Effects of Occlusal Contact on Maxillary Alveolar Bone Morphology in Patients with and without Anterior Open Bite: A Cross-Sectional Study
Abstract
:1. Introduction
2. Materials and Methods
2.1. Samples
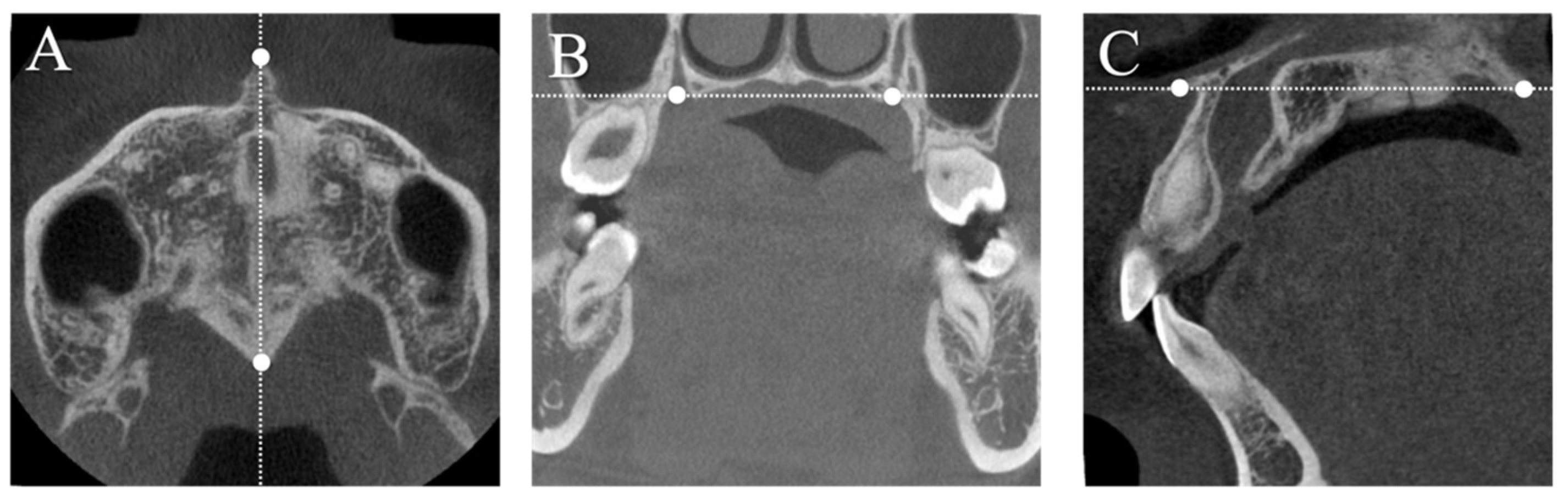
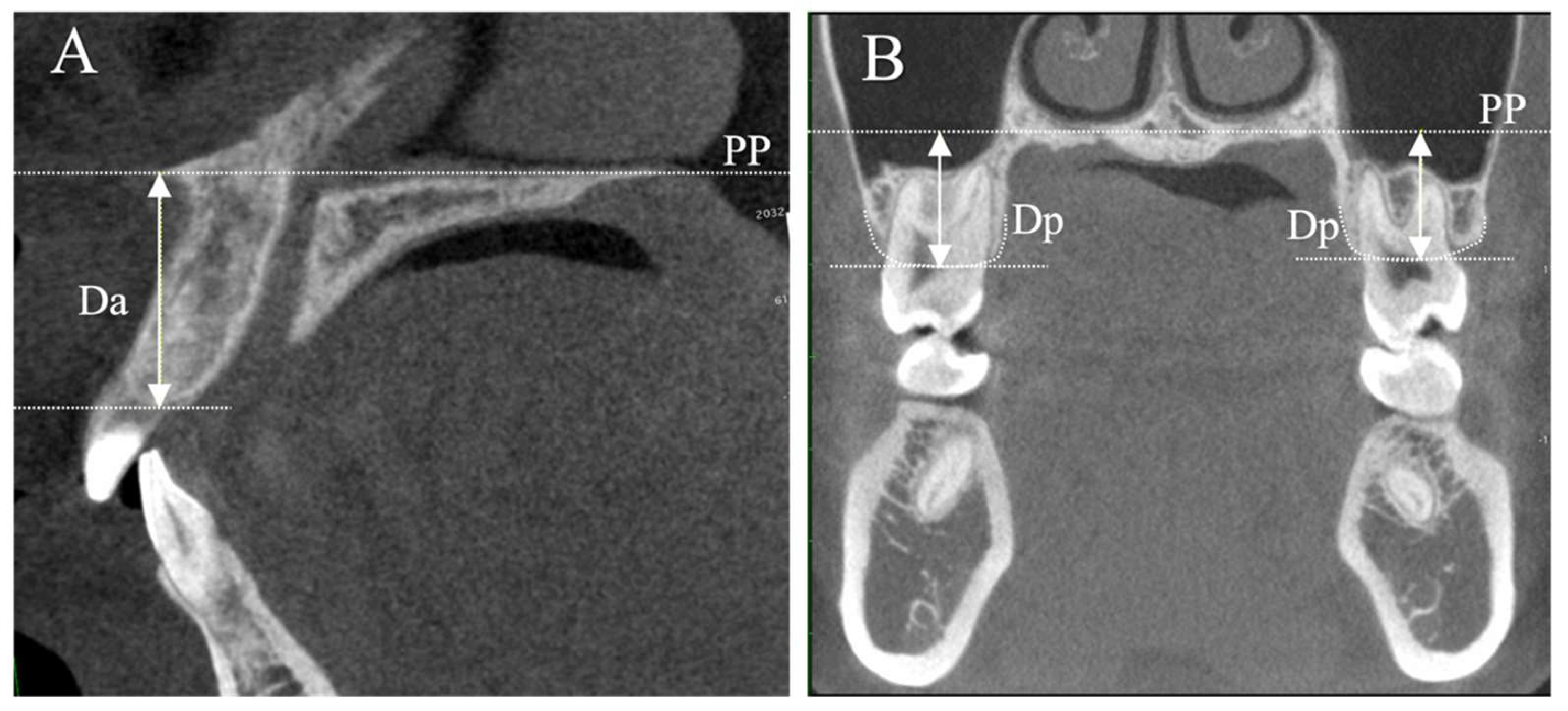
2.2. Measurements
2.3. Statistical Analyses
3. Results
4. Discussion
5. Conclusions
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Acknowledgments
Conflicts of Interest
References
- Kwon, H.J.; Bevis, R.R.; Waite, D.E. Apertognathia (open bite) and its surgical management. Int. J. Oral Surg. 1984, 13, 278–289. [Google Scholar] [CrossRef]
- Kelly, J.E.; Sanchez, M.; Van Kirk, L.E. An assessment of the occlusion of the teeth of children 6–11years, United States. Vital Health Stat. 1973, 130, 1–60. [Google Scholar]
- Ng, C.S.T.; Wong, W.K.R.; Hagg, U. Orthodontic treatment of anterior open bite. Int. J. Paediatr. Dent. 2008, 18, 78–83. [Google Scholar] [CrossRef]
- Curto, A.; Albaladejo, A.; Alvarado-Lorenzo, A. Oral Health-related quality of life (OHRQoL) and anterior open bite in adult patients: A case-control study. Healthcare 2022, 10, 129. [Google Scholar] [CrossRef] [PubMed]
- Keyser, M.M.B.; Lathrop, H.; Jhingree, S.; Giduz, N.; Bocklage, C.; Couldwell, S.; Oliver, S.; Moss, K.; Frazier-Bowers, S.; Phillips, C.; et al. Impacts of skeletal anterior open bite malocclusion on speech. FACE 2022, 3, 339–349. [Google Scholar] [CrossRef] [PubMed]
- Lentini-Oliveira, D.A.; Carvalho, F.R.; Rodrigues, C.G.; Ye, Q.; Prado, L.B.F.; Prado, G.F.; Hu, R. Orthodontic and orthopaedic treatment for anterior open bite in children. Cochrane Database Syst. Rev. 2014, 2014, CD005515. [Google Scholar] [CrossRef]
- Ngan, P.; Fields, H.W. Open bite: A review of etiology and management. Pediatr. Dent. 1997, 19, 91–98. [Google Scholar] [PubMed]
- Huang, G.; Baltuck, C.; Funkhouser, E.; Wang, H.-F.C.; Todoki, L.; Finkleman, S.; Shapiro, P.; Khosravi, R.; Ko, H.-C.J.; Greenlee, G.; et al. The national dental practice-based research network adult anterior open bite study: Treatment recommendations and their association with patient and practitioner characteristics. Am. J. Orthod. Dentofac. Orthop. 2019, 156, 312–325. [Google Scholar] [CrossRef]
- Choi, K.W.; Ko, H.C.; Todoki, L.S.; Finkleman, S.A.; Khosravi, R.; Wang, H.F.; Funkhouser, E.; Baltuck, C.; Raj, V.; Allareddy, V.; et al. The national dental practice-based research network adult anterior open bite study: A description of the practitioners and patients. Angle Orthod. 2018, 88, 675–683. [Google Scholar] [CrossRef]
- Mavropoulos, A.; Kiliaridis, S.; Bresin, A.; Ammann, P. Effect of different masticatory functional and mechanical demands on the structural adaptation of the mandibular alveolar bone in young growing rats. Bone 2004, 35, 191–197. [Google Scholar] [CrossRef]
- Inoue, M.; Ono, T.; Kameo, Y.; Sasaki, F.; Ono, T.; Adachi, T.; Nakashima, T. Forceful mastication activates osteocytes and builds a stout jawbone. Sci. Rep. 2019, 9, 4404. [Google Scholar] [CrossRef] [PubMed]
- Denes, B.J.; Mavropoulos, A.; Bresin, A.; Kiliaridis, S. Influence of masticatory hypofunction on the alveolar bone and the molar periodontal ligament space in the rat maxilla. Eur. J. Oral Sci. 2013, 121, 532–537. [Google Scholar] [CrossRef] [PubMed]
- Enomoto, A.; Watahiki, J.; Yamaguchi, T.; Irie, T.; Tachikawa, T.; Maki, K. Effects of mastication on mandibular growth evaluated by microcomputed tomography. Eur. J. Orthod. 2010, 32, 66–70. [Google Scholar] [CrossRef] [PubMed]
- Sato, H.; Kawamura, A.; Yamaguchi, M.; Kasai, K. Relationship between masticatory function and internal structure of the mandible based on computed tomography findings. Am. J. Orthod. Dentofac. Orthop. 2005, 128, 766–773. [Google Scholar] [CrossRef] [PubMed]
- Kiliaridis, S.; Bresin, A.; Holm, J.; Strid, K.G. Effects of masticatory muscle function on bone mass in the mandible of the growing rat. Acta Anat. 1996, 155, 200–205. [Google Scholar] [CrossRef] [PubMed]
- Shimomoto, Y.; Chung, C.J.; Iwasaki-Hayashi, Y.; Muramoto, T.; Soma, K. Effects of occlusal stimuli on alveolar/jaw bone formation. J. Dent. Res. 2007, 86, 47–51. [Google Scholar] [CrossRef]
- Yamada, K.; Kimmel, D.B. The effect of dietary consistency on bone mass and turnover in the growing rat mandible. Arch. Oral Biol. 1991, 36, 129–138. [Google Scholar] [CrossRef] [PubMed]
- Thongudomporn, U.; Chongsuvivatwong, V.; Geater, A.F. The effect of maximum bite force on alveolar bone morphology. Orthod. Craniofac. Res. 2009, 12, 1–8. [Google Scholar] [CrossRef] [PubMed]
- Jonasson, G.; Kiliaridis, S. The association between the masseter muscle, the mandibular alveolar bone mass and thickness in dentate women. Arch. Oral Biol. 2004, 49, 1001–1006. [Google Scholar] [CrossRef]
- Zhang, X.; Li, Y.; Ge, Z.; Zhao, H.; Miao, L.; Pan, Y. The dimension and morphology of alveolar bone at maxillary anterior teeth in periodontitis: A retrospective analysis-using CBCT. Int. J. Oral Sci. 2020, 12, 4. [Google Scholar] [CrossRef]
- Tang, Y.; Lu, W.; Wu, W.; Sun, Q.; Zhang, Y.; Xu, T.; Chen, S.; Liang, W.; Han, B. Alveolar bone morphology in patients with palatally-displaced maxillary lateral incisors before and after orthodontic treatment: A cone-beam computed tomography study. Orthod. Craniofac. Res. 2024, 27, 55–63. [Google Scholar] [CrossRef] [PubMed]
- Okuzawa-Iwasaki, M.; Ishida, Y.; Ikeda, Y.; Imamura, T.; Oishi, S.; Kita, S.; Matsumura, T.; Sakaguchi-Kuma, T.; Ono, T. Alveolar bone morphology in patients with a unilateral palatally displaced maxillary lateral incisor: A cone-beam computed tomography study. Am. J. Orthod. Dentofac. Orthop. 2020, 158, 28–34. [Google Scholar] [CrossRef] [PubMed]
- Ito, A.; Mayama, A.; Oyanagi, T.; Ogura, H.; Seiryu, M.; Fukunaga, T.; Kitaura, H.; Mizoguchi, I. Three-dimensional morphologic analysis of the maxillary alveolar bone after anterior tooth retraction with temporary anchorage devices. Angle Orthod. 2023, 93, 667–674. [Google Scholar] [CrossRef] [PubMed]
- Tang, Y.; Xu, J.; Hu, Y.; Huang, Y.; Liu, Y.; Daraqel, B.; Zheng, L. Three-dimensional analysis of alveolar bone morphological characteristics in skeletal Class II open bite malocclusion: A cone-beam computed tomography study. Diagnostics 2022, 13, 39. [Google Scholar] [CrossRef] [PubMed]
- Heil, A.; Lazo Gonzalez, E.; Hilgenfeld, T.; Kickingereder, P.; Bendszus, M.; Heiland, S.; Ozga, A.K.; Sommer, A.; Lux, C.J.; Zingler, S. Lateral cephalometric analysis for treatment planning in orthodontics based on MRI compared with radiographs: A feasibility study in children and adolescents. PLoS ONE 2017, 12, e0174524. [Google Scholar] [CrossRef] [PubMed]
- Gandikota, C.S.; Rayapudi, N.; Challa, P.L.; Juvvadi, S.R.; Yudhister, P.V.; Rao, G.H. A comparative study of linear measurements on facial skeleton with frontal and lateral cephalogram. Contemp. Clin. Dent. 2012, 3, 176–179. [Google Scholar] [CrossRef]
- Horibe, Y.; Matsuo, K.; Ikebe, K.; Minakuchi, S.; Sato, Y.; Sakurai, K.; Ueda, T. Relationship between two pressure-sensitive films for testing reduced occlusal force in diagnostic criteria for oral hypofunction. Gerodontology 2022, 39, 3–9. [Google Scholar] [CrossRef] [PubMed]
- Shiga, H.; Komino, M.; Yokoyama, M.; Sano, M.; Arakawa, I.; Nakajima, K.; Fujii, S. Relationship between age and occlusal force in adults with natural dentition. Odontology 2023, 111, 487–492. [Google Scholar] [CrossRef]
- David, O.T.; Tuce, R.A.; Munteanu, O.; Neagu, A.; Panainte, I. Evaluation of the influence of patient positioning on the reliability of lateral cephalometry. Radiol. Med. 2017, 122, 520–529. [Google Scholar] [CrossRef]
- Springate, S.D. The effect of sample size and bias on the reliability of estimates of error: A comparative study of Dahlberg’s formula. Eur. J. Orthod. 2012, 34, 158–163. [Google Scholar] [CrossRef]
- Kim, H.Y. Statistical notes for clinical researchers: The independent samples t-test. Restor. Dent. Endod. 2019, 44, e26. [Google Scholar] [CrossRef] [PubMed]
- Enlow, D.H.; Harvold, E.P.; Latham, R.A.; Moffett, B.C.; Christiansen, R.L.; Hausch, H.G. Research on control of craniofacial morphogenesis: An NIDR state-of-the-art workshop. Am. J. Orthod. 1977, 71, 509–530. [Google Scholar] [CrossRef] [PubMed]
- Yassaei, S.; Ezoddini-Ardakani, F.; Ostovar, N. Predicting the actual length of premolar teeth on the basis of panoramic radiology. Indian J. Dent. Res. 2010, 21, 468–473. [Google Scholar] [CrossRef] [PubMed]
- Brezniak, N.; Goren, S.; Zoizner, R.; Dinbar, A.; Arad, A.; Wasserstein, A.; Heller, M. A comparison of three methods to accurately measure root length. Angle Orthod. 2004, 74, 786–791. [Google Scholar] [CrossRef] [PubMed]
- Hölttä, P.; Nyström, M.; Evälahti, M.; Alaluusua, S. Root-crown ratios of permanent teeth in a healthy Finnish population assessed from panoramic radiographs. Eur. J. Orthod. 2004, 26, 491–497. [Google Scholar] [CrossRef] [PubMed]
- Lund, H.; Gröndahl, K.; Gröndahl, H.G. Cone beam computed tomography for assessment of root length and marginal bone level during orthodontic treatment. Angle Orthod. 2010, 80, 466–473. [Google Scholar] [CrossRef] [PubMed]
- Usumi-Fujita, R.; Hosomichi, J.; Ono, N.; Shibutani, N.; Kaneko, S.; Shimizu, Y.; Ono, T. Occlusal hypofunction causes periodontal atrophy and VEGF/VEGFR inhibition in tooth movement. Angle Orthod. 2013, 83, 48–56. [Google Scholar] [CrossRef] [PubMed]
- Kokich, V.G. Cone-beam computed tomography: Have we identified the orthodontic benefits? Am. J. Orthod. Dentofac. Orthop. 2010, 137, S16. [Google Scholar] [CrossRef] [PubMed]
- Laranjo, F.; Pinho, T. Cephalometric study of the upper airways and dentoalveolar height in open bite patients. Int. Orthod. 2014, 12, 467–482. [Google Scholar] [CrossRef]
- Arriola-Guillén, L.E.; Flores-Mir, C. Molar heights and incisor inclinations in adults with Class II and Class III skeletal open-bite malocclusions. Am. J. Orthod. Dentofac. Orthop. 2014, 145, 325–332. [Google Scholar] [CrossRef]
- Kucera, J.; Marek, I.; Tycova, H.; Baccetti, T. Molar height and dentoalveolar compensation in adult subjects with skeletal open bite. Angle Orthod. 2011, 81, 564–569. [Google Scholar] [CrossRef] [PubMed]
- Teerakanok, S.; Charoemratrote, C.; Chanmanee, P. The accuracy of lateral cephalogram in representing the anterior maxillary dentoalveolar position. Diagnostics 2022, 12, 1840. [Google Scholar] [CrossRef] [PubMed]
- Enlow, D.H. A study of the post-natal growth and remodeling of bone. Am. J. Anat. 1962, 110, 79–101. [Google Scholar] [CrossRef] [PubMed]
- Enlow, D.H.; Bang, S. Growth and remodeling of the human maxilla. Am. J. Orthod. 1965, 51, 446–464. [Google Scholar] [CrossRef] [PubMed]
- Karavade, R.; Kalia, A.; Nene, S.; Khandekar, S.; Patil, V. Comparison of root—Crown lengths and occlusal contacts in patients with Class-III skeletal relationship, anterior Open-Bite and high mandibular plane angle. Int. J. Dent. Med. Spec. 2015, 2, 7. [Google Scholar] [CrossRef]
- Dean, D. Facial Growth, 3rd Ed. By D. H. Enlow. Philadelphia: W. B. Saunders. 1990. 576 Pp. $79.00 (Cloth). Am. J. Phys. Anthropol. 1991, 86, 90–92. [Google Scholar] [CrossRef]
- Kaczmarek, P.; Janiszewska, K.; Metscher, B.; Rupik, W. Development of the squamate Naso-palatal complex: Detailed 3D analysis of the vomeronasal organ and nasal cavity in the brown anole Anolis sagrei (Squamata: Iguania). Front. Zool. 2020, 17, 28. [Google Scholar] [CrossRef] [PubMed]
- Choi, Y.J.; Kim, D.J.; Nam, J.; Chung, C.J.; Kim, K.H. Cephalometric configuration of the occlusal plane in patients with anterior open bite. Am. J. Orthod. Dentofac. Orthop. 2016, 149, 391–400. [Google Scholar] [CrossRef]
- Isaacson, J.R.; Isaacson, R.J.; Speidel, T.M.; Worms, F.W. Extreme variation in vertical facial growth and associated variation in skeletal and dental relations. Angle Orthod. 1971, 41, 219–229. [Google Scholar] [CrossRef]
- Subtelny, J.D.; Sakuda, M. Open-Bite: Diagnosis and treatment. Am. J. Orthod. 1964, 50, 337–358. [Google Scholar] [CrossRef]
- Sassouni, V.; Nanda, S. Analysis of dentofacial vertical proportions. Am. J. Orthod. 1964, 50, 801–823. [Google Scholar] [CrossRef]
- Urzal, V.; Braga, A.C.; Ferreira, A.P. Oral habits as risk factors for anterior open bite in the deciduous and mixed dentition—Cross-sectional study. Eur. J. Paediatr. Dent. 2013, 14, 299–302. [Google Scholar] [PubMed]
- Graber, T.M. The “three M’s”: Muscles, malformation, and malocclusion. Am. J. Orthod. 1963, 49, 418–450. [Google Scholar] [CrossRef]
- Arriola-Guillén, L.E.; Flores-Mir, C. Anterior maxillary dentoalveolar and skeletal cephalometric factors involved in upper incisor crown exposure in subjects with Class II and III skeletal open bite. Angle Orthod. 2015, 85, 72–79. [Google Scholar] [CrossRef] [PubMed]
- Nahoum, H.I.; Horowitz, S.L.; Benedicto, E.A. Varieties of anterior Open-Bite. Am. J. Orthod. 1972, 61, 486–492. [Google Scholar] [CrossRef] [PubMed]
- Nahoum, H.I. Vertical proportions: A guide for prognosis and treatment in anterior Open-Bite. Am. J. Orthod. 1977, 72, 128–146. [Google Scholar] [CrossRef] [PubMed]
- Enokida, M.; Kaneko, S.; Yanagishita, M.; Soma, K. Influence of occlusal stimuli on the remodelling of alveolar bone in a rat hypofunction-recovery model. J. Oral Biosci. 2005, 47, 321–334. [Google Scholar] [CrossRef]
- Watari, I.; Kaneko, S.; Podyma-Inoue, K.A.; Yanagishita, M.; Soma, K. The effect of leptin on rat maxillary alveolar bone under mechanical stimuli. J. Oral Biosci. 2007, 49, 74–83. [Google Scholar] [CrossRef]
- Uehara, S.; Maeda, A.; Tomonari, H.; Miyawaki, S. Relationships between the root–crown ratio and the loss of occlusal contact and high mandibular plane angle in patients with open bite. Angle Orthod. 2013, 83, 36–42. [Google Scholar] [CrossRef]

| Control (n = 25) | AOB (n = 25) | p-Value | |
|---|---|---|---|
| Sex (male/female) | 13/12 | 9/16 | 0.393 |
| Age (year) | 22.2 ± 4.5 | 24.2 ± 6.4 | 0.190 |
| Overbite (mm) | 2.7 ± 1.7 | −2.1 ± 2.2 | <0.001 * |
| SNA (degree) | 82.6 ± 3.1 | 81.2 ± 3.7 | 0.168 |
| SNB (degree) | 80.8 ± 4.5 | 79.8 ± 4.2 | 0.434 |
| ANB (degree) | 1.8 ± 3.3 | 1.4 ± 4.4 | 0.762 |
| MPA (degree) | 26.7 ± 5.9 | 29.2 ± 6.6 | 0.160 |
| SN-GoGn (degree) | 33.6 ± 5.9 | 36.6 ± 6.6 | 0.102 |
| U1 to FH (degree) | 120.8 ± 8.8 | 121.6 ± 7.8 | 0.710 |
| Bite force (N) | 426.7 ± 167.8 | 363.5 ± 148.8 | 0.165 |
| Control | AOB | p-Value | |
|---|---|---|---|
| Da (mm) | 18.67 ± 2.21 | 19.76 ± 2.66 | 0.130 |
| Dp (mm) | 14.12 ± 1.35 | 15.09 ± 1.38 | 0.016 * |
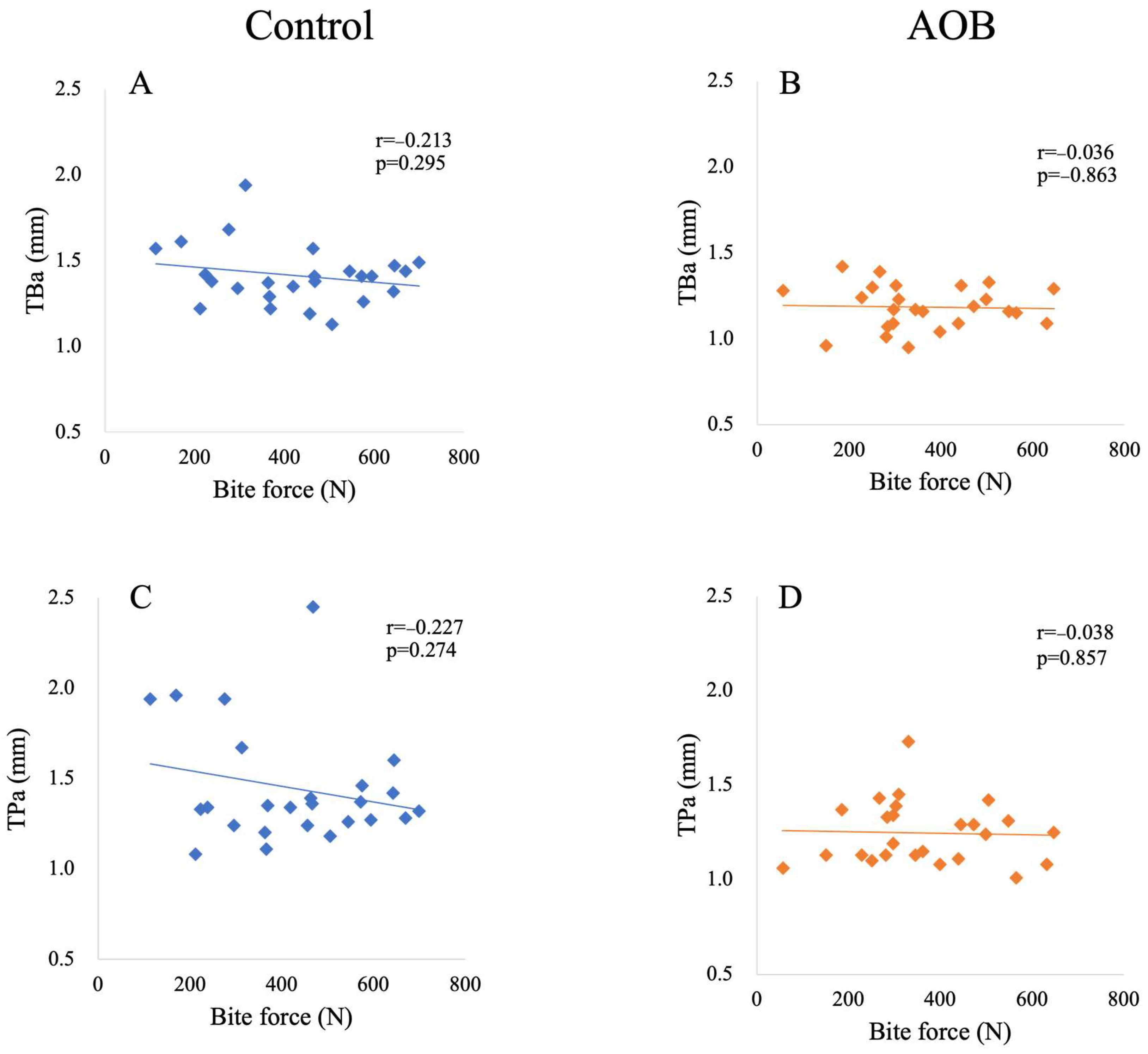
| TBa (mm) | 1.41 ± 0.17 | 1.19 ± 0.13 | <0.001 * |
| TPa (mm) | 1.44 ± 0.32 | 1.25 ± 0.16 | 0.009 * |
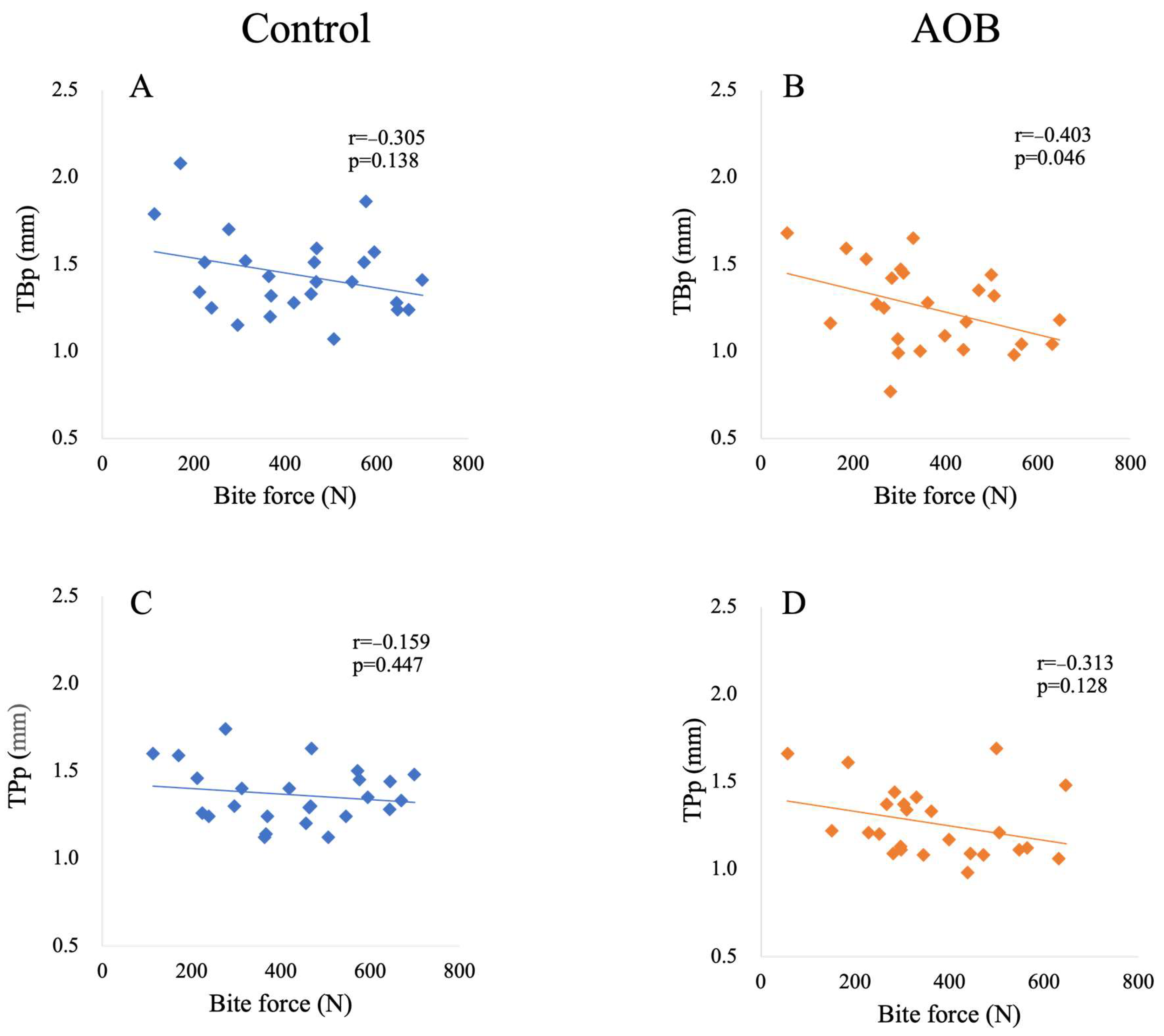
| TBp (mm) | 1.44 ± 0.23 | 1.25 ± 0.24 | 0.006 * |
| TPp (mm) | 1.36 ± 0.16 | 1.26 ± 0.20 | 0.055 |
| Coefficients of Correlation (p-Value) | ||
|---|---|---|
| Control | AOB | |
| TBa vs. bite force | −0.213 (0.295) | −0.036 (0.863) |
| TPa vs. bite force | −0.227 (0.274) | −0.038 (0.857) |
| TBp vs. bite force | −0.305 (0.138) | −0.403 (0.046 *) |
| TPp vs. bite force | −0.159 (0.447) | −0.313 (0.128) |
Disclaimer/Publisher’s Note: The statements, opinions and data contained in all publications are solely those of the individual author(s) and contributor(s) and not of MDPI and/or the editor(s). MDPI and/or the editor(s) disclaim responsibility for any injury to people or property resulting from any ideas, methods, instructions or products referred to in the content. |
© 2024 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Shimizu-Tomoda, C.; Ishida, Y.; Ishizaki-Terauchi, A.; Mizoguchi, Y.; Oishi, S.; Ono, T. Effects of Occlusal Contact on Maxillary Alveolar Bone Morphology in Patients with and without Anterior Open Bite: A Cross-Sectional Study. J. Clin. Med. 2024, 13, 3061. https://doi.org/10.3390/jcm13113061
Shimizu-Tomoda C, Ishida Y, Ishizaki-Terauchi A, Mizoguchi Y, Oishi S, Ono T. Effects of Occlusal Contact on Maxillary Alveolar Bone Morphology in Patients with and without Anterior Open Bite: A Cross-Sectional Study. Journal of Clinical Medicine. 2024; 13(11):3061. https://doi.org/10.3390/jcm13113061
Chicago/Turabian StyleShimizu-Tomoda, Chiyo, Yuji Ishida, Aiko Ishizaki-Terauchi, Yukari Mizoguchi, Shuji Oishi, and Takashi Ono. 2024. "Effects of Occlusal Contact on Maxillary Alveolar Bone Morphology in Patients with and without Anterior Open Bite: A Cross-Sectional Study" Journal of Clinical Medicine 13, no. 11: 3061. https://doi.org/10.3390/jcm13113061





