A Comprehensive Approach to PROMs in Elective Orthopedic Surgery: Comparing Effect Sizes across Patient Subgroups
Abstract
1. Introduction
2. Materials and Methods
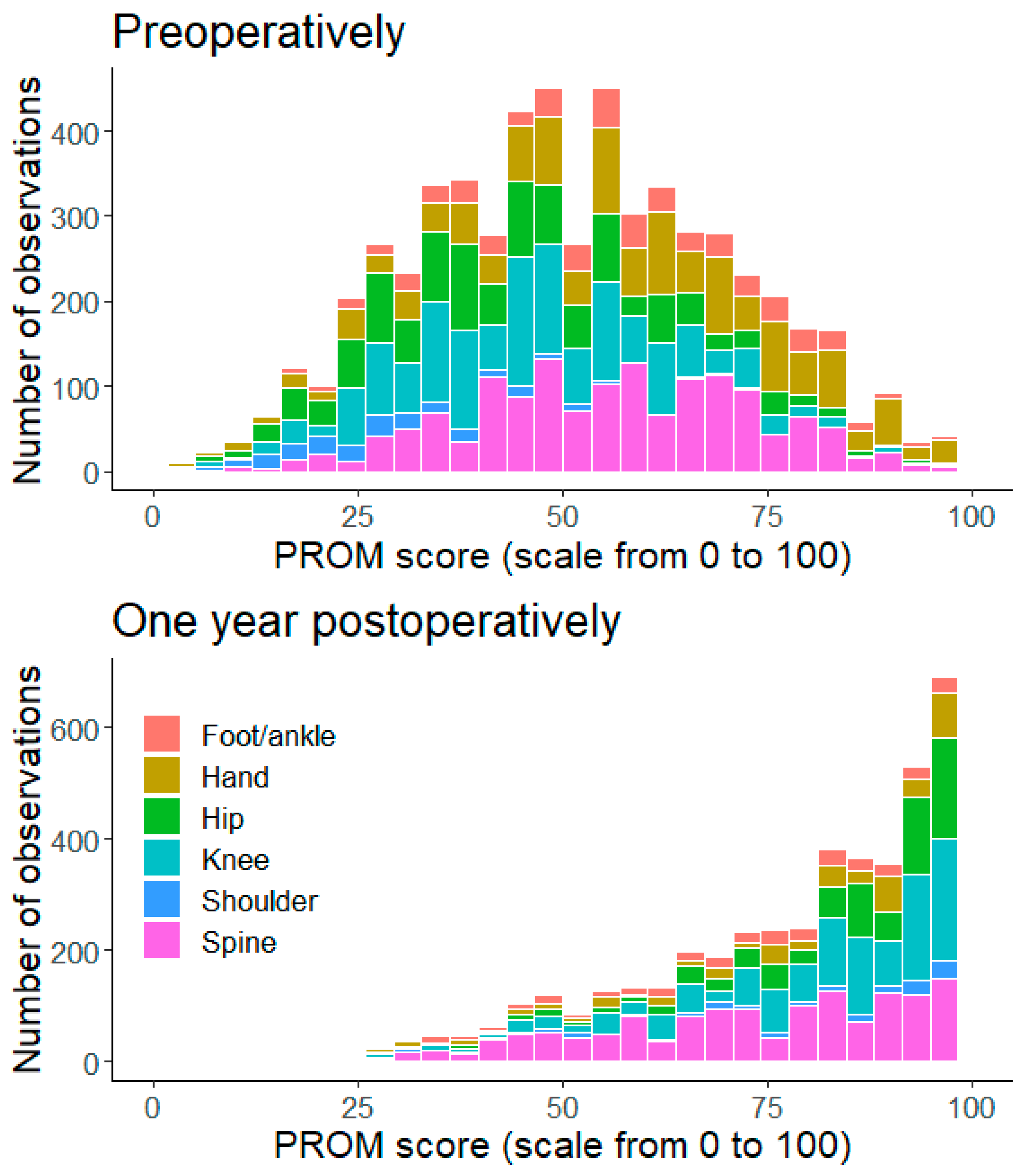
3. Results
4. Discussion
Limitations and Strengths
5. Conclusions
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Acknowledgments
Conflicts of Interest
References
- Wilson, I.; Bohm, E.; Lübbeke, A.; Lyman, S.; Overgaard, S.; Rolfson, O.; W-Dahl, A.; Wilkinson, M.; Dunbar, M. Orthopaedic registries with patient-reported outcome measures. EFORT Open Rev. 2019, 4, 357–367. [Google Scholar] [CrossRef] [PubMed]
- Churruca, K.; Pomare, C.; Ellis, L.A.; Long, J.C.; Henderson, S.B.; Murphy, L.E.D.; Leahy, C.J.; Braithwaite, J. Patient-reported outcome measures (PROMs): A review of generic and condition-specific measures and a discussion of trends and issues. Health Expect. 2021, 24, 1015–1024. [Google Scholar] [CrossRef] [PubMed]
- Rolfson, O.; Bohm, E.; Franklin, P.; Lyman, S.; Denissen, G.; Dawson, J.; Dunn, J.; Eresian Chenok, K.; Dunbar, M.; Overgaard, S.; et al. Patient-reported outcome measures in arthroplasty registries: Report of the Patient-Reported Outcome Measures Working Group of the International Society of Arthroplasty Registries Part II. Recommendations for selection, administration, and analysis. Acta Orthop. 2016, 87, 9–23. [Google Scholar] [CrossRef]
- Harris, K.; Dawson, J.; Gibbons, E.; Lim, C.; Beard, D.; Fitzpatrick, R.; Price, A. Systematic review of measurement properties of patient-reported outcome measures used in patients undergoing hip and knee arthroplasty. Patient Relat. Outcome Meas. 2016, 7, 101–108. [Google Scholar] [CrossRef]
- Pivec, R.; Johnson, A.J.; Mears, S.C.; Mont, M.A. Hip arthroplasty. Lancet 2012, 380, 1768–1777. [Google Scholar] [CrossRef] [PubMed]
- Beard, D.J.; Rees, J.L.; Cook, J.A.; Rombach, I.; Cooper, C.; Merritt, N.; Shirkey, B.A.; Donovan, J.L.; Gwilym, S.; Savulescu, J.; et al. Arthroscopic subacromial decompression for subacromial shoulder pain (CSAW): A multicentre, pragmatic, parallel group, placebo-controlled, three-group, randomised surgical trial. Lancet 2018, 391, 329–338. [Google Scholar] [CrossRef]
- Paavola, M.; Kanto, K.; Ranstam, J.; Malmivaara, A.; Inkinen, J.; Kalske, J.; Savolainen, V.; Sinisaari, I.; Taimela, S.; Järvinen, T.L. Subacromial decompression versus diagnostic arthroscopy for shoulder impingement: A 5-year follow-up of a randomised, placebo surgery controlled clinical trial. Br. J. Sports Med. 2021, 55, 99–107. [Google Scholar] [CrossRef]
- Sihvonen, R.; Paavola, M.; Malmivaara, A.; Itälä, A.; Joukainen, A.; Kalske, J.; Nurmi, H.; Kumm, J.; Sillanpää, N.; Kiekara, T.; et al. Arthroscopic partial meniscectomy for a degenerative meniscus tear: A 5 year follow-up of the placebo-surgery controlled FIDELITY (Finnish Degenerative Meniscus Lesion Study) trial. Br. J. Sports Med. 2020, 54, 1332–1339. [Google Scholar] [CrossRef]
- Brognara, L.; Mazzotti, A.; Arceri, A.; Artioli, E.; Casadei, G.; Bonelli, S.; Traina, F.; Faldini, C. Patient Reported Outcome Measures (PROMs) in Surgery: Evaluation after Minimally Invasive Reduction and Percutaneous K-Wires Fixation for Intra-Articular Calcaneal Fractures. Diseases 2023, 11, 57. [Google Scholar] [CrossRef]
- Gajebasia, S.; Jennison, T.; Blackstone, J.; Zaidi, R.; Muller, P.; Goldberg, A. Patient reported outcome measures in ankle replacement versus ankle arthrodesis—A systematic review. Foot 2022, 51, 101874. [Google Scholar] [CrossRef]
- Black, N. Patient reported outcome measures could help transform healthcare. BMJ 2013, 346, f167. [Google Scholar] [CrossRef]
- Dunbar, M.J.; Richardson, G.; Robertsson, O. I can’t get no satisfaction after my total knee replacement: Rhymes and reasons. Bone Jt. J. 2013, 95-B, 148–152. [Google Scholar] [CrossRef]
- Su, F.; Allahabadi, S.; Bongbong, D.N.; Feeley, B.T.; Lansdown, D.A. Minimal Clinically Important Difference, Substantial Clinical Benefit, and Patient Acceptable Symptom State of Outcome Measures Relating to Shoulder Pathology and Surgery: A Systematic Review. Curr. Rev. Musculoskelet. Med. 2021, 14, 27–46. [Google Scholar] [CrossRef]
- Nyring MR, K.; Olsen, B.S.; Amundsen, A.; Rasmussen, J.V. Minimal Clinically Important Differences (MCID) for the Western Ontario Osteoarthritis of the Shoulder Index (WOOS) and the Oxford Shoulder Score (OSS). Patient Relat. Outcome Meas. 2021, 12, 299–306. [Google Scholar] [CrossRef]
- Steinhaus, M.E.; Iyer, S.; Lovecchio, F.; Khechen, B.; Stein, D.; Ross, T.; Yang, J.; Singh, K.; Albert, T.J.; Lebl, D.; et al. Minimal Clinically Important Difference and Substantial Clinical Benefit Using PROMIS CAT in Cervical Spine Surgery. Clin. Spine Surg. 2019, 32, 392–397. [Google Scholar] [CrossRef]
- Maughan, E.F.; Lewis, J.S. Outcome measures in chronic low back pain. Eur. Spine J. 2010, 19, 1484–1494. [Google Scholar] [CrossRef]
- Yeo, M.G.H.; Goh, G.S.; Chen, J.Y.; Lo, N.-N.; Yeo, S.-J.; Liow, M.H.L. Are Oxford Hip Score and Western Ontario and McMaster Universities Osteoarthritis Index Useful Predictors of Clinical Meaningful Improvement and Satisfaction After Total Hip Arthroplasty? J. Arthroplast. 2020, 35, 2458–2464. [Google Scholar] [CrossRef]
- Ingelsrud, L.H.; Terwee, C.B.; Terluin, B.; Granan, L.P.; Engebretsen, L.; Mills, K.A.G.; Roos, E.M. Meaningful Change Scores in the Knee Injury and Osteoarthritis Outcome Score in Patients Undergoing Anterior Cruciate Ligament Reconstruction. Am. J. Sports Med. 2018, 46, 1120–1128. [Google Scholar] [CrossRef]
- Maredupaka, S.; Meshram, P.; Chatte, M.; Kim, W.H.; Kim, T.K. Minimal clinically important difference of commonly used patient-reported outcome measures in total knee arthroplasty: Review of terminologies, methods and proposed values. Knee Surg. Relat. Res. 2020, 32, 19. [Google Scholar] [CrossRef]
- Larsen, P.; Al-Bayati, M.; Elsøe, R. The Foot and Ankle Outcome Score (FAOS) During Early Recovery After Ankle Fracture. Foot Ankle Int. 2021, 42, 1179–1184. [Google Scholar] [CrossRef] [PubMed]
- Jaeschke, R.; Singer, J.; Guyatt, G.H. Measurement of health status. Ascertaining the minimal clinically important difference. Control. Clin. Trials 1989, 10, 407–415. [Google Scholar] [CrossRef] [PubMed]
- R Core Team. R: A Language and Environment for Statistical Computing; R Foundation for Statistical Computing: Vienna, Austria, 2023; Available online: https://www.R-project.org (accessed on 13 April 2023).
- Karjalainen, T.; Heikkinen, J.; Busija, L.; Jokihaara, J.; Lewin, A.M.; Naylor, J.M.; Harris, L.; Harris, I.A.; Buchbinder, R.; Adie, S. Use of Placebo and Nonoperative Control Groups in Surgical Trials: A Systematic Review and Meta-analysis. JAMA Netw. Open 2022, 5, e2223903. [Google Scholar] [CrossRef] [PubMed]
- Sung, J.; Siegel, J.; Tornetta, P.; Bhandari, M. The orthopaedic trauma literature: An evaluation of statistically significant findings in orthopaedic trauma randomized trials. BMC Musculoskelet. Disord. 2008, 9, 14. [Google Scholar] [CrossRef]
- Cohen, J. A power primer. Psychol. Bull. 1992, 112, 155–159. [Google Scholar] [CrossRef]
- Gates, M.; Tang, A.R.; Godil, S.S.; Devin, C.J.; McGirt, M.J.; Zuckerman, S.L. Defining the relative utility of lumbar spine surgery: A systematic literature review of common surgical procedures and their impact on health states. J. Clin. Neurosci. 2021, 93, 160–167. [Google Scholar] [CrossRef]
- Learmonth, I.D.; Young, C.; Rorabeck, C. The operation of the century: Total hip replacement. Lancet 2007, 370, 1508–1519. [Google Scholar] [CrossRef]
- Rasmussen, J.; Jakobsen, J.; Olsen, B.S.; Brorson, S. Translation and validation of the Western Ontario Osteoarthritis of the Shoulder (WOOS) index—The Danish version. Patient Relat. Outcome Meas. 2013, 4, 49–54. [Google Scholar] [CrossRef] [PubMed]
- Rasmussen, J.V.; Hole, R.; Metlie, T.; Brorson, S.; Äärimaa, V.; Demir, Y.; Salomonsson, B.; Jensen, S.L. Anatomical total shoulder arthroplasty used for glenohumeral osteoarthritis has higher survival rates than hemiarthroplasty: A Nordic registry-based study. Osteoarthr. Cartil. 2018, 26, 659–665. [Google Scholar] [CrossRef]
- Hurley, E.T.; Manjunath, A.K.; Bloom, D.A.; Pauzenberger, L.; Mullett, H.; Alaia, M.J.; Strauss, E.J. Arthroscopic Bankart Repair Versus Conservative Management for First-Time Traumatic Anterior Shoulder Instability: A Systematic Review and Meta-analysis. Arthrosc. J. Arthrosc. Relat. Surg. 2020, 36, 2526–2532. [Google Scholar] [CrossRef]
- Hurley, E.T.; Davey, M.S.; Montgomery, C.; O’Doherty, R.; Gaafar, M.; Pauzenberger, L.; Mullett, H. Arthroscopic Bankart Repair Versus Open Latarjet for Recurrent Shoulder Instability in Athletes. Orthop. J. Sports Med. 2021, 9, 23259671211023801. [Google Scholar] [CrossRef]
- Vandvik, P.O.; Lähdeoja, T.; Ardern, C.; Buchbinder, R.; Moro, J.; Brox, J.I.; Burgers, J.; Hao, Q.; Karjalainen, T.; Bekerom, M.v.D.; et al. Subacromial decompression surgery for adults with shoulder pain: A clinical practice guideline. BMJ 2019, 364, l294. [Google Scholar] [CrossRef] [PubMed]
- Vos, T.; Abajobir, A.A.; Abbafati, C.; Abbas, K.M.; Abate, K.H.; Abd-Allah, F.; Abdulle, A.M.; Abebo, T.A.; Abera, S.F.; Aboyans, V.; et al. Global, regional, and national incidence, prevalence, and years lived with disability for 328 diseases and injuries for 195 countries, 1990–2016: A systematic analysis for the Global Burden of Disease Study 2016. Lancet 2017, 390, 1211–1259. [Google Scholar] [CrossRef] [PubMed]
- World Health Organization (WHO). WHO Web Page. Available online: https://www.who.int (accessed on 25 May 2023).
- Galea, V.P.; Rojanasopondist, P.; Ingelsrud, L.H.; Troelsen, A.; Rubash, H.E.; Bragdon, C.; Malchau, H.; Huddleston, J.I. Longitudinal changes in patient-reported outcome measures following total hip arthroplasty and predictors of deterioration during follow-up: A seven-year prospective international multicentre study. Bone Jt. J. 2019, 101, 768–778. [Google Scholar] [CrossRef] [PubMed]
- Jayakumar, P.; Heng, M.; Okelana, B.; Vrahas, M.; Rodriguez-Villalon, A.; Joeris, A. Patient-Reported Outcome Measurement in Orthopaedic Trauma. J. Am. Acad. Orthop. Surg. 2023, 31, E906–E919. [Google Scholar] [CrossRef] [PubMed]
- Berliner, J.L.; Brodke, D.J.; Chan, V.; SooHoo, N.F.; Bozic, K.J. Can Preoperative Patient-reported Outcome Measures Be Used to Predict Meaningful Improvement in Function After TKA? Clin. Orthop. Relat. Res. 2017, 475, 149–157. [Google Scholar] [CrossRef] [PubMed]
- Wamper, K.E.; Sierevelt, I.N.; Poolman, R.W.; Bhandari, M.; Haverkamp, D. The Harris hip score: Do ceiling effects limit its usefulness in orthopedics? A systematic review. Acta Orthop. 2010, 81, 703–707. [Google Scholar] [CrossRef] [PubMed]
- Gagnier, J.J.; Johnston, B.C. Poor quality patient reported outcome measures bias effect estimates in orthopaedic randomized studies. J. Clin. Epidemiol. 2019, 116, 36–38. [Google Scholar] [CrossRef] [PubMed]
- Angst, F.; Aeschlimann, A.; Angst, J. The minimal clinically important difference raised the significance of outcome effects above the statistical level, with methodological implications for future studies. J. Clin. Epidemiol. 2017, 82, 128–136. [Google Scholar] [CrossRef] [PubMed]
- International Consortium for Health Outcomes Measurement (ICHOM). ICHOM Web Site. Available online: https://www.ichom.org/ (accessed on 7 May 2023).
- Elamo, S.P.; Kukkonen, J.P.; Flinkkilä, T.E.; Lehtinen, J.T.; Joukainen, A.K.; Paloneva, J.J.; Lehtimäki, K.K.; Kauko, T.T.; Äärimaa, V.O. Cross cultural adaptation and psychometric properties of the Finnish version of Western Ontario shoulder instability index (WOSI). BMC Musculoskelet. Disord. 2022, 23, 1127. [Google Scholar] [CrossRef]
- Ketola, H.; Kask, G.; Barner-Rasmussen, I.; Tukiainen, E.; Blomqvist, C.; Laitinen, M.K.; Kautiainen, H.; Kiiski, J.; Repo, J.P. Measuring functional outcome in upper extremity soft-tissue sarcoma: Validation of the Toronto extremity salvage score and the QuickDASH patient-reported outcome instruments. J. Plast. Reconstr. Aesthetic Surg. 2022, 75, 1543–1550. [Google Scholar] [CrossRef]
- Multanen, J.; Honkanen, M.; Häkkinen, A.; Kiviranta, I. Construct validity and reliability of the Finnish version of the Knee Injury and Osteoarthritis Outcome Score. BMC Musculoskelet. Disord. 2018, 19, 155. [Google Scholar] [CrossRef] [PubMed]
- Pekkanen, L.; Kautiainen, H.; Ylinen, J.; Salo, P.; Häkkinen, A. Reliability and validity study of the finnish version 2.0 of the oswestry disability index. Spine 2011, 36, 332–338. [Google Scholar] [CrossRef] [PubMed]
- Reito, A.; Järvistö, A.; Jämsen, E.; Skyttä, E.; Remes, V.; Huhtala, H.; Niemeläinen, M.; Eskelinen, A. Translation and validation of the 12-item Oxford knee score for use in Finland. BMC Musculoskelet. Disord. 2017, 18, 74. [Google Scholar] [CrossRef] [PubMed]
- Salo, P.; Ylinen, J.; Kautiainen, H.; Arkela-Kautiainen, M.; Häkkinen, A. Reliability and validity of the finnish version of the neck disability index and the modified neck pain and disability scale. Spine 2010, 35, 552–556. [Google Scholar] [CrossRef] [PubMed]
- Tapaninaho, K.; Saarinen, A.J.; Ilves, O.; Uimonen, M.M.; Häkkinen, A.H.; Sandelin, H.; Repo, J.P. Structural validity of the foot and ankle outcome score for orthopaedic pathologies with Rasch Measurement Theory. Foot Ankle Surg. 2022, 28, 193–199. [Google Scholar] [CrossRef] [PubMed]
- Edwards, P.; Roberts, I.; Clarke, M.; DiGuiseppi, C.; Pratap, S.; Wentz, R.; Kwan, I. Increasing response rates to postal questionnaires: Systematic review. Br. Med. J. 2002, 324, 1183. [Google Scholar] [CrossRef] [PubMed]
- Edwards, P.J.; Roberts, I.; Clarke, M.J.; DiGuiseppi, C.; Wentz, R.; Kwan, I.; Cooper, R.; Felix, L.M.; Pratap, S. Methods to increase response to postal and electronic questionnaires. Cochrane Database Syst. Rev. 2009, 2009, MR000008. [Google Scholar] [CrossRef] [PubMed]
- Weldring, T.; Smith, S.M.S. Article Commentary: Patient-Reported Outcomes (PROs) and Patient-Reported Outcome Measures (PROMs). Health Serv. Insights 2013, 6, 61–68. [Google Scholar] [CrossRef]
- Karhade, A.V.; Bernstein, D.N.; Desai, V.; Bedair, H.S.; O’Donnell, E.; Tanaka, M.J.; Bono, C.M.; Harris, M.B.; Schwab, J.H.; Tobert, D.G. What Is the Clinical Benefit of Common Orthopaedic Procedures as Assessed by the PROMIS Versus Other Validated Outcomes Tools? Clin. Orthop. Relat. Res. 2022, 480, 1672–1681. [Google Scholar] [CrossRef]
- Ingelsrud, L.H.P.; Wilkinson, J.M.M.C.; Overgaard, S.; Rolfson, O.; Hallstrom, B.; Navarro, R.A.; Terner, M.M.; Karmakar-Hore, S.P.; Webster, G.M.; Slawomirski, L.P.; et al. How do Patient-reported Outcome Scores in International Hip and Knee Arthroplasty Registries Compare? Clin. Orthop. Relat. Res. 2022, 480, 1884–1896. [Google Scholar] [CrossRef]
- Frahm Olsen, M.; Bjerre, E.; Hansen, M.D.; Tendal, B.; Hilden, J.; Hróbjartsson, A. Minimum clinically important differences in chronic pain vary considerably by baseline pain and methodological factors: Systematic review of empirical studies. J. Clin. Epidemiol. 2018, 101, 87–106. [Google Scholar] [CrossRef] [PubMed]

| Patient Group | PROM | Previously Reported MCID | Reference |
|---|---|---|---|
| Hand | Disability of Arm, Shoulder and Hand (quickDASH) | 15.7 ± 8.4 (7.3–24.1%) | [13] |
| Shoulder instability | Western Ontario Shoulder Instability (WOSI) | 510.0 ± 83.4 (20.3–28.3%) | [13] |
| Shoulder rotator cuff | Western Ontario Rotator Cuff (WORC) | 343.6 ± 94.3 (11.9–20.9%) | [13] |
| Shoulder arthroplasty | Western Ontario Osteoarthritis of Shoulder (WOOS) | 12.3 (12.3%) | [14] |
| Cervical spine | Neck Disability Index (NDI) | 8.5 (17%) | [15] |
| Lumbar spine | Oswestry Disability Index (ODI) | 7.5 (7.5%) | [16] |
| Hip | Oxford Hip Score (OHS) | 5.2 (10.8%) | [17] |
| Hip arthroplasty | Oxford Hip Score (OHS) | 5.2 (10.8%) | [17] |
| Knee | Knee Injury and Osteoarthritis Outcome Score (KOOS) | ||
| Pain | 7.9 (7.9%) | [18] | |
| Symptoms | 1.2 (1.2%) | ||
| Activities of Daily Living (ADL) | 8.1 (8.1%) | ||
| Sport and Recreational Function (Sport/Rec) | 21.7 (21.7%) | ||
| Knee-Related Quality of Life (QOL) | 27.3 (27.3%) | ||
| Knee arthroplasty | Oxford Knee Score (OKS) | 4.7–10 (9.8–20.8%) | [19] |
| Foot/Ankle | Foot and Ankle Outcome Score (FAOS) | 14 (20.1%) | [20] |
| Age: Mean (SD) | Female (%) | BMI: Mean (SD) | ASA ≥ 3 | Surgeons | Response Coverage | N | |
|---|---|---|---|---|---|---|---|
| Hand (quickDASH) | 56 (13) | 64 | 29.6 (6.0) | 19% | 12 | 24% | 403 |
| Shoulder (WOSI, WORC, WOOS) | 62 (15) | 53 | 28.8 (4.9) | 34% | 13 | 57% | 160 |
| Spine (NDI, ODI) | 60 (15) | 51 | 28.2 (4.8) | 38% | 36 | 57% | 1217 |
| Hip (OHS) | 67 (12) | 60 | 28.4 (4.6) | 38% | 21 | 67% | 843 |
| Knee (OKS, KOOS) | 68 (11) | 62 | 29.6 (4.4) | 41% | 25 | 69% | 1112 |
| Foot/Ankle (FAOS) | 56 (14) | 71 | 28.2 (5.2) | 21% | 15 | 42% | 304 |
| ALL | 63 (14) | 59% | 28.9 (4.9) | 36% | 74 | 52% | 4039 |
| Diagnosis | Operation | |||
|---|---|---|---|---|
| Hand (quickDASH) | G56.0 | 26% | ACC51 | 22% |
| M72.0 | 8% | NDM10 | 8% | |
| M65.3 | 5% | NDM40 | 5% | |
| Shoulder (WOSI, WORC, WOOS) | M19.0 | 54% | NBB20 | 56% |
| M75.1 | 18% | NBL05 | 13% | |
| M24.4 | 9% | NBL22 | 7% | |
| Spine (NDI, ODI) | M48.0 | 35% | ABC16 | 18% |
| G55.1*M51.1 | 11% | ABC56 | 17% | |
| M51.1 | 10% | ABC36 | 15% | |
| Hip (OHS) | M16.1 | 49% | NFB40 | 64% |
| M16.0 | 35% | NFB30 | 26% | |
| T84.0 | 3% | NFC20 | 3% | |
| Knee (OKS, KOOS) | M17.1 | 47% | NGB20 | 85% |
| M17.0 | 40% | NGB10 | 4% | |
| T84.0 | 2% | NGB40 | 2% | |
| Foot/Ankle (FAOS) | M20.1 | 24% | NHG80 | 20% |
| M19.0 | 12% | NHG26 | 13% | |
| M20.2 | 8% | NHK30 | 10% |
| Mean Effect Size | 95%-C.I. | |
|---|---|---|
| Hand (quickDASH) | 0.93 A | [0.84, 1.03] |
| Shoulder (WOSI, WORC, WOOS) | 3.64 B | [3.36, 3.92] |
| Spine (NDI, ODI) | 1.14 C | [1.07, 1.20] |
| Hip (OHS) | 2.50 D | [2.42, 2.58] |
| Knee (KOOS, OKS) | 2.26 E | [2.18, 2.33] |
| Foot/Ankle (FAOS) | 1.01 A | [0.90, 1.12] |
| MCID Estimate 0.5 SD | Clinically Significant Deterioration | Clinically Significant Improvement | |
|---|---|---|---|
| Hand (quickDASH) | 10.5 | 6% A | 70% A |
| Shoulder (WOSI, WORC, WOOS) | 6.8, 6.0, 7.1 | 2% BC | 93% BC |
| Spine (NDI, ODI) | 8.3, 8.8 | 6% AB | 69% A |
| Hip (OHS) | 8.7 | 1% C | 94% B |
| Knee (KOOS, OKS) | 10.3, 7.7 | 2% C | 91% C |
| Foot/Ankle (FAOS) | 9.3 | 6% AB | 70% A |
Disclaimer/Publisher’s Note: The statements, opinions and data contained in all publications are solely those of the individual author(s) and contributor(s) and not of MDPI and/or the editor(s). MDPI and/or the editor(s) disclaim responsibility for any injury to people or property resulting from any ideas, methods, instructions or products referred to in the content. |
© 2024 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Äärimaa, V.; Kohtala, K.; Rantalaiho, I.; Ekman, E.; Mäkelä, K.; Taskinen, H.-S.; Ryösä, A.; Kostensalo, J.; Meronen, S.; Laaksonen, I. A Comprehensive Approach to PROMs in Elective Orthopedic Surgery: Comparing Effect Sizes across Patient Subgroups. J. Clin. Med. 2024, 13, 3073. https://doi.org/10.3390/jcm13113073
Äärimaa V, Kohtala K, Rantalaiho I, Ekman E, Mäkelä K, Taskinen H-S, Ryösä A, Kostensalo J, Meronen S, Laaksonen I. A Comprehensive Approach to PROMs in Elective Orthopedic Surgery: Comparing Effect Sizes across Patient Subgroups. Journal of Clinical Medicine. 2024; 13(11):3073. https://doi.org/10.3390/jcm13113073
Chicago/Turabian StyleÄärimaa, Ville, Karita Kohtala, Ida Rantalaiho, Elina Ekman, Keijo Mäkelä, Hanna-Stiina Taskinen, Anssi Ryösä, Joel Kostensalo, Saara Meronen, and Inari Laaksonen. 2024. "A Comprehensive Approach to PROMs in Elective Orthopedic Surgery: Comparing Effect Sizes across Patient Subgroups" Journal of Clinical Medicine 13, no. 11: 3073. https://doi.org/10.3390/jcm13113073
APA StyleÄärimaa, V., Kohtala, K., Rantalaiho, I., Ekman, E., Mäkelä, K., Taskinen, H.-S., Ryösä, A., Kostensalo, J., Meronen, S., & Laaksonen, I. (2024). A Comprehensive Approach to PROMs in Elective Orthopedic Surgery: Comparing Effect Sizes across Patient Subgroups. Journal of Clinical Medicine, 13(11), 3073. https://doi.org/10.3390/jcm13113073





