Comparison of Macintosh Laryngoscope, King Vision®, VividTrac®, AirAngel Blade®, and a Custom-Made 3D-Printed Video Laryngoscope for Difficult and Normal Airways in Mannequins by Novices—A Non-Inferiority Trial
Abstract
1. Introduction
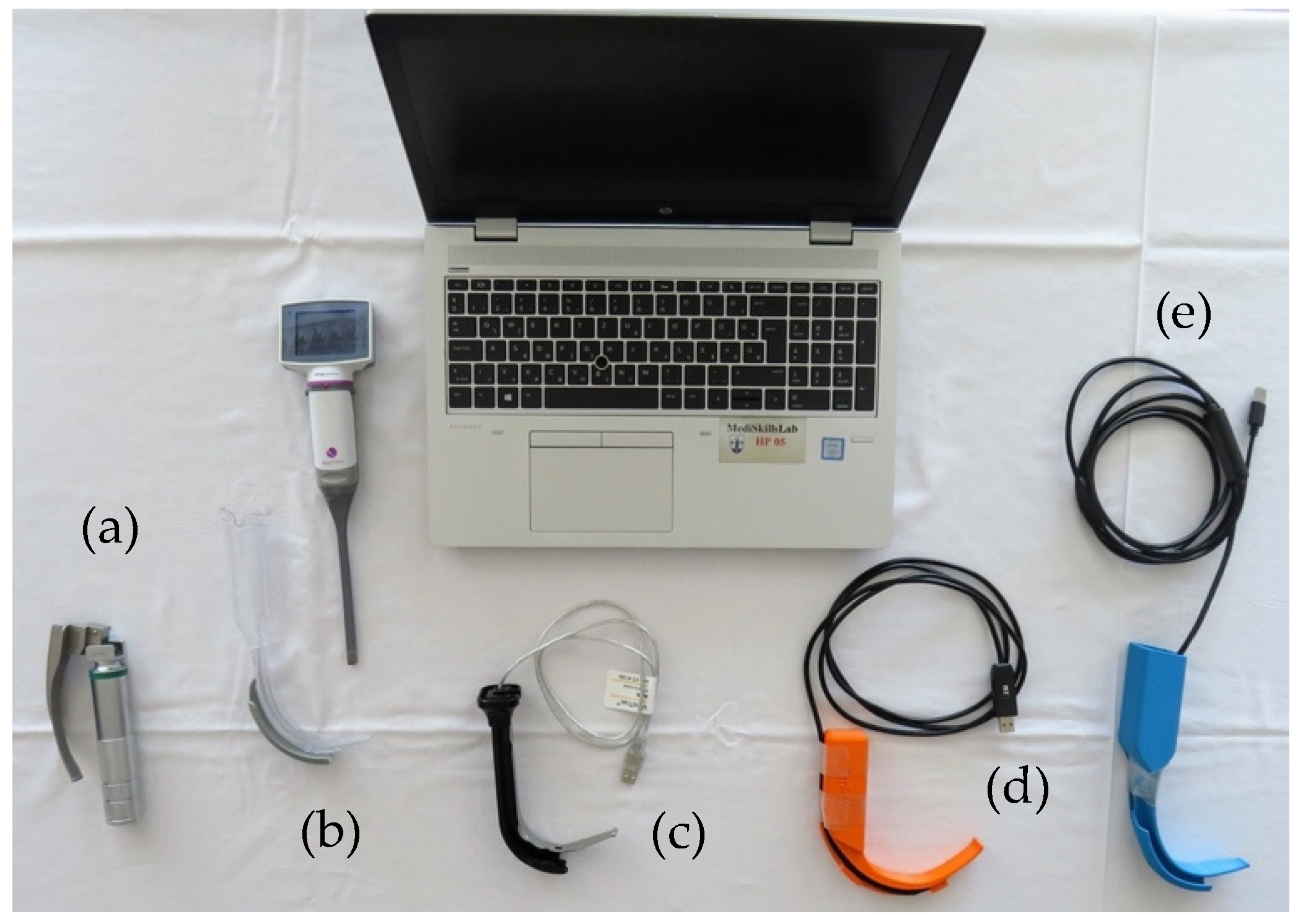
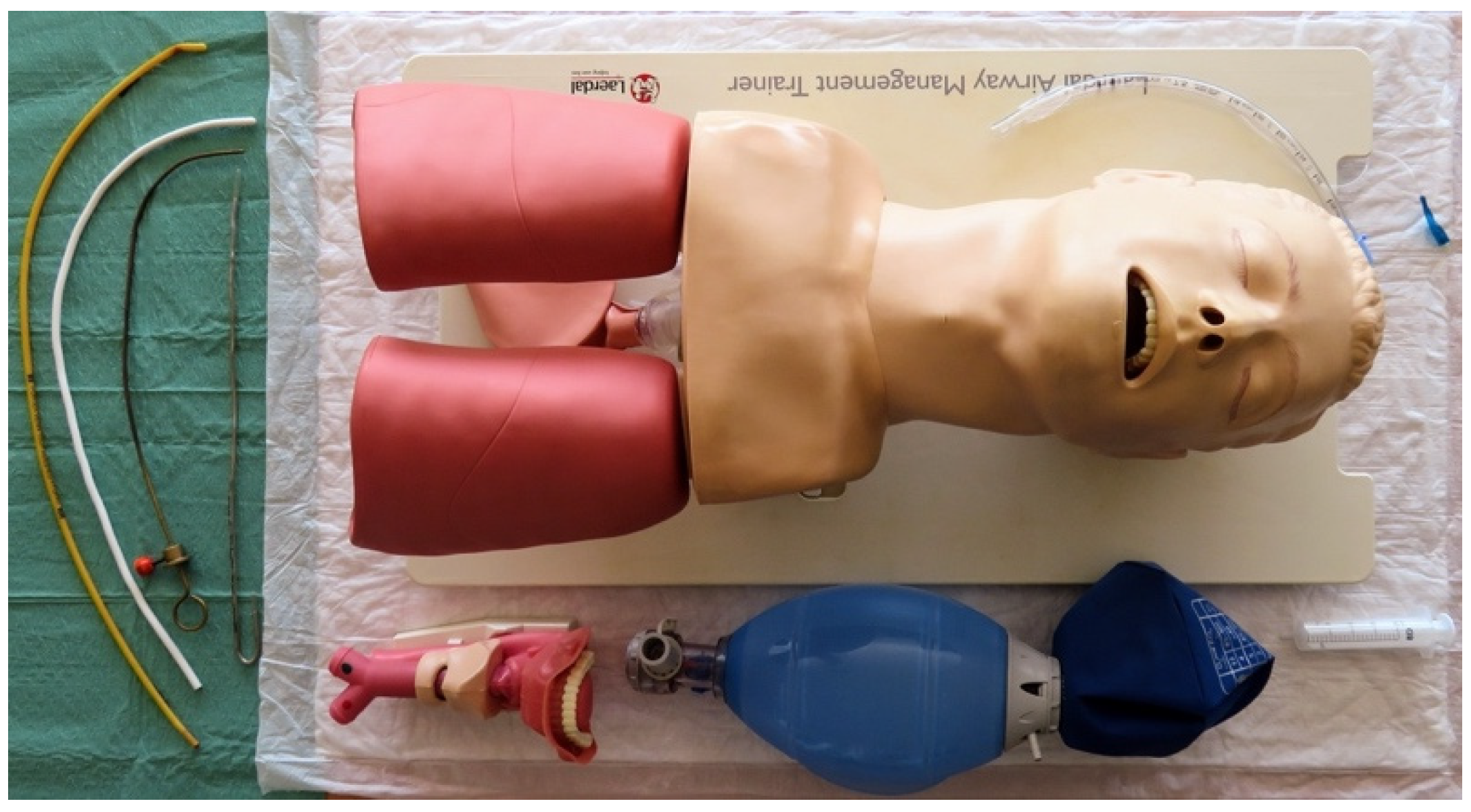
2. Materials and Methods
3. Results
3.1. Scenario A
3.2. Scenario B
4. Discussion
5. Conclusions
6. Limitations of the Study
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Acknowledgments
Conflicts of Interest
References
- Vogel, J.; Stübinger, S.; Kaufmann, M.; Krastl, G.; Filippi, A. Dental injuries resulting from tracheal intubation—A retrospective study. Dent. Traumatol. 2009, 25, 73–77. [Google Scholar] [CrossRef] [PubMed]
- Cook, T.M.; Macdougall-Davis, S.R. Complications and failure of airway management. Br. J. Anaesth. 2012, 109, i68–i85. [Google Scholar] [CrossRef] [PubMed]
- Pacheco-Lopez, P.C.; Berkow, L.C.; Hillel, A.T.; Akst, L.M. Complications of airway management. In Respiratory Care; American Association for Respiratory Care: Irving, TX, USA, 2014; pp. 1006–1021. [Google Scholar] [CrossRef]
- Russotto, V.; Myatra, S.N.; Laffey, J.G.; Tassistro, E.; Antolini, L.; Bauer, P.; Lascarrou, J.B.; Szuldrzynski, K.; Camporota, L.; Pelosi, P.; et al. Intubation Practices and Adverse Peri-intubation Events in Critically Ill Patients From 29 Countries. JAMA 2021, 325, 1164–1172. [Google Scholar] [CrossRef] [PubMed]
- Frerk, C.; Mitchell, V.; McNarry, A.; Mendonca, C.; Bhagrath, R.; Patel, A.; O’sullivan, E.; Woodall, N.; Ahmad, I. Difficult Airway Society 2015 guidelines for management of unanticipated difficult intubation in adults. Br. J. Anaesth. 2015, 115, 827–848. [Google Scholar] [CrossRef] [PubMed]
- Doyle, D.J. The GlideScope Video Laryngoscope: A Narrative Review. Open Anesthesiol. J. 2017, 11, 48–67. [Google Scholar] [CrossRef]
- Kleine-Brueggeney, M.; Greif, R.; Schoettker, P.; Savoldelli, G.L.; Nabecker, S.; Theiler, L.G. Evaluation of six videolaryngoscopes in 720 patients with a simulated difficult airway: A multicentre randomized controlled trial. Br. J. Anaesth. 2016, 116, 670–679. [Google Scholar] [CrossRef] [PubMed]
- Myatra, S.N.; Patwa, A.; Divatia, J.V. Videolaryngoscopy for all intubations: Is direct laryngoscopy obsolete? Indian. J. Anaesth. 2022, 66, 169–173. [Google Scholar] [CrossRef] [PubMed]
- Cook, T.M.; Aziz, M.F. Has the time really come for universal videolaryngoscopy? Br. J. Anaesth. 2022, 129, 474–477. [Google Scholar] [CrossRef] [PubMed]
- Hoshijima, H.; Mihara, T.; Maruyama, K.; Denawa, Y.; Mizuta, K.; Shiga, T.; Nagasaka, H. C-MAC videolaryngoscope versus Macintosh laryngoscope for tracheal intubation: A systematic review and meta-analysis with trial sequential analysis. J. Clin. Anesth. 2018, 49, 53–62. [Google Scholar] [CrossRef]
- Hoshijima, H.; Mihara, T.; Maruyama, K.; Denawa, Y.; Takahashi, M.; Shiga, T.; Nagasaka, H. McGrath videolaryngoscope versus Macintosh laryngoscope for tracheal intubation: A systematic review and meta-analysis with trial sequential analysis. J. Clin. Anesth. 2018, 46, 25–32. [Google Scholar] [CrossRef]
- Russell, T.M.; Hormis, A. Should the Glidescope video laryngoscope be used first line for all oral intubations or only in those with a difficult airway? A review of current literature. J. Perioper. Pract. 2018, 28, 322–333. [Google Scholar] [CrossRef] [PubMed]
- Griesdale, D.E.G.; Liu, D.; McKinney, J.; Choi, P.T. Glidescope ® video-laryngoscopy versus direct laryngoscopy for endotracheal intubation: A systematic review and meta-analysis. Can. J. Anesth. 2012, 59, 41–52. [Google Scholar] [CrossRef] [PubMed]
- Apfelbaum, J.L.; Hagberg, C.A.; Connis, R.T.; Abdelmalak, B.B.; Agarkar, M.; Dutton, R.P.; Fiadjoe, J.E.; Greif, R.; Klock, P.A.; Mercier, D.; et al. 2022 American Society of Anesthesiologists Practice Guidelines for Management of the Difficult Airway. Anesthesiology 2022, 136, 31–81. [Google Scholar] [CrossRef] [PubMed]
- Chemsian, R.; Bhananker, S.; Ramaiah, R. Videolaryngoscopy. Int. J. Crit. Illn. Inj. Sci. 2014, 4, 35. [Google Scholar] [CrossRef] [PubMed]
- Maharaj, C.H.; Costello, J.F.; Higgins, B.D.; Harte, B.H.; Laffey, J.G. Learning and performance of tracheal intubation by novice personnel: A comparison of the Airtraq® and Mancintosh laryngoscope. Anaesthesia 2006, 61, 671–677. [Google Scholar] [CrossRef] [PubMed]
- Ji, Y.; Ma, Z.; Peppelenbosch, M.P.; Pan, Q. Potential association between COVID-19 mortality and health-care resource availability. Lancet Glob. Health 2020, 8, e480. [Google Scholar] [CrossRef] [PubMed]
- Bong, C.L.; Brasher, C.; Chikumba, E.; Mcdougall, R.; Mellin-Olsen, J.; Enright, A. The COVID-19 Pandemic: Effects on Low- And Middle-Income Countries. Anesth. Analg. 2020, 131, 86–92. [Google Scholar] [CrossRef] [PubMed]
- Nauka, P.C.; Chen, J.T.; Shiloh, A.L.; Eisen, L.A.; Fein, D.G. Practice, Outcomes, and Complications of Emergent Endotracheal Intubation by Critical Care Practitioners During the COVID-19 Pandemic. Chest 2021, 160, 2112–2122. [Google Scholar] [CrossRef] [PubMed]
- Wax, R.S.; Christian, M.D. Practical recommendations for critical care and anesthesiology teams caring for novel coronavirus (2019-nCoV) patients. Can. J. Anesth. 2020, 67, 568–576. [Google Scholar] [CrossRef]
- Fillat-Gomà, F.; Coderch-Navarro, S.; Martínez-Carreres, L.; Monill-Raya, N.; Nadal-Mir, T.; Lalmolda, C.; Luján, M.; de Haro, C.; Blanch, L. Integrated 3D printing solution to mitigate shortages of airway consumables and personal protective equipment during the COVID-19 pandemic. BMC Health Serv. Res. 2020, 20, 1–8. [Google Scholar] [CrossRef]
- Told, R.; Marada, G.; Rendeki, S.; Pentek, A.; Nagy, B.; Molnar, F.J.; Maroti, P. Manufacturing a first upper molar dental forceps using continuous fiber reinforcement (Cfr) additive manufacturing technology with carbon-reinforced polyamide. Polymers 2021, 13, 2647. [Google Scholar] [CrossRef] [PubMed]
- Rendeki, S.; Nagy, B.; Bene, M.; Pentek, A.; Toth, L.; Szanto, Z.; Told, R.; Maroti, P. An overview on personal protective equipment (PPE) fabricated with additive manufacturing technologies in the era of COVID-19 pandemic. Polymers 2020, 12, 2703. [Google Scholar] [CrossRef] [PubMed]
- Aydin, A.; Demirtas, Z.; Ok, M.; Erkus, H.; Cebi, G.; Uysal, E.; Gunduz, O.; Ustundag, C.B. 3D printing in the battle against COVID-19. Emergent Mater. 2021, 4, 363–386. [Google Scholar]
- Longhitano, G.A.; Nunes, G.B.; Candido, G.; da Silva, J.V.L. The role of 3D printing during COVID-19 pandemic: A review. Prog. Addit. Manuf. 2021, 6, 19–37. [Google Scholar] [CrossRef] [PubMed]
- Wong, J.Y. Ultra-portable solar-powered 3D printers for onsite manufacturing of medical resources. Aerosp. Med. Hum. Perform. 2015, 86, 830–834. [Google Scholar] [CrossRef] [PubMed]
- Wong, J.Y.; Pfahnl, A.C. 3D printing of surgical instruments for long-duration space missions. Aviat. Space Env. Med. 2014, 85, 758–763. [Google Scholar] [CrossRef] [PubMed]
- Durfee, W.K.; Iaizzo, P.A. Medical applications of 3D printing. In Engineering in Medicine: Advances and Challenges; Elsevier: Amsterdam, The Netherlands, 2018; pp. 527–543. [Google Scholar] [CrossRef]
- Zuniga, J.M.; Young, K.J.; Peck, J.L.; Srivastava, R.; Pierce, J.E.; Dudley, D.R.; Salazar, D.A.; Bergmann, J. Remote fitting procedures for upper limb 3d printed prostheses. Expert. Rev. Med. Devices 2019, 16, 257–266. [Google Scholar] [CrossRef] [PubMed]
- Lambert, C.T.; John, S.C.; John, A.V. Development and performance testing of the low-cost, 3D-printed, smartphone-compatible ‘Tansen Videolaryngoscope’ vs. Pentax-AWS videolaryngoscope vs. direct Macintosh laryngoscope: A manikin study. Eur. J. Anaesthesiol. 2020, 37, 992–998. [Google Scholar] [CrossRef] [PubMed]
- Ataman, A.K.; Altıntas, E. Comparison of a commercial 3D fabricated laryngoscope (Airangel®) with a widely-used video laryngoscope (Glidescope®): Randomized controlled cross-over study. Trends Anaesth. Crit. Care 2021, 40, 35–40. [Google Scholar] [CrossRef]
- Gorman, L.; Dickson, A.N.; Monaghan, M.; Vaughan, F.; Murphy, B.; Dowling, D.P.; McCaul, C.; Jones, J.F. Novel co-axial, disposable, low-cost 3D printed videolaryngoscopes for patients with COVID-19: A manikin study. Eur. J. Anaesthesiol. Intensive Care 2023, 2, e0015. [Google Scholar] [CrossRef]
- Erel, K.V.; Karacan, N.Ü. Conventional videolaryngoscope versus 3D printed videolaryngoscope. J. Clin. Med. Kazakhstan 2023, 20, 60–64. [Google Scholar] [CrossRef] [PubMed]
- Fonternel, T.; van Rooyen, H.; Joubert, G.; Turton, E. Evaluating the Usability of a 3D-Printed Video Laryngoscope for Tracheal Intubation of a Manikin. Med. Devices 2023, 16, 157–165. [Google Scholar] [CrossRef] [PubMed]
- Brasel, K.J. Advanced trauma life support (ATLS®): The ninth edition. J. Trauma. Acute Care Surg. 2013, 74, 1363–1366. [Google Scholar] [CrossRef] [PubMed]
- Levitan, R.M.; Ochroch, E.A.; Shofer, F.S.; Hollander, J.E. Assessment of Airway Visualization: Validation of the Percentage of Glottic Opening (POGO) Scale. Acad. Emerg. Med. 1998, 5, 919–923. [Google Scholar] [CrossRef] [PubMed]
- Ali, M.S.; Bakri, M.H.; Mohamed, H.A.; Shehab, H.; al Taher, W. External laryngeal manipulation done by the laryngoscopist makes the best laryngeal view for intubation. Saudi J. Anaesth. 2014, 8, 351–354. [Google Scholar] [CrossRef] [PubMed]
- Pieters, B.M.A.; Wilbers, N.E.R.; Huijzer, M.; Winkens, B.; van Zundert, A.A.J. Comparison of seven videolaryngoscopes with the Macintosh laryngoscope in manikins by experienced and novice personnel. Anaesthesia 2016, 71, 556–564. [Google Scholar] [CrossRef]
- Malik, M.A.; O’Donoghue, C.; Carney, J.; Maharaj, C.H.; Harte, B.H.; Laffey, J.G. Comparison of the Glidescope®, the Pentax AWS®, and the Truview EVO2® with the Macintosh laryngoscope in experienced anaesthetists: A manikin study. Br. J. Anaesth. 2009, 102, 128–134. [Google Scholar] [CrossRef] [PubMed]
- Mulcaster, J.T.; Mills, J.; Hung, O.R.; MacQuarrie, K.; Law, J.A.; Pytka, S.; Imrie, D.; Field, C. Laryngoscopic Intubation Learning and Performance. J. Am. Soc. Anesthesiol. 2003, 98, 23–27. [Google Scholar] [CrossRef]
- Rendeki, S.; Keresztes, D.; Woth, G.; Mérei, Á.; Rozanovic, M.; Rendeki, M.; Farkas, J.; Mühl, D.; Nagy, B. Comparison of VividTrac®, Airtraq®, King Vision®, Macintosh Laryngoscope and a Custom-Made Videolaryngoscope for difficult and normal airways in mannequins by novices. BMC Anesthesiol. 2017, 17, 1–6. [Google Scholar] [CrossRef]
- Hoshijima, H.; Denawa, Y.; Tominaga, A.; Nakamura, C.; Shiga, T.; Nagasaka, H. Videolaryngoscope versus Macintosh laryngoscope for tracheal intubation in adults with obesity: A systematic review and meta-analysis. J. Clin. Anesth. 2018, 44, 69–75. [Google Scholar] [CrossRef]
- Kluj, P.; Fedorczak, A.; Fedorczak, M.; Gaszyński, T.; Kułak, C.; Wasilewski, M.; Znyk, M.; Bartczak, M.; Ratajczyk, P. Comparison of Three Video Laryngoscopes and Direct Laryngoscopy for Emergency Endotracheal Intubation While Wearing PPE-AGP: A Randomized, Crossover, Simulation Trial. Healthcare 2023, 11, 884. [Google Scholar] [CrossRef] [PubMed]
- Muhamed, L.; Parapurath, D.; Abna, P.K. Comparative analysis of direct laryngoscopy and video laryngoscopy performance by medical students in simulated airway management scenarios. Indian. J. Clin. Anaesth. 2024, 11, 53–61. [Google Scholar] [CrossRef]
- Narang, A.T.; Oldeg, P.F.; Medzon, R.; Mahmood, A.R.; Spector, J.A.; Robinett, D.A. Comparison of intubation success of video laryngoscopy versus direct laryngoscopy in the difficult airway using high-fidelity simulation. Simul. Health 2009, 4, 160–165. [Google Scholar] [CrossRef] [PubMed]
- La Via, L.; Messina, S.; Merola, F.; Tornitore, F.; Sanfilippo, G.; Santonocito, C.; Noto, A.; Longhini, F.; Astuto, M.; Sanfilippo, F. Combined laryngo-bronchoscopy intubation approach in the normal airway scenario: A simulation study on anesthesiology residents. Signa Vitae 2023, 19, 91–98. [Google Scholar]
- Biro, P.; Schlaepfer, M. Tracheal intubation with channeled vs. non-channeled videolaryngoscope blades. Rom. J. Anaesth. Intensive Care 2018, 25, 97. [Google Scholar] [CrossRef] [PubMed]
- Kriege, M.; Alflen, C.; Noppens, R.R. Using King Vision video laryngoscope with a channeled blade prolongs time for tracheal intubation in different training levels, compared to non-channeled blade. PLoS ONE 2017, 12, e0183382. [Google Scholar] [CrossRef] [PubMed]
- Nabecker, S.; Koennecke, X.; Theiler, L.; Riggenbach, C.; Greif, R.; Kleine-Brueggeney, M. Effect of the tube-guiding channel on intubation success with videolaryngoscopes. Trends Anaesth. Crit. Care 2018, 18, 16–22. [Google Scholar] [CrossRef]
- Kaplan, M.B.; Hagberg, C.A.; Ward, D.S.; Brambrink, A.; Chhibber, A.K.; Heidegger, T.; Lozada, L.; Ovassapian, A.; Parsons, D.; Ramsay, J.; et al. Comparison of direct and video-assisted views of the larynx during routine intubation. J. Clin. Anesth. 2006, 18, 357–362. [Google Scholar] [CrossRef] [PubMed]
- Ruetzler, K.; Imach, S.; Weiss, M.; Haas, T.; Schmidt, A.R. Vergleich von fünf Videolaryngoskopen und direkter konventioneller Laryngoskopie: Untersuchung des einfachen und simulierten schwierigen Atemweg am Intubationstrainer. Anaesthesist 2015, 64, 513–519. [Google Scholar] [CrossRef]
- Tan, Y.; Loganathan, N.; Thinn, K.K.; Liu, E.H.C.; Loh, N.H.W. Dental injury in anaesthesia: A tertiary hospital’s experience. BMC Anesthesiol. 2018, 18, 1–5. [Google Scholar] [CrossRef]
- Schieren, M.; Kleinschmidt, J.; Schmutz, A.; Loop, T.; Staat, M.; Gatzweiler, K.; Wappler, F.; Defosse, J. Comparison of forces acting on maxillary incisors during tracheal intubation with different laryngoscopy techniques: A blinded manikin study. Anaesthesia 2019, 74, 1563–1571. [Google Scholar] [CrossRef]
- Chew, S.H.; Lim, J.Z.M.; Chin, B.Z.B.; Chan, J.X.; Siew, R.C.H. Intubation with channeled versus non-channeled video laryngoscopes in simulated difficult airway by junior doctors in an out-of-hospital setting: A crossover manikin study. PLoS ONE 2019, 14, e0224017. [Google Scholar] [CrossRef]
| Scenario A | DL (n = 48) | 3DVL (n = 48) | KV (n = 48) | AAB (n = 48) | VT (n = 48) |
|---|---|---|---|---|---|
| Number of attempts (n, 1/2/3/not successful) | 43/2/1/2 | 46/2/0/0 ¶ | 45/2/0/1 | 38/9/0/1 §# | 48/0/0/0 ¶ |
| Laryngoscopy time (s) | 8.12 [6.79–10.46] | 7.44 [5.82–9.74] | 7.1 [5.55–9.37] ¶ | 8.95 [7.76–12.1] †§ | 7.14 [5.65–9.02] ¶ |
| Tube insertion time (s) | 5.46 [3.67–8.44] ¶† | 6.12 [3.25–10.25] † | 3.5 [2.21–5.45] *¶# | 8.64 [5.1–16.1] *†§ | 5.62 [3.1–7.1] ¶ |
| Intubation time (s) | 14.12 [11.69–18.22] ¶† | 14.23 [9.97–20.6] †¶ | 11.12 [8.8–12.9] *¶# | 18.68 [14.3–25.1] *†§# | 12.25 [9.98–15.29] ¶ |
| POGO (%) | 70 [50, 80] †§#¶ | 90 [85–95] *§ | 95 [80–100] *§ | 90 [70–95] *§ | 100 [95–100] *#†¶ |
| Ease of technical use (1–5) | 3 [2–3] §¶ | 2 [2–3] §¶ | 2 [1–2] ¶ | 3 [3–4] *#†§ | 1 [1–2] *#¶ |
| Ease of physical use (1–5) | 2 [2–3] †§ | 2 [1–3] ¶ | 1 [1–2] *¶ | 3 [2–3] #†§ | 1 [1–2] *¶ |
| Willingness of reuse (1–5) | 4 [3–5] †¶ | 4 [3–5] †¶§ | 5 [4–5] *#¶ | 3 [2–3] *#†§ | 5 [4–5] #¶ |
| Use of bougie (n) | 1 | 0 | 0 | 2 | 0 |
| Use of stylet (n) | 17 †§#¶ | 0 *¶ | 0 *¶ | 38 *†§# | 0 *¶ |
| Dental injury (n) | 17 †§# | 2 *¶ | 1 *¶ | 9 §†# | 1 *¶ |
| Esophageal intubation (n) | 3 | 0 | 0 | 0 | 0 |
| Scenario A | DL vs. 3DVL | DL vs. KV | DL vs. AAB | DL vs. VT | 3DVL vs. KV | 3DVL vs. AAB | 3DVL vs. VT | KV vs. AAB | KV vs. VT | AAB vs. VT |
|---|---|---|---|---|---|---|---|---|---|---|
| Number of attempts (n, 1/2/3/not successful) | NS | NS | NS | NS | NS | p < 0.05 | NS | NS | NS | p < 0.05 |
| Laryngoscopy time (s) | NS | NS | NS | NS | NS | NS | NS | p < 0.05 | NS | p < 0.05 |
| Tube insertion time (s) | NS | p < 0.05 | p < 0.05 | NS | p < 0.05 | NS | NS | p < 0.05 | NS | p < 0.05 |
| Intubation time (s) | NS | p < 0.05 | p < 0.05 | NS | p < 0.05 | p < 0.05 | NS | p < 0.05 | NS | p < 0.05 |
| POGO (%) | p < 0.05 | p < 0.05 | p < 0.05 | p < 0.05 | NS | NS | p < 0.05 | NS | p < 0.05 | p < 0.05 |
| Ease of technical use (1–5) | NS | NS | p < 0.05 | p < 0.05 | NS | p < 0.05 | p < 0.05 | p < 0.05 | NS | p < 0.05 |
| Ease of physical use (1–5) | NS | p < 0.05 | NS | p < 0.05 | NS | p < 0.05 | NS | p < 0.05 | NS | p < 0.05 |
| Willingness of reuse (1–5) | NS | p < 0.05 | p < 0.05 | NS | p < 0.05 | p < 0.05 | p < 0.05 | p < 0.05 | NS | p < 0.05 |
| Use of bougie (n) | NS | NS | NS | NS | NS | NS | NS | NS | NS | NS |
| Use of stylet (n) | p < 0.05 | p < 0.05 | p < 0.05 | p < 0.05 | NS | p < 0.05 | NS | p < 0.05 | NS | p < 0.05 |
| Dental injury (n) | p < 0.05 | p < 0.05 | NS | p < 0.05 | NS | p < 0.05 | NS | p < 0.05 | NS | p < 0.05 |
| Esophageal intubation (n) | NS | NS | NS | NS | NS | NS | NS | NS | NS | NS |
| Scenario B | DL (n = 48) | 3DVL (n = 48) | KV (n = 48) | AAB (n = 48) | VT (n = 48) |
|---|---|---|---|---|---|
| Number of attempts (n, 1/2/3/not successful) | 43/1/1/3 ¶ | 46/2/0/0 †¶ | 37/5/1/5 # | 33/11/1/3 *#§ | 45/2/1/0 ¶ |
| Laryngoscopy time (s) | 12.18 [9.03–18] †§ | 10.2 [7.7–13.3] | 8.6 [7–14.5] *¶ | 12.8 [7.37–11.7] †§ | 8.7 [6.9–10.3] *¶ |
| Tube insertion time (s) | 6.3 [3.8–11.1] #†§ | 2.6 [1.5–4.2] *¶ | 3.4 [2.1–5.2] *¶ | 8.1 [4.3–11.4] #†§ | 4.2 [2.4–6.7] *¶ |
| Intubation time (s) | 19.5 [14.9–26.1] #†§ | 14.5 [9.8–16.8] *¶ | 13 [10.3–20.1] *¶ | 21.2 [16.5–26.7] #†§ | 13.3 [10.3–18.1] *¶ |
| POGO (%) | 50 [32.5–60] #†§ | 65 [50–84] *¶ | 70 [50–80] *¶ | 50 [30–65] #†§ | 72.5 [60–90] *¶ |
| Ease of technical use (1–5) | 3 [2–4] #†§ | 2 [2–3] *¶ | 2 [2–3] *¶ | 3 [3–4] #†§ | 2 [2–3] *¶ |
| Ease of physical use (1–5) | 3 [2–4] #†§ | 2 [1–3] *¶ | 2 [1–3] *¶ | 3 [3–4] #†§ | 2 [1–2] *¶ |
| Willingness of reuse (1–5) | 3 [2–4] †§ | 4 [3–5] ¶ | 5 [4–5] *¶ | 3 [2–3] #†§ | 4 [4–5] *¶ |
| Use of bougie (n) | 6 #†§ | 0 * | 0 * | 1 | 0 * |
| Use of stylet (n) | 21 #†¶§ | 0 *¶ | 0 *¶ | 41 *#†§ | 0 *¶ |
| Dental injury (n) | 29 | 26 ¶ | 26 ¶ | 35 #† | 30 |
| Esophageal intubation (n) | 3 | 0 | 2 | 0 | 0 |
| Scenario B | DL vs. 3DVL | DL vs. KV | DL vs. AAB | DL vs. VT | 3DVL vs. KV | 3DVL vs. AAB | 3DVL vs. VT | KV vs. AAB | KV vs. VT | AAB vs. VT |
|---|---|---|---|---|---|---|---|---|---|---|
| Number of attempts (n, 1/2/3/not successful) | NS | NS | p < 0.05 | NS | p < 0.05 | p < 0.05 | NS | NS | NS | p < 0.05 |
| Laryngoscopy time (s) | NS | p < 0.05 | NS | p < 0.05 | NS | NS | NS | p < 0.05 | NS | p < 0.05 |
| Tube insertion time (s) | p < 0.05 | p < 0.05 | NS | p < 0.05 | NS | p < 0.05 | NS | p < 0.05 | NS | p < 0.05 |
| Intubation time (s) | p < 0.05 | p < 0.05 | NS | p < 0.05 | NS | p < 0.05 | NS | p < 0.05 | NS | p < 0.05 |
| POGO (%) | p < 0.05 | p < 0.05 | NS | p < 0.05 | NS | p < 0.05 | NS | p < 0.05 | NS | p < 0.05 |
| Ease of technical use (1–5) | p < 0.05 | p < 0.05 | NS | p < 0.05 | NS | p < 0.05 | NS | p < 0.05 | NS | p < 0.05 |
| Ease of physical use (1–5) | p < 0.05 | p < 0.05 | NS | p < 0.05 | NS | p < 0.05 | NS | p < 0.05 | NS | p < 0.05 |
| Willingness of reuse (1–5) | NS | p < 0.05 | NS | p < 0.05 | NS | p < 0.05 | NS | p < 0.05 | NS | p < 0.05 |
| Use of bougie (n) | p < 0.05 | p < 0.05 | NS | p < 0.05 | NS | NS | NS | NS | NS | NS |
| Use of stylet (n) | p < 0.05 | p < 0.05 | p < 0.05 | p < 0.05 | NS | p < 0.05 | NS | p < 0.05 | NS | p < 0.05 |
| Dental injury (n) | NS | NS | NS | NS | NS | p < 0.05 | NS | p < 0.05 | NS | NS |
| Esophageal intubation (n) | NS | NS | NS | NS | NS | NS | NS | NS | NS | NS |
Disclaimer/Publisher’s Note: The statements, opinions and data contained in all publications are solely those of the individual author(s) and contributor(s) and not of MDPI and/or the editor(s). MDPI and/or the editor(s) disclaim responsibility for any injury to people or property resulting from any ideas, methods, instructions or products referred to in the content. |
© 2024 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Bacher, V.; Németh, M.; Rendeki, S.; Tornai, B.; Rozanovic, M.; Pankaczi, A.; Oláh, J.; Farkas, J.; Chikhi, M.; Schlégl, Á.; et al. Comparison of Macintosh Laryngoscope, King Vision®, VividTrac®, AirAngel Blade®, and a Custom-Made 3D-Printed Video Laryngoscope for Difficult and Normal Airways in Mannequins by Novices—A Non-Inferiority Trial. J. Clin. Med. 2024, 13, 3213. https://doi.org/10.3390/jcm13113213
Bacher V, Németh M, Rendeki S, Tornai B, Rozanovic M, Pankaczi A, Oláh J, Farkas J, Chikhi M, Schlégl Á, et al. Comparison of Macintosh Laryngoscope, King Vision®, VividTrac®, AirAngel Blade®, and a Custom-Made 3D-Printed Video Laryngoscope for Difficult and Normal Airways in Mannequins by Novices—A Non-Inferiority Trial. Journal of Clinical Medicine. 2024; 13(11):3213. https://doi.org/10.3390/jcm13113213
Chicago/Turabian StyleBacher, Viktor, Márton Németh, Szilárd Rendeki, Balázs Tornai, Martin Rozanovic, Andrea Pankaczi, János Oláh, József Farkas, Melánia Chikhi, Ádám Schlégl, and et al. 2024. "Comparison of Macintosh Laryngoscope, King Vision®, VividTrac®, AirAngel Blade®, and a Custom-Made 3D-Printed Video Laryngoscope for Difficult and Normal Airways in Mannequins by Novices—A Non-Inferiority Trial" Journal of Clinical Medicine 13, no. 11: 3213. https://doi.org/10.3390/jcm13113213
APA StyleBacher, V., Németh, M., Rendeki, S., Tornai, B., Rozanovic, M., Pankaczi, A., Oláh, J., Farkas, J., Chikhi, M., Schlégl, Á., Maróti, P., & Nagy, B. (2024). Comparison of Macintosh Laryngoscope, King Vision®, VividTrac®, AirAngel Blade®, and a Custom-Made 3D-Printed Video Laryngoscope for Difficult and Normal Airways in Mannequins by Novices—A Non-Inferiority Trial. Journal of Clinical Medicine, 13(11), 3213. https://doi.org/10.3390/jcm13113213







