Short-Term Clinical Results of Minimally Invasive Direct Coronary Artery Bypass (MIDCAB) Procedure
Abstract
1. Introduction
2. Material and Methods
2.1. Study Design and Population
2.2. Patient Selection Criteria
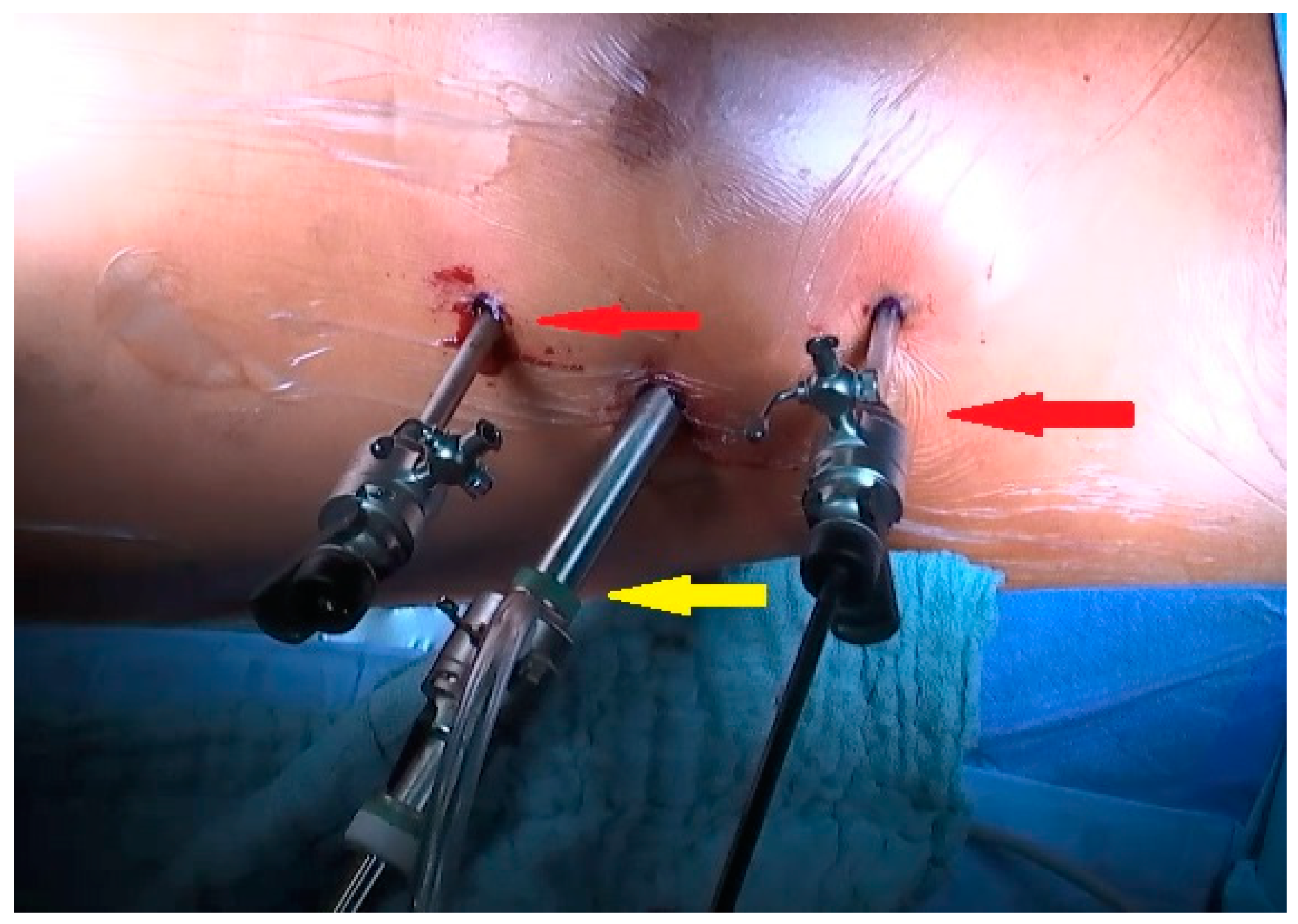
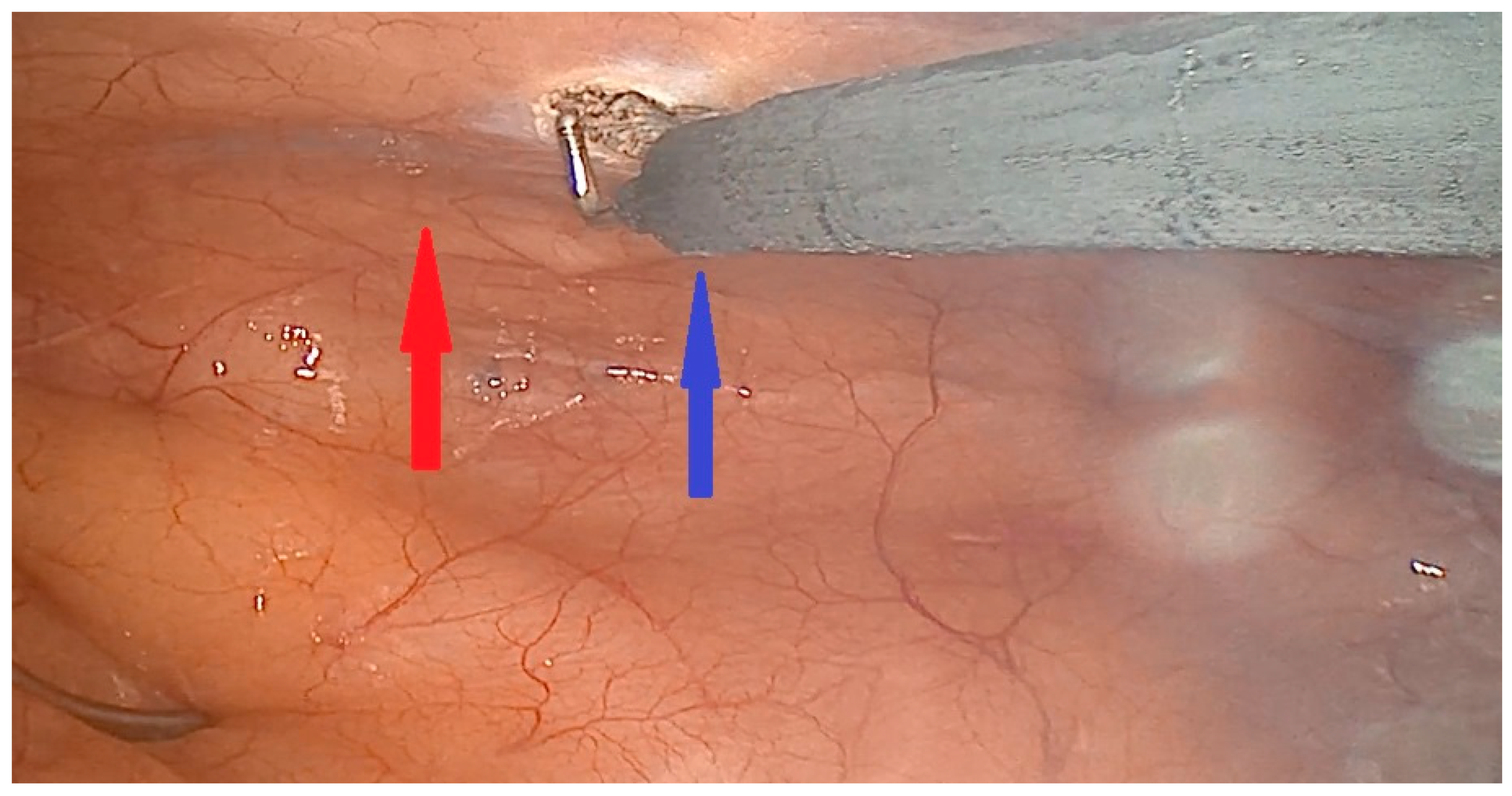
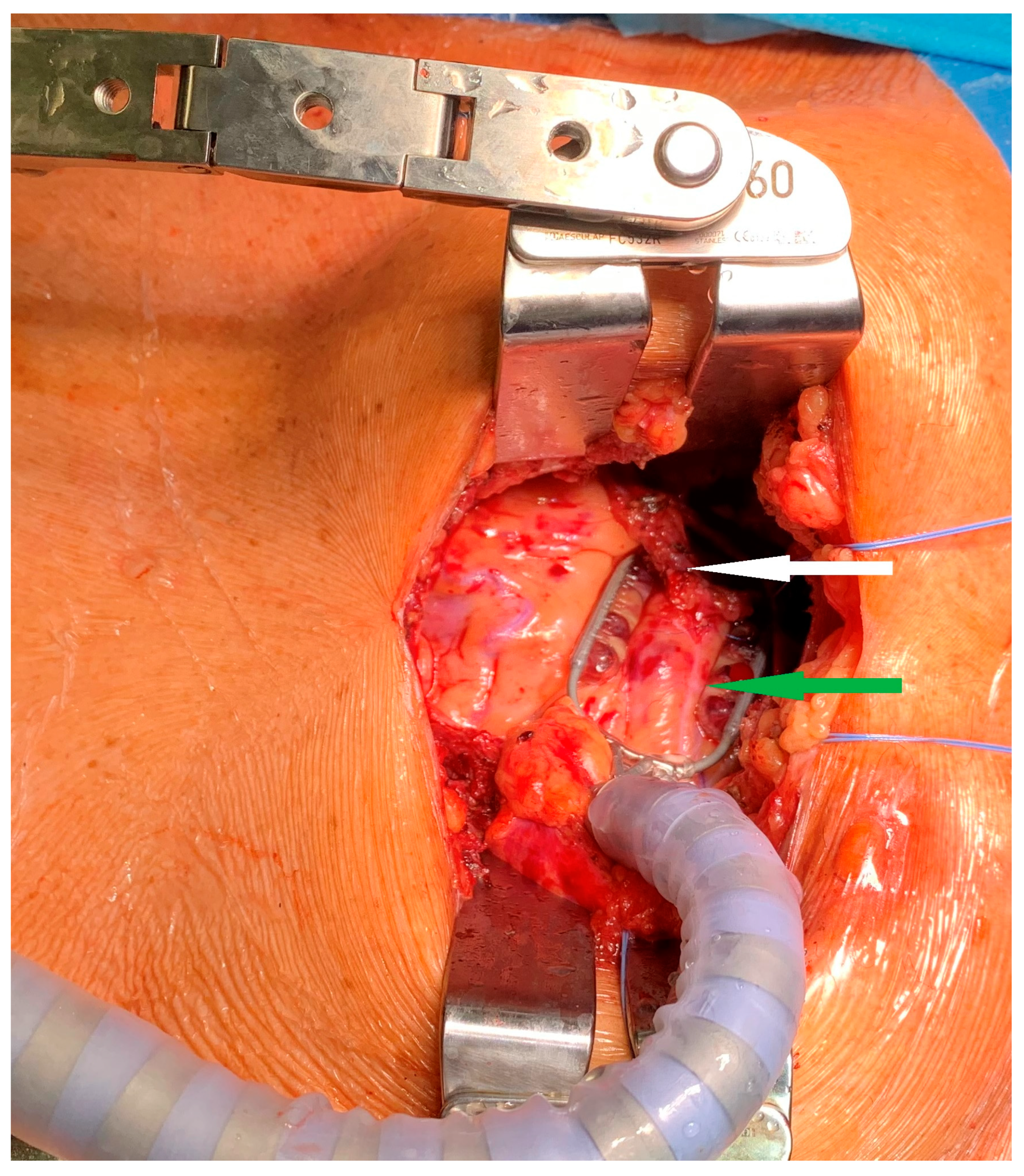
2.3. Surgical Technique
2.4. Postoperative Care and Clinical Follow-Up
2.5. Statistical Analysis
3. Results
3.1. Preoperative Data
3.2. Operative and Postoperative Results
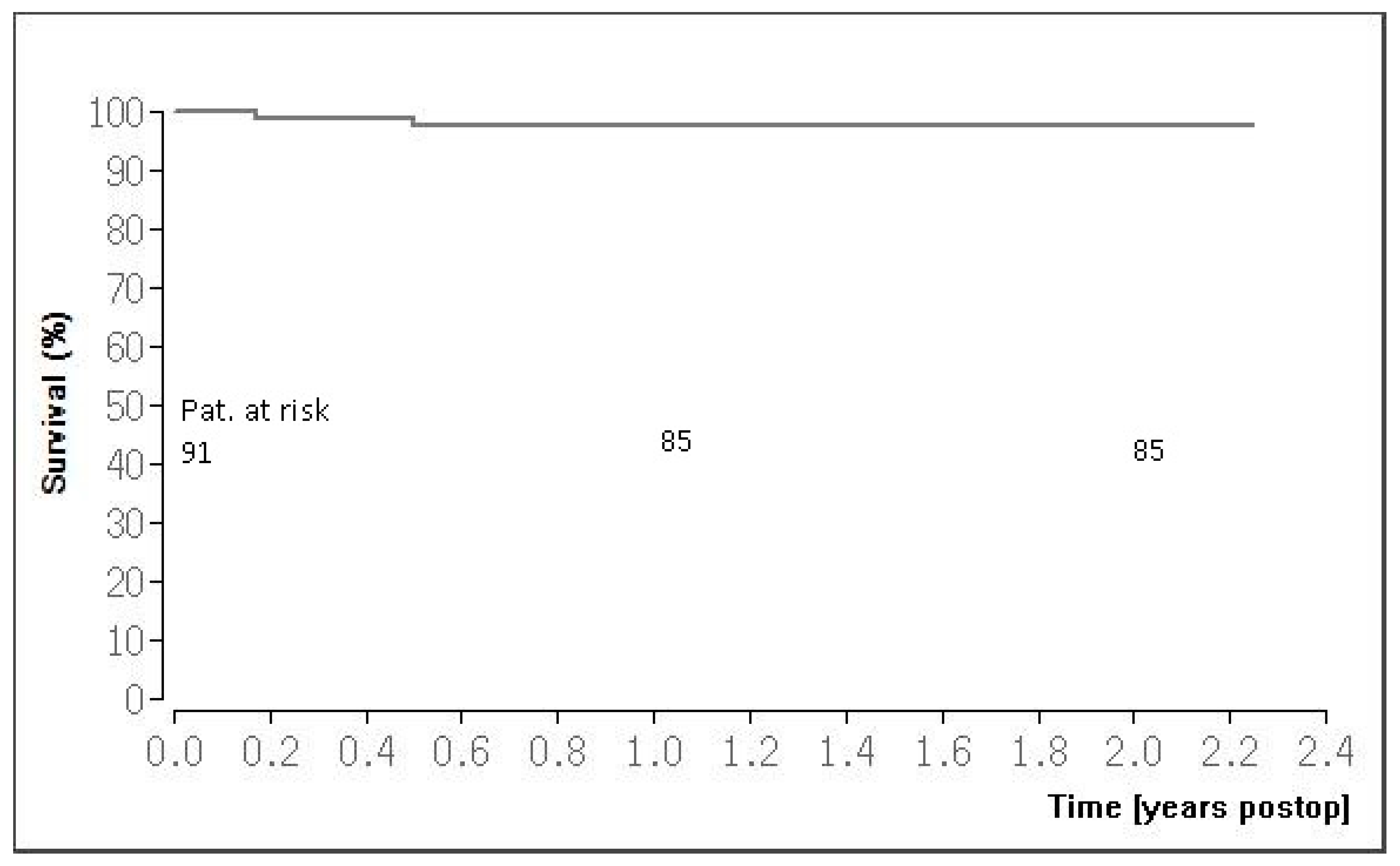
3.3. Follow-Up Results
4. Discussion
5. Conclusions
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Conflicts of Interest
References
- Smith, S.C.; Benjamin, E.J.; Bonow, R.O.; Braun, L.T.; Creager, M.A.; Franklin, B.A.; Gibbons, R.J.; Grundy, S.M.; Hiratzka, L.F.; Jones, D.W.; et al. AHA/ACCF Secondary Prevention and Risk Reduction Therapy for Patients with Coronary and other Atherosclerotic Vascular Disease: 2011 update: A guideline from the American Heart Association and American College of Cardiology foundation endorsed by the World Heart Federation and the Preventive Cardiovascular Nurses Association. J. Am. Coll Cardiol. 2011, 58, 2432–2446. [Google Scholar] [PubMed]
- Chang, M.; Lee, C.W.; Ahn, J.M.; Cavalcante, R.; Sotomi, Y.; Onuma, Y.; Park, D.-W.; Kang, S.-J.; Lee, S.-W.; Kim, Y.-H.; et al. Coronary artery bypass graft surgery versus drug-eluting stent implantation for high-surgical-risk patients with left main or multivessel coronary artery disease. Eur. J. Cardiothorac. Surg. 2017, 51, 943–949. [Google Scholar] [CrossRef] [PubMed]
- Van Praet, K.M.; Kofler, M.; Nazari Shafti, T.Z.; Abd, A.; van Kampen, A.; Amabile, A.; Torregrossa, G.; Kempfert, J.; Falk, V.; Balkhy, H.H.; et al. Minimally invasive coronary revascularisation surgery: A focused review of the available literature. Interv. Cardiol. Rev. 2021, 16, e08. [Google Scholar] [CrossRef] [PubMed]
- Varrone, M.; Sarmiento, I.C.; Pirelli, L.; Brinster, D.R.; Singh, V.P.; Kim, M.C.; Scheinerman, S.J.; Patel, N.C.; Hemli, J.M. Minimally invasive direct coronary artery bypass: An evolving paradigm over the past 25 years. Innovations 2022, 17, 521–527. [Google Scholar] [CrossRef] [PubMed]
- Tiwari, K.K.; Wadhawa, V.; Jawarkar, M.; Rathod, D.; Shah, M.; Manek, P.; Doshi, C. Total arterial multivessels minimally invasive direct coronary artery bypass grafting via left minithoracotomy. Gen. Thorac. Cardiovasc. Surg. 2021, 69, 8–13. [Google Scholar] [CrossRef] [PubMed]
- Al-Ruzzeh, S.; Mazrani, W.; Wray, J.; Modine, T.; Nakamura, K.; George, S.; Ilsley, C.; Amrani, M. The clinical outcome and quality of life following minimally invasive direct coronary artery bypass surgery. J. Card. Surg. 2004, 19, 12–16. [Google Scholar] [CrossRef]
- Tekin, A.I.; Arslan, Ü. Perioperative outcomes in minimally invasive direct coronary artery bypass versus off-pump coronary artery bypass with sternotomy. Videosurg. Other Miniinvasive Tech. 2017, 12, 285–290. [Google Scholar] [CrossRef]
- Yang, M.; Xiao, L.-B.; Gao, Z.-S.; Zhou, J.-W. Clinical effect and prognosis of off-pump minimally invasive direct coronary artery bypass. Med. Sci. Monit. 2017, 23, 1123–1128. [Google Scholar] [CrossRef] [PubMed]
- Monsefi, N.; Alaj, E.; Sirat, S.; Bakhtiary, F. Postoperative results in minimally invasive direct coronary artery bypass procedure in 234 patients. Front. Cardiovasc. Med. 2023, 9, 1051105. [Google Scholar] [CrossRef] [PubMed]
- Kettering, K.; Dapunt, O.; Baer, F.M. Minimally invasive direct coronary artery bypass grafting: A systematic review. J. Cardiovasc. Surg. 2004, 45, 255–264. [Google Scholar]
- Blum, A. Gender differences in vascular aging and in coronary artery disease pathophysiology. QJM Int. J. Med. 2023, 116, 745–749. [Google Scholar] [CrossRef] [PubMed]
- Raja, S.G.; Garg, S.; Rochon, M.; Daley, S.; De Robertis, F.; Bahrami, T. Short-term clinical outcomes and long-term survival of minimally invasive direct coronary artery bypass grafting. Ann. Cardiothorac. Surg. 2018, 7, 521–627. [Google Scholar] [CrossRef] [PubMed]
- Holzhey, D.M.; Cornely, J.P.; Rastan, A.J.; Davierwala, P.; Mohr, F.W. Review of a 13-year single-center experience with minimally invasive direct coronary artery bypass as the primary surgical treatment of coronary artery disease. Heart. Surg. Forum. 2012, 15, E61–E68. [Google Scholar] [CrossRef] [PubMed]
- Calafiore, A.M.; Angelini, G.D.; Bergsland, J.; Salerno, T.A. Minimally invasive coronary artery bypass grafting. Ann. Thorac. Surg. 1996, 62, 1445–1448. [Google Scholar] [CrossRef] [PubMed]
- Manuel, L.; Fong, L.S.; Betts, K.; Bassin, L.; Wolfenden, H. LIMA to LAD grafting returns patient survival to age-matched population: 20-year outcomes of MIDCAB surgery. Interact. Cardiovasc. Thorac. Surg. 2022, 35, ivac243. [Google Scholar] [CrossRef] [PubMed]
- Reuthebuch, O.; Stein, A.; Koechlin, L.; Gahl, B.; Berdajs, D.; Santer, D.; Eckstein, F. Five-Year Survival of Patients Treated with Minimally Invasive Direct Coronary Artery Bypass (MIDCAB) Compared with the General Swiss Population. Thorac. Cardiovasc. Surg. 2023. online ahead of print. [Google Scholar] [CrossRef]
| Parameter | |
|---|---|
| Number of patients, n | 91 |
| Age, M ± SD (years) | 65.1 ± 10.1 |
| Gender, male n (%) | 79 (86.8%) |
| NYHA class 1 | 0 |
| NYHA class 2 | 16 (17.6%) |
| NYHA class 3 | 71 (78.0%) |
| NYHA class 4 | 4 (4.4%) |
| CCS class 0 | 0 |
| CCS class 1 | 3 (3.3%) |
| CCS class 2 | 23 (25.3%) |
| CCS class 3 | 62 (68.1%) |
| CCS class 4 | 3 (3.3%) |
| CAD 1 Vessel, n (%) CAD 2 Vessels, n (%) CAD 3 Vessels, n (%) | 18 (19.7%) 24 (26.3%) 49 (53.8%) |
| Ejection Fraction, M ± SD (%) Comorbidities | 50.2 ± 10.7 |
| Diabetes mellitus, n (%) | 26 (28.6%) |
| COPD, n (%) | 9 (9.9%) |
| Renal insufficiency, n (%) | 8 (8.8%) |
| Myocardial infarction, n (%) | 29 (31.9%) |
| Arterial hypertension, n (%) | 63 (69.2%) |
| EUROScore I log., (M ± SD %) | 5.2 ± 11.2 |
| Peripheral Arterial Disease (PAD), n (%) | 19 (20.9%) |
| Stent, n (%) | 14 (15.4%) |
| Operative | |
|---|---|
| One coronary art anastomosis, n (%) | 77(84.6%) |
| Two coronary artery anastomoses, n (%) | 10 (11.0%) |
| Three coronary artery anastomoses, n (%) | 4 (4.4%) |
| Operation time, M ± SD (h) | 2.6 ± 0.8 |
| Conversion to sternotomy, n (%) | 0 |
| Number of anastomoses, n | 109 |
| postoperative | |
| Intensive care unit (ICU) length of stay M ± SD (Days) | 1.5 ± 1.6 |
| Ventilation time, M ± SD (hours) | 4.0 ± 6.0 |
| Rethoracotomy, n (%) | 4 (4.4%) |
| Stroke, n (%) | 0 |
| Wound infection, n (%) | 2 (2.2%) |
| 30-day mortality, n (%) | 0 |
| Myocardial infarction, n (%) | 1 (1.0%) |
| Stent, n (%) | 1 (1.0%) |
| Coronary angiography, n (%) | 1 (1.0%) |
| Blood transfusion (pRBCs), n (%) | 0.4 ± 1.2 |
| Complete revascularization, n (%) | 73 (80.2%) |
| Hybrid revascularization, n (%) | 18 (19.8%) |
| Parameter | |
|---|---|
| Number of patients, n | 89 |
| NYHA class 1 | 78 (87.6%) |
| NYHA class 2 | 11 (12.4%) |
| NYHA class 3 | 0 |
| NYHA class 4 | 0 |
| CCS class 0 | 85 (95.5%) |
| CCS class 1 | 4 (4.5%) |
| CCS class 2 | 0 |
| CCS class 3 | 0 |
| CCS class 4 | 0 |
| Coronary angiography, n (%) Stent, PCI n (%) Mortality, n (%) | 1 (1.1%) 1 (1.1%) 2 (2.2%) |
| Myocardial infarction, n (%) | 0 |
Disclaimer/Publisher’s Note: The statements, opinions and data contained in all publications are solely those of the individual author(s) and contributor(s) and not of MDPI and/or the editor(s). MDPI and/or the editor(s) disclaim responsibility for any injury to people or property resulting from any ideas, methods, instructions or products referred to in the content. |
© 2024 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Alaj, E.; Seidiramool, V.; Ciobanu, V.; Bakhtiary, F.; Monsefi, N. Short-Term Clinical Results of Minimally Invasive Direct Coronary Artery Bypass (MIDCAB) Procedure. J. Clin. Med. 2024, 13, 3124. https://doi.org/10.3390/jcm13113124
Alaj E, Seidiramool V, Ciobanu V, Bakhtiary F, Monsefi N. Short-Term Clinical Results of Minimally Invasive Direct Coronary Artery Bypass (MIDCAB) Procedure. Journal of Clinical Medicine. 2024; 13(11):3124. https://doi.org/10.3390/jcm13113124
Chicago/Turabian StyleAlaj, Eissa, Vahid Seidiramool, Veaceslav Ciobanu, Farhad Bakhtiary, and Nadejda Monsefi. 2024. "Short-Term Clinical Results of Minimally Invasive Direct Coronary Artery Bypass (MIDCAB) Procedure" Journal of Clinical Medicine 13, no. 11: 3124. https://doi.org/10.3390/jcm13113124
APA StyleAlaj, E., Seidiramool, V., Ciobanu, V., Bakhtiary, F., & Monsefi, N. (2024). Short-Term Clinical Results of Minimally Invasive Direct Coronary Artery Bypass (MIDCAB) Procedure. Journal of Clinical Medicine, 13(11), 3124. https://doi.org/10.3390/jcm13113124







