–82. [Google Scholar] [CrossRef] [PubMed]
- Guedeney, P.; Farjat-Pasos, J.I.; Asslo, G.; Roule, V.; Beygui, F.; Hermida, A.; Gabrion, P.; Leborgne, L.; Houde, D.C.; Huang, F.; et al. Impact of the Antiplatelet Strategy Following Patent Foramen Ovale Percutaneous Closure. Eur. Heart J. Cardiovasc. Pharmacother. 2023, pvad023. [Google Scholar] [CrossRef]
- Trabattoni, D.; Gili, S.; Calligaris, G.; Teruzzi, G.; Troiano, S.; Ravagnani, P.; Santagostino Baldi, G.; Montorsi, P. Patent Foramen Ovale Closure with the Occlutech Figulla Flex II Device: A Long-Term (up to 10-Years) Follow-Up. Int. J. Cardiol. 2023, 387, 131116. [Google Scholar] [CrossRef] [PubMed]
- Deng, W.; Yin, S.; McMullin, D.; Inglessis-Azuaje, I.; Elmariah, S.; Hung, J.; Lo, E.H.; Palacios, I.F.; Buonanno, F.S.; Ning, M. Residual Shunt After Patent Foramen Ovale Closure and Long-Term Stroke Recurrence: A Prospective Cohort Study. Ann. Intern. Med. 2020, 172, 717–725. [Google Scholar] [CrossRef]
- He, L.; Cheng, G.; Du, Y.; Zhang, Y. Importance of Persistent Right-to-Left Shunt After Patent Foramen Ovale Closure in Cryptogenic Stroke Patients. Tex. Heart Inst. J. 2020, 47, 244–249. [Google Scholar] [CrossRef]
- Karagianni, A.; Mandalenakis, Z.; Dellborg, M.; Mirzada, N.; Johansson, M.C.; Eriksson, P. Recurrent Cerebrovascular Events in Patients after Percutaneous Closure of Patent Foramen Ovale. J. Stroke Cerebrovasc. Dis. 2020, 29, 104860. [Google Scholar] [CrossRef]
- Ben-Assa, E.; Rengifo-Moreno, P.; Al-Bawardy, R.; Kolte, D.; Cigarroa, R.; Cruz-Gonzalez, I.; Sakhuja, R.; Elmariah, S.; Pomerantsev, E.; Vaina, L.M.; et al. Effect of Residual Interatrial Shunt on Migraine Burden After Transcatheter Closure of Patent Foramen Ovale. JACC Cardiovasc. Interv. 2020, 13, 293–302. [Google Scholar] [CrossRef]
- Wintzer-Wehekind, J.; Alperi, A.; Houde, C.; Côté, J.-M.; Asmarats, L.; Côté, M.; Rodés-Cabau, J. Long-Term Follow-Up After Closure of Patent Foramen Ovale in Patients with Cryptogenic Embolism. J. Am. Coll. Cardiol. 2019, 73, 278–287. [Google Scholar] [CrossRef] [PubMed]
- Snijder, R.J.R.; Renes, L.E.; Suttorp, M.J.; Ten Berg, J.M.; Post, M.C. Percutaneous Patent Foramen Ovale Closure Using the Occlutech Figulla Device: More than 1,300 Patient-years of Follow Up. Catheter. Cardiovasc. Interv. 2019, 93, 1080–1084. [Google Scholar] [CrossRef] [PubMed]
- Moon, J.; Kim, M.; Oh, P.C.; Shin, D.H.; Park, H.-M.; Jo, Y.Y.; Lee, J.S.; Kang, W.C. Residual Shunt after Patent Foramen Ovale Device Closure in Patients with Cryptogenic Stroke: Serial Bubble Contrast Transesophageal Echocardiography Data. J. Stroke Cerebrovasc. Dis. 2019, 28, 347–353. [Google Scholar] [CrossRef] [PubMed]
- Cheli, M.; Canepa, M.; Brunelli, C.; Bezante, G.P.; Favorini, S.; Rollando, D.; Sivori, G.; Viani, E.; Finocchi, C.; Balbi, M. Recurrent and Residual Shunts After Patent Foramen Ovale Closure: Results From a Long-Term Transcranial Doppler Study: SHUNTS AFTER PATENT FORAMEN OVALE CLOSURE. J. Interv. Cardiol. 2015, 28, 600–608. [Google Scholar] [CrossRef]
- Matsumura, K.; Gevorgyan, R.; Mangels, D.; Masoomi, R.; Mojadidi, M.K.; Tobis, J. Comparison of Residual Shunt Rates in Five Devices Used to Treat Patent Foramen Ovale: Comparison of Residual Shunt Rates. Cathet. Cardiovasc. Intervent. 2014, 84, 455–463. [Google Scholar] [CrossRef]
- Caputi, L.; Butera, G.; Anzola, G.P.; Carminati, M.; Carriero, M.R.; Chessa, M.; Onorato, E.; Rigatelli, G.; Sangiorgi, G.; Santoro, G.; et al. Residual Shunt after Patent Foramen Ovale Closure: Preliminary Results from Italian Patent Foramen Ovale Survey. J. Stroke Cerebrovasc. Dis. 2013, 22, e219–e226. [Google Scholar] [CrossRef] [PubMed]
- Butera, G.; Sarabia, J.F.; Saracino, A.; Chessa, M.; Piazza, L.; Carminati, M. Residual Shunting after Percutaneous PFO Closure: How to Manage and How to Close: Over the Wire Device Implantation. Cathet. Cardiovasc. Intervent. 2013, 82, 950–958. [Google Scholar] [CrossRef]
- Marchese, N.; Pacilli, M.A.; Inchingolo, V.; Fanelli, R.; Loperfido, F.; Vigna, C. Residual Shunt after Percutaneous Closure of Patent Foramen Ovale with AMPLATZER Occluder Devices—Influence of Anatomic Features: A Transcranial Doppler and Intracardiac Echocardiography Study. EuroIntervention 2013, 9, 382–388. [Google Scholar] [CrossRef]
- Wallenborn, J.; Bertog, S.C.; Franke, J.; Steinberg, D.H.; Majunke, N.; Wilson, N.; Wunderlich, N.; Sievert, H. Recurrent Events after Percutaneous Closure of Patent Foramen Ovale: Recurrent Events After PFO Closure. Cathet. Cardiovasc. Intervent. 2013, 82, 541–546. [Google Scholar] [CrossRef]
- Wöhrle, J.; Bertrand, B.; Søndergaard, L.; Turner, M.; Scholtz, W.; Ibrahim, R.; Bourlon, F. PFO closuRE and CryptogenIc StrokE (PRECISE) Registry: A Multi-Center, International Registry. Clin. Res. Cardiol. 2012, 101, 787–793. [Google Scholar] [CrossRef]
- Sorensen, S.G.; Spruance, S.L.; Smout, R.; Horn, S. Transcranial Doppler Quantification of Residual Shunt after Percutaneous Patent Foramen Ovale Closure: Correlation of Device Efficacy with Intracardiac Anatomic Measures: TRANSCRANIAL DOPPLER QUANTIFICATION OF RESIDUAL SHUNT. J. Interv. Cardiol. 2012, 25, 304–312. [Google Scholar] [CrossRef] [PubMed]
- Hammerstingl, C.; Bauriedel, B.; Stüsser, C.; Momcilovic, D.; Tuleta, I.; Nickenig, G.; Skowasch, D. Risk and Fate of Residual Interatrial Shunting after Transcatheter Closure of Patent Foramen Ovale: A Long Term Follow up Study. Eur. J. Med. Res. 2011, 16, 13–19. [Google Scholar] [CrossRef] [PubMed]
- Diaz, T.; Cubeddu, R.J.; Rengifo-Moreno, P.A.; Cruz-Gonzalez, I.; Solis-Martin, J.; Buonanno, F.S.; Inglessis, I.; Palacios, I.F. Management of Residual Shunts after Initial Percutaneous Patent Foramen Ovale Closure: A Single Center Experience with Immediate and Long-Term Follow-Up. Cathet. Cardiovasc. Intervent. 2010, 76, 145–150. [Google Scholar] [CrossRef] [PubMed]
- Greutmann, M.; Greutmann-Yantiri, M.; Kretschmar, O.; Senn, O.; Roffi, M.; Jenni, R.; Luescher, T.F.; Eberli, F.R. Percutaneous PFO Closure with Amplatzer PFO Occluder: Predictors of Residual Shunts at 6 Months Follow-Up. Congenital Heart Disease 2009, 4, 252–257. [Google Scholar] [CrossRef] [PubMed]
- Shafi, N.A.; McKay, R.G.; Kiernan, F.J.; Silverman, I.E.; Ahlquist, M.; Silverman, D.I. Determinants and Clinical Significance of Persistent Residual Shunting in Patients with Percutaneous Patent Foramen Ovale Closure Devices. Int. J. Cardiol. 2009, 137, 314–316. [Google Scholar] [CrossRef] [PubMed]
- Mazzucco, S.; Li, L.; Binney, L.; Rothwell, P.M. Prevalence of Patent Foramen Ovale in Cryptogenic Transient Ischaemic Attack and Non-Disabling Stroke at Older Ages: A Population-Based Study, Systematic Review, and Meta-Analysis. Lancet Neurol. 2018, 17, 609–617. [Google Scholar] [CrossRef]
- Alperi, A.; Guedeney, P.; Horlick, E.; Nombela-Franco, L.; Freixa, X.; Pascual, I.; Mesnier, J.; Houde, C.; Abrahamyan, L.; Monta-lescot, G.; et al. Transcatheter Closure of Patent Foramen Ovale in Older Patients with Cryptogenic Thromboembolic Events. Circ. Cardiovasc. Interv. 2022, 15, 557–565. [Google Scholar] [CrossRef]
- Guedeney, P.; Mesnier, J.; Zeitouni, M.; Hauguel-Moreau, M.; Silvain, J.; Houde, C.; Alperi, A.; Panagides, V.; Collet, J.-P.; Wallet, T.; et al. Outcomes Following Patent Foramen Ovale Percutaneous Closure According to the Delay From Last Ischemic Event. Can. J. Cardiol. 2022, 38, 1228–1234. [Google Scholar] [CrossRef]
| Study | Prevalence of Migraine in Patients Referred for PFO Closure | Endpoint | % Migraine Improvement or Resolution | Follow-Up (Month) |
|---|---|---|---|---|
| Anzola et al., 2006 [60] | 50/163 (31%) | Improvement of migraine score | 88 | 12 |
| Azarbal et al., 2005 [45] | 37/89 (42%) | No. of patients with migraine | 76 | 18 |
| Biasco et al., 2014 [46] | 217/835 (26%) | No. of patients with migraine | 83 | 45 |
| Donti et al.,2006 [47] | 35/131 (27%) | No. of patients with migraine | 91 | 20 |
| Dubiel et al., 2007 [48] | 46/191 (24%) | No. of patients with migraine | 87 | 38 |
| Giardini et al., 2006 [49] | 35/131 (27%) | No. of patients with migraine | 91 | 20.4 |
| Jesurum et al., 2008 [50] | NA | No. of patients with migraine | 77 | 9 |
| Khessali et al., 2012 [51] | 204/590 (35%) | No. of patients with migraine | 76 | 12 |
| Kimmelstiel et al., 2007 [52] | 24/41 (59%) | Patients with migraine and migraine score | 83 | 3 |
| Morandi et al., 2003 [53] | 17/62 (27%) | No. of patients with migraine | 88 | 6 |
| Papa et al.,2009 [54] | 28/76 (37%) | No. of patients with migraine | 82 | 12 |
| Post et al.,2004 [61] | 26/66 (39%) | No. of patients with migraine | 65 | 6 |
| Reisman et al., 2005 [55] | 57/162 (35%) | No. of patients with migraine | 70 | 12 |
| Schwerzmann et al., 2004 [57] | 48/215 (22%) | No. of migraine attacks | 81 | 12 |
| Vigna et al., 2009 [56] | NA | No. of migraine attacks | 89 | 16 |
| Wahl et al., 2010 [62] | 150/603 (25%) | No. of migraine attacks | 85 | 58 |
| Wilmshurst et al., 2000 [43] | 21/37 (57%) | No. of patients with migraine | 86 | 30 |
| Trial | Number of Patients | Device | Follow-Up (Month) | Primary Endpoint | Results |
|---|---|---|---|---|---|
| MIST, Dowson et al., Circulation, 2008 [63] | 432 | Starflex | 6 | Cessation of migraine | No difference between implant and sham groups (3 of 74 versus 3 of 73) (p = 0.51) |
| PREMIUM, Tobis et al., JACC, 2017 [64] | 230 | Amplatzer PFO occlutech | 12 | 50% reduction in migraine attacks | No difference in responder rate in the PFO closure versus control (45 of 117 vs. 33 of 103) (p = 0.32) |
| PRIMA, Mattle et al., EHJ, 2016 [65] | 107 | Amplatzer PFO occlutech | 12 | Reduction in monthly migraine days during months 9–12 after randomization | −2.9 days after PFO closure vs. −1.7 days in control group (p = 0.17) |
| International Position Paper of Underwater Medicine Societies [80] | European Position Paper [58] |
|---|---|
|
|
| Indication | Position Statements |
|---|---|
| Migraine | PFO closure for migraine can be considered for clinical trials or in migraine with aura for compassionate use |
| Desaturation syndromes | Propose PFO closure with shared decision making, if no other factor involved in the desaturation syndrome |
| Decompression sickness | Consider PFO closure in patients with history of DCS when flying/diving cessation is not an option |
| Neurosurgery in sitting position | Consider surgery in prone position |
| Device | Size (Right/Left Atrial Disc) | Sheath Size |
|---|---|---|
| AMPLATZER PFO OCCLUDER (Abbott) | 18 mm (18/18) 25 mm (25/18) 30 mm (30/30) 35 mm (35/25) | 8F 8F 8F 9F |
| AMPLATZER MULTIFENESTRATED SEPTAL OCCLUDER-Cribriform (Abbott) | 18 mm (18/18) 25 mm (25/25) 30 mm (30/30) 35 mm (35/35) 40 mm (40/40) | 8F 8F 8F 9F 9F |
| FIGULLA FLEX II (Occlutech) | 18 mm (18/16) 25 mm (25/23) 30 mm (30/25) 35 mm (35/31) | 7F 9F 9F 11F |
| CARDIOFORM SEPTAL OCCLUDER (Gore) | 20 mm (20/20) 25 mm (25/25) 30 mm (30/30) | 10F 10F 10F |
| Trial | Antiplatelet Therapy |
|---|---|
| CLOSURE-1 | Clopidogrel (75 mg) for 6 months + Aspirin (81–325 mg) for 2 years |
| PC TRIAL | Aspirin (100–325 mg) for 5 to 6 months + Ticlopidine (250–500 mg) or Clopidogrel (75–100 mg) for 1 to 6 months |
| RESPECT | Clopidogrel for 1 month + Aspirin for 6 months, followed by mono-antiplatelet therapy upon investigator’s choice |
| REDUCE | Clopidogrel 300 mg before or after the procedure, followed by Clopidogrel 75 mg for 3 days, and antiplatelet therapy until the end of the study |
| CLOSE | Clopidogrel + Aspirin for 3 months, followed by antiplatelet therapy until the end of the study |
| DEFENSE-PFO | Clopidogrel + Aspirin for at least 6 months, followed by antiplatelet therapy or anticoagulation upon investigator’s choice |
| Study | Prevalence of RS at 6 Month Follow-Up | Risk Factors for RS | Impact on Neurological Recurrences |
|---|---|---|---|
| Trabattoni, 2023 [110] | 3/442 (0.6%) * | NA | 2 patients had recurrent TIA (without RS) |
| Deng, 2020 [111] | 243/1078 (22.5%) $ | NA | RS was associated with an increased risk for stroke or TIA recurrence |
| lu He, 2020 [112] | 3/268 (1.1%) | Persistent RS during normal breathing and the Valsalva maneuver | 2 patients had recurrent TIA (1 with trace RS and 1 without RS) |
| Alexia Karagianni, 2020 [113] | 65/282 (23.7%) | NA | The risk ratio of rCVEs in patients with RS was 2.9 times higher than it was in patients without RS (95% CI: 1.4–6.1) at follow-up visit |
| Eyal Ben-Assa, 2020 [114] | 29/110 (26.3%) | NA | NA |
| Wintzer-Wehekind, 2019 [115] | 6/183 (3.3%) | NA | 2 stroke events (1 related to atherothrombotic disease and 1 due to a vertebral artery dissection) |
| Roel J R Snijder, 2019 [116] | 60/250 (24%) $ | NA | Within the first 12 months, recurrent events occurred in 5 patients (2 with RS) |
| Moon, 2019 [117] | 10/38 (26%) * | NA | NA |
| Cheli, 2015 [118] | 20/120 (17%) | Post-procedural shunt, use of a bigger device (35 vs. 25 mm) | Neurological recurrences (1 stroke, 6 TIA) were equally distributed between the groups |
| Biasco, 2014 [46] | 16/70 (22.8%) | NA | NA |
| Matsumura, 2014 [119] | 17/167 (10.2%) $ | NA | NA |
| Caputi, 2013 [120] | 78/401 (19.5%) | NA | 33.3% of patients with neurological events had RS |
| Butera, 2013 [121] | 27/525 (5.1%) $* | NA | NA |
| Marchese, 2013 [122] | 17/127 (13.3%) $ | Presence of ASA and longitudinal FO dimension > 20.8 mm | NA |
| Wallenborn, 2013 [123] | 146/1775 (8.2%) # | NA | 54/63 events occurred in patients without RS. HR 1.7 [0.8–3.6], p 0.16 |
| Jochen Wöhrle, 2012 [124] | 78/267 (29%) | NA | There was no stroke or TIA during follow-up |
| Sherman G Sorensen, 2012 [125] | 21/135(7%) * | width of the left atrial opening and balloon size | NA |
| Christoph Hammerstingl, 2011 [126] | 22/127 (17.7%) | Helex occluder, PFo- canal- length and extend of atrial-septal-aneurysm | All ischemic events occurred in patients without incidence of RS |
| Tulio Diaz, 2010 [127] | 21/424 (5%) * | 24-hr postprocedure shunt | No deaths, strokes or TIAs were reported in patients with RS |
| Matthias Greutmann, 2009 [128] | 26/135 (17%) | atrial septal aneurysm, devices’s size patients treated (35 mm vs. 25 mm) | 2 patients (1.5%) had recurrent ischemic events during follow-up (1 had RS) |
| Nabil A Shafi, 2009 [129] | 10/51 (19.6%) | PFO canal lengh | No short-term increased risk of TE events |
Disclaimer/Publisher’s Note: The statements, opinions and data contained in all publications are solely those of the individual author(s) and contributor(s) and not of MDPI and/or the editor(s). MDPI and/or the editor(s) disclaim responsibility for any injury to people or property resulting from any ideas, methods, instructions or products referred to in the content. |
© 2023 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Devos, P.; Guedeney, P.; Montalescot, G., on behalf of the ACTION Study Group. Patent Foramen Ovale Percutaneous Closure: Evolution and Ongoing Challenges. J. Clin. Med. 2024, 13, 54. https://doi.org/10.3390/jcm13010054
Devos P, Guedeney P, Montalescot G on behalf of the ACTION Study Group. Patent Foramen Ovale Percutaneous Closure: Evolution and Ongoing Challenges. Journal of Clinical Medicine. 2024; 13(1):54. https://doi.org/10.3390/jcm13010054
Chicago/Turabian StyleDevos, Perrine, Paul Guedeney, and Gilles Montalescot on behalf of the ACTION Study Group. 2024. "Patent Foramen Ovale Percutaneous Closure: Evolution and Ongoing Challenges" Journal of Clinical Medicine 13, no. 1: 54. https://doi.org/10.3390/jcm13010054
APA StyleDevos, P., Guedeney, P., & Montalescot, G., on behalf of the ACTION Study Group. (2024). Patent Foramen Ovale Percutaneous Closure: Evolution and Ongoing Challenges. Journal of Clinical Medicine, 13(1), 54. https://doi.org/10.3390/jcm13010054








